Chapter 17 Introduction to ultrasound
 The sound waves are transmitted into the body and reflected back in varying amounts from an anatomical interface and these reflected waves are detected to produce an image.
The sound waves are transmitted into the body and reflected back in varying amounts from an anatomical interface and these reflected waves are detected to produce an image. Modern ultrasound machines interpret the returning signals to generate images, which they send either to film or to a picture archiving communication system.
Modern ultrasound machines interpret the returning signals to generate images, which they send either to film or to a picture archiving communication system. Ultrasound is operator dependent and improper use of ultrasound techniques and equipment can lead to missed or misdiagnosis.
Ultrasound is operator dependent and improper use of ultrasound techniques and equipment can lead to missed or misdiagnosis. Ultrasound studies include motion mode; spectral; colour and power Doppler; two-, three- and four-dimensional imaging.
Ultrasound studies include motion mode; spectral; colour and power Doppler; two-, three- and four-dimensional imaging. Although ultrasound has been in use for several decades with no proven evidence of damaging effects, high levels of ultrasound energy can cause bio effects in tissue; therefore prudent use of ultrasound is recommended.
Although ultrasound has been in use for several decades with no proven evidence of damaging effects, high levels of ultrasound energy can cause bio effects in tissue; therefore prudent use of ultrasound is recommended. Ergonomics play an important part in minimising ultrasound work related disorders, especially affecting the upper limbs due to repeated movements, stretching and twisting.
Ergonomics play an important part in minimising ultrasound work related disorders, especially affecting the upper limbs due to repeated movements, stretching and twisting. Training, quality assurance and audits are all important factors for maintaining high quality patient-focussed ultrasound examinations.
Training, quality assurance and audits are all important factors for maintaining high quality patient-focussed ultrasound examinations.SOUND WAVES
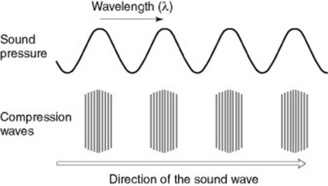
Sound is a wave that is created by vibrating objects and propagated through a medium from one location to another, via particle interaction (Fig. 17.1). These particles move in a direction parallel to the direction of the wave; that is, longitudinally. Each individual particle pushes on its neighbouring particle and propels it in a forwards direction whilst restoring its original position at the end of the interaction. This backwards and forwards motion of particles in the direction of the wave creates regions of high pressure within the medium, where the particles are compressed together (compressions), and also regions of low pressure, where the particles are spread apart (rarefactions). The wavelength of sound is the distance between two successive high pressure pulses or two successive low pressure pulses.
ULTRASOUND
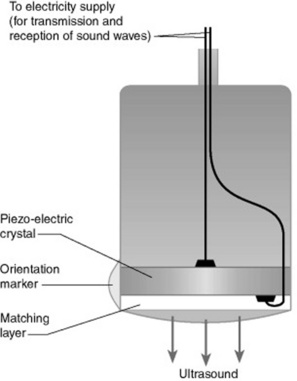
Ultrasound is high frequency sound beyond the hearing of the human ear. The frequencies of ultrasound required for diagnostic medical imaging are in the range 1–20 MHz. These frequencies can be obtained by using piezoelectric materials (particularly crystals). When an electric current is applied and reversed across a slice of one of these materials, the material contracts or expands. So a rapidly alternating electric field can cause a crystal to vibrate. These vibrations are then passed through any adjacent materials, or into the air as a longitudinal wave is produced – a sound wave (Fig. 17.2).
Normally the transmitting and receiving crystals are built into the same hand-held unit, known as an ultrasonic transducer or probe. The transducer emits ultrasound in rapid pulses and also acts as a receiver most of the time.
