CHAPTER 27 Intracranial region
The cranial cavity contains the brain, the intracranial portions of cranial and spinal nerves, blood vessels, meninges and cerebrospinal fluid. Its walls are formed by parts of the frontal, ethmoid, parietal, sphenoid, temporal and occipital bones.
INTERNAL SURFACE OF CRANIAL VAULT
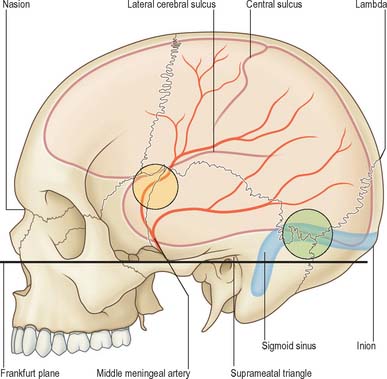
The internal surface of the cranial vault is deeply concave. It includes most of the frontal and parietal bones and the squamous part of the occipital bone, variously united at the coronal, sagittal and lambdoid sutures (Fig. 27.1). With increasing age, these sutures become obliterated by a gradual process that begins on their intracranial surfaces. Inconstant foramina may occur in the parietal bones near the sagittal sulcus and anterior to the lambdoid suture: they admit emissary veins associated with the superior sagittal sinus. The internal surfaces of the frontal and parietal bones are grooved by furrows that house the frontal and parietal branches of the middle meningeal vessels; the grooves contain the openings of minute channels that admit perforating vessels to the haemopoietic marrow within the diploic bone. Impressions for cerebral gyri are less distinct on the vault than they are on the cranial base.
CRANIAL FOSSAE (ANTERIOR, MIDDLE, POSTERIOR)
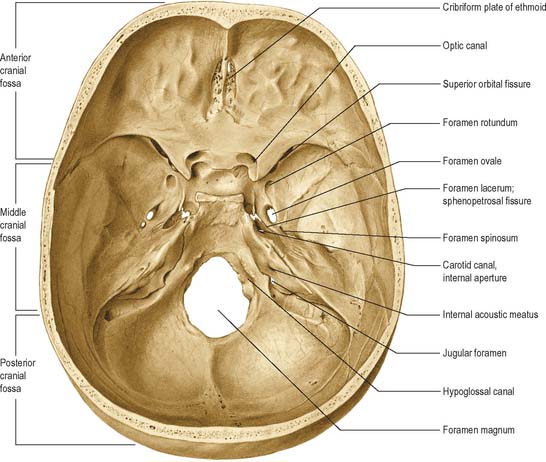
The base of the cranial cavity is divided into three distinct fossae, the anterior, middle and posterior cranial fossae (Fig. 27.2). The floor of the anterior cranial fossa is at the highest level and the floor of the posterior fossa is at the lowest.
ANTERIOR CRANIAL FOSSA
The convex cranial surface of the frontal bone separates the brain from the orbit and bears impressions of cerebral gyri and small grooves for meningeal vessels. Posteriorly, it articulates with the anterior border of the lesser wing of the sphenoid bone which forms the posterior boundary of the anterior cranial fossa. The medial end of the lesser wing constitutes the anterior clinoid process. The lesser wing joins the body of the sphenoid body by two roots which are separated by the optic canal. The anterior root, broad and flat, is continuous with the jugum sphenoidale, while the smaller and thicker posterior root joins the body of the sphenoid bone near the posterior bank of the sulcus chiasmatis. The frontosphenoid and sphenoethmoidal sutures divide the sphenoid from the adjacent bones.
MIDDLE CRANIAL FOSSA
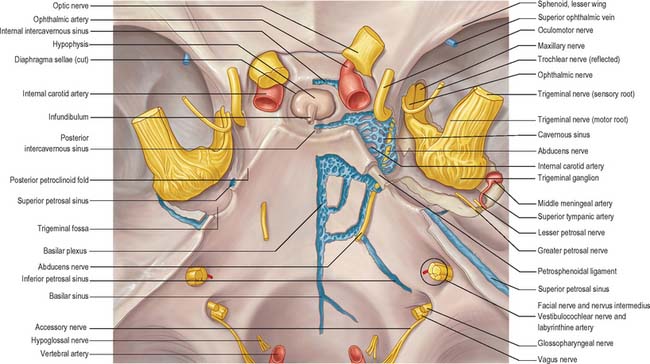
The middle cranial fossa communicates with the orbits by the superior orbital fissures, each bounded above by a lesser wing, below by a greater wing, and medially by the body of the sphenoid bone. The fissures are wider medially, and each has a long axis sloping inferomedially and forwards. They are the major gateways into the orbit from the cranial cavity and contain the oculomotor, trochlear and abducens nerves, and the lacrimal, frontal and nasociliary branches of the ophthalmic division of the trigeminal nerve, together with filaments from the internal carotid plexus (sympathetic), the ophthalmic veins, the orbital branch of the middle meningeal artery, and the recurrent branch of the lacrimal artery (see Ch. 39).
