16 Intralesional Injections
Indications
Indications for the use of intralesional steroid injections in dermatology include the following:
Equipment
The equipment used for intralesional injections is listed here and shown in Figure 16-1:
Informed Consent
Patients should be informed of the risks of skin atrophy, incomplete resolution of the lesion, and hypopigmentation. Have the patient sign a consent form, especially if the lesion is on the face. Special care should be taken when treating lesions on the face in darkly pigmented individuals because hypopigmentation can be a particularly unacceptable side effect. As with all informed consents, the patient should be made aware of alternative therapies. Alternative therapies for keloids are listed in Table 16-1.
| Topical | |
| Corticosteroids | |
| Retinoids | |
| Imiquimod | |
| Mederma | |
| Vitamin E | |
| Injectable | |
| Corticosteroids | |
| Interferons | |
| 5-Fluorouracil | |
| Verapamil | |
| Bleomycin | |
| Surgical | |
| Surgical debulking or excision | |
| Laser debulking or excision | |
| Radio-frequency electrosurgery planing | |
| Physical | |
| Laser therapy | |
| Radiation therapy | |
| Compression therapy | |
| Silicone sheeting | |
| Cryotherapy | |
| Fractional laser ablation |
Source: Adapted from Baldwin H. Keloid management (Chap 44). In: Robinson JK, et al., eds., Surgery of the Skin: Procedural Dermatology. Philadelphia: Elsevier; 2005.
Steroid Strength
Once the appropriate-strength steroid for the injection has been chosen, the standard-strength preparations may need to be diluted to produce the desired strength. Recommendations for steroid strength and needle size are listed in Table 16-2. Triamcinolone acetonide suspension is available in two strengths: 10 and 40 mg/mL. It is essential to dilute the steroid, especially for injections of cystic acne of the face. Dilution may be done for each patient just before giving the injection or may be done in a sterile vial of saline and saved for the injection of multiple patients over time. Unless giving intralesional injections frequently, it is probably better to perform the dilution for each patient. Diluted vials can lose their potency and have a higher theoretical risk of contamination.
TABLE 16-2 Recommended Steroid Strength and Needle Size for Intralesional Injections
|
Lesions |
Triamcinolone (mg/mL)a |
Needle size (gauge) |
|---|---|---|
| Acne cysts (face and neck) | 1–2 | 30 |
| Acne cysts (trunk) | 2–3.3 | 27–30 |
| Acne keloidalis nuchae | 5–10 | 25–27 |
| Alopecia areata | 5 for scalp and 3.3 for face | 27 |
| Discoid lupus | 2.5–5 | 27 |
| Granuloma annulare | 5 | 27 |
| Hidradenitis suppurativa | 3.3–5 | 27 |
| Hypertrophic scars | 10–20 | 25–27 |
| Keloids | 10–40 | 25–27 |
| Lichen simplex chronicus | 2.5–5 | 27 |
| Prurigo nodularis | 5 | 27 |
| Psoriasis | 2.5–5 | 27 |
| Sarcoidosis | 2.5 on face and 5 on body | 27–30 |
a For lesions on the face, always start with lower concentrations.
A 1-mL Luer-Lok or tuberculin syringe is useful for making a single dilution before injection. To create a 2 mg/mL concentration, draw 0.4 mL of sterile saline into a 1-mL syringe and add 0.1 mL of 10 mg/mL triamcinolone. Other dilutions are listed in Table 16-3. Turn the syringe upside down a number of times to mix the new suspension. It is recommended that the saline be drawn up first because it is more acceptable to get a little saline into the triamcinolone than vice versa. Recommended needle sizes by lesion are listed in Table 16-2.
TABLE 16-3 Common Triamcinolone Dilutions in a 1-mL Syringe
|
Concentration (mg/mL) |
mL of Triamcinolone 10 mg/mL |
mL of Sterile Saline for Injection |
|---|---|---|
| 1 | 0.1 | 0.8 |
| 2 | 0.1 | 0.4 |
| 2.5 | 0.2 | 0.6 |
| 3.3 | 0.2 | 0.4 |
| 5 | 0.3 | 0.3 |
Treating Specific Lesions
Acne Nodules and Cysts
Patients with tender large nodulocystic lesions can expect to get symptomatic relief within 24 hours of an intralesional injection. The lesion will flatten within 2 to 3 days with an effective injection.1 Although this should not be the primary treatment of acne, it can provide short-term relief while employing more long-term treatment regimens.
