Introduction to Pelvic
Anatomy 2
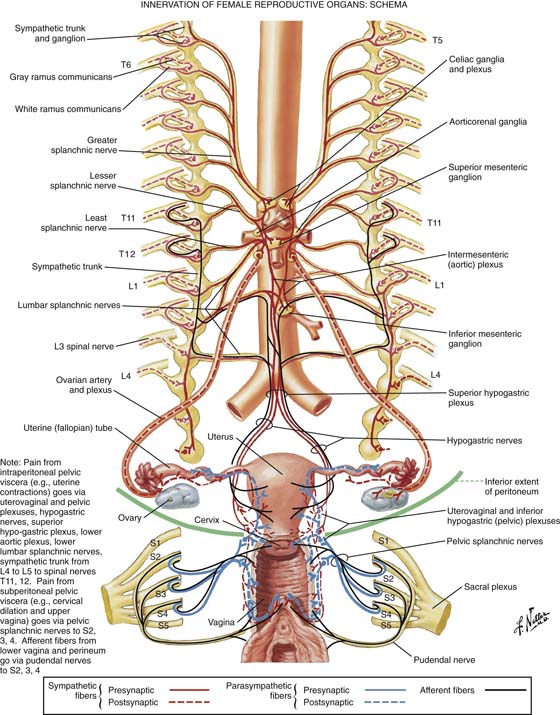
Autonomic Nervous System
The motor innervation of the intestines, ureter, urinary bladder, uterus, and adnexa is derived from the autonomic nervous system (Fig. 2–1).
The latter system in turn is divided into sympathetic and parasympathetic components.
The sympathetic cells are located within the lower thoracic and lumbar segments of the spinal cord; the parasympathetic cells are located in the sacral portion of the spinal cord. In general, the two systems work in opposition to each other (dual intervention) to maintain homeostasis. For example, the smooth muscles of the bronchioles relax under sympathetic mediation and constrict under parasympathetic stimulation.
Two types of cholinergic receptors are known: nicotinic, which are found on the postganglionic cells (postsynaptic) of both sympathetic and parasympathetic effectors, and muscarinic, which are found only in the parasympathetic portion of the autonomic nervous system.
Adrenergic receptors for norepinephrine and epinephrine are divided into α and β and into further subtypes, which demonstrate sundry agonist and antagonist activities. For example, β one (β1) receptors are present in cardiac muscle, and β two (β2) receptors are present in the coronary arterioles.
Fibers that emanate from the central nervous system are designated as preganglionic. In the case of sympathetic preganglionic fibers, synapses occur in paravertebral and prevertebral ganglia, where acetylcholine is the transmitter. Parasympathetic fibers synapse near or within the effector organ, with acetylcholine as the neurotransmitter. Postganglionic sympathetic fibers travel from the ganglion to the effector (e.g., a blood vessel in which norepinephrine is the neurotransmitter). Parasympathetic postganglionic fibers are short and acetylcholine is the neurotransmitter at the postganglionic synapse. Additionally, peptide neuromodulators such as enkephalin and somatostatin are simultaneously released with acetylcholine or norepinephrine.