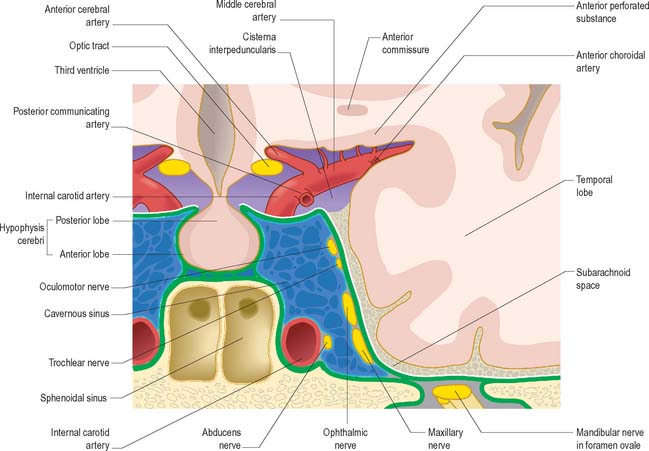
Centrally the floor of the fossa is narrower and formed by the body of the sphenoid bone which contains the sphenoidal sinuses (see Ch. 32). The roof of the sinus is deeply concave and houses the pituitary gland (hypophysis): it is therefore termed the pituitary (hypophysial) fossa, also known as the sella turcica because it resembles the shape of a Turkish saddle. The anterior edge of the pituitary fossa is completed laterally by a middle clinoid process, the floor forms the roof of the sphenoidal air sinuses, and the posterior boundary presents a vertical pillar of bone, the dorsum sellae. The superolateral angles of the dorsum are expanded as the posterior clinoid processes. A fold of dura, the diaphragma sella, is attached to the anterior and posterior clinoid processes and roofs over the pituitary fossa. The smooth upper part of the anterior wall of the fossa, the jugum sphenoidale, is bounded behind by the anterior border of the grooved sulcus chiasmatis which leads laterally into the optic canals. Each canal transmits the optic nerve and ophthalmic artery. The optic chiasma usually lies posterosuperior to the sulcus chiasmatis, the tuberculum sellae lies below the sulcus. The cavernous sinus lies lateral to the pituitary fossa. The lateral wall of the body of the sphenoid contains a shallow carotid groove related to the internal carotid artery as it ascends from the carotid canal and runs through the cavernous sinus. Posterolaterally the groove may be deepened by a small projecting lingula.
The trigeminal impression, which accommodates the trigeminal ganglion, is situated posterior to the foramen lacerum on the anterior surface of the petrous part of the temporal bone near its apex. Its depth is variable. Posterolateral to the impression is a small, shallow, pit, limited posteriorly by a rounded arcuate eminence (produced by the underlying anterior semicircular canal). Lateral to the impression a narrow groove passes posterolaterally into the hiatus for the greater petrosal nerve, and even further laterally is the hiatus for the lesser petrosal nerve. A smooth trigeminal notch leads into the impression. It lies on the upper border of the petrous temporal, anteromedial to the groove for the superior petrosal sinus; at this point, the trigeminal nerve separates the sinus from bone. At the anterior end of the trigeminal notch is the petrosphenoidal ligament (of Gruber), attached to a minute bony spicule, directed anteromedially. The abducens nerve bends sharply across the upper petrous border, and passes between the ligament and the dorsum sellae anterior to the petrosphenoidal ligament (for a detailed analysis of the course of the abducens nerve in the petroclival region see Ozveren et al 2002).
POSTERIOR CRANIAL FOSSA
The hypoglossal (anterior condylar) canal lies medial to and below the lower border of the jugular foramen, at the junction of the basilar and lateral parts of the occipital bone. It transmits the hypoglossal nerve and its recurrent branch together with the meningeal branch of the ascending pharyngeal artery and an emissary vein which links the (intracranial) basilar plexus with the (extracranial) internal jugular vein. When a posterior condylar canal is present behind the occipital condyle, its internal orifice is posterolateral to that of the hypoglossal canal and it contains a sigmoid emissary vein (associated with the occipital veins) and a meningeal branch of the occipital artery. The occipital condyles lie within the anterior aspect of the foramen magnum: their medial aspects are roughened for the attachments of the alar ligaments associated with the atlanto-axial joints.
MENINGES
Cranial and spinal meninges are continuous through the foramen magnum. The cranial meninges are described in this section and the spinal meninges are described on p. 751).
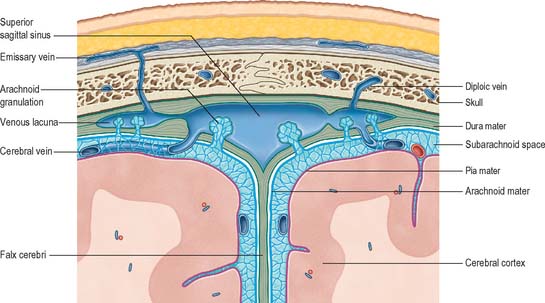
DURA MATER
The cranial dura, which lines the cranial cavity, differs from the spinal dura mainly in its relationship to the surrounding bones. It has an inner, or meningeal, layer and an outer, or endosteal, layer. These layers are united except where they separate to enclose the venous sinuses that drain blood from the brain. There is little histological difference between the endosteal and meningeal layers. Both contain fibroblasts, and the endosteal layer also contains osteoblasts. Focal calcification may occur in the falx cerebri.
