26
Introduction to Orthotics and Prosthetics
1. Define the terms orthotics and prosthetics.
2. Obtain basic understanding of materials.
3. Learn the nomenclature—the naming of orthoses and prostheses in relation to the joint they support or replace.
4. Describe the key differences when off-the-shelf orthoses can be chosen instead of custom fabricated.
5. Have a general understanding of orthotic options for supporting major joints in the body.
6. List levels of amputation sites as well as the reasons for amputation.
7. Develop an understanding of basic prosthetic componentry and how the selection of componentry relates to patient function and outcome.
The process developed for naming orthoses and prostheses is a fairly simple technique. The International Standards Organization (ISO) recognizes common descriptors for orthoses and prostheses, based on the acronyms from the body joint or joints that are supported or replaced (Table 26-1). This method of nomenclature is both effective and easily learned.
Table 26-1
ISO Naming Conventions for Orthoses and Prostheses
| Device Type | Amputation Level | Nomenclature | |
| Orthoses | Upper extremity | Finger orthosis | FO |
| Hand orthosis | HO | ||
| Wrist-hand orthosis | WHO | ||
| Wrist orthosis | WO | ||
| Elbow orthosis | EO | ||
| Elbow-wrist-hand orthosis | EWHO | ||
| Shoulder orthosis | SO | ||
| Spinal | Cervical-thoracic-lumbosacral orthosis | CTLSO | |
| Cervical orthosis | CO | ||
| Thoracic-lumbosacral orthosis | TLSO | ||
| Lumbosacral orthosis | LSO | ||
| Sacroiliac orthosis | SIO | ||
| Lower extremity | Foot orthosis | FO | |
| Knee orthosis | KO | ||
| Ankle-foot orthosis | AFO | ||
| Knee-ankle-foot orthosis | KAFO | ||
| Hip-knee-ankle-foot orthosis | HKAFO | ||
| Prostheses | Upper extremity | Shoulder disarticulation | SD |
| Trans-humeral | TH | ||
| Elbow disarticulation | ED | ||
| Trans-radial | TR | ||
| Wrist disarticulation | WD | ||
| Lower extremity | Hip disarticulation | HD | |
| Trans-femoral | TF | ||
| Knee disarticulation | KD | ||
| Trans-tibial | TT | ||
| Ankle disarticulation | Symes | ||
| Trans-metatarsal amputation | TMA | ||
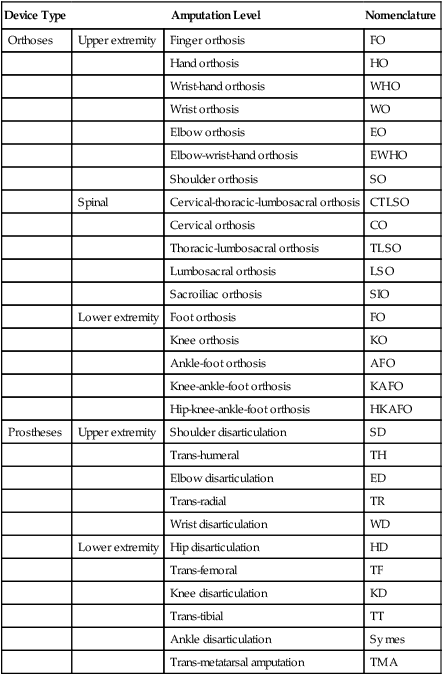
From Shurr DG, Michael JW: Prosthetics and orthotics, ed 2, Upper Saddle River, NJ, 2002, Prentice Hall, p 16.
PROSTHETICS
A prosthesis is any device that replaces a body part. This group consists of arms, legs, partial feet, hands, ears, breasts, and so on. The goal for each prosthesis is to provide function, body balance, ease of use, and optimal cosmesis in order to restore self image, quality of life, and independence (Table 26-2). Prostheses are custom fabricated and require adjustments and realignment on a regular basis.
Table 26-2
Specifications for the Ideal Prosthesis/Orthosis
| Need | Definition |
| Function | Meets the user’s needs, simple, easily learned, dependable |
| Comfort | Fits well, easy to don/doff, lightweight, adjustable |
| Cosmesis | Looks, smells, sounds “normal,” cleans easily, stain-resistant |
| Fabrication | Fast, modular, readily and widely available |
| Economics | Affordable, worth cost of monetary investment |
From Shurr DG, Michael JW: Prosthetics and orthotics, ed 2, Upper Saddle River, NJ, 2002, Prentice Hall, p 29.
Fitting for Orthoses or Prostheses
Material Selection
When fabricating orthoses and prostheses, the material selection is the first consideration of the process. There are multiple types of thermoplastics, metals, carbon fiber composites, and interface materials to choose from. Each type of material will have certain desirable characteristics or properties that will best suit each patient’s needs. Body weight, activity level, amount of rigidity needed, flexibility of material, energy storing properties, amount of cushioning required, and patient strength are all variables to consider when selecting fabrication materials (Table 26-3).
Table 26-3
Important Characteristics of Prosthetic and Orthotic Materials
| Need | Definition |
| Strength | Maximum external load that can be withstood |
| Stiffness | Stress/strain or force-to-displacement ratio |
| Durability | Ability to withstand repeated loading |
| Density | Weight per unit volume |
| Corrosion resistance | Resistance to chemical degradation |
| Ease of fabrication | Equipment and techniques needed to shape it |
From Shurr DG, Michael JW: Prosthetics and orthotics, ed 2, Upper Saddle River, NJ, 2002, Prentice Hall, p 29.