One small study evaluated the effectiveness of intralesional injections of steroids in the therapy of nodulocystic acne.1 They found that 0.63 mg/mL of triamcinolone was as effective as 2.5 mg/mL.1 Betamethasone injections were no better than saline controls.1 One review article states that concentrations of 3.3 and 5 mg/mL of triamcinolone are standard dilutions for intralesional acne injections.2
We recommend using 1 to 3.3 mg/mL of triamcinolone for nodulocystic acne depending on the location of the lesions and the experience of the clinician and patient. Triamcinolone can be injected with minimal pain using a 30-gauge needle on a 1-mL syringe at a 45- to 90-degree angle with the skin (Figure 16-3).
Acne Keloidalis Nuchae
Acne keloidalis (Figure 16-4) occurs on the posterior neck most commonly in men with highly pigmented skin. It is an inflammatory condition that is exacerbated by shaving the back of the neck. It has features of acne and folliculitis. Over time keloidal-type scars occur and can become very large. Treatment and prevention include not cutting the hair too short and using topical steroids and topical retinoids. Tender and painful keloidal nodules can be injected with triamcinolone for some relief. Concentrations of 5 to 10 mg/mL can be used. The heavier the fibrosis and scarring, the larger the needle needed to inject the lesion.
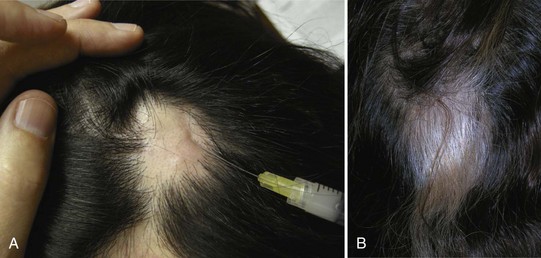
Alopecia Areata (Figure 16-5)
Although a recent Cochrane review on the treatment of alopecia areata (Figure 16-5) found no RCTs on the use of intralesional steroids (and many other treatments), they did acknowledge that this is a commonly used treatment for alopecia areata.3 Considering the possibility of spontaneous remission in the early stages of the disease, it is reasonable to reassure the patient and recommend tincture of time. However, many patients are seeking an active treatment. Intralesional steroid for alopecia areata is a well-accepted standard treatment and often gives patients hope that they will regain their hair. Recommended concentrations of triamcinolone range from 5 to 10 mg/mL for the scalp, but the higher concentrations often cause scalp atrophy. Therefore we recommend using 5 mg/mL of triamcinolone for the scalp. Alopecia areata can affect the eyebrows and the beard. For those regions it is safer to stick with a lower concentration of triamcinolone such as 3.3 mg/mL. A long 27-gauge needle (1.25 to 1.5 inches) will allow for treatment of larger areas with fewer injections per site.
Cutaneous Lupus
Intralesional steroids have been used for decades to treat patients with all types of localized cutaneous lupus (Figure 16-6).4,5 Widespread cutaneous lupus is best treated with topical steroids and systemic agents when indicated. For specific local lesions that are not responding well, discuss the option of intralesional steroids with the patient. Our recommendation is to use from 2.5 to 5 mg/mL depending on the site. Special care should be taken when treating lupus on the face in a darkly pigmented individual because hypopigmentation can be a particularly unacceptable adverse effect.
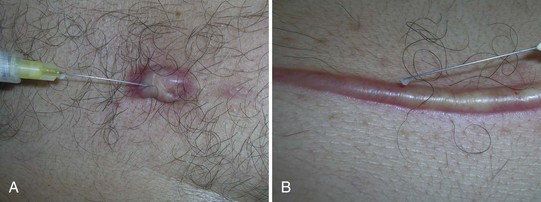
Hidradenitis Suppurativa
Injecting painful acute hidradenitis suppurativa cysts (Figure 16-7) is similar to injecting acne cysts, but a higher concentration of triamcinolone (3.3 to 5 mg/mL) is acceptable because these lesions are usually in the axilla, chest, or groin and less prone to atrophy. Also a little skin atrophy is generally more acceptable in these locations than the face. It may be best to use the lower end of this range when injecting hidradenitis around the breasts because this area is of more cosmetic concern. Because the cysts are often larger than acne, a 3-mL syringe may be needed to provide more volume for injection. Large, purulent cysts can be drained with a No. 11 scalpel first before injecting the steroid.