Dural partitions
Falx cerebri
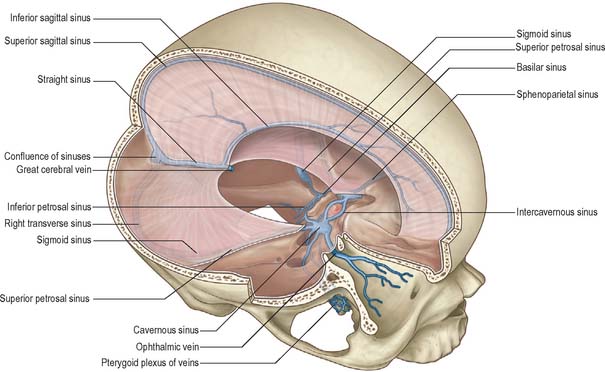
The falx cerebri is a strong, crescent-shaped sheet that lies in the sagittal plane and occupies the longitudinal fissure between the two cerebral hemispheres (Fig. 27.3). The crescent is narrow in front, where the falx is fixed to the crista galli, and broad behind, where it blends with the tentorium cerebelli: the straight sinus runs along this line of attachment (Fig. 27.3). The anterior part of the falx is thin and may have a number of irregular perforations. Its convex upper margin is attached to the internal cranial surface on each side of the midline, as far back as the internal occipital protuberance. The superior sagittal sinus runs in a cranial groove within the dura along this margin: the falx is attached to the lips of this groove. The lower edge of the falx is free and concave and contains the inferior sagittal sinus.
Tentorium cerebelli
The shape of the tentorium cerebelli (Fig. 27.3) is reminiscent of a single-poled tent, from which its name is derived. It lies between the cerebellum and the occipital lobes of the cerebral hemispheres and divides the cranial cavity into supratentorial and infratentorial compartments, which contain the forebrain and hindbrain respectively. Its concave anterior edge is free and separated from the dorsum sellae of the sphenoid bone by a large curved hiatus, the tentorial incisure or notch, which is filled by the midbrain and the anterior part of the superior aspect of the cerebellar vermis. The convex outer limit of the tentorium is attached posteriorly to the lips of the transverse sulci of the occipital bone and to the posterior-inferior angles of the parietal bones, where it encloses the transverse sinuses. Laterally, it is attached to the superior borders of the petrous parts of the temporal bones, where it contains the superior petrosal sinuses. On each side, near the apex of the petrous temporal bone, the lower layer of the tentorium is evaginated anterolaterally under the superior petrosal sinus to form a recess between the endosteal and meningeal layers in the middle cranial fossa. The recess contains the roots and ganglion of the trigeminal nerve; the evaginated meningeal layer fuses in front with the anterior part of the ganglion.
Transtentorial coning
Normally, the arrangement of dural partitions such as the falx cerebri and tentorium cerebelli may help to stabilize the brain within the cranial cavity. However, when there is focal brain swelling or a focal space-occupying lesion within the brain or cranial cavity, raised intracranial pressure may cause the brain to herniate under the falx cerebri or, more significantly, through the tentorial incisure, which will compress the oculomotor nerve, midbrain and arteries on the inferior medial surface of the temporal lobe. This process of transtentorial coning is particularly dangerous because of the risk of secondary vascular compression; it often represents the terminal event in patients with supratentorial space-occupying lesions. Similarly, space-occupying lesions in the small infratentorial compartment may cause upward herniation through the tentorial hiatus or downward herniation through the foramen magnum (see Fig. 19.22).
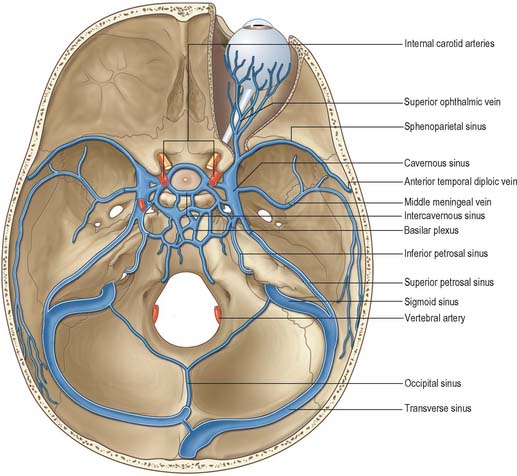
Dural venous sinuses
Dural venous sinuses form a complex network of venous channels which drain blood from the brain and cranial bones (Fig. 27.4, see Fig. 17.10). They lie between the endosteal and meningeal layers of dura mater, are lined by endothelium, have no valves, and their walls are devoid of muscular tissue. They develop initially as venous plexuses, and most adult sinuses preserve a plexiform arrangement (to a variable degree), rather than being simple vessels with a single lumen. Plexiform arrays of small veins adjoin the sagittal superior and inferior sagittal and straight sinuses and, less frequently, the transverse sinuses, and ridges of ‘spongy’ venous tissue often project into the lumina of the superior sagittal and transverse sinuses (Browder & Kaplan 1976; Kaplan & Browder 1976).
