Intestinal Nematodes (Roundworms)
1. Describe the distinguishing morphologic characteristics and basic life cycle (vectors, hosts, and stages of infectivity) for each of the parasites listed.
2. Define and identify the following parasitic structures when appropriate: mammillated ovum, gravid, rhabditiform larvae, buccal capsule, esophagus, genital primordia, polar hyaline plugs, copulatory bursa, embryonated egg, cutting plates, and filariform larvae.
3. Describe the diseases and mechanism of pathogenicity including route of transmission for each of the species listed.
4. Differentiate Ascaris lumbricoides adult male and female worms.
5. Define and differentiate direct versus indirect life cycle as related to nematodes and the routes of transmission including autoinfection and hyperinfections.
6. Identify and differentiate the characteristic morphologies and eggs for A. lumbricoides, E. vermicularis, and T. trichiura.
7. Compare clinical signs and symptoms, morphologic characteristics, and identification of hookworm’s rhabditiform larvae for Ancylostoma duodenale and Necator americanus.
8. Compare and contrast the morphologic characteristics and identification of the larval forms of Strongyloides stercoralis.
9. List the various methods used to diagnosis intestinal nematode infections.
10. Identify the appropriate intestinal nematodes where the following techniques are useful and explain the principle for each including the Baermann concentration method, agar culture, and Harada-Mori filter paper method for the recovery of intestinal nematodes.
Ascaris Lumbricoides
General Characteristics
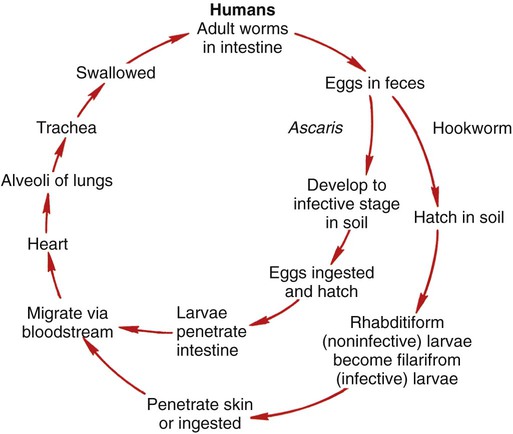
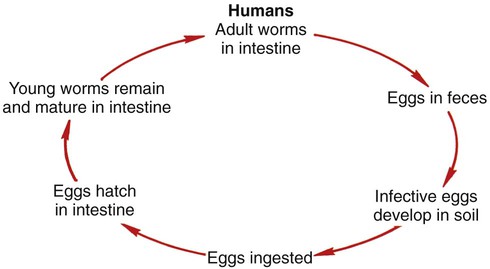
Ascaris lumbricoides is the most common and the largest roundworm. The parasite has a worldwide distribution with higher prevalence in the tropical regions. Eggs are ingested and hatch in the duodenum, penetrate the intestinal wall, and migrate to the hepatic portal circulation. The adult worms live and reproduce in the lumen of the small intestine. The ovum is a thick, oval mammillated (outer protrusions) and embryonated egg. The eggs are passed in the feces and become infective 2 to 6 weeks following deposition, depending on the environment. The general life cycle is outlined in Figure 51-1. A. lumbricoides life cycle is classified as an indirect life cycle; transmission is not via a direct route from one host to the next.
Pathogenesis and Spectrum of Disease
Many A. lumbricoides infections are asymptomatic. The presentation of symptoms correlates with the length of infection, the number of worms present, and the overall health of the host. Intestinal symptoms range from mild to severe intestinal obstruction. Some patients will develop pulmonary symptoms and present with immune-mediated hypersensitivity pneumonia. The worms may cause an immune condition known as Löffler’s syndrome characterized by peripheral eosinophilia. See Table 51-1 for a summarized detail of associated diseases.