The speed of sound itself varies from one material to another (Table 17.1) and is dependent on temperature, pressure and other factors.
| Medium | Speed (m s−1) |
|---|---|
| Air | 330 |
| Water | 1497 |
| Fat | 1440 |
| Blood | 1570 |
| Metal | 3000–6000 |
| Soft tissue | 1540 |
ACOUSTIC IMPEDANCE
The strength of the reflected sound wave depends on the difference in ‘acoustic impedance’ between adjacent structures. The acoustic impedance of a medium is related to its density and the speed of sound through that medium (Table 17.2). The greater the difference in acoustic impedance between two adjacent structures, the more sound will be reflected, refracted or absorbed at their boundary rather than transmitted.
Table 17.2 Typical acoustic impedance of various mediums found in the body
| Medium | Acoustic impedance (in acoustic ohms) |
|---|---|
| Air | 0.000429 |
| Water | 1.50 |
| Blood | 1.59 |
| Fat | 1.38 |
| Muscle | 1.70 |
| Bone | 6.50 |
Example
On the other hand, body layers such as fat, muscle and many body organs have very similar acoustic impedances, enabling most of the beam to pass from one layer into the next, with only a small fraction being reflected, and making this modality ideal for imaging soft tissue organs (Table 17.3).
| Type of scan | How echo is received | Example of scan |
|---|---|---|
| A mode | Amplitude mode | Amplitude mode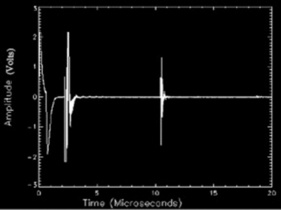 |
| Each layer producing a reflection shows up as a peak on the trace. The larger the echo, the higher the peak | ||
| B mode | Brightness mode | Musculoskeletal detail |
| Each reflecting echo is registered as a bright spot; the larger the amplitude of the reflecting echoes, the brighter the spots | ||
| M mode | Motion mode | Fetal pole (B mode) + waveform (M mode)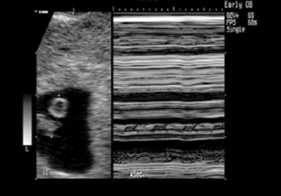 |
| Moving echoes are recorded to give traces of fetal heart pulsations |
ULTRASOUND ENERGY
There are two types of ultrasound energy used in diagnostics: continuous energy and pulsed energy.
TRANSDUCERS
Ultrasound transducers, also called probes, come in different shapes, sizes and frequencies to allow use in different scanning situations (Fig. 17.3). For example, in an obstetric or upper abdominal scan the transducer used is known as a ‘convex-array’ or curvilinear transducer. This contour allows the transducer to be moved across the abdomen whilst maintaining good contact with the abdominal surface and also giving the wide field of view needed to see the upper abdomen or the whole fetus. Examples of Doppler studies are spectral, colour and power Doppler.
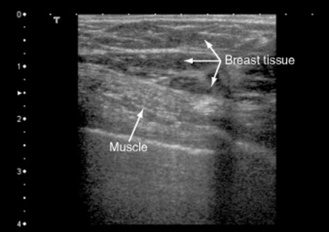
For thyroid, breast or musculoskeletal scans, a transducer with a flat surface – a ‘linear-array’ transducer – is commonly used.
FREQUENCY SELECTION
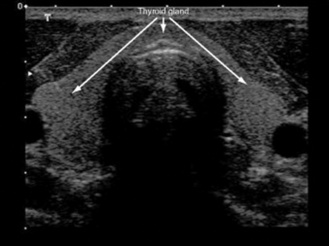
Typically, for general use of ultrasound in obstetrics and upper abdominal scans, a range of 3.5–6 MHz probe is suitable, and a high frequency transducer (7–12 MHz) can be used for scanning the thyroid gland, breast and testes. It can also be used to examine paediatric and neonatal patients.
SAFETY
A vast amount of research has been carried out in laboratories and animal studies to investigate the effect of using high intensity ultrasound. These studies have found that there are two main changes occurring within the body tissues:
ULTRASOUND MACHINES
Nowadays, advanced technology has enabled ultrasound machines to be smaller, more compact, more mobile and portable (Fig. 17.4). So ultrasound can be used in different settings – from departments with dedicated ultrasound rooms to bedside examinations where ultrasound can be used without moving the patient to another place. Wherever it is used, it important to select a machine that is fit for the purpose for which it is required (i.e. the needs of a department, particular clinic or practitioner).