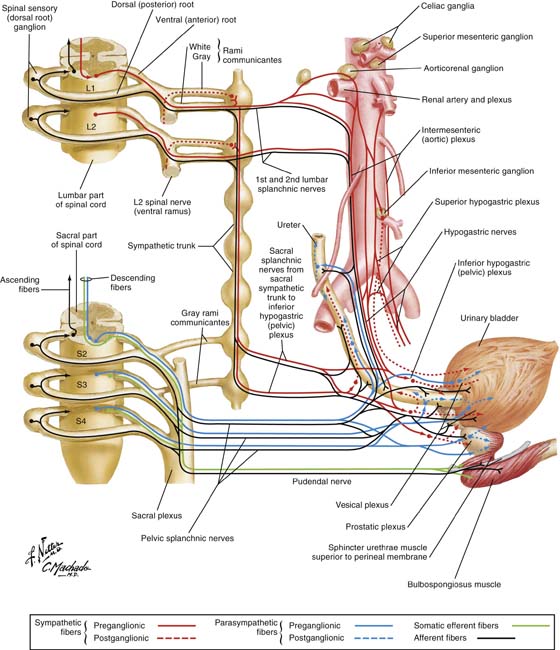
Figure 2–2 details three groups of nerves supplying the autonomic input for female reproductive structures. One group originates from the 9th through the 12th thoracic cord segments, with preganglionic sympathetic fibers synapsing in the celiac and superior mesenteric ganglia, and postganglionic fibers following the ovarian vessels to synapse in the ovary and uterine tubes (oviducts). Afferent sensory fibers follow the same route in reverse. The second group, which is derived from T12, L1, and L2 segments, supplies the oviducts and the great pelvic vessels and enters the pelvis via the superior hypogastric plexus. The third group emanates from L2–L5 segments and synapses within the inferior mesenteric plexus and/or transmits via the inferior hypogastric plexus to the uterine and vagina plexuses. Postganglionic fibers in turn synapse in the uterine body, cervix, vagina, and erectile structures within the vulva.
Parasympathetic preganglionic fibers arising from the sacral nerve roots follow the branches of the hypogastric vessels and synapse in the uterovaginal plexus.
As previously noted, the hypogastric plexus (nerves) descends into the pelvis over (anterior to) the aorta and the left common iliac vein, entering the presacral space.
The inferior hypogastric plexus descends deep into the pelvis of the periosteum of the sacrum, where it is dispersed with remnants of the uterosacral ligaments and fat and numerous small blood vessels at a 3 : 1 ratio of venules to arterioles.
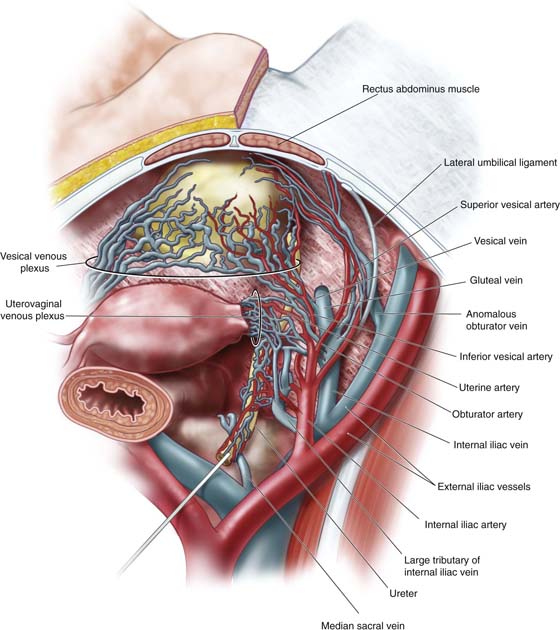
The bladder and the lower ureters are innervated via the pelvic plexuses by the autonomic nervous system (Fig. 2–3). Sympathetic nerves emanate from T10, T11, T12, L1, and L2.
Spinal cord segments and somatic motor neurons controlling perivesical muscle and parasympathetic preganglionic neurons are located in S2, S3, and S4 segments.
Sensory impulses (visceral sensory) return to the spinal cord via similar pathways, transmitting via parasympathetic pathways and sacral cord segments. The latter transmit pain and proprioception (e.g., distention). Some sensory fibers from the trigone and the urethrovesical junction transmit pain via the pudendal nerves. Clearly, some sensory afferents reach the spinal cord via the hypogastric nerve plexus.
Parasympathetic postganglionic fibers synapse within the bladder’s detrusor muscle and exit via the postsynaptic muscarinic receptors, resulting in muscle contraction.
Contemporary neuroanatomy data suggest a sparse number of sympathetic nerves in the bladder musculature, with the exception of the trigone, where greater numbers of sympathetic versus parasympathetic nerves are found.