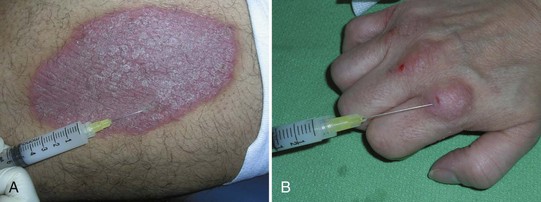
Granuloma Annulare
Granuloma annulare (Figure 16-8) is an idiopathic granulomatous disease that typically appears in ringlike formations. Treatments for localized disease include high-potency topical steroids and injections of triamcinolone. We recommend using 5 mg/mL of triamcinolone and a 27-gauge needle. Four injection sites are usually needed to cover one annular lesion, so a syringe larger than 1 mL is often needed. We prefer not to inject more than 4 mL total. Inject into the granulomatous lesion and not below the lesion. Our experience has shown steroid injections to be more effective than topical steroids. If the condition is disseminated, there are other treatments to consider.
Hypertrophic Scars and Keloids
A hypertrophic scar (Figure 16-9) is one in which the scar tissue is raised and prominent over the area that was cut, burned, or traumatized. It may show prominent suture marks and can be redder or differently pigmented compared with the surrounding tissue. Hypertrophic scars frequently regress over a few years. A keloid is similar to a hypertrophic scar but it grows beyond the limits of the original surgery. Keloids tend to become quite raised and enlarged. There are histologic differences between hypertrophic scars and keloids. For the purpose of intralesional injection, however, they are treated identically.
Persons with darker skin are at higher risk than light-skinned persons of developing keloids. Keloids most commonly occur on the chest, shoulders, and other areas of increased skin tension but can occur anywhere on the skin. They tend to be more common after a traumatic lesion. Keloids frequently occur after ear piercing and acne scarring. Table 16-1 provides a list of possible treatments for keloids. Surgical excision frequently induces more scarring exacerbating the original problem. If excision is deemed necessary, scarring can be limited by including dilute steroids in the anesthetic, injecting steroids into the surgical site after surgery, using minimal tissue pressure techniques, and postoperative occlusion with silicone sheets for several months.
Keloids can be treated with cryosurgery alone or in combination with intralesional steroids. In one small controlled study, ten patients with keloids were treated with intralesional steroid and cryosurgery vs. intralesional steroid or cryosurgery alone.6 Patients were treated at least three times 4 weeks apart. In terms of keloid thickness, the keloids responded significantly better to combined cryosurgery and triamcinolone vs. triamcinolone alone or cryotherapy alone. Pain intensity was significantly lowered with all treatment modalities. Pruritus was lowered only with the combined treatment and intralesional corticosteroid alone.6
In another study 20 patients with hypertrophic and keloidal scars received two 15-second cycles (total 30 seconds) of cryosurgery treatments once monthly for 12 months with intralesional injections of 10 to 40 mg/mL triamcinolone once monthly for 3 months.7 Topical application of silicone gel was added three times daily for 12 months. The control group included 10 patients who received treatment with silicone sheeting only. After 1 year, improvement was seen in all parameters, especially in terms of symptoms, cosmetic appearance, and associated signs compared to baseline and compared to the control group.7
Layton et al. reported that the intralesional injection of a steroid is helpful but cryotherapy is more effective (85% improvement in terms of flattening) for recent acne keloids located on the back.8 Treatment with intralesional triamcinolone was beneficial, but the response to cryosurgery was significantly better in early, vascular lesions.8
In one double-blind clinical trial, 40 patients were randomized to receive intralesional triamcinolone (TAC) or a combination of TAC and 5-fluorouracil (5-FU).9 Both groups received injections at weekly intervals for 8 weeks and lesions were assessed for erythema, pruritus, pliability, height, length, and width. Both groups showed an acceptable improvement in nearly all parameters, but these were more significant improvement in the TAC + 5-FU group (P < 0.05 for all except pruritus and percentage of itch reduction). Good to excellent improvement were reported by 20% of the patients receiving TAC alone and 55% of the patients in the group receiving TAC and 5-FU.9
Earlobe keloids may be excised with a shave excision and injection of the base with steroid (Figure 16-10). It is hard to get much volume of steroid into the base of these keloids, so 40 mg/mL triamcinolone is preferred as the concentration for injection. Another option is to use the radio-frequency electrosurgery technique with a pure cutting setting and a steroid in the anesthetic.