DEVICE SELECTION
Orthoses
Upper Extremity
Fingers, hand, and wrist
A splint for the fingers and hand should only support the affected joint or joints and allow the unaffected joints free ROM. There are single joint splints for the fingers available, such as proximal interphalangeal (PIP) and distal interphalangeal (DIP) splints which maintain or promote active range of motion (AROM) in the phalanges after sprains, fractures, or contractures. Some splints maintain or hold the joint in a fixed position, whereas dynamic splints that are spring-loaded allow the patient some movement of flexion or extension while applying constant force in the desired direction (Fig. 26-1). One particular type of wrist-hand-finger orthosis (WHFO) is the Thomas suspension splint. The function of this splint is to apply tension to the wrist joint and thumb in order to dorsiflex the wrist for diagnoses such as radial palsy. The long opponens splint is often used for flexion contractures, nerve or tendon damage due to traumatic accidents, or rheumatoid arthritis. These splints offer dynamic finger extension and allow the patient to use flexors needed for gripping.
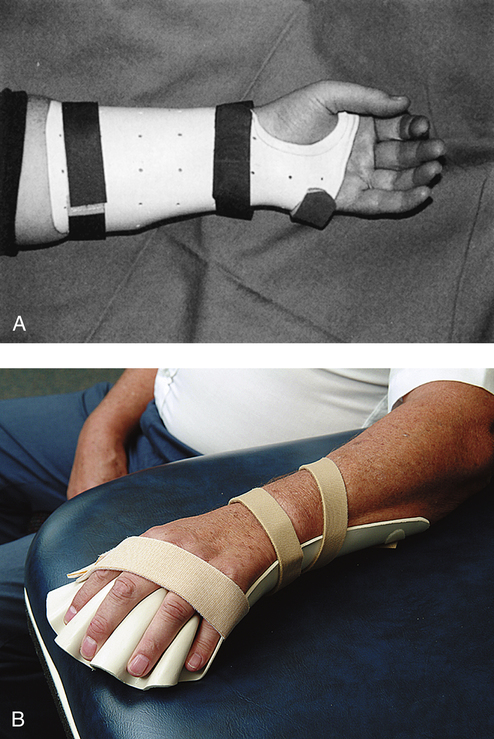
Another example of a functional custom fabricated WHFO is the tenodesis splint (also known as a wrist action splint) (Fig. 26-2). This splint is used to increase functional levels and independence mainly for quadriplegia. The design is ultra lightweight and uses the available ability to flex the wrist to accentuate the natural movement of opposition for gripping objects by using the three-jaw chuck pinch position. The wrist-driven wrist/hand orthosis employs the flexor hinge principle. The fingers and thumb are stabilized in the position of function. A small amount of wrist extensor strength will create flexion motion in the metacarpal phalangeal (MP) joints to produce adequate pinch for a variety of daily activities. Because it is custom fabricated, this style of splint requires a cast of the hand and forearm and measurements for fabrication.
There are multiple orthotic options available when supporting the hand and wrist, depending on the diagnosis and desired limitations for movement. For diagnoses such as carpal tunnel syndrome, tendonitis, or a sprain, a cock-up wrist splint, which holds the wrist in a neutral position is the most common choice (Fig. 26-3, A). This splint is a prefabricated brace that is readily available in varying sizes. For diagnoses such as a contracture secondary to a cerebral vascular accident (CVA) or rheumatoid arthritis (RA), a prefabricated malleable wrist-hand-finger orthosis will suffice. This orthosis is progressive in design because the wrist joint and finger platform is easily flexed or extended to accommodate gains made by stretching protocols in physical therapy sessions. These prefabricated, lightweight splints are called platform or resting splints and provide static positioning (Fig. 26-3, B). Some of the soft versions of these splints are more skin-friendly because they offer the option of a cover that can be removed and washed, which promotes good hygiene.
Elbow
Fitting choices for elbow orthoses can usually be prefabricated. A lateral epicondylitis splint (a band with a silicone or air pocket), is used to disperse the pressure placed on the tendon caused by use over a greater area, thus decreasing the point of high stress and pain (Fig. 26-4). ROM splints that limit AROM or provide pressure to increase ROM can also be purchased as prefabricated orthoses. The Flex POP Elbow Orthosis by RCAI (St. Petersburg, Fla.), for example, provides rehabilitation for joint stiffness and contractures, instabilities, strains, sprains, and ligament repairs. This ROM elbow orthosis offers flexion/extension stop sets at 5-degree increments, which allows changes to be made in therapy sessions as the patient progresses. Dynamic elbow splints can be used when the function desired is to gain ROM by applying a constant stretch to the elbow joint tendons and muscles. Protocols are set for wear time and when the tension placed upon the joint can be increased. Static splints can be set to a designated degree of flexion or extension and depending upon the style or brand, may or may not be adjustable. The physician’s prescription, rehabilitation protocols, and the patient’s level of compliance and tolerance all contribute to the decision-making process when fitting these types of elbow splints. Elbow contractures can be caused by a variety of injuries or diseases, such as cerebral palsy and CVA.
Shoulder
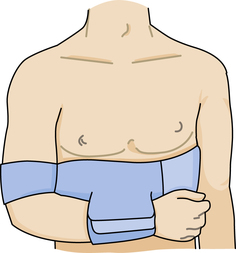
Shoulder splinting for immobilization can use a sling and swath or a shoulder immobilizer that will support the shoulder joint. One commonly used design utilizes a chest band, upper arm cuff, and a forearm cuff that is adjustable and positions the arm securely against the body (Fig. 26-5). If the required position is abduction, then an airplane splint can be fitted.