During the filling phase, bladder volume increases while parasympathetic output is inhibited. At the same time, α sympathetic discharge causes the urethral muscle to contract, thereby retaining a high-pressure gradient that favors the urethra over the bladder. When the level of fullness transmits, via afferent sensors and fibers, a feeling of discomfort (associated with high bladder volume), the brain in turn dispatches a release message, which triggers a parasympathetic discharge. The bladder muscle contracts and empties. Concurrently, sympathetic synapses in parasympathetic ganglia modulate ganglionic transmission, resulting in urethral muscle relaxation (by blocking contraction). The pressure gradient shifts in such a way that bladder pressure exceeds urethral pressure, thereby allowing micturition.
Sympathetic and parasympathetic fibers supplying the large and small intestines emanate from the celiac, superior and inferior mesenteric, and hypogastric plexuses (Fig. 2–4). Preganglionic parasympathetic fibers likewise originate in medullary nuclei (e.g., the medulla oblongata) of the vagus nerve and sacral cord segments. Vagally derived fibers supply the duodenum, jejunum, and ileum. Sympathetic preganglionic fibers are distributed from cord nuclei located at T8, T9, T10, T11, and T12, and at L1, L2, and L3; the latter relay within the ganglia of the sympathetic trunks and from there to plexuses, where synapses occur and postganglionic fibers distribute themselves to the intestines. Afferent and efferent somatic fibers, via the pudendal nerves, innervate voluntary (striated) muscles such as the levator ani and external sphincter ani. Because they are pelvic structures, innervation of the sigmoid colon, rectum, and anus is of special interest to gynecologists and obstetricians.
FIGURE 2–1 Details of the autonomic nervous system. Sympathetic efferents are red, and parasympathetics (vagal and sacral) are blue. The autonomic nervous system, totally consisting of motor (efferent) somatic nerves that control voluntary muscle activity, is shown in green; sensory (afferent) organs and muscles are black and may share pathways with autonomic and somatic nerves. (By permission, Netter’s Atlas of Human Anatomy.)
FIGURE 2–2 The autonomic nerve supply to the female reproductive organs is shown here. Preganglionic fibers are shown as solid red (sympathetic) blue (parasympathetic) lines. Somatic (afferent) sensory nerves are shown as solid black lines. Sympathetic nerves arise from the lower thoracic and lumbar cord segments and synapse in outlying ganglia on the aorta or its main branches. Others enter the pelvis via the hypogastric nerves (plexuses). Postganglionic fibers travel along the ovarian vessels or the uterovaginal vessels. Parasympathetic input arises in the sacral cord and travels via pelvic splanchnic nerves to the various organs where synapses occur and short postganglionic fibers transmit impulses. (By permission, Netter’s Atlas of Human Anatomy.)
FIGURE 2–3 The bladder and the lower ureter are innervated via pelvic plexuses. Sympathetic fibers emanate from cord segments T10, T11, T12, L1, and L2. Parasympathetic preganglionic neurons are located in S2, S3, and S4 cord segments. Postganglionic parasympathetic neurons lie within the walls of the bladder and the ureter, whereas preganglionic sympathetic fibers are found in the vesical plexus (pelvic plexus). (By permission, Netter’s Atlas of Human Anatomy.)
FIGURE 2–4 Large and small intestines are supplied with autonomic input via celiac, superior mesenteric, and inferior mesenteric plexuses, the vagus, and sacral nerves. The pelvic portion of the sigmoid colon, rectum, and anus receives sympathetic fibers via the superior and inferior hypogastric plexuses. The inferior hypogastric plexus receives parasympathetic fibers from S2, S3, and S4 nerve roots. The rectal plexus (pelvic plexus) is closely applied to the rectal connective tissue and carries sympathetic, parasympathetic, and afferent nerves. The pudendal nerve carries somatic efferent fibers to the levator ani and the external sphincter ani. (By permission, Netter’s Atlas of Human Anatomy.)
