Investigation of renal function (2)
Investigation of tubular function
The water deprivation test
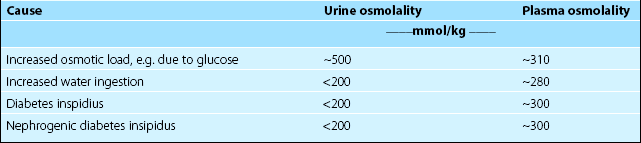
The causes of polyuria are summarized in Table 15.1. Renal tubular dysfunction is one of several causes of disordered water homeostasis. Where measurement of baseline urine osmolality is inconclusive, formal water deprivation may be indicated. The normal physiological response to water deprivation is water retention, which minimizes the rise in plasma osmolality that would otherwise be observed. The body achieves this water retention by means of AVP, the action of which on the renal tubules may be inferred from a rising urine osmolality. In practice, if the urine osmolality rises to 600 mmol/kg or more in response to water deprivation, diabetes insipidus is effectively excluded. A flat urine osmolality response is characteristically seen in diabetes insipidus where the hormone AVP is lacking. In compulsive water drinkers, a normal (rising) response is usually seen.
Urine pH and the acid load test
 Type I. There is defective hydrogen ion secretion in the distal tubule that may be inherited or acquired.
Type I. There is defective hydrogen ion secretion in the distal tubule that may be inherited or acquired.
 Type II. The capacity to reabsorb bicarbonate in the proximal tubule is reduced.
Type II. The capacity to reabsorb bicarbonate in the proximal tubule is reduced.
 Type III. Is a paediatric variant of type I renal tubular acidosis.
Type III. Is a paediatric variant of type I renal tubular acidosis.
 Type IV. Bicarbonate reabsorption by the renal tubule is impaired as a consequence of aldosterone deficiency, aldosterone receptor defects, or drugs which block aldosterone action.
Type IV. Bicarbonate reabsorption by the renal tubule is impaired as a consequence of aldosterone deficiency, aldosterone receptor defects, or drugs which block aldosterone action.
Specific proteinuria
Mention has already been made of protein in urine as an indicator of leaky glomeruli (p. 29). β2-microglobulin and α1-microglobulin are small proteins that are filtered at the glomeruli and are usually reabsorbed by the tubular cells. An increased concentration of these proteins in urine is a sensitive indicator of renal tubular cell damage. Proteinuria is discussed in detail on pages 34–35.
Specific tubular defects
Renal stones
Renal stones (calculi) produce severe pain and discomfort, and are common causes of obstruction in the urinary tract (Fig 15.1). Chemical analysis of renal stones is important in the investigation of why they have formed. Types of stone include:
 Calcium phosphate: may be a consequence of primary hyperparathyroidism or renal tubular acidosis.
Calcium phosphate: may be a consequence of primary hyperparathyroidism or renal tubular acidosis.
 Magnesium, ammonium and phosphate: are often associated with urinary tract infections.
Magnesium, ammonium and phosphate: are often associated with urinary tract infections.
 Oxalate: may be a consequence of hyperoxaluria.
Oxalate: may be a consequence of hyperoxaluria.
 Uric acid: may be a consequence of hyperuricaemia (see pp. 144–145).
Uric acid: may be a consequence of hyperuricaemia (see pp. 144–145).
 Cystine: these are rare and a feature of the inherited metabolic disorder cystinuria (see p. 162).
Cystine: these are rare and a feature of the inherited metabolic disorder cystinuria (see p. 162).