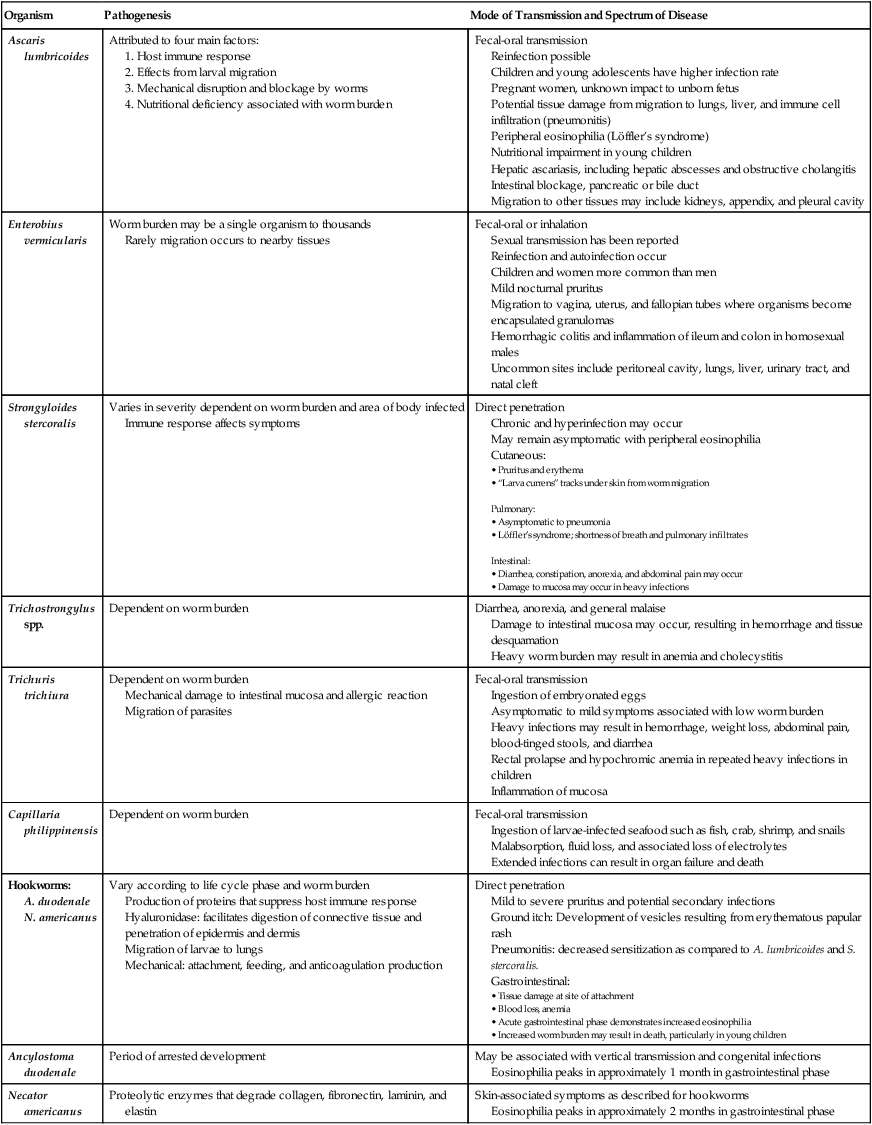
TABLE 51-1
Pathogenesis and Spectrum of Associated Diseases
| Organism | Pathogenesis | Mode of Transmission and Spectrum of Disease |
| Ascaris lumbricoides | Attributed to four main factors: |
Reinfection possible
Children and young adolescents have higher infection rate
Pregnant women, unknown impact to unborn fetus
Potential tissue damage from migration to lungs, liver, and immune cell infiltration (pneumonitis)
Peripheral eosinophilia (Löffler’s syndrome)
Nutritional impairment in young children
Hepatic ascariasis, including hepatic abscesses and obstructive cholangitis
Intestinal blockage, pancreatic or bile duct
Migration to other tissues may include kidneys, appendix, and pleural cavity
Rarely migration occurs to nearby tissues
Sexual transmission has been reported
Reinfection and autoinfection occur
Children and women more common than men
Mild nocturnal pruritus
Migration to vagina, uterus, and fallopian tubes where organisms become encapsulated granulomas
Hemorrhagic colitis and inflammation of ileum and colon in homosexual males
Uncommon sites include peritoneal cavity, lungs, liver, urinary tract, and natal cleft
Immune response affects symptoms
Chronic and hyperinfection may occur
May remain asymptomatic with peripheral eosinophilia
Cutaneous:
Pulmonary:
Intestinal:
Damage to intestinal mucosa may occur, resulting in hemorrhage and tissue desquamation
Heavy worm burden may result in anemia and cholecystitis
Mechanical damage to intestinal mucosa and allergic reaction
Migration of parasites
Ingestion of embryonated eggs
Asymptomatic to mild symptoms associated with low worm burden
Heavy infections may result in hemorrhage, weight loss, abdominal pain, blood-tinged stools, and diarrhea
Rectal prolapse and hypochromic anemia in repeated heavy infections in children
Inflammation of mucosa
Ingestion of larvae-infected seafood such as fish, crab, shrimp, and snails
Malabsorption, fluid loss, and associated loss of electrolytes
Extended infections can result in organ failure and death
A. duodenale
N. americanus
Production of proteins that suppress host immune response
Hyaluronidase: facilitates digestion of connective tissue and penetration of epidermis and dermis
Migration of larvae to lungs
Mechanical: attachment, feeding, and anticoagulation production
Mild to severe pruritus and potential secondary infections
Ground itch: Development of vesicles resulting from erythematous papular rash
Pneumonitis: decreased sensitization as compared to A. lumbricoides and S. stercoralis.