Pelvic Plexus
The inferior mesenteric plexus receives fibers from the superior mesenteric plexus via the lumbar splanchnic nerves. Branches from the inferior mesenteric plexus accompany arteries to respective intestinal segments (e.g., left colon, upper sigmoid colon). The superior hypogastric plexus carries sympathetic preganglionic nerves and afferent nerves, which lie on either side of the rectosigmoid and rectum and become the inferior hypogastric plexus (presacral) (Fig. 2–5). This plexus receives parasympathetic preganglionic nerves, as well as somatic branches, from S2, S3, and S4 nerve roots via pelvic splanchnic nerves. The rectal plexus is a subdivision of the inferior hypogastric plexus and carries sympathetic preganglionic fibers, afferent sensory fibers, and parasympathetic preganglionic fibers. The inferior hemorrhoidal branches of the pudendal nerves receive sensory impulses from anal receptors located in the mucosa and the submucosa, especially in the anal valves. They transmit impulses via somatic efferents located in the sacral cord. The internal anal sphincter is supplied by sympathetic nerves originating in the L5 cord segment. The external anal sphincter is innervated by somatic efferent fibers via the inferior hemorrhoidal nerves and perianal branches (S4).
Sigmoid Colon
The anatomic relationships of the sigmoid colon and the rectum to other pelvic viscera are critically important to the gynecologist. Figure 2–6 shows the entire sigmoid colon and its S configuration as it descends into the depths of the pelvis. Note that the sigmoid colon drapes over the left adnexa, virtually covering the tube and the ovary. The lower sigmoid colon then may be located at least partially posterior to the ovary and broad ligament. The entire sigmoid colon is attached to a mesentery and therefore is an intraperitoneal structure. Within the hollow of the sacrum, the sigmoid colon joins to the short straight rectum. The rectum becomes progressively extraperitoneal as it descends even deeper into the pelvis. The relationships to the draped-over sigmoid are anterior to the bladder and to the broad ligament as well as the anterior abdominal wall. The sigmoid colon is in contact with the posterior aspect of the uterine corpus, and the posterior leaf of the broad ligament at the midpelvis. The rectum and the rectosigmoid lie medial to the uterosacral ligaments. The rectum is directly posterior to the cervix where that structure connects to the uterosacral ligaments and to the posterior vaginal fornix. The rectum in fact is intimately close to the vagina and is susceptible to damage during hysterectomy (Fig. 2–7). Posterior to the rectum and the rectosigmoid are the middle sacral vessels and a large number of veins and venous sinuses.
The sigmoid mesentery receives branches of the inferior mesenteric vessels and crosses superficially over the left iliac vessels and the left ureter.
Venous drainage is frequently overlooked in anatomic drawings of the female pelvis. This is rather strange in that most bleeding encountered during surgical operations is venous in origin. Figure 2–8 details the relationship between the levator ani muscles and the anal sphincters. Venous drainage of the rectum and anus is detailed. Note the collateral circulation that exists between the inferior mesenteric vein (portal system) via the superior rectal vein and the internal iliac veins (systemic system) via the middle rectal and inferior rectal veins. Note the connectors between the internal pudendal veins via the inferior rectal veins and the middle rectal veins to the internal iliac veins.
The rectal plexus of the veins surrounds the rectum. Veins lie internal (submucosal) and external to the muscularis. Note the longitudinal pattern and the numerous venous sinuses.
Figure 2–9 shows a unique exposure that demonstrates critical muscular relationships between the levator ani and the anal sphincter in terms of topographic and deeper anatomy.
Bladder and Pelvic Supports
The bladder neck (i.e., the urethrovesical junction) is located posteriorly to the lower margin of the pubic symphysis. Thus it is difficult to access and see under most circumstances. Most surgeons do not consider the extensive venous network of veins and sinuses surrounding the perivesical tissues, as well as the bladder wall and terminal ureter (Fig. 2–10). The support of the bladder neck can be readily seen in the anatomy laboratory by sawing through symphysis and tilting it forward. The posterior pubourethral ligaments can be seen to be the principle structures that anchor the urethra to the pubic bone (Fig. 2–11). The anterior pubourethral ligaments are less prominent but attach the urethra as it emerges under the symphysis to the anteroposterior margin of the symphysis pubis. The posterior aspect and bladder base are in close contact to the lower uterine corpus (anterior surface of the uterus) and are, in fact, attached to the cervix and vagina by the bladder pillars or vesicocervical and vesicovaginal pillars. These structures and their relationships are shown in Figure 2–12.