Specialized orthoses for the upper extremity
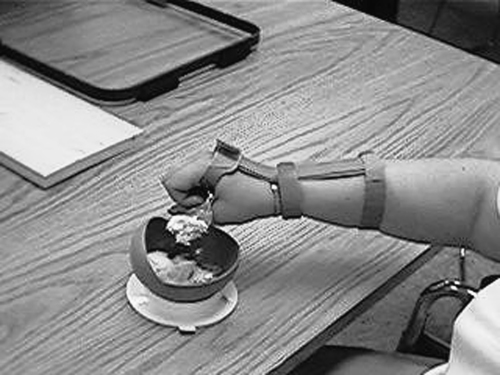
ADLs require a multitude of orthoses to promote independence for individuals who have suffered a stroke or debilitating injury. There are hand and wrist splints that are used to assist with feeding oneself, holding an ink pen, using a brush, and so on (Fig. 26-6). There are many types of foam available to place around utensils and items with handles to increase their circumference, therefore decreasing the grip strength and ROM needed to hold and use such items.
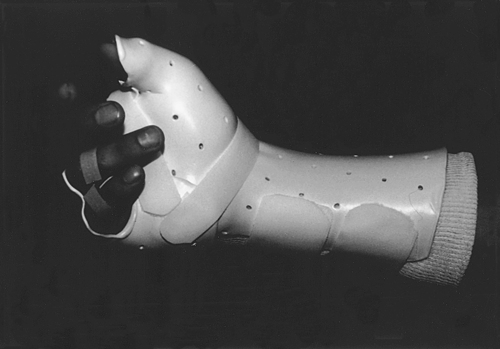
Fracture splinting uses a compression method for stabilization of the fracture site. The compression of fluid and soft tissue around the fracture site is key when providing a femoral, humeral, radial, or ulnar splint. These splints can be modified to a custom fit by heating and/or adding a soft interface material to provide added comfort. The fracture splint is a bivalve, two-piece orthosis and uses adjustable hook and loop strapping (Fig. 26-7). The splint will allow movement of the unaffected joints such as elbow and wrist for the ulnar fracture. The technique and principles used in splinting for upper extremity fractures is the same for lower extremity fractures.
Spine and Trunk
Cervical spine
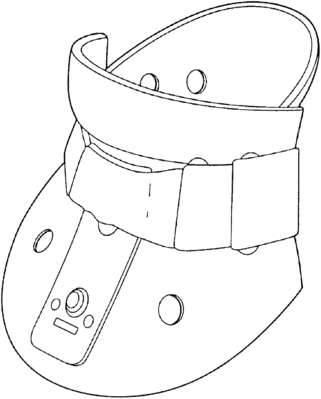
Cervical orthoses are fitted for the purpose of supporting the cervical muscles; limiting rotation, flexion, and extension; or immobilization of the cervical spine. A soft cervical collar can be fitted for lesser injuries such as sprains and strains. The soft collar is a prefabricated orthosis made of foam with a cotton cover and has a hook and loop closure in the back (Fig. 26-8). They are available in different heights and lengths. A cervicothoracic orthosis is a semirigid, two-piece brace that can be fitted for whiplash, degenerative joint disease, arthritis, and presurgical or postsurgical repairs. These collars are adjustable in height, circumference, and rigidity, but, as with all bracing, the therapist must always check pressure points to make sure that there is no skin breakdown.
Lumbosacral spine
There are numerous styles of rigid back panel LSOs. Depending upon where the injury or disease is in the lumbar region, there are two choices for which orthosis style to fit. If the region lies between L1 and L5, there are supports that fit and support this narrow region. This type of orthosis limits motion in the sagittal plane. This support is created by intracavity pressure to reduce the intervertebral load on the discs. The Aspen QuickDraw RAP is an example of a prefabricated orthosis that falls into this category. This LSO is easy to don and doff, which contributes to the compliance of the patient in wearing the support. It is fabricated of a material that is made to be worn next to the skin. This decreases the occurrence of migration. The fabric is lightweight and breathable, which makes cleaning easier and prolongs the life of the orthosis and increases the patient’s hygiene. The back panel has a pocket in which to insert the customizable rigid panel, and a hot or cold pack can be placed in the pocket for therapeutic benefit. This LSO uses effective compression and leverage to give strong support and immediate pain relief.3
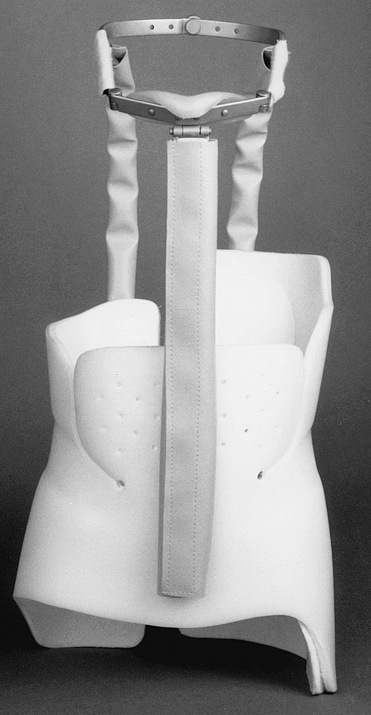
An LSO can be transformed into a thoracolumbosacral orthosis (TLSO) by adding shoulder straps, chest panel, and the torso straps. With the additional strapping and pads, the region of support now includes the posterior side from the sacrococcygeal junction to just inferior to the scapular spine. The anterior section of the TLSO extends from the symphysis pubis to the sternal notch, restricting motion in the transverse and sagittal planes and therefore restricting gross trunk movement (Fig. 26-9). TLSOs also provide intracavity pressure to the lumbar and lower thoracic region. Typically, using the least software and hardware necessary makes it easier to don and doff the orthosis. Therefore a higher level of compliance by the wearer is required when adding more componentry (or pieces) to the orthosis.2
In order to provide complete spinal support throughout the cervical to lumbar vertebrae, a cervicalthoracolumbosacral orthosis (CTLSO) should be fitted. A CTLSO has a mandibular piece on which the chin rests (Fig. 26-10). A forehead strap is also incorporated to assist in controlling the rotation on the head. This type of orthosis is very rigid and therefore immobilizing. These devices are usually fitted for degenerative diseases, fractures, or after spinal surgeries.
