11 Intraoperative Echocardiography for Heart and Lung Transplantation
Background
Heart Transplant: Donor Echocardiography
Overview of Echocardiographic Approach
Anatomic Imaging and Physiologic Data: Acquisition, Analysis, and Pitfalls
Heart Transplant: Recipient Echocardiography
Background
Overview of the Echocardiographic Approach
Anatomic Imaging and Physiologic Data: Acquisition, Analysis, and Pitfalls
Before Cardiopulmonary Bypass
Weaning from Cardiopulmonary Bypass and after Cardiopulmonary Bypass
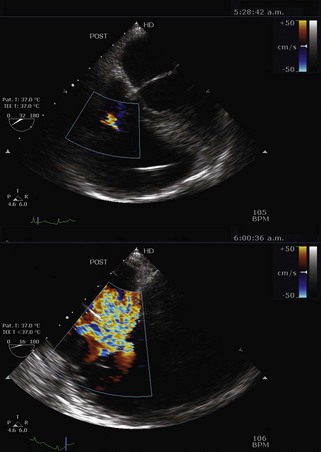
Step 1: Assess for Deairing
Step 2: Assess Left Ventricular Function
Step 3: Assess Right Ventricular Function
Box 11-1 Potential Etiologies of Right Ventricular Impairment during Separation from Cardiopulmonary Bypass and the Early Post-Cardiopulmonary Bypass Period in Heart Transplant Patients
Step 4: Assess Valvular Function
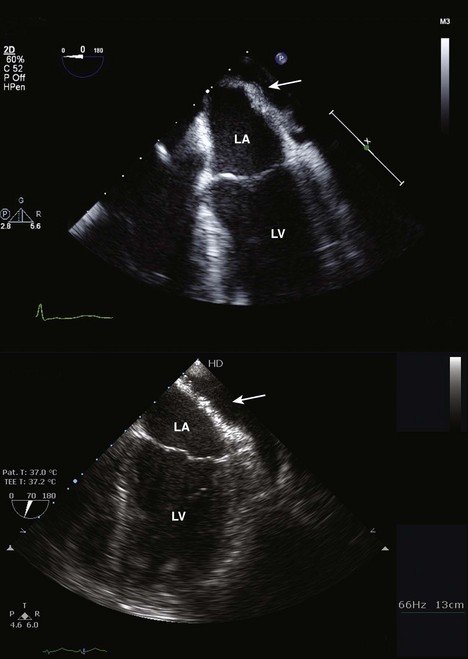
Step 5: Assess the Atria
Step 6: Assess the Caval Anastomoses
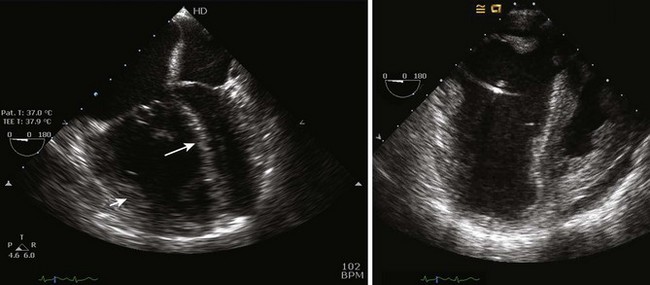
Step 7: Assess the Pulmonary Veins
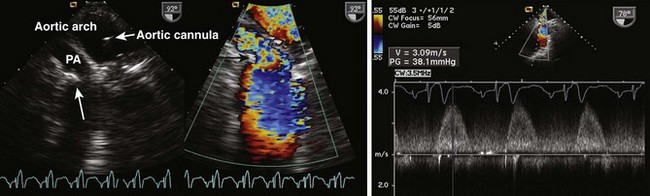
Step 8: Assess the Pulmonary Artery and Aorta
Step 9: Check for Patent Foramen Ovale
Key Points Post-Cardiopulmonary Bypass Transesophageal Echocardiography Assessment during Heart Transplant
Lung Transplant: Recipient Echocardiography
Background
Overview of Echocardiographic Approach
Anatomic Imaging and Physiologic Data
Acquisition, Analysis, and Pitfalls: Initial Assessment after Anesthetic Induction
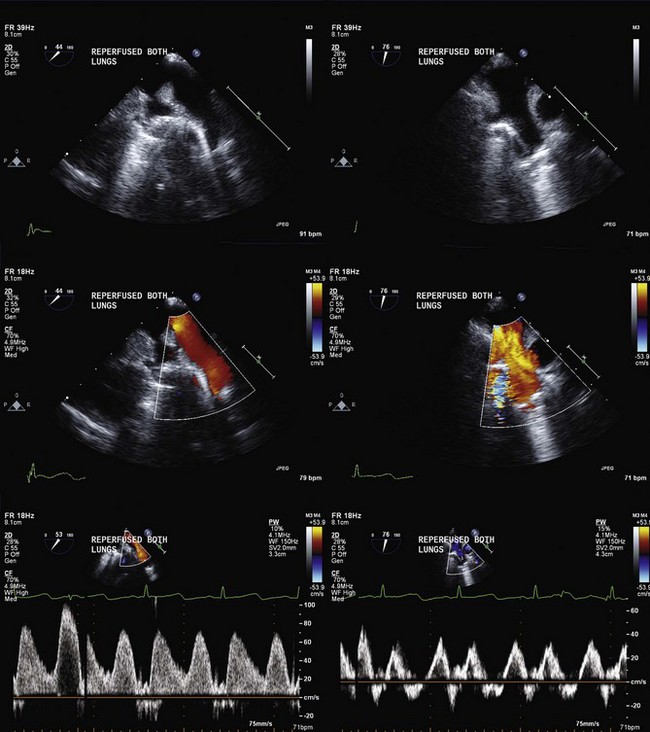
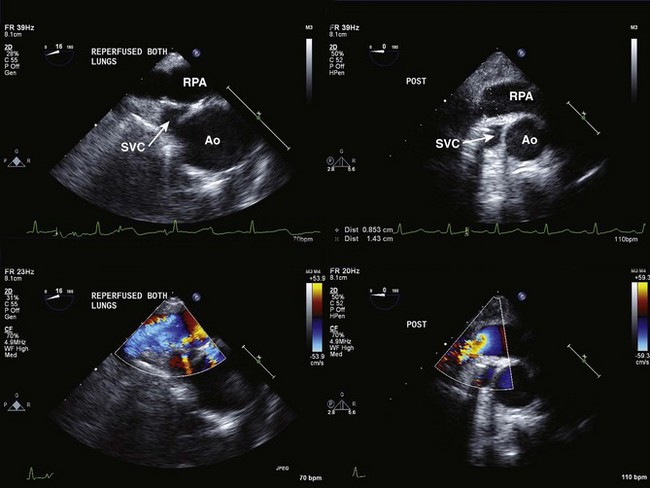
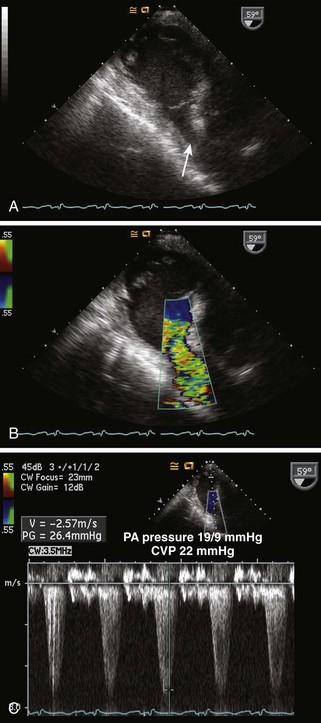
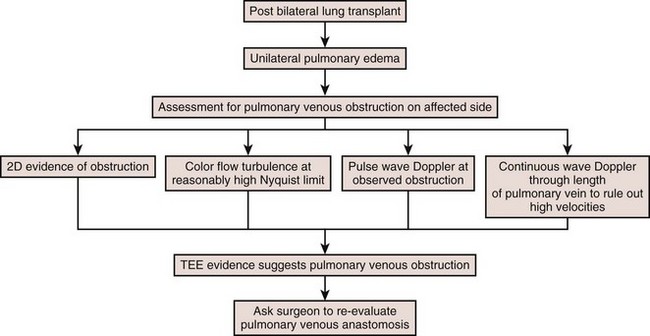
Acquisition, Analysis and Pitfalls: Native Lung Explant and Allograft Implant (No Cardiopulmonary Bypass)
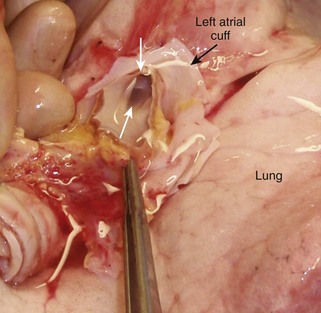
Figure 11-5 The donor lung. The white arrows show the orifices of the pulmonary veins surrounded by the LA cuff.
Key Points Transesophageal Echocardiography Assessment Post-Implantation Lung Transplant
Acquisition, Analysis, and Pitfalls: Procedure Performed with Cardiopulmonary Bypass