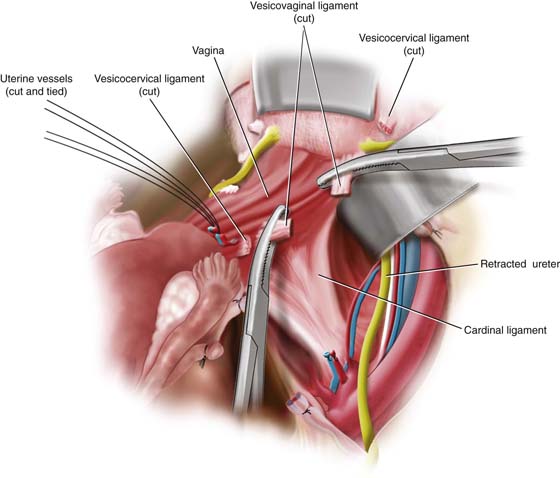
The urinary bladder, cervix, and vagina share common supporting structures (Fig. 2–12). Critical relationships exist between the distal ureter and branches of the anterior division of the hypogastric vessels, together with cardinal ligaments and bladder pillars (Fig. 2–13). The deeper portions of the cardinal ligaments are attached to the bladder base and the upper anterolateral vagina. The terminal ureter just cranial to entry into the bladder wall is intimately in contact with the vesicocervical and vesicovaginal ligaments (Fig. 2–14). To free the ureter from the cardinal ligament and vagina, the bladder pillars (vesicocervical and vesicovaginal ligaments) must be safely divided and ligated (Fig. 2–15). The most substantial supporting structures for the bladder base and the upper vagina are deep parametrial structures (deep cardinal ligaments). These substantial structures consist of fat, connective tissue (fibrous), and vascular channels. When these are severed, the bladder and the vagina may be more or less totally mobilized.
The only remaining support consists of common fibromuscular walls shared between the bladder, vagina, and rectum (Fig. 2–16).
A not-uncommon location for ureteral injury is the ureterovesical junction, which is intrinsically within the substance of the bladder. The course of the ureter within the bladder itself is oblique. This oblique course creates constriction and closure of the terminal ureter when the bladder contracts and empties. The ureteral closure aspect of bladder anatomy is important in that it prevents reflux of urine retrograde into the ureters when bladder pressure rises (e.g., during a detrusor contraction) (Fig. 2–17).
FIGURE 2–5 Sagittal view of the hypogastric nerve plexus, which spawns several regional plexuses. The superior hypogastric plexus overlies the fifth lumbar and first sacral vertebrae. The plexus descends into the pelvis to the right or left side of the rectum. Sympathetic and parasympathetic nerves travel within the hypogastric plexus and the rectal plexus, both of which supply autonomic input to the rectum. These structures likewise supply the uterus (uterine plexus) and the bladder (vesical plexus). Sensory inferior afferent fibers traverse the same plexuses. Anal sensation is transmitted via the inferior rectal branch of the pudendal nerve. Motor innervation to the external sphincter ani and the levator ani is supplied by the pudendal nerve and its rectal branches.
FIGURE 2–6 The relationship of the sigmoid colon and the rectum to the reproductive organs is shown here. The sigmoid colon drapes over the left adnexa and rotates from left to right and then back to the midline, where it joins the rectum posterior to the cervix and the vagina; between the posterior vaginal fornix and the closely applied rectosigmoid is the pouch of Douglas. The mesentery of the sigmoid colon is best seen on the medial aspect of the colon and is attached to the posterior peritoneum covering the lumbar and sacral vertebrae.
FIGURE 2–7 The relationships of the sigmoid colon and the rectum from the perspective of a sagittal cut. This picture shows the extent of peritoneum covering relative to the sigmoid colon and rectum, as well as a cut-away depiction of the large bowel wall from mucosa to serosa. The course of the anus relative to the rectum and vagina is accurately depicted, including the positions of external and internal anal sphincters. Note the position of the rectovaginal septum, which is defined more cranially than caudally. The septum consists of shared components of the anterior rectal wall and the posterior vaginal wall. A similar relationship exists between the anterior vaginal wall and the posterior wall of the bladder and urethra.