Lower Extremity
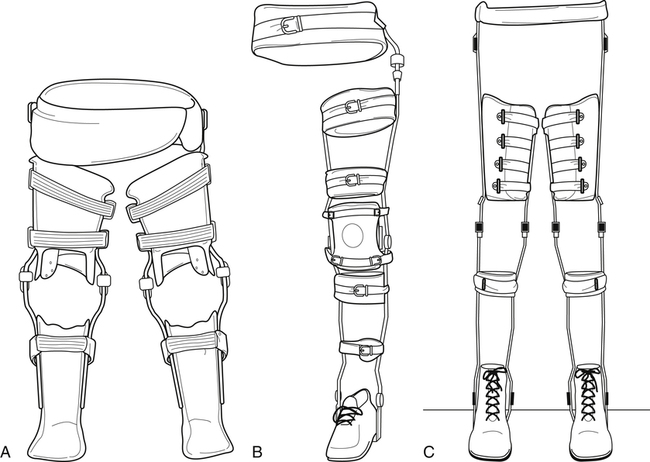
Hip orthoses
The realm of splinting for the hip joint encompasses immobilization during injury, presurgical and postsurgical intervention, and limited ROM control to meet rehabilitation protocols. When splinting for hip dislocations, subluxations, or postsurgical hip replacement, a hip spica abduction orthosis is often selected (Fig. 26-11). The hip orthosis provides hip stability and proper hip alignment, limits unwanted motion, and reduces stress on the hip. The hip orthosis is prefabricated and offers hip joint options to provide the best orthosis to meet individual rehabilitation protocols. Hip joints will have settings for flexion, extension, abduction, and adduction. The pelvic section and the thigh cuff section can be ordered individually for optimum fit. The interface is soft and can be removed for cleaning. Depending upon the need, there can be either one or two hip joint hinges and thigh cuffs attached to the pelvic section, making the orthosis adaptable for one or two leg spica supports.12
Certain neuromuscular disorders, especially cerebral palsy, are associated with pronounced instability and poor balance due to spastic hip adduction. This hip adduction creates a very narrow base of support when sitting and standing, causing crouched posture, genu valgum, foot pronation, and poor gait. One hip orthosis on the market today that may be helpful for these conditions is called the S.W.A.S.H. (Standing, Walking And Sitting Hip Orthosis) by Allard (Rockaway, NJ) (Fig. 26-12). This orthosis is designed for children with neuromuscular diagnoses, such as spastic hemiplegia, quadriplegia, low trunk tone, or cerebral palsy, or who have a risk of hip displacement. This orthosis should not be fit to patients with chronic hip dislocation or fixed hip flexion contracture greater than 20°. The S.W.A.S.H. is designed to reduce hip adduction, promote hip abduction, and allow for better control in gait and sitting. This product has been shown to reduce hip adduction and tone, improve hip alignment and ambulation, and create greater independence for patients over time. Maximum success can be achieved with ongoing therapy while wearing this device. S.W.A.S.H. also allows for greater interaction during play and rehabilitation since it frees the patient’s hands.1
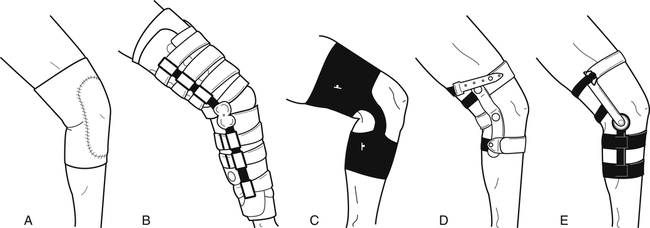
Knee orthoses
A hinged knee orthoses may be indicated when more significant knee pain or some mild instabilities are involved. A knee sprain or strain or possible meniscal tear is indicated for the fitting of a hinged knee brace. By adding the hinges to the knee orthosis, medial and lateral stability is gained; therefore the hinged splint provides more stability. Hinged knee orthosis may be neoprene with hinges, a single upright hinge with strapping for placement and support, or a more structured combined instability brace (Fig. 26-13). Combined instability orthoses are used for anterior cruciate ligament (ACL) tears, posterior cruciate ligament (PCL) tears, medial collateral ligament (MCL) tears, or meniscal tears. These orthoses are also fit for prophylactic needs for athletes to prevent ligament injuries or instabilities. Combined instability knee orthoses can be either prefabricated or custom-made depending upon the size and deformity of the knee. These braces provide protection against hyperextension and medial and lateral shifting.