Gastrointestinal:
Eosinophilia peaks in approximately 1 month in gastrointestinal phase
Eosinophilia peaks in approximately 2 months in gastrointestinal phase
Laboratory Diagnosis
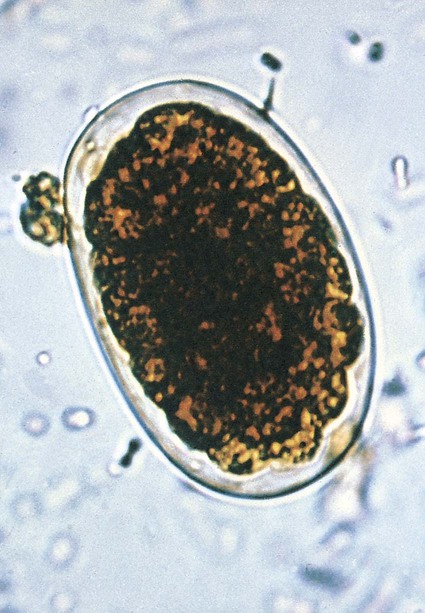
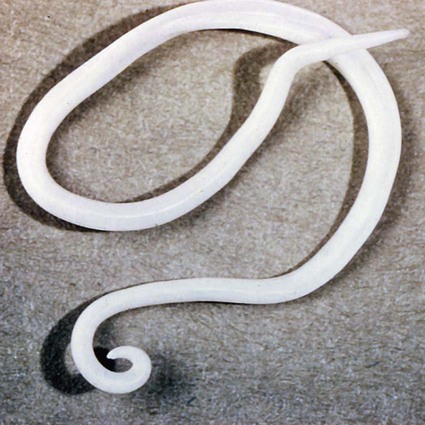
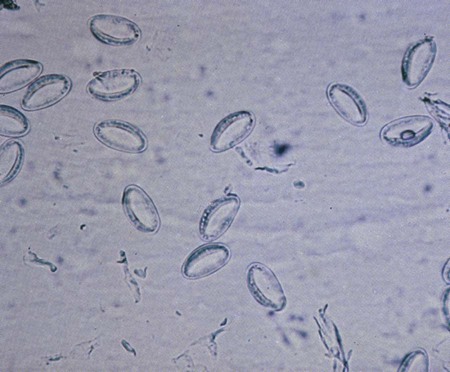
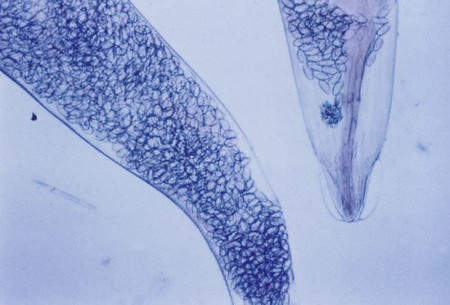
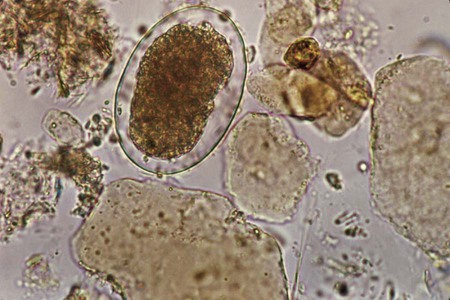
Female worms have an extremely high daily output of eggs, making diagnosis relatively easy through the identification of eggs in feces. The large, broadly oval mammillated ova are typically stained brown from bile (Figure 51-2). Some eggs will be decorticated, or lacking the mammillated outer cover. Infertile eggs may be oval or irregular shaped with a thin shell and containing internal granules. Adult worms may also be identified in feces. The male is smaller (15 to 31 cm) with a curved posterior end (Figure 51-3) and contains three well-characterized lips. Larvae may be found in sputum or gastric aspirates as a result of larval migration during development within the human host.