APPLICATION OF ULTRASOUND TECHNIQUE
Ultrasound is usually utilised as a first line investigation, due to its advantages, but may have to be complemented with other cross-sectional imaging studies (e.g. MRI or CT). Information can be obtained by using different imaging planes, such as sagittal, coronal and transverse (Box 17.1).
ADVANTAGES OF ULTRASOUND COMPARED WITH OTHER MODALITIES
DISADVANTAGES OF ULTRASOUND COMPARED WITH OTHER MODALITIES
ROLE OF AN ULTRASOUND DEPARTMENT
PATIENT PREPARATION
The patient should eat and drink normally before and after the scan unless otherwise instructed; for example for gall bladder scans the patient will have to avoid fatty foods for 6 hours before the scan; for renal and bladder scans the patient will be required to attend with a full bladder. In obstetrics and gynaecology a full bladder may also be necessary to displace the bowel gas upwards and laterally to allow good visualisation of the pelvic structures. Usually patients are advised to carry on taking their usual medication.
COMMON APPLICATIONS OF ULTRASOUND
OBSTETRIC ULTRASOUND
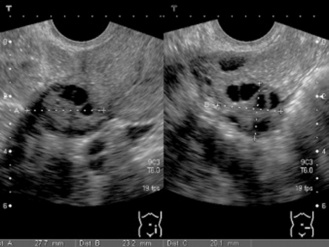
Early pregnancy
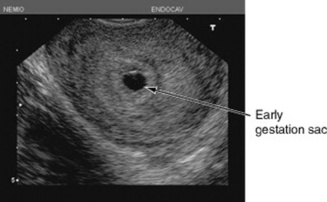
Diagnosis and confirmation of on-going early pregnancy can be done by a high frequency trans vaginal scan. A gestation sac can be seen as early as 5 weeks of pregnancy (Fig. 17.5). It is very important to initially confirm the site of the pregnancy within the cavity of the uterus, thereby excluding the possibility of an ectopic pregnancy (although in very rare cases, an intra- and extrauterine pregnancy can occur together). A fetal pole and a visible heartbeat can be detectable by ultrasound by about 6–7 weeks. For women with vaginal bleeding an ultrasound scan is important to exclude miscarriage. Complicated conditions such as molar pregnancies (a pre-cancerous condition of the placental tissue) can also be detected in time for effective management. Multiple pregnancies can be excluded or confirmed, and the type of twins (identical or non-identical – ‘chorionicity’) can also be determined by ultrasound (Fig. 17.6).
Dating pregnancies
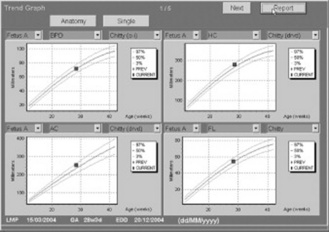
The establishment of correct gestational age and assessment of fetal size is very important for pregnancy management in terms of delivery and the timing of further tests; therefore ultrasounddating scans provide an accurate estimated date of delivery (EDD) by evaluating the fetal size. Fetal measurements (Table 17.4) include crown rump length (CRL), biparietal diameter (BPD), head circumference (HC) and femur length (FL). In later scans, the abdominal circumference (AC) is used in the assessment of fetal growth. Growth trends can be monitored by serial scans to exclude intrauterine growth retardation, or macrosomia in high-risk women (Fig. 17.7).