Combination orthoses
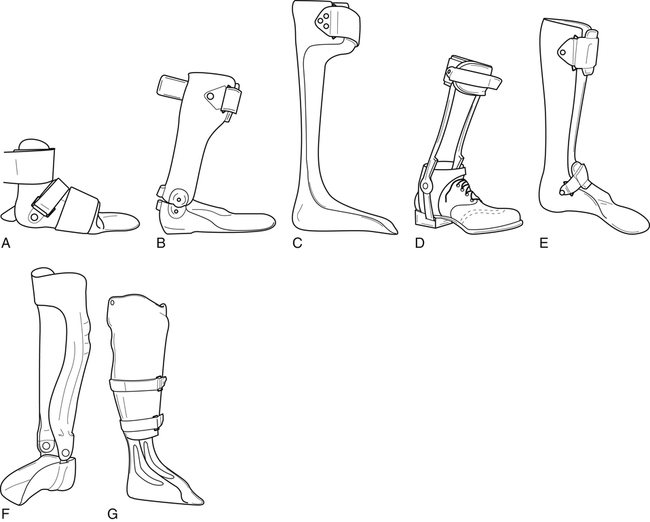
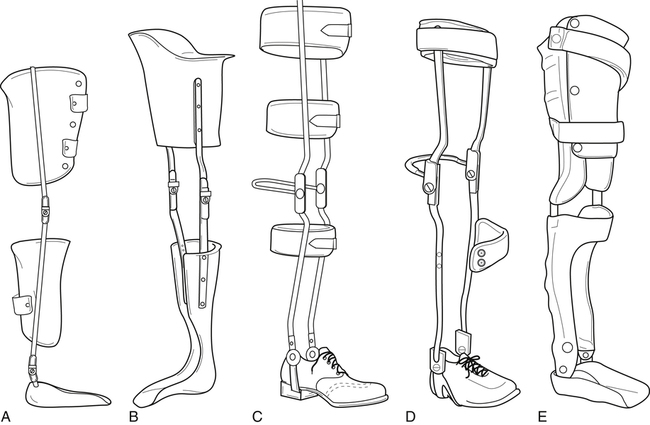
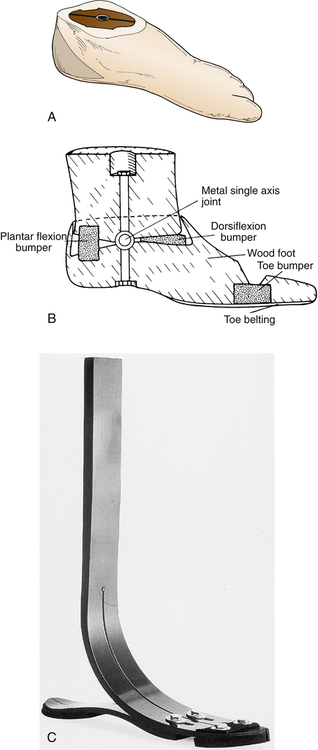
Ankle-foot orthoses
There are several types of AFO, including leaf spring, solid ankle, free ankle, and dorsi-assist (Fig. 26-14). These orthoses fall into two categories, static or dynamic, with both types consisting of either prefabricated or custom fabricated devices. AFOs can be classified either as static orthoses (prohibiting motion at the ankle) or dynamic orthoses (permitting ankle motion, primarily in the sagittal plane). The solid ankle AFO, the anterior floor reaction brace, and the patellar tendon-bearing (PTB) AFO are examples of static AFOs. Those in the dynamic group include posterior leaf spring and hinged-ankle (articulating) AFO designs.9 Dynamic AFOs are contraindicated in patients with severe edema, nonhealing diabetic ulcers, and severe foot deformity.
Knee-ankle-foot orthoses
Types of Knee-Ankle-Foot Orthoses
For the KAFO, there are options for different types of knee joints in order to accommodate varied levels of instabilities (Fig. 26-15). Locked knee joints hold the patient in full extension to prevent knee buckling during ambulation. The patient must use hip hiking or circumduction to progress the limb forward during ambulation, thus providing supported and secure ambulation. The use of drop locks enables the patient to release the locked position and allow knee flexion for sitting. The drop locks can be unlocked by simply grasping with the hands and pulling up until the joint is cleared, or by the use of a trigger release mechanism attached to the upper, lateral portion of the KAFO. If quadriceps strength is adequate, a free knee joint can be used to allow full ROM and a more natural gait for ambulation. This type KAFO will not lock during heel strike, and therefore will not protect against knee buckling. For patients with a disease such as OA or deformity, this type of orthosis provides adequate support for ambulation due to the patient having adequate quadriceps strength while still providing medial and lateral support.
The Free Walk KAFO by Otto Bock (Minneapolis, Minn.) helps achieve a more natural gait by locking during the stance phase and unlocking during the swing phase. The automatic lock is initiated by knee extension moment, and is only released to swing freely when a knee extension moment and dorsiflexion occur simultaneously in terminal stance. The KAFO joint requires the simultaneous extension moment and 10° of dorsiflexion to release the lock, making it safe for descents and ascents. The Free Walk has an open frame design that uses only one upright instead of two (Fig. 26-16, A). The upright is on the lateral side of the leg. The locking mechanism control cable is contained in the tubular stainless steel sidebar. The Free Walk is a custom fabricated orthosis, but the patient must be able to obtain a knee extension moment and dorsiflexion of ankle and foot to operate this device.7
Fillauer Company (Chattanooga, Tenn.) has designed a dynamic KAFO called the Swing Phase Lock (SPL). The SPL KAFO utilizes a simple internal pendulum mechanism to lock and unlock the knee depending upon the angle of the joint in the sagittal plane (Fig. 26-16, B). During the gait cycle, the knee joint will lock just before heel strike for support during stance and unlock the knee at heel off in preparation for swing phase. The SPL KAFO has three modes of operation controlled by a proximal remote push-button switch: automatic lock and unlock, manual unlock, and manual lock. These three modes allow the patient to select automatic lock for walking, unlock for sitting, or lock for standing. Candidate selections for this KAFO are patients with post-polio syndrome, spinal involvement, CVA, peripheral paresis or paralysis, nerve inflammations, neurological failures, myopathies, and MS or similar diseases. Contraindications are knee flexion contractures greater than 10°, central paralysis, hip flexion contractures, hip musculature involvement, poor balance/coordination, and knee hyperextension greater than 10°.7
Hip-knee-ankle-foot orthoses
The HKAFO is a hip-knee-ankle-foot orthosis that supports all of the joints that it crosses. There are different styles, materials, and componentry to choose from to design every orthosis specifically to each individual’s needs (Fig. 26-17). Some styles of HKAFO can be heavy and cumbersome simply because of the bulk of the orthosis and the number of anatomical joints that it crosses, creating a steep learning curve for the patient as well as the PT and PTA. Practicing the donning and doffing process, focusing rehabilitation sessions on upper body strength, ROM, and developing a successful gait pattern are a few of the hurdles that face the patient, PT, PTA, and family members and caregivers. In addition to the physical demands, the emotional stressors should also be addressed by setting clear, concise, attainable goals and ensuring that each individual has the patience needed to fulfill the physical therapy sessions and protocols. Indications are spina bifida, traumatic paraplegia, muscular dystrophy, and osteogenesis imperfecta. The patient must have plantigrade feet, knees should not have flexion contractures greater than 5° to 10°, hips should be free of contractures and flexible (not rigid or spastic), upper extremity strength should be good, the patient should be well motivated and have a supportive family, and goals and expectations should be realistic.