Enterobius Vermicularis
General Characteristics
Enterobius vermicularis (pinworm) is distributed worldwide and commonly identified in group settings of children ages 5 to 10 years. The life cycle is considered direct; transmission occurs from an infected host to another individual (Figure 51-4). During the night, the mature female worm migrates out of the anus of the infected host and lays eggs in the perianal region. The embryonated eggs will mature and a third-stage larva stage develops, resulting in infectivity within hours. Transmission occurs by ingestion or inhalation of eggs. Reinfection may also occur when the eggs hatch and larvae return to the intestine where they mature.
Pathogenesis and Spectrum of Disease
Infections with E. vermicularis are typically asymptomatic. The most common complaint is perianal pruritus (itching) and resultant restless sleep. Occasionally, the parasite may migrate to other nearby tissues, causing pelvic, cervical, or peritoneal granulomas. See Table 51-1 for a summarized detail of associated diseases.
Laboratory Diagnosis
Diagnosis is typically by microscopic identification of the characteristic flat-sided ovum (Figure 51-5). The eggs are collected using a sticky paddle or cellophane tape pressed against the perianal region. Eggs are not typically identified in feces, although they may occasionally be found in a stool specimen. Although adult pinworms may be visible, they can be easily confused with small pieces of thread. The female worm measures 8 to 13 mm long with a pointed “pin” shaped tail. In gravid females, almost the entire body will be filled with eggs (Figure 51-6). The males measure only 2 to 5 mm in length, die following fertilization, and may be passed in feces.
Strongyloides Stercoralis
General Characteristics
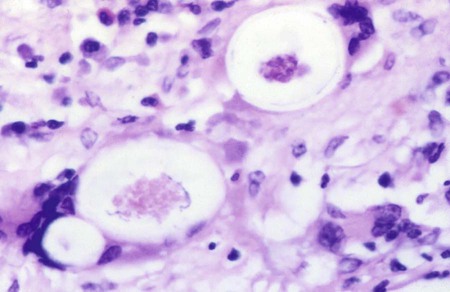
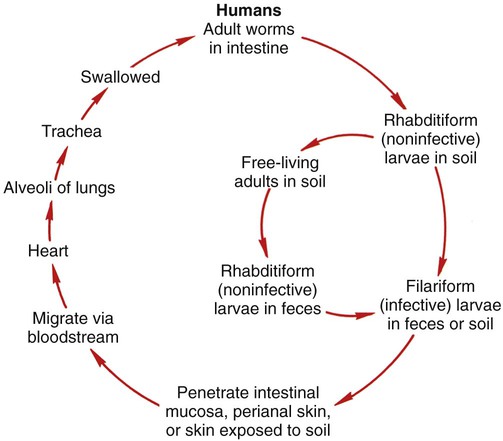
S. stercoralis, commonly referred to as the threadworm, may inhabit the intestine or exist as a free-living organism in the soil. The life cycle can be classified as direct, indirect (free-living phase), or autoinfective (Figure 51-7). The filariform (infective larvae) penetrate the skin and migrate via the circulatory system to the heart and lungs. The organism enters the bronchial tree and then is swallowed, where it lives in the digestive tract and matures into an adult worm. In the intestine the filariform larvae may also penetrate the mucosa, resulting in autoinfection. The female worm produces eggs by parthenogenesis (a form of asexual reproduction where growth and development occur without fertilization), because parasitic adult male worms are nonexistent. Within the indirect life cycle, the rhabditiform (noninfective) larvae develop into mature males and egg-producing females (Figure 51-8). The free-living life cycle may revert to the production of infective larvae at any time.
