Investigation of renal function (1)
Functions of the kidney
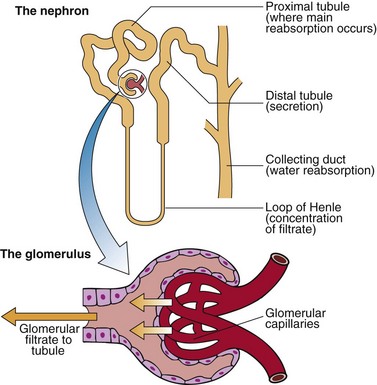
The functional unit of the kidney is the nephron, shown in Figure 14.1. The functions of the kidneys include:
 regulation of water, electrolyte and acid–base balance
regulation of water, electrolyte and acid–base balance
 excretion of the products of protein and nucleic acid metabolism: e.g. urea, creatinine and uric acid.
excretion of the products of protein and nucleic acid metabolism: e.g. urea, creatinine and uric acid.
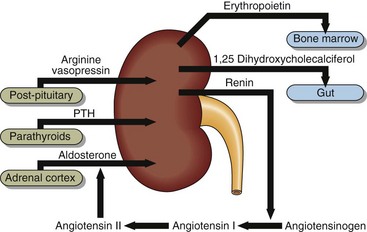
The kidneys are also endocrine organs, producing a number of hormones, and are subject to control by others (Fig 14.2). Arginine vasopressin (AVP) acts to influence water balance, and aldosterone affects sodium reabsorption in the nephron. Parathyroid hormone promotes tubular reabsorption of calcium, phosphate excretion and the synthesis of 1,25-dihydrocholecalciferol (the active form of vitamin D). Renin is made by the juxtaglomerular cells and catalyses the formation of angiotensin I and ultimately aldosterone synthesis.
It is convenient to discuss renal function in terms of glomerular and tubular function.
Glomerular function
The first step in urine formation is the filtration of plasma at the glomeruli (Fig 14.1). The glomerular filtration rate (GFR) is defined as the volume of plasma from which a given substance is completely cleared by glomerular filtration per unit time. This is approximately 140 mL/min in a healthy adult, but varies enormously with body size, and so is usually normalized to take account of this. Conventionally, it is corrected to a body surface area (BSA) of 1.73 m2 (so the units are mL/min/1.73 m2).
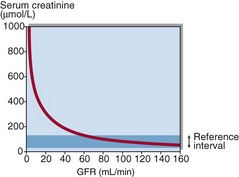
Historically, measurement of creatinine in serum has been used as a convenient but insensitive measure of glomerular function. Figure 14.3 shows that GFR has to halve before a significant rise in serum creatinine becomes apparent – a ‘normal’ serum creatinine does not necessarily mean all is well. By way of example, consider an asymptomatic person who shows a serum creatinine of 130 µmol/L:
Estimated GFR (eGFR)
The relatively poor inverse correlation between serum creatinine and GFR can be improved by taking into account some of the confounding variables, such as age, sex, ethnic origin and body weight. The formula developed by Cockcroft and Gault in the 1970s, and the four-variable equation derived more recently from the Modification of Diet in Renal Disease (MDRD) Study are the most widely used of these prediction equations. These are compared in Table 14.1.
Table 14.1
Cockcroft–Gault versus four-variable (‘simplified’) MDRD equation
| Cockcroft–Gault | Four-variable (‘simplified’) MDRD equation |
| Developed in the mid-1970s | Developed in the late 1990s |
| Incorporates age, sex and weight | Incorporates age, sex and ethnicity* |
| Widely used to calculate drug dosages | Widely used on biochemistry reports |
| Developed in a population with reduced GFR | Developed in a population with reduced GFR |
*But has only been validated in some ethnic groups, e.g. Caucasians, Afro-Caribbeans.
eGFR – additional observations
It is worth putting the limitations of eGFR outlined in the previous section into their proper context. Estimates of GFR e.g. the four-variable MDRD formula, are undoubtedly better than serum creatinine on its own at identifying reduced glomerular function, simply because they take some of the confounding variables into account (see Table 14.1). The Cockcroft–Gault formula requires weight in addition to age and sex (and creatinine) in order to be applied. It is therefore much easier to apply the MDRD formula which incorporates age, sex and ethnicity, but not weight. This is one of the reasons why the MDRD equation is widely used. However, Cockcroft–Gault is still widely used to calculate drug dosages.