Contraindications are severe contractures, spasticity or other involuntary movements, obesity, and poor upper extremity strength. The reciprocating gait orthosis (RGO) provides excellent walking function and hands-free standing, and the use of the orthosis helps to stretch the hip flexors to prevent contractures. With every step, as one leg flexes, the other leg must extend and thus stretch the hip flexors. The age one can be fitted with the isocentric RGO is as young as 17 months, giving them a better chance for walking and standing and therefore enjoying earlier the physiologic, skeletal, and psychological benefits of being upright. In order to ambulate, the patient must be able to use forearm crutches to provide upper body support. A tripod gait is often used when covering a greater distance is required, such as when outdoors. When using the isocentric RGO inside one’s house or indoors, the patient can use a normal ambulation pattern with their crutches. The RGO is a custom-made device in which measurements and a cast of the torso and hip portion of the patient is required. There are two styles available. One is an open design in which the wearer will don the device by slipping into the open posterior side. It fits over all clothing including shoes. The second will fit more intimately to the patient and the ankle-foot portion will fit into a shoe.6
Prostheses
 Evaluation to determine the type of prosthesis to be fabricated based upon activity level, strength, amputation site, personal goals set, and, of course, insurance guidelines
Evaluation to determine the type of prosthesis to be fabricated based upon activity level, strength, amputation site, personal goals set, and, of course, insurance guidelines
 Casting or scanning of the patient’s affected body area; manufacture of a check socket to assess fit
Casting or scanning of the patient’s affected body area; manufacture of a check socket to assess fit
 Fabrication of the permanent socket and assembly of the prosthesis
Fabrication of the permanent socket and assembly of the prosthesis
 Fitting of the prosthesis, and delivery of all necessary componentry and accessories
Fitting of the prosthesis, and delivery of all necessary componentry and accessories
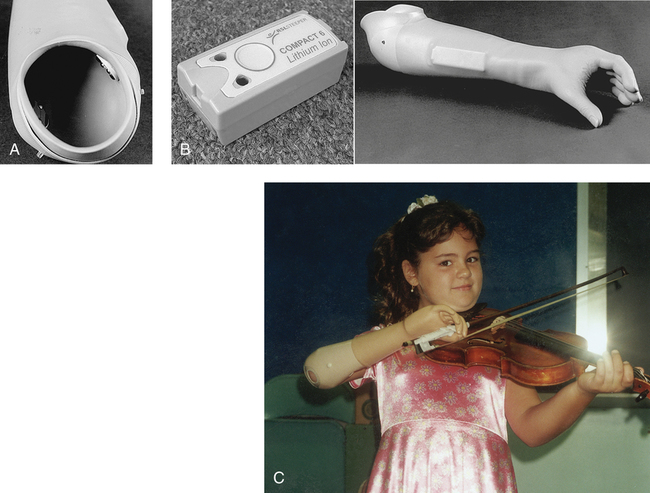
Reasons for Amputations
There are numerous reasons for amputations, including traumatic injury, cancer, infections, and diabetes. Many amputees are born with congenital deformities in which the limb did not develop, or the limb deformity is so great that it must be amputated. The younger the amputee, the better the outcome for most cases because there is a longer period of time available to learn coping skills, compensation techniques, and ways to adapt physically to their environment. The younger the amputee, the greater the likelihood that they will have higher levels of flexibility, strength, and balance, and have marked improvements at a faster rate. For the congenital amputee, whether upper or lower extremity, they will learn many ways to compensate for the absence of the limb, thus becoming very efficient in ambulation or tasks that require upper extremity involvement and dexterity. The psychological involvement can also be lessened for the congenital or very young amputee for issues such as self image if the family maintains a positive attitude. Experts in the pediatric prosthetics field believe that as long as the parents, extended family, and support team maintain a positive attitude toward the missing limb or deficiency whether acquired or congenital, then the child will also have a positive attitude and outlook on life. If the parents do not handle the limb deficiency well, it is likely that the child will also not cope well with the limb loss. When the patient or family begins to have difficulty coping with the limb loss, then referring them to a psychologist, a peer group, or both becomes essential. The earlier the intervention and support for the family and the child, the better the outcome.4
In a recent study done by National Limb Loss Information Center, revised in 2008, there are approximately 1.7 million people living in the United States with limb loss.10 An average of one out of every 200 people in the United States has had an amputation. Table 26-4 lists the possible causes for amputation.
Table 26-4
| Cause | Rationale |
| Dysvascular-related amputations | Problems associated with the blood vessels: 38.30 per 100,000 in 1988 increased to 46.19 per 100,000 in 1996 Lower-limb amputations: 97% In all age groups, the highest risks were for males and African-Americans |
| Trauma-related amputations | Upper extremity accounts for 68.6% Males were at slightly higher risk For both males and females, risk of traumatic amputation increased steadily with age, reaching its highest level among people aged 85 years and older |
| Cancer-related amputations | Most common occurrence in the lower limb accounting for 36% No notable differences found between sexes and races, and lower occurrence rate found in African-Americans |
| Congenital-related incidences | Rates for newborns were 26 per 100,000 live births, relatively unchanged over the study period Upper limb accounted for 58.5% |
From National Limb Loss Information Center. Amputation Statistics by Cause: Limb Loss in the United States. Published by the National Limb Loss Information Center. Available online: http://www.amputee-coalition.org/fact_sheets/limbloss_us.html.