| Measurement | Example of scan |
|---|---|
Crown rump length (CR length) |
Bi-parietal diameter (head circumference, HC) |
Femur length (FL) |
Abdominal circumference (AC) |
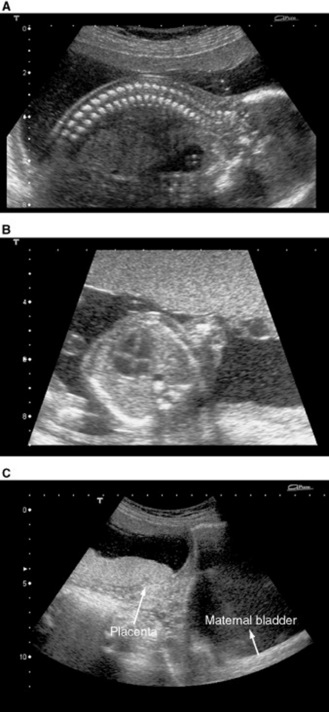
Diagnosis of fetal anomalies
The National Screening Committee recommends that every woman should be offered a routine scan to allow her the choice to screen her baby for abnormalities. This scan is usually performed at about 18–20 weeks of pregnancy (Fig. 17.8). Although ultrasound is sensitive for the detection of a variety of fetal anomalies, such as spina bifida, skeletal dysplasia, abdominal hernias, renal problems, it cannot detect all abnormalities as some problems may either be too subtle to be seen on a scan or develop late in pregnancy. Some fetal organs may be more challenging to assess; for example the detection of certain heart defects in the fetus is made more difficult, owing to its size and movement. Doppler studies of the fetal heart can be useful in some cases.
The placenta can also be assessed for its site to exclude complications in later pregnancies, such as placenta praevia (see Fig. 17.8C). Amniotic fluid volumes (liquor) can be assessed to exclude excessive (polyhydramnios) or reduced (oligohydramnios) liquor volumes in cases of certain fetal abnormalities or growth disorders. Fetal presentations (breech, oblique) and fetal intrauterine death can also be confirmed. A pregnancy scan may also reveal other pathology, such as uterine fibroids and ovarian cysts.
Fetal chromosomal disorders
Ultrasound is not very sensitive in the detection of chromosomal abnormalities; the most promising feature so far that is used in the assessment of Down syndrome is fetal nuchal translucency (fluid area behind the fetal neck; Fig. 17.9). This measurement can be used alongside blood results, fetal age, and maternal age to determine the risk of Down syndrome. Invasive diagnostic tests such as amniocentesis (sampling the liquor); chorionic villus sampling (CVS; sampling the placenta) andfetal blood sampling (from the umbilical cord) can be performed under ultrasound guidance to obtain fetal cells to determine the genetic composition (karyotype).
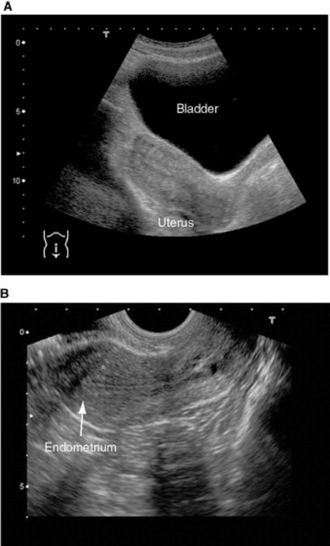
GYNAECOLOGICAL ULTRASOUND
Ultrasound is primarily used in the assessment of uterine and ovarian structures (Figs 17.10 and 17.11). The uterus can be examined to exclude normal uterine variants such as bicornuate or didelphic uterus, or pathologies in the presence of pelvic pain, abnormal vaginal bleeding or palpable masses within the pelvis. Pathologies such as fibroids, simple or complex ovarian cysts, endometrial polyps, tubo-ovarian abscess and suspected endometrial cancer can be detected by ultrasound. This modality is also very extensively used in the assessment and monitoring of patients with infertility, by monitoring and tracking follicular and endometrial development and determining correct timings for infertility procedures. The role of ultrasound in screening for ovarian cancer is still being researched, as the ultrasound appearances are sometimes very subtle to interpret in non-postmenopausal women.