1 Stehlik J, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: Twenty-seventh official adult heart transplant report—2010. J Heart Lung Transplant. 2010;29:1089-1103.
2 Christie JD, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: Twenty-seventh official adult lung and heart-lung transplant report—2010. J Heart Lung Transplant. 2010;29:1104-1118.
3 Venkateswaran RV, Townend JN, Wilson IC, et al. Echocardiography in the potential heart donor. Transplantation. 2010;89:894-901.
Excellent review of what to look for in assessing a donor heart for transplant suitability.
4 Asante-Korang A. Echocardiographic evaluation before and after cardiac transplantation. Cardiol Young. 2004;14(Suppl 1):88-92.
5 Romano P, Mangion JM. The role of intraoperative transesophageal echocardiography in heart. Echocardiography. 2002;19:599-604.
Two nice reviews of what to look for in children and adults after cardiac transplantation.
6 Chumnanvej S, Wood MJ, MacGillivray TE, Melo MF. Perioperative echocardiographic examination for ventricular assist device implantation. Anesth Analg. 2007;105:583-601.
7 Augoustides JG. Perioperative echocardiographic assessment of left ventricular assist device implantation: Additional causes of inflow cannula obstruction. Anesth Analg. 2008;106:673-674.
Two nice reviews of the specifics in the examination of patients with assist devices.
8 Michel-Cherqui M, Brusset A, Liu N, et al. Intraoperative transesophageal echocardiographic assessment of vascular anastomoses in lung transplantation. A report on 18 cases. Chest. 1997;111:1229-1235.
9 Huang YC, Cheng YJ, Lin YH, et al. Graft failure caused by pulmonary venous obstruction diagnosed by intraoperative transesophageal echocardiography during lung transplantation. Anesth Analg. 2000;91:558-560.
10 Myles PS, Marasco S. Misleading turbulent flow through pulmonary venous anastomoses during lung transplantation. Anesth Analg. 2008;107:1504-1505.
11 McIlroy DR, Sesto AC, Buckland MR. Pulmonary vein thrombosis, lung transplantation, and intraoperative transesophageal echocardiography. J Cardiothorac Vasc Anesth. 2006;20:712-715.