FIGURE 2–8 Venous drainage of the rectum is shown here. The arterial supply follows similar pathways but is more discrete. Within the muscularis and submucosa of the bowel wall are numerous anastomosing venules and sinuses. When cut or traumatized, these do not retract, as do arteries. Therefore, bleeding from the venous side may be relentless and difficult to stop. Two major systems drain rectal and perirectal tissues. The superior rectal venous system drains into the inferior mesenteric vein (portal system). The middle rectal vein drains into the internal iliac vein (systemic system), and the inferior rectal vein drains into the internal pudendal vein.
Increasing venous pressures that develop during pregnancy may lead to venous distention and stasis of outflow. Subsequent damage to the valves within the middle and inferior rectal veins by obstruction and congestion can lead to the development of internal and external hemorrhoids.
FIGURE 2–9 The topographic and deep anatomy of the perineum and the anal sphincter complex. Note the intermingling of the levator ani with the external sphincter ani. The levator ani plays a significant role in the mechanism of anal continence. When the sphincter ani muscle is injured, the levator ani may maintain continence (e.g., squeeze pressure). The levator action may be felt by the gynecologist during rectovaginal examination by having the patient contract her anal sphincter (and levator ani muscle).
FIGURE 2–10 Blood supply to the urinary bladder is plentiful and emanates from several sources. Venous return may consist of a number of variable plexuses, which ultimately drain into the internal iliac vein. Extensive bleeding may be encountered as the result of disruption of these numerous venous channels during dissection of the perivesical space and paravaginal tissues. This figure shows the vasculature within the cardinal ligament after the round and broad ligaments have been removed. Note that the superior and inferior vesical arteries come off the anterior division of the hypogastric artery, as well as the lateral umbilical and uterine arteries, respectively. An anomalous obturator vein is shown. Venous drainage even for large vessels, including major internal iliac tributaries, may be anomalous. As shown in this drawing, two large internal iliac veins join with a single external iliac vein to form a short right common iliac vein.
FIGURE 2–11 The pubourethral (puboprostatic) ligaments extend from the proximal urethra to the posteroinferior and anteroinferior surfaces of the symphysis pubis. Note that the pubourethral ligament is a direct continuum of the arcus tendineus.
FIGURE 2–12 The bladder dome has been cut away, allowing viewers to peer into the depths of the bladder. The trigone is visible. The uterine corpus has also been removed, as in the case of the supracervical hysterectomy. The sigmoid colon and rectum are intact. Note the relationships of the bladder pillars to the cervix, vagina, and ureters.
FIGURE 2–13 The central portion of the urinary bladder is retracted following incision of the vesicouterine peritoneal fold separation of the bladder from the cervix and vagina. Peripherally, the bladder remains attached to the cervix and vagina by the bladder pillars. Relationships of the vesical, uterine, and obturator vessels are seen here. The dotted line indicates where the vesicocervical ligament will be transsected.
Note that the ureter passes deep to the vesicocervical ligament (the anterior bladder pillar).
FIGURE 2–14 The uterine vessels have been divided. The anterior bladder pillar (vesicocervical ligament) has been doubly clamped with tonsil clamps and has been divided. This fully exposes the ureter at the ureterovesical junction.
FIGURE 2–15 The vesicovaginal ligament has been clamped and cut, which permits mobilization of the bladder and ureters. The upper vagina and the bladder base are held in place by the deep parametrium (deep cardinal ligaments) only.
FIGURE 2–16 The upper vagina has been exposed and a portion of the anterior wall excised. The bladder dome has also been excised. The right cardinal ligament and a portion of the deep parametrium on the right have also been severed. Note that the deep parametrial attachment to the bladder base remains intact. This drawing illustrates the fibrofatty composition of these endopelvic “ligaments.”
FIGURE 2–17 The anterior portion of the bladder has been cut away to reveal the trigone and the full posterior wall, as well as the posterior wall of the urethra. The trigone and the intravesical course of the ureter can be seen (dotted lines).
The upper right figure shows the bladder wall contracting and the intravesical ureter closing off. This picture is a frontal view.