ACUTE ABDOMINAL ULTRASOUND
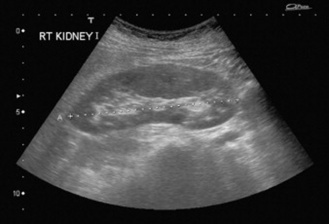
In acute medicine, ultrasound is an ideal first line investigation (Figs 17.12–17.15); for example forright upper quadrant pain, biliary colic can be assessed by investigating the gall bladder and the bile ducts to exclude stones. In cases of renal colic, obstruction can be detected by the presence of pelvicalyceal dilatation and the presence of calculi, depending on their size. Acute pancreatitis and cholecystitis may well present with an oedematous appearances and wall thickening. Acute pelvic pain can be investigated to exclude ectopic pregnancy, ruptured ovarian cysts or inflammation caused by appendicitis. Pyrexia can be as a result of abscesses present within the abdomen or acute appendicitis, which ultrasound scans can confirm or exclude.
In cases of blunt abdominal trauma, FAST scanning (Focussed Assessment with Sonography for Trauma), is used in some accident and emergency departments to determine any organ injury. A scan is performed to detect abnormal interabdominal fluid collections, which can be a result of haematomas and interabdominal bleeding.
NON-ACUTE ABDOMINAL ULTRASOUND
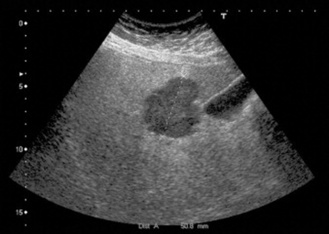
In the presence of abnormal liver function tests (LFTs), ultrasound can be used to assess the liver for obstructive jaundice and detect any focal lesions (e.g. metastasis, Fig. 17.16) or generaldiffuse disease such as cirrhosis. Hepato- or splenomegaly can be assessed by measurements and reference to the normal ranges. In urogenital cases, congenital renal abnormalities can be excluded, such as ectopic or horseshoe kidney, and the kidneys can be examined to exclude any focal benign or malignant lesions, stones or obstruction. Urinary bladder volumes can be calculated if required. Inflammatory conditions like acute or chronic cholecystitis and pancreatitis can be excluded with ultrasound. Ultrasound is also a useful screening tool for the detection of abdominal aortic aneurysm by measuring the diameter of the aorta (Fig. 17.17). Depending on the size of the aneurysm, the patients can either be monitored over a period of time for any changes or referred for surgery. Ultrasound is an accepted tool to investigate and monitor patients after renal transplants to detect any signs of rejection.
HEAD AND NECK ULTRASOUND
Ultrasound can be useful in cases of abnormal thyroid function tests in detecting palpable thyroid lumps, enlarged thyroids and non-functioning thyroids (Fig. 17.18). Pathology such as nodular goitres and cystic disease can be detected in cases of thyroid lumps; it is not always possible to distinguish between benign and malignant tumours. Parathyroid glands are difficult to see on an ultrasound scan unless there is enlargement present due to disease. Salivary glands (i.e. parotid, submandibular and sublingual glands) can also be assessed with ultrasound to exclude pathology such as inflammation, stones and benign or malignant tumours. Doppler colour flow studies, fine needle aspirations (FNAs) and biopsies under ultrasound control may be necessary for further evaluation.
BREAST ULTRASOUND
Ultrasound can provide information concerning the breasts and the axillary lymph nodes (Fig. 17.19). It acts as a complementary imaging modality to characterise lesions that are non-specific on amammogram. It is also the method of choice over mammograms when examining patients with a breast prosthesis. It can detect benign breast changes such as adenomas and cystic disease. However, FNAs and biopsies are needed to confirm more sinister pathology such as breast carcinomas.
VASCULAR ULTRASOUND
Using the Doppler principle, blood flow can be assessed with ultrasound (Figs 17.20 and 17.21). Complications such as stenosis of a blood vessel (narrowing), thrombus (blood clot) andassociated haemodynamics can be easily assessed. It is also used to detect various other conditions such as ischaemic stroke, vascular occlusion and blood vessel malformation.