The structure of cranial venous sinuses, their plexiform nature and wide connections with cerebral and cerebellar veins, vary considerably, particularly in earlier years, e.g. in infancy the falx cerebelli may contain large plexiform channels and venous lacunae that augment the occipital sinus. These variations cannot be detailed in a general text but must be established for the individual by angiography when clinical necessity arises. There is experimental evidence that parts of sinuses (and even diploic veins) can be filled by forcible internal carotid injection, from which it has been inferred that arteriovenous shunts may exist (Browder & Kaplan 1976). A connection between the middle meningeal arteries and the superior sagittal sinus has been demonstrated in this way, although the sites of communication are unknown. Dural arteriovenous fistulas are thought to be acquired lesions that form in an area of thrombosis within a sinus. If the sinus remains completely thrombosed, venous drainage from these lesions occurs through cortical veins, or, if the sinus is open, venous drainage is usually into the involved sinus.
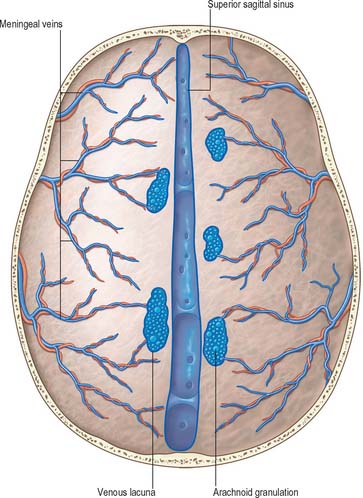
Superior sagittal sinus
The superior sagittal sinus runs in the attached convex margin of the falx cerebri. It grooves the internal surface of the frontal bone, the adjacent margins of the two parietal bones and the squamous part of the occipital bone (Fig. 27.3, Fig. 27.5, see Fig. 17.10). It begins near the crista galli, a few millimetres posterior to the foramen caecum, and receives primary tributaries from cortical veins of the frontal lobes, the ascending frontal veins. The sinus is triangular in cross-section and invaded, in its intermediate third, by variable bands and projections from its dural walls, which may extend as horizontal shelves that divide its lumen into superior and inferior channels. It is narrow anteriorly, and widens gradually to approximately 1 cm diameter as it runs backwards. At its posterior end, the sinus enters the confluence of the sinuses (Fig. 27.4) which is situated to one side (usually the right) of the internal occipital protruberance. At the confluence the superior sagittal sinus usually deviates to become continuous with the right transverse sinus, but it also usually connects with the occipital and contralateral transverse sinuses. The size and degree of communication of the channels meeting at the confluence are highly variable: any sinus involved may be duplicated, narrowed, or widened near the confluence. In more than half of subjects all venous channels that converge towards the occiput interconnect, including the straight and occipital sinuses, but communication between channels may be absent or tenuous.
The superior sagittal sinus receives the superior cerebral veins and communicates by small orifices with irregular venous lacunae which lie near it in the dura mater. There are usually two or three lateral lacunae on each side of the midline, named frontal (small), parietal (large) and occipital (intermediate) lacunae: they tend to become confluent in the elderly, producing a single elongated lacuna on each side. These venous spaces are often so complex as to be almost plexiform. Fine fibrous bands cross the lacunae, and numerous arachnoid granulations project into them (Fig. 27.5, Fig. 27.6). The lacunae drain diploic and meningeal veins. Near its posterior end, the superior sagittal sinus receives veins from the pericranium which pass through parietal foramina.
Inferior sagittal sinus
The inferior sagittal sinus is located in the posterior half or two-thirds of the free margin of the falx cerebri (Fig. 27.3). It increases in size posteriorly, ends in the straight sinus and receives veins from the falx and sometimes from the medial surfaces of the cerebral hemispheres.
Straight sinus
The straight sinus lies in the junction of the falx cerebri with the tentorium cerebelli (Fig. 27.3, see Fig. 17.10). It runs posteroinferiorly as a continuation of the inferior sagittal sinus and drains into the transverse sinus. It is not (or only tenuously) continuous with the superior sagittal sinus. Its tributaries include the great cerebral vein and some superior cerebellar veins. It is triangular in cross-section.
Transverse sinus
The transverse sinuses begin at the internal occipital protuberance (Fig. 27.3, Fig. 27.4). One, usually the right, is directly continuous with the superior sagittal sinus, the other with the straight sinus. On both sides the sinuses run in the attached margin of the tentorium cerebelli, first on the squama of the occipital bone, then on the mastoid angle of the parietal bone. Each follows a gentle anterolateral curve, increasing in size as it does so, to the posterolateral part of the petrous temporal bone. Here it turns down as a sigmoid sinus, which ultimately becomes continuous with the internal jugular vein. Transverse sinuses are triangular in section and usually unequal in size; the one draining the superior sagittal sinus is the larger. They receive the inferior cerebral, inferior cerebellar, diploic and inferior anastomotic veins, and are joined by the superior petrosal sinuses where they continue as sigmoid sinuses.