According to one article, simple excision of earlobe keloids can result in recurrence rates approaching 80%.10 A randomized prospective trial comparing steroid injections versus radiation therapy found that 2 of 16 keloids (12.5%) recurred after surgery and radiation therapy, whereas 4 of 12 (33%) recurred after surgery and steroid injections. These results did not produce a statistically significant difference. No alteration of skin pigmentation, wound dehiscence, or chronic dermatitis was observed in any patient in either group.10 While radiation therapy was considered easy to obtain in this study, it is reasonable to use steroid injections in office practice.
Localized Dermatitis (Lichen Simplex Chronicus, Prurigo Nodularis)
In a recent review paper, no studies were found on the use of intralesional steroids for psoriasis or localized dermatitis since the 1960s.11 The authors describe their personal experience as excellent using 2.5 mg/mL triamcinolone for localized dermatitis (such as lichen simplex chronicus, prurigo nodularis, and nonspecific eczema).11 We recommend using 2.5 to 5.0 mg/mL triamcinolone with a 27-gauge needle for the treatment of localized dermatitis. Because prurigo nodularis (Figure 16-11) can be particularly difficult to treat, the higher concentration may be needed.
Psoriasis
In the same review paper, no good clinical studies were found on the use of intralesional steroids for psoriasis (Figure 16-12).11 The authors describe their personal experience as virtually 100% effective using 2.5 mg/mL triamcinolone for small plaques of psoriasis on the trunk and limbs.11 In one small series, five patients with chronic intermittent palmoplantar pustulosis were treated with intralesional injections of 3.3 to 5.0 mg/mL of triamcinolone acetonide.12 Prompt clearing of symptoms and lesions occurred and lasted 3 to 6 months. Despite the discomfort experienced from the injections, patients preferred this treatment modality over others available in 1984. Side effects included hypopigmentation, cutaneous atrophy, and, in one patient, exacerbation of a latent dermatophyte infection.12 Despite the lack of evidence for the use of intralesional steroid injections for localized psoriasis, it is an accepted treatment option. We recommend using from 2.5 to 5.0 mg/mL with a 27-gauge needle for injection.
Sarcoidosis
Cutaneous sarcoidosis (Figure 16-13) may respond to intralesional steroids in a similar manner as other granulomatous diseases such as granuloma annulare. Cutaneous sarcoidosis is often found on the face of black women so the concentration of steroid must take the risks of atrophy and hypopigmentation into account. Concentrations of 2.5 mg/mL on the face and 5 mg/mL on the body should provide some relief from cutaneous sarcoidosis.

FIGURE 16-14 Hypopigmentation from cryosurgery and intralesional triamcinolone used to treat acne keloidalis nuchae.
(Copyright Richard P. Usatine, MD.)
Complications of Steroid Injections
Complications of steroid injections include skin atrophy and hypopigmentation (Figure 16-14). If skin atrophy occurs, it is worth waiting a number of months to see if the atrophy will resolve. If the atrophy is particularly bothersome after 4 months, the patient could be referred for injections of their own fat to restore the depressed area. This can be performed with liposuction and injection technique.
Candida Antigen and Bleomycin Intralesional Injections
Candida Antigen
The first study of more than 100 patients who were treated with intralesional Candida was published in 2000. It reported that 85% of patients were completely cleared after three injections at 1-month intervals.13 The advantages to this method of treatment are that if the patient’s immune system recognizes the verrucous protein as foreign, then all lesions disappear, recurrences are rare, and there are no open wounds to deal with after treatment.
This technique has not been tried on condyloma but can be used for virtually all other warts.