Suspension Methods
Locking pins
Many prostheses, whether upper or lower extremity, are suspended by the use of a liner with a locking pin. The pin is located on the distal end of the liner and slips into a locking mechanism that is housed within the distal end of the socket (Fig. 26-18). A liner is a means of interface that lies between the skin and the socket. Liners are made of silicone, polypropylene, elastomer gels, or urethane blends. The liners act as a cushion for shock absorbency, prevent abrasions, and protect against shearing forces and skin breakdown of the residual limb. This type of suspension provides a secure attachment, and because of the visual and audible cues made as the pin engages into the lock, this type of suspension provides a factor of emotional security that the prosthesis is donned correctly. There is a release button to press that will disengage the lock and allow the prosthesis to be removed.
The Alpha Liner, for example, is composed of a unique, mineral oil–based, thermoplastic, elastomer gel with durable fabric covering that makes the liner last longer. The mineral oil within the liner seeps into the skin, creating a skin friendly environment. This gel liner also conforms to the shape of the residual limb providing a custom fit. The Alpha Liner is available in prefabricated and custom-made variations for pediatric, transfemoral, transtibial, and upper extremity amputees. Liners are also available without the distal umbrella for pin attachment and provide an interface between the socket and the limb.11
Suction/vacuum suspension
Suction is also a viable and desirable way to suspend a prosthesis. Suction creates an airtight socket through the use of an expulsion valve. At the distal end of the prosthesis there is a valve that the wearer pulls a thin sock through, which pulls the residual limb completely into the socket, and then the valve cap is placed back into the opening to create a closed environment (Fig. 26-19). The top cap of the valve uses an expulsion valve that the amputee can press to release air that may get trapped inside the socket to regain optimal fit.
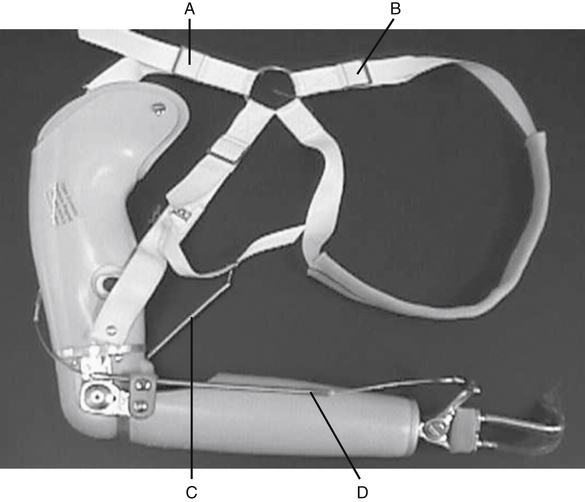
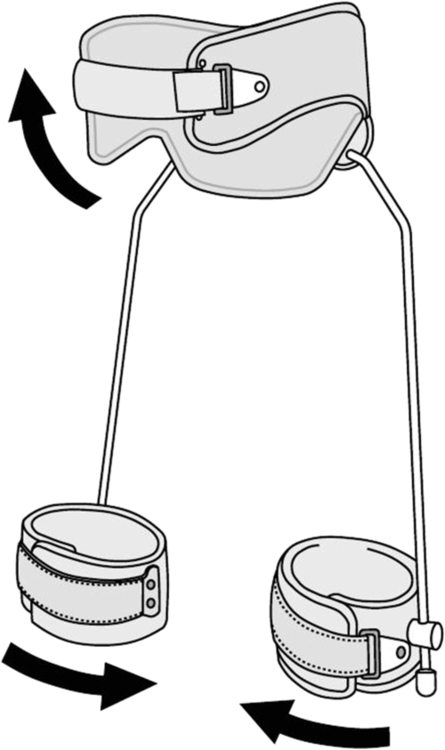
Harnesses
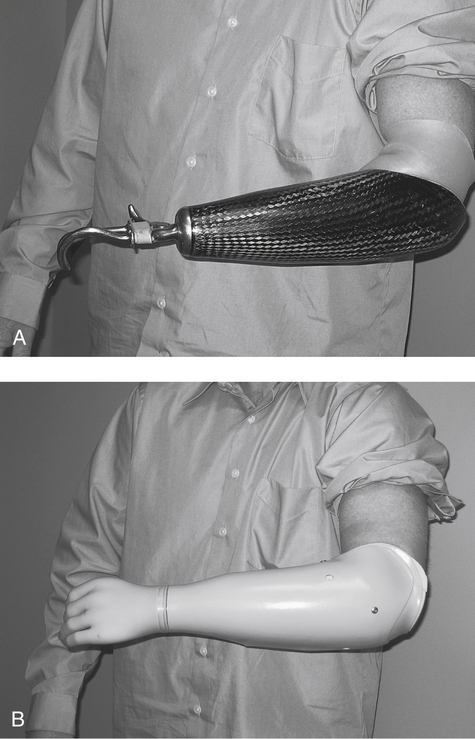
For upper extremity prostheses, the use of a harness for suspension is widely used. The harness not only suspends the prosthesis, but also acts as a mechanism for control of the terminal device (TD) or hand for opening and closing the hand for grip (Fig. 26-20). The hand can be one of several types of hooks or a hand that has more cosmesis and looks like a real hand. By elevating or depressing the shoulder or scapular manipulations, the cables that connect to the hand are tightened, and this tension on the cable opens the hand. The harness will also operate the elbow unit for the transhumeral amputee. There are separate cables, controls, and body movements necessary to lock and unlock the elbow joint.