Sigmoid sinus
The sigmoid sinuses are continuations of the transverse sinuses, beginning where these leave the tentorium cerebelli (Fig. 27.4, Fig. 27.7). Each sigmoid sinus curves inferomedially in a groove on the mastoid process of the temporal bone, crosses the jugular process of the occipital bone and turns forward to the superior jugular bulb, lying posterior in the jugular foramen. Anteriorly, a thin plate of bone separates its upper part from the mastoid antrum and air cells. It connects with pericranial veins via mastoid and condylar emissary veins.
Occipital sinus
The occipital sinus is the smallest of the sinuses. It lies in the attached margin of the falx cerebelli (Fig. 27.4) and is occasionally paired. It commences near the foramen magnum in several small channels, one joining the end of the sigmoid sinus, and connects with the internal vertebral plexuses. It ends in the confluence of the sinuses.
Cavernous sinus
The cavernous sinuses are two large venous plexuses that lie on either side of the body of the sphenoid bone, extending from the superior orbital fissure to the apex of the petrous temporal bone, with an average length of 2 cm and width of 1 cm. Each sinus contains the cavernous portions of the internal carotid artery, associated with a perivascular sympathetic plexus that can be seen with the naked eye, and several cranial nerves which run forward through the sinus to access the orbit via the superior orbital fissure (Fig. 27.4, Fig. 27.8, Fig. 27.9). Three major venous spaces have been described within the sinus, posterosuperior, anteroinferior, and medial to the cavernous portion of the carotid artery (Harris & Rhoton 1976). The sphenoidal air sinus and pituitary gland are medial relations and the uncus of the temporal lobe is lateral to the sinus. The trigeminal cave is near the inferoposterior part of its lateral wall, and extends posteriorly beyond it to enclose the trigeminal ganglion.
The oculomotor and trochlear nerves and the ophthalmic and maxillary divisions of the trigeminal nerve all lie in the lateral wall of the sinus. They project into the lumen and are usually covered medially by little more than endothelium. The abducens nerve pierces the dura close to the upper border of the apex of the petrous part of the temporal bone and enters the cavernous sinus by passing below the petrosphenoid ligament within a dural tunnel (Dorello’s canal). The abducens lies on the lateral side of the internal carotid artery, medial to the ophthalmic nerve, and below and medial to the nasociliary nerve. Numerous branches from the cavernous portion of the internal carotid artery, especially from the meningohypophysial and inferolateral trunks, supply the cavernous portions of all of the nerves that pass through the sinus. The preservation of these vessels during cavernous sinus surgery is important in preventing or minimizing postoperative cranial nerve deficits. (For more detailed descriptions of these branches, including their main variations, see Tran-Dinh 1987; Krisht et al 1994; Reisch et al 1996; Tekdemir et al 1998). Propulsion of blood in the cavernous sinus is partly due to pulsation of the internal carotid artery, but it is also influenced by gravity, and hence by the position of the head.
Tributaries of the cavernous sinus are the superior ophthalmic vein, inferior ophthalmic vein (either a branch or the whole vessel), superficial middle cerebral vein, inferior cerebral veins and sphenoparietal sinus. Less frequently, the central retinal vein and frontal tributary of the middle meningeal vein drain into it. The cavernous sinus drains to the transverse sinus via the superior petrosal sinus; to the internal jugular vein via the inferior petrosal sinus and a plexus of veins associated with the internal carotid artery; to the pterygoid plexus by veins traversing the emissary sphenoidal foramen, foramen ovale and foramen lacerum; and to the facial vein via the superior ophthalmic vein.
For more detailed descriptions of the microsurgical anatomy of the cavernous sinus, see Umansky et al 1994; Seoane et al 1998; Yasuda et al 2004.
Middle fossa triangles and the cavernous sinus
Parkinson described a triangle within the lateral wall of the cavernous sinus through which the cavernous portion of the carotid artery could be exposed for the surgical treatment of carotid-cavernous fistulae. At least ten triangles, formed by the convergence or divergence of the cranial nerves that lie either in the middle cranial fossa or in the cavernous sinus, have now been described. They may be used as intra-operative landmarks in approaching cavernous sinus lesions or in gaining access to the posterior cranial fossa from the middle cranial fossa (Watanabe et al 2003). The middle fossa triangles are formed as the three main divisions of the trigeminal nerve diverge from the trigeminal ganglion and head towards their exit foramina. The cavernous sinus triangles are formed as the optic, oculomotor, trochlear, and ophthalmic nerves converge on the optic canal and on the superior orbital fissure.
Intercavernous sinuses
The two cavernous sinuses are connected by anterior and posterior intercavernous sinuses and the basilar plexus (Fig. 27.4, Fig. 27.8). The intercavernous sinuses lie in the anterior and posterior attached borders of the diaphragma sellae and they thus form a complete circular venous sinus. All connections are valveless and the direction of flow in them is reversible. Small irregular sinuses inferior to the pituitary gland drain into the intercavernous sinuses. The inferior intercavernous sinuses are plexiform in nature and important in a surgical transnasal approach to the pituitary gland.