The Pfenninger Candida Protocol: Steps and Principles13,14
|
Creating 1.0 mL for Injection |
Candida Antigen (mL) |
2% Lidocaine (no Epinephrine) (mL) |
|---|---|---|
| Generic 1 : 1000 | 0.25 | 0.75 |
| Candin 1 : 500 | 0.5 | 0.5 |
Bleomycin
Bleomycin sulfate is a chemotherapeutic agent. Like Candida antigen, it too has not been approved by the FDA for the treatment of verrucae but it has been well studied and used for more than 20 years.15,16 Its efficacy is similar to that of Candida antigen but reactions are often more robust. It has not been used for the treatment of condyloma but can be used in all other areas where warts develop.
Bleomycin Injections: Steps and Principles
|
Wart Size |
Amount of Solution (0.5 unit/mL) |
|---|---|
| <5 mm | 0.1-0.2 mL |
| 5–10 mm | 0.2-0.4 mL |
| >10 mm | Up to a maximum of 1 mL (rarely needed) |
| Multiple warts | Up to 3 mL (1.5 unit) per visit |
Coding and Billing Pearls
Intralesional injections have two CPT codes for giving the injections (see Box 16-1). These should be simple to use since there is one code for up to and including seven lesions (not separate injections) and one code for eight lesions and above. If it takes three injections to inject one large plaque of psoriasis, this is still counted as one lesion.
1. Levine RM, Rasmussen JE. Intralesional corticosteroids in the treatment of nodulocystic acne. Arch Dermatol. 1983;119:480-481.
2. Taub AF. Procedural treatments for acne vulgaris. Dermatol Surg. 2007;33:1005-1026.
3. Delamere FM, Sladden MM, Dobbins HM, Leonardi-Bee J. Interventions for alopecia areata. Cochrane Database Syst Rev. 2008;CD004413.
4. Verbov J. The place of intralesional steroid therapy in dermatology. Br J Dermatol. 1976;94(suppl 12):51-58.
5. Callen JP. Treatment of cutaneous lesions in patients with lupus erythematosus. Dermatol Clin. 1994;12:201-206.
6. Yosipovitch G, Widijanti SM, Goon A, et al. A comparison of the combined effect of cryotherapy and corticosteroid injections versus corticosteroids and cryotherapy alone on keloids: a controlled study. J Dermatolog Treat. 2001;12:87-90.
7. Boutli-Kasapidou F, Tsakiri A, Anagnostou E, Mourellou O. Hypertrophic and keloidal scars: an approach to polytherapy. Int J Dermatol. 2005;44:324-327.
8. Layton AM, Yip J, Cunliffe WJ. A comparison of intralesional triamcinolone and cryosurgery in the treatment of acne keloids. Br J Dermatol. 1994;130:498-501.
9. Darougheh A, Asilian A, Shariati F. Intralesional triamcinolone alone or in combination with 5-fluorouracil for the treatment of keloid and hypertrophic scars. Clin Exp Dermatol. 2009;34:219-223.
10. Sclafani AP, Gordon L, Chadha M, Romo TIII. Prevention of earlobe keloid recurrence with postoperative corticosteroid injections versus radiation therapy: a randomized, prospective study and review of the literature. Dermatol Surg. 1996;22:569-574.
11. Richards RN. Update on intralesional steroid: focus on dermatoses. J Cutan Med Surg. 2010;14:19-23.
12. Goette DK, Morgan AM, Fox BJ, Horn RT. Treatment of palmoplantar pustulosis with intralesional triamcinolone injections. Arch Dermatol. 1984;120:319-323.
13. Phillips RC, Ruhl TS, Pfenninger JL, Garber MR. Treatment of warts with Candida antigen injection. Arch Dermatol. 2000;136:1274-1275.
14. Pfenninger JL, Fowler GC. Pfenninger and Fowler’s Procedures for Primary Care, 3rd ed. Philadelphia: Elsevier; 2010.
15. Amer M, Diab N, Ramadan A, et al. Therapeutic evaluation for intralesional injection of bleomycin sulfate in 143 resistant warts. J Am Acad Dermatol. 1988;18:1313-1316.
16. Sollitto RJ, Pizzano DM. Bleomycin sulfate in the treatment of mosaic plantar verrucae: a follow-up study. J Foot Ankle Surg. 1996;35:169-172.