CHAPTER 6 Investigation of salivary gland disease
Introduction
This pathology division is reflected in the radiological techniques employed when imaging patients with salivary gland disease. For those patients presenting with inflammatory disease, plain film radiography, either alone or in combination with contrast studies and/or ultrasonography, often comprises ‘first-line’ imaging. These techniques provide the high resolution images with which to detail the presence of salivary calculi and allow the clinician to document accurately any significant changes within the ductal architecture of the gland. For those patients in whom a mass lesion is suspected then computed tomography (CT) and magnetic resonance imaging (MRI) are the imaging modalities of choice.
Sialography
Indications
Complementary and competing investigations
Ultrasonography
Newer ultrasound equipment exhibits high spatial resolution. This factor, combined with the relative superficial anatomical position of the salivary gland tissue relative to the ultrasound probe, allows the operator to obtain high definition images. Similarly, the superficial topography of the salivary gland tissue also permits fine-needle aspiration biopsy and core biopsy techniques to be performed with relative ease for both the patient and the operator (Bialek et al., 2006).
Computed tomography (CT)
Advantages of the technique
Magnetic resonance (MR)
Radioisotope imaging (sialoscintigraphy)
Advantages of the technique
Preoperative assessment of the patient and room preparation
The type of room used will be dependent on where the examination is performed. Sialography may well be performed in the dental chair in some institutions while, in others, a dedicated angiography room (Figure 6.1) may be used to conduct the examination.
Plain intraoral films for identifying calcified sialoliths
For the submandibular salivary gland:
An alternative method to the lower posterior oblique occlusal has been devised by Semple and Gibb (1982) for those patients who have a shortneck or limited neck movement. For those patients who cannot tolerate intraoral placement of dental films, a sectional panoramic radiograph related to the side under consideration or an extra-orally positioned occlusal film can be used (Harkin, 1983).
For the parotid salivary gland:
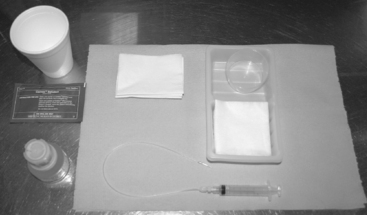
The basic equipment to perform sialography
The basic equipment to perform sialography is as follows:
The remaining equipment (Figures 6.3 and 6.4) comprises:
The standard procedure
Variation of the standard technique
Subtraction radiography
Post processing subtraction of bony structures provides the clinician with high definition sialographic images with which to evaluate the salivary gland ductal system. The equipment used is commonplace in digital imaging suites consisting of a C-arm, a 17 cm (smallest film/largest magnification) field image intensifier and a 512 × 512 matrix. The exposure sequence used is identical for both the parotid and the submandibular glands. It consists of one frame per second on a subtracted run followed by single acquired images. The contrast is hand injected allowing the operator to control visibly the volume of contrast entering the gland preventing overfilling.
For the parotid gland, the standard views are: a true lateral and an anteroposterior view followed by an emptying view post catheter removal. If emptying is delayed, then a sialogogue is given and a further lateral view is obtained. For the submandibular gland, the true lateral is the view of choice both for contrast filling of the gland, the emptying film and after the sialogogue has been administered (Ilgit et al., 1992; Buckenham et al., 1994).
Image interpretation
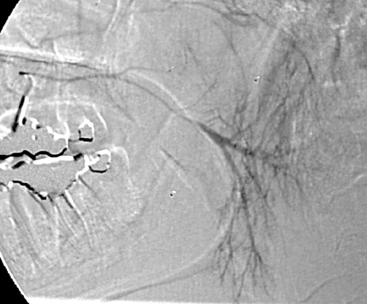
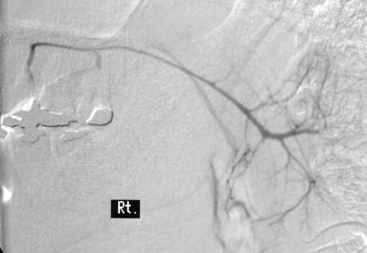
Before commencing sialography, the pattern of the normal anatomy of the parotid gland (Figure 6.6) and the submandibular gland (Figure 6.7) should be thoroughly understood.