Superior petrosal sinus
This small narrow sinus drains the cavernous sinus into the transverse sinus on either side (Fig. 27.4, Fig. 27.8). It leaves the posterosuperior part of the cavernous sinus and runs posterolaterally in the attached margin of the tentorium cerebelli. It then crosses above the trigeminal nerve to lie in a groove on the superior border of the petrous part of the temporal bone and ends by joining a transverse sinus at the point where this curves down to become the sigmoid sinus. The superior petrosal sinus receives cerebellar, inferior cerebral and tympanic veins, and connects with the inferior petrosal sinus and the basilar plexus.
Inferior petrosal sinus
The inferior petrosal sinus drains the cavernous sinus into the internal jugular vein (Fig. 27.4, Fig. 27.8, see Fig. 17.10). It begins at the posteroinferior aspect of the cavernous sinus and runs back in a groove between the petrous temporal and basilar occipital bones. It next passes through the anteromedial part of the jugular foramen, accompanied by a meningeal branch of the ascending pharyngeal artery, and descends obliquely backwards to drain into the superior jugular bulb. It sometimes drains by a vein in the hypoglossal canal to the suboccipital vertebral plexus.
The sinus is often plexiform. It receives labyrinthine veins via the cochlear canaliculus and the vestibular aqueduct, and tributaries from the medulla oblongata, pons and inferior cerebellar surface. The venous spaces in the sphenopetroclival area, which are filled anteriorly by blood from the lateral sellar compartment of the cavernous sinus, medially by blood from the basilar plexus, and laterally by blood from the superior petrosal sinus, typically drain into the inferior petrosal sinus (Iaconetta et al 2003).
Sphenoparietal sinus
Understanding the venous anatomy related to the lesser wing of the sphenoid is of clinical importance in the diagnosis, classification, and treatment of dural arteriovenous fistulas in this region. The classic description of the sphenoparietal sinus is that it is a dural venous channel under the lesser wing of the sphenoid bone, lying near its posterior edge (Fig. 27.4). It curves medially to open into the anterior part of the cavernous sinus and receives small veins from the adjacent dura mater and sometimes the frontal ramus of the middle meningeal vein. It may also receive connecting rami, in its middle course, from the superficial middle cerebral vein, and veins from the temporal lobe and the anterior temporal diploic vein. When these connections are well developed, the sphenoparietal sinus is a large channel. It has recently been suggested that the term sphenoparietal sinus should be abandoned on the basis that it is not an anatomical entity, but an artificial combination of two independent meningeal vessels, namely the parietal portion of the anterior branch of the middle meningeal veins and the sinus of the lesser wing of the sphenoid (see Ruiz et al 2004).
Basilar sinus and plexus
The basilar sinus and plexus consist of interconnecting channels between layers of dura mater on the clivus (Fig. 27.4, Fig. 27.8). The basilar venous plexus interconnects the inferior petrosal sinuses and joins the internal vertebral venous plexus. It also usually connects with the cavernous and superior petrosal sinuses at its anterior end.
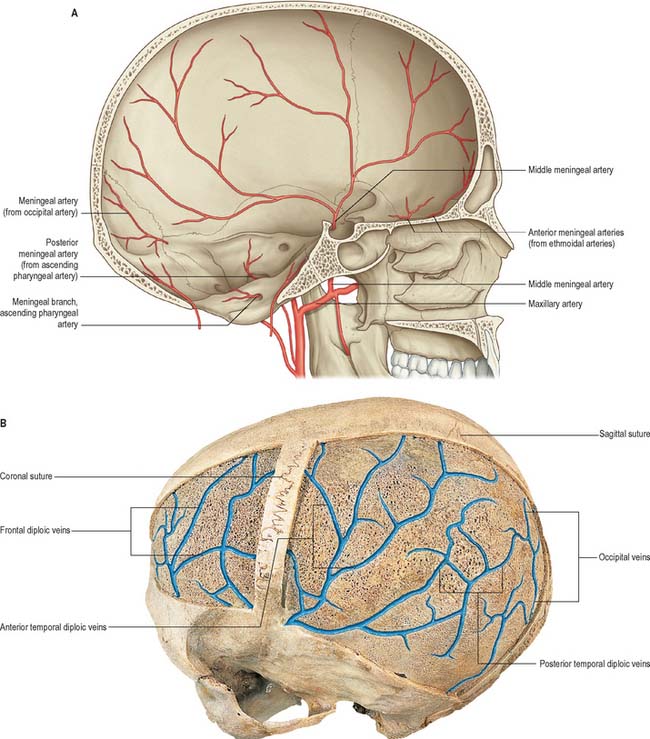
Arterial supply and venous drainage of the cranial dura mater
Despite their names, the cranial meningeal arteries are predominantly periosteal (Fig. 27.10A). Their main targets are bone and haemopoietic marrow, and only very fine arterial branches are distributed to the cranial dura mater per se.