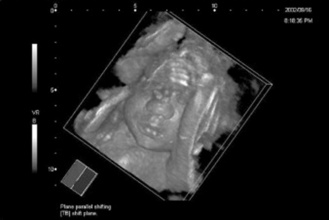
3D ULTRASOUND
3D scans require special transducers and software to accumulate and render the images, and with advancing technology the rendering time has been reduced from minutes to seconds (Fig. 17.22). A good 3D image is often quite impressive and further 2D scans may be extracted from 3D blocks of scanned information. Volumetricmeasurements are more accurate and sonographers can appreciate the presence or absence of a certain abnormality in a 3D scan more easily than in a 2D one; for example a cleft lip. There is also the possibility, in obstetric ultrasound, of increasing psychological bonding between the parents and the unborn baby. The ability to obtain a good 3D picture is nevertheless still very much dependent on operator skill. Its greatest potential is still in research, and particularly in the study of fetal embryology.
THE FUTURE OF ULTRASOUND
Ultrasound has established its role in modern medicine, and its future is ensured until an alternative imaging modality emerges that offers similar advantages of rapidity, accuracy and cheapness. With advancing computer and software technology, ultrasound machines will most likely become more sophisticated, with better image quality, and have more memory for storing data. Transducer probes may get smaller; more intracavity applications will be developed to gain better images of internal organs. 3D and 4D (real-time 3D) ultrasound will be more highly developed and become more popular. Wireless technology will minimise work-related disorders by enabling sonographers to control the ultrasound machine remotely and by voice activation. Ultrasound practices are destined to move further into every field of medicine, not only in diagnostic capabilities but also in the treatment of diseases.
Bates J. Practical gynaecological ultrasound, 2nd revised edn. Cambridge, UK: Cambridge University Press, 2006.
Bates JA. Abdominal ultrasound: how, why and when. London: Churchill Livingstone, 2004.
Bradley M, O’Donnell P, editors. Atlas of musculoskeletal ultrasound anatomy. London: Greenwich Medical Media, 2003.
Cardenosa G. Breast imaging. Baltimore: Lippincott Williams & Wilkins, 2000.
Chudleigh P, Thilaganathan B. Obstetric ultrasound: how, why and when, 2nd edn. London: Churchill Livingstone, 2004.
College of Radiographers. Occupational standards for diagnostic ultrasound: an abridged version. London: College of Radiographers, 1999.
De Bruyn R. Paediatric ultrasound: how, why, when. London: Churchill Livingstone, 2004.
Gaspari R. Emergency ultrasound; principles and practice. Philadelphia: Mosby, 2005.
Hoskins P. Diagnostic ultrasound physics and equipment. London: Greenwich Medical Media, 2002.
Kremkau FW. Diagnostic ultrasound: principles and instruments, 7th edn. Philadelphia: WB Saunders, 2005.
Kurjak A, Jackson D. Atlas of three- and four-dimensional sonography. London: Taylor and Francis, 2004.
Rumack CM, Wilson SR, Charboneau JM. Diagnostic ultrasound. Philadelphia: Mosby, 1998.
Sidhu P. Ultrasound of abdominal transplantation. St Louis: Thieme Publishing Group, 2002.
Tempkin BB. Ultrasound scanning: principles and protocols, 3rd edn. Philadelphia: WB Saunders, 2007.
Ter Haar G, Duck FA, editors. The safe use of ultrasound in medical diagnosis. London: British Institute of Radiology, 2000.
Thrush A. Peripheral vascular ultrasound: how, why and when. London: Greenwich Medical Media, 2000.
Twining P, McHugo JM, Pilling DW, editors. Textbook of fetal abnormalities. Edinburgh: Churchill Livingstone, 2006.
Zagzebski JA. Essentials of ultrasound physics. Philadelphia: Mosby, 1996.