There are many designs for harnesses. The style desired is the most simple that will provide the amputee with the ability to control the TD. Harnessing uses the body’s movements and transmits them to the cable portion of the harness and causes movement of the TD. The movements necessary for TD control are glenohumeral forward flexion, biscapular abduction, shoulder depression and elevation and chest expansion. Depending upon the level of amputation and the amputee’s strength and ROM, the correct harness can be chosen. Different motions can be used to control the TD or the elbow joint. Each movement must be mastered to efficiently use the prosthesis.16
There are advantages and disadvantages to using a harness. These can be found in Box 26-1.
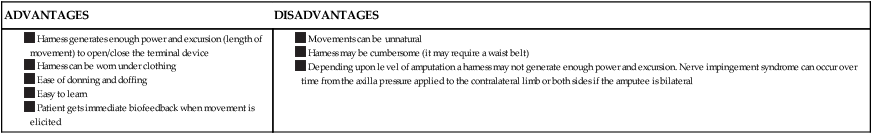
Data from Uellendahl JE, Uellendahl EN: Body-powered upper-limb, prosthetic designs. In Carroll K, Edelstein JE, editors: Prosthetics and patient management: a comprehensive clinical approach, Thorofare, N.J., 2006, Slack.
Upper Extremity Prostheses
Prosthetic elbows
Body powered elbow components are controlled by friction or locking positions. The elbows with locking positions have as many as 11 positions in which to place the elbow and can also assist in lifting. The units that are friction controlled can be manually placed in desired flexion or extension. The elbows are available in adult or pediatric sizes (Fig. 26-21).
Myoelectric elbow units are also a consideration to make. One such type is the DynamicArm, a myoelectric prosthetic elbow unit by Otto Bock. This unit lifts loads up to 13 pounds and offers a feature called Automated Forearm Balance (AFB). AFB stores energy when the arm is extended and reuses it for flexion, which results in a smooth, natural swing during walking. The DynamicArm unlocks easily, even when under load. It can be positioned without having to send an unlocking signal, which enables the user to make fewer compensatory movements while providing a more natural appearance.14
Prosthetic hands
There are two main types of TDs or hands offered: hooks and hands (Fig. 26-22). They can both be either body powered, where the hand is controlled by a cable system through a harness, or myoelectrically powered, where the hand is controlled by muscle stimulus received by sensors placed within the socket.
Lower Extremity Prostheses
Componentry selection guidelines
When selecting the appropriate foot or knee for each patient, there are set medical guidelines for levels of ambulation to direct the prosthetist’s choice. Depending upon the activity and ambulation abilities or potential of each amputee, the Medicare chart found in Box 26-2 can be adhered to when selecting the foot or knee for each prosthesis. Careful consideration and evaluation for this potential to regain ambulatory ability is a crucial step in determining appropriate componentry. The PTA in conjunction with the prosthetist can make optimal decisions as a team and create better outcomes for the patient.
An additional tool that can be used when evaluating the activity level of the amputee is the Amputee Mobility Predictor Questionnaire and the Amputee Mobility Predictor (AMP) Testing Methodology.8 These evaluation tools where developed by Robert Gailey, PhD, PT, and are widely used in the clinical setting to determine the functional level of each amputee. By gathering qualitative data, the PT, PTA, and the prosthetist can have shared data to use while collaborating on treatment plans for shared patients.
Prosthetic knees
Types of knees
Current technology has added some very important control features that have not been offered until the past few years. The use of computerized componentry to control swing and stance phase has provided transfemoral amputees with a new type of freedom. The C-Leg, Rheo Knee, Plié MPC Knee, and Smart Adaptive are all examples of microprocessor (MPC) knee components (Fig. 26-23). Each knee works on a slightly different mechanism of gait, but this freedom of cadence change without the fear of falling and less use of mental focus required by traditional knee units provides huge gains for the transfemoral amputees.13
Summary
This introduction to orthotics and prosthetics has provided a brief overview of products and indications for use of the orthotic or prosthetic componentry. There are many considerations involved with each patient, and familiarizing oneself can be time consuming and ongoing throughout one’s career. When fitting an orthosis, the main concerns are finding a proper fit, not compromising the patient’s function, using as little orthotic support as required, and supporting only the joint or joints that are deficient in strength or ROM or have deformity. Prosthetic componentry for lower extremity amputees should be selected based upon the patient’s ability to ambulate using the Activity Guidelines chart to gauge the selection process (see Box 26-2). For upper extremity amputees, the choice can be decided based upon ability to operate the TD, the patient’s AROM, and strength. Preprosthetic therapy is beginning to be discussed in the medical field among professionals. According to the American Geriatrics Society (AGS), which is composed of more than 6800 health care professionals who are focused on the issues of the aging, more than 75% of all amputations are performed on persons older than 65 years. Approximately 90% of those involved are lower limb, and approximately two thirds of lower-limb amputations are transtibial. More than 65% of all amputations performed on people age 50 years and older are due to diabetes or peripheral vascular disease (PVD), according to the Amputee Coalition of America (ACA). What can help the patient to have a satisfying quality of life and achieve their functional goals after amputation? “Approximately 75 percent of older adults can regain their ability to walk with or without assistive devices if they undergo the proper rehabilitation program before and after they receive…a prosthesis.”8 The physical therapy program should address the patient’s strength, stamina, flexibility, and improved heart and lung function in order to be optimally prepared before the amputation surgery. Wearing a prosthesis for ambulation requires an increased level of energy consumption of about 60%. Providing a team approach to each patient, including a PT, physician, physiatrist, counselor, and a prosthetist, enables the patient to be better prepared mentally and physically and more educated about the process and the answer to the question of exactly what is a prosthesis.5
GLOSSARY
Brace A term, now mostly used outside of a clinical setting, referring to a splint.
Componentry The parts of a prosthesis.
Doff The removal of a residual limb.