Middle meningeal artery
The middle meningeal artery is the largest of the meningeal arteries. It arises from the first part of the maxillary artery and passes between the roots of the auriculotemporal nerve. It may lie lateral to tensor veli palatini, then enters the cranial cavity through the foramen spinosum and runs in an anterolateral groove on the squamous part of the temporal bone, dividing into frontal and parietal branches. The larger frontal (anterior) branch crosses the greater wing of the sphenoid and enters a groove or canal in the sphenoidal angle of the parietal bone (the sphenoparietal canal). It divides into branches between the dura mater and cranium; some branches ascend to the vertex, others to the occipital region. One ascending branch grooves the parietal bone approximately 15 mm behind the coronal suture, and corresponds approximately to the precentral sulcus (Fig. 27.7). The parietal (posterior) branch curves back on the squamous temporal bone, reaches the lower border of the parietal bone anterior to its mastoid angle and divides to supply the posterior parts of the dura mater and cranium. These branches anastomose with their fellows and with the anterior and posterior meningeal arteries.
Middle meningeal vein (sinus)
The parietal (posterior) trunk of the middle meningeal vein may traverse the foramen spinosum to end in the pterygoid venous plexus. The frontal trunk may also reach this plexus via the foramen ovale, or it may end in the sphenoparietal or cavernous sinus (Fig. 27.4). The middle meningeal vein receives meningeal tributaries and small inferior cerebral veins, and connects with the diploic and superficial middle cerebral veins. It frequently bears arachnoid granulations.
Diploic veins
The diploic veins are large, thin-walled vessels that occupy channels in the diploë of the cranial bones (Fig. 27.10B). Four main trunks are usually described; these are the frontal, anterior and posterior temporal, and occipital diploic veins. The frontal opens into the supraorbital vein and the superior sagittal sinus; the anterior temporal is mainly confined to the frontal bone, and opens into the sphenoparietal sinus, and one of the deep temporal veins through an aperture in the great wing of the sphenoid; the posterior temporal is situated in the parietal bone, and empties into the transverse sinus either through an opening at the mastoid angle of the parietal bone or through the mastoid foramen; and the occipital, the largest of the four, is confined to the occipital bone, and may open externally into the occipital vein, or internally into either the transverse sinus or the confluence of the sinuses.
Emissary veins
The following emissary veins have been recognized. A mastoid emissary vein in the mastoid foramen connects the sigmoid sinus with the posterior auricular or occipital veins. A parietal emissary vein in the parietal foramen connects the superior sagittal sinus with the veins of the scalp (these veins are usually minute and do not appear to connect with veins of the scalp in corrosion casts). The venous plexus of the hypoglossal canal, which is occasionally a single vein, connects the sigmoid sinus and the internal jugular vein. A (posterior) condylar emissary vein connects the sigmoid sinus and veins in the suboccipital triangle via the (posterior) condylar canal. A plexus of emissary veins (venous plexus of foramen ovale) connects the cavernous sinus to the pterygoid plexus via the foramen ovale. Two or three small veins which traverse the foramen lacerum and connect the cavernous sinus and the pharyngeal veins and pterygoid plexus. A vein in the emissary sphenoidal foramen (of Vesalius) connects the cavernous sinus with the pharyngeal veins and pterygoid plexus. The internal carotid venous plexus, which passes through the carotid canal, connects the cavernous sinus and the internal jugular vein. The petrosquamous sinus connects the transverse sinus with the external jugular vein. A vein may traverse the foramen caecum (which is patent in about 1% of adult skulls) and connect nasal veins with the superior sagittal sinus. An occipital emissary vein usually connects the confluence of sinuses with the occipital vein through the occipital protuberance, and also receives the occipital diploic vein. The occipital sinus connects with variably developed veins around the foramen magnum (so-called marginal sinuses) and thus with the vertebral venous plexuses; this pathway provides an alternative venous drainage when the jugular vein is blocked or tied. The ophthalmic veins are potentially emissary, because they connect intracranial to extracranial veins.
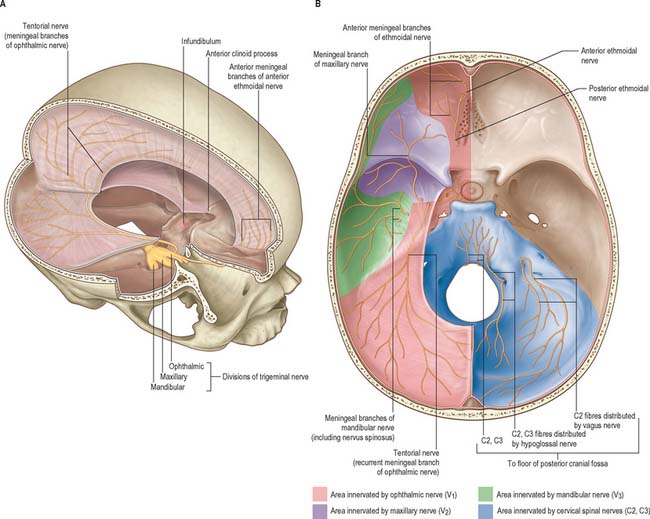
Innervation of the cranial dura mater
The innervation of the cranial dura mater is derived mainly from the three divisions of the trigeminal nerve, the second and third cervical spinal nerves, and the cervical sympathetic trunk (Fig. 27.11). Less well-established meningeal branches have been described arising from the vagus and hypoglossal nerves and possibly from the facial and glossopharyngeal nerves.