The clinical presentation of patients requiring sialography can be summarized as follows:
Obstructive sialadenitis
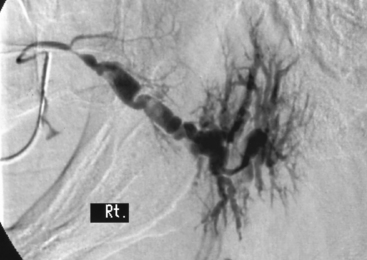
Obstructive sialadenitis is the result of recurrent infection within the salivary gland which usually results in a combination of both ductal strictures and dilation. The sialographic examination displays the extent of ductal damage within the gland due to these repeated inflammatory episodes. For those patients with grossly distorted ducts (Figure 6.8), gland removal is often the treatment of choice. Conversely, those patients with a localized focal stricture might well benefit from balloon dilatation. In addition, the status of the salivary gland ductal system in which a stone has recently been passed can also be assessed.
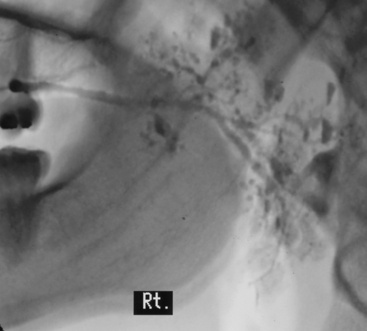
Autoimmune sialadenitis
The majority of patients presenting with this condition will be suffering from Sjögren’s syndrome (Roberts et al., 2008). The patients present with salivary gland enlargement and classification of the sialographic findings relate primarily to the size of the dilated secondary ducts. Punctate sialectasis is used to describe cases with dilation less than 1 mm in diameter, globular sialectasis for those between 1 and 2 mm and for those cases with non-uniform duct diameter greater than 2 mm, the term cavitatory sialectasis is used (Figure 6.10).
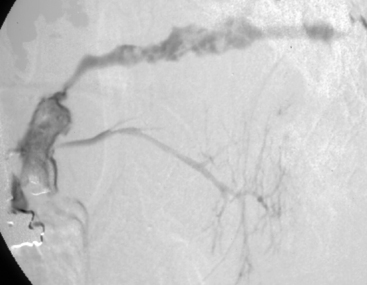
Trauma and post-trauma evaluation
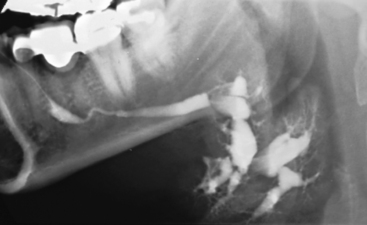
Sialography can be extremely useful in identifying the site and extent of duct and/or glandular trauma. Common findings are the presence of a fistula (Figure 6.11) or complete occlusion of the duct.
Bialek E.J., Jakubowski W., Zajkowski P., et al. US of the major salivary glands: anatomy and spatial relationships, pathological conditions and pitfalls. Radiographics. 2006;26:745-763.
Bradley M.J. Ultrasonography in the investigation of salivary gland disease. Dentomaxillofac. Radiol.. 1993;22:115-119.
Buckenham T.M., George C.D., McVicar D., Moody A.R., Coles G.S. Digital sialography: imaging and intervention. Br. J. Radiol.. 1994;67:524-529.
Harkin P. Demonstration of submandibular calculi. Radiography. 1983;49:84.
Ilgit E.T., Cizmeli O., Isit S., et al. Digital subtraction sialography: technique, advantages and results in 107 cases. Eur. J. Radiol.. 1992;15:244-247.
Roberts C., Parker G.J.M., et al. Glandular function in Sjögren’s syndrome: assessment with dynamic contrast enhanced MR imaging and tracer kinetic modelling-initial experience. Radiology. 2008;246:845-853.
Rushton V.E. Section 10: dental radiography. In Whitely A.S., editor: Clark’s positioning in radiography, twelth ed., Hodder Arnold Publication, 2005.
Semple J., Gibb D. The posterior-anterior lower occlusal view – a routine projection for the submandibular gland. Radiography. 1982;48:122-124.
Blair G.S. Hydrostatic sialography: an analysis of the technique. Oral Surg.. 1973;36:116-130.
Buckenham T.M., Page J.E., Jeddy T. Technical report: interventional sialography – balloon dilatation of a Stenson’s duct stricture using digital subtraction sialography. Clin. Radiol.. 1992;45:34.
Luyk N.H., Doyle T., Fergusson M.M. Recent trends in imaging the salivary glands. Dentomaxillofac. Radiol.. 1991;20:3-10.
McGurk M., Escudier M.P., Brown J.E. Modern management of salivary calculi. Br. J. Oral. Surg.. 2005;92:107-112.
Murray M.E., Buckenham T.M., Joseph A.E.A. The role of ultrasound in screening patients referred for sialography: a possible protocol. Clin. Otolaryngol. 1996;21:21-23.