In the anterior cranial fossa, the dura is innervated by meningeal branches of the anterior and posterior ethmoidal nerves and anterior filaments of the meningeal rami of the maxillary (nervus meningeus medius) and mandibular (nervus spinosus) divisions of the trigeminal nerve. Nervi meningeus medius and spinosus are, however, largely distributed to the dura of the middle cranial fossa, which also receives filaments from the trigeminal ganglion. The nervus spinosus re-enters the cranium through the foramen spinosum with the middle meningeal artery, and divides into anterior and posterior branches which accompany the main divisions of the artery and supply the dura mater in the middle cranial fossa and, to a lesser extent, the anterior fossa and calvarium. The anterior branch communicates with the meningeal branch of the maxillary nerve; the posterior branch also supplies the mucous lining of the mastoid air cells. The nervus spinosus contains sympathetic postganglionic fibres from the middle meningeal plexus. The nervus tentorii, a recurrent branch of the intracranial portion of the ophthalmic division of the trigeminal supplies the supratentorial falx cerebri and the tentorium cerebelli. Intraoperative mechanical stimulation of the falx may trigger the trigeminocardiac reflex (Bauer et al 2005). The dura in the posterior cranial fossa is innervated by ascending meningeal branches of the upper cervical nerves which enter through the anterior part of the foramen magnum (second and third cervical nerves) and through the hypoglossal canal and jugular foramen (first and second cervical nerves).
Bauer DF, Youkilis A, Schenck C, Turner CR, Thompson BG. The falcine trigeminocardiac reflex: case report and review of the literature. Surg Neurol. 2005;63:143-148.
Browder J, Kaplan HA. Cerebral Dural Sinuses and their Tributaries. Springfield, Illinois: Thomas, 1976.
Describes variations in the form of the superior sagittal and other venous sinuses..
Harris FS, Rhoton AL. Anatomy of the cavernous sinus. A microsurgical study. J Neurosurg. 1976;45:169-180.
Iaconetta G, Fusco M, Samii M. The sphenopetroclival venous gulf: a microanatomical study. J Neurosurg. 2003;99:366-375.
Kaplan HA, Browder J. Neurosurgical consideration of some features of the cerebral dural sinuses and their tributaries. Clin Neurosurg. 1976;23:155-169.
Kida S, Weller RO. Morphology of CSF drainage pathways in man. Raimondi A, editor. Principles of Pediatric Neurosurgery, vol 4. Berlin: Springer, 1994.
Klintworth GK. The ontogeny and growth of the human tentorium cerebelli. Anat Rec. 1967;158:433-442.
Krisht A, Barnett DW, Barrow DL, Bonner G. The blood supply of the intracavernous cranial nerves: an anatomic study. Neurosurgery. 1994;34:275-279.
Ozveren MF, Uchida K, Aiso S, Kawase T. Meningovenous structures of the petroclival region: clinical importance for surgery and intravascular surgery. Neurosurgery. 2002;50:829-836.
Reisch R, Vutskits L, Patonay L, Fries G. The meningohypophyseal trunk and its blood supply to different intracranial structures. An anatomical study. Minim Invasive Neurosurg. 1996;39:78-81.
Ruïz DSM, Fasel JHD, Rüfenacht DA, Gailloud P. The sphenoparietal sinus of Breschet: Does it exist? An anatomic study. Am J Neuroradiol. 2004;25:112-120.
Seoane E, Rhoton ALJr, de Oliveira E. Microsurgical anatomy of the dural collar (carotid collar) and rings around the clinoid segment of the internal carotid artery. Neurosurgery. 1998;42:869-884.
Sheu M, Fauteux G, Chang H, Taylor W, Stopa E, Robinson-Bostom L. Sinus pericranii: dermatologic considerations and literature review. J Am Acad Dermatol. 2002;46:934-941.
Tekdemir I, Tuccar E, Aslan A, et al. The jugular foramen. A comparative radioanatomic study. Surg Neurol. 1998;50:557-562.
Tekdemir I, Tuccar E, Cubuk HE, Ersoy M, Elhan A, Deda H. Branches of the intracavernous internal carotid artery and the blood supply of the intracavernous cranial nerves. Ann Anat. 1998;180:343-348.
Umansky F, Valarezo A, Elidan J. The superior wall of the cavernous sinus: a microanatomical study. J Neurosurg. 1994;81:914-920.
Watanabe A, Nagaseki Y, Ohkubo S, Ohhashi Y, Horikoshi T, Nishigaya K, Nukui H. Anatomical variations of the ten triangles around the cavernous sinus. Clin Anat. 2003;16:9-14.
Williams JL. Rowe and Williams’ Maxillofacial Injuries. Edinburgh: Churchill Livingstone, 1994.
Yasuda A, Campero A, Martins C, Rhoton ALJr, Ribas GC. The medial wall of the cavernous sinus: microsurgical anatomy. Neurosurgery. 2004;55:179-189.
Zhang ET, Inman CBE, Weller RO. Interrelationships of the pia mater and the perivascular (Virchow-Robin) spaces in the human cerebrum. J Anat. 1990;170:111-123.