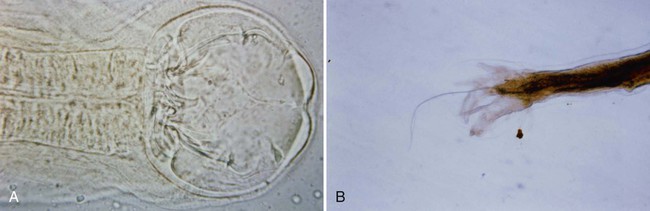
Laboratory Diagnosis
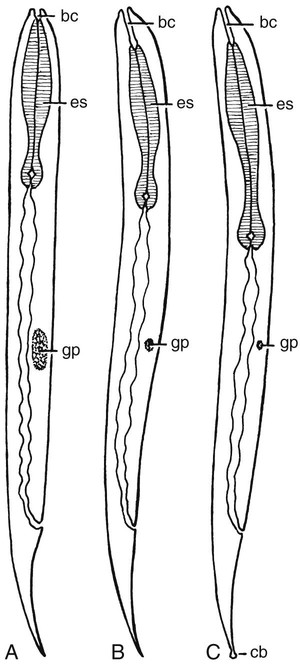
The rhabditiform larva is the primary diagnostic stage for strongyloidiasis in humans through microscopic examination of stool. The larvae are 250 to 300 µm long with a short buccal capsule, a large bulb on the esophagus, and a prominent genital primordium (Figure 51-9). The filariform larvae are larger (up to 500 µm) and have a notched tail with an esophageal to intestinal ratio of 1 : 1. The eggs, which are rarely identified, are segmented with a thin shell.
Trichostrongylus spp.
General Characteristics
Trichuris Trichiura
General Characteristics
Pathogenesis and Spectrum of Disease
Pathogenesis and severity of the disease are closely related to the worm burden. The lack of symptoms is related to the life cycle that does not include a tissue migration stage, as is seen in other nematode infections. Infections range from mild, very low worm burden, to severe infections with bleeding and weight loss in heavy worm infestations. The characteristic whiplike worm buries its threadlike anterior into the intestinal mucosa and feeds on tissue secretions, causing an inflammatory reaction and peripheral eosinophilia. See Table 51-1 for a summarized detail of associated diseases.
Laboratory Diagnosis
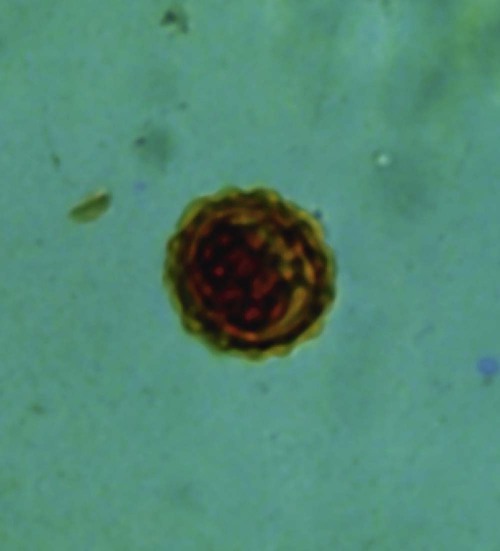
Diagnosis is typically from the identification of eggs and rarely the adult worm within the feces. An adult female may produce up to 20,000 eggs per day. However, during the lengthy development of mature worms within the intestine, there may be no shedding of eggs for up to 3 months. Eggs appear as brown barrel-shaped structures. They are unembryonated and contain a thick wall with hyaline polar plugs at each end (Figure 51-11). The adult female worm ranges in size from 35 to 50 mm and demonstrates a gradually increasing width from anterior to posterior, with a straight end (Figure 51-12). The adult male ranges in size from 30 to 45 mm and demonstrates the same broadening morphology with a coiled posterior end.
Capillaria Philippinensis
General Characteristics
Pathogenesis and Spectrum of Disease
Symptoms vary with the level of worm burden. The larvae are ingested and reside in the small intestine where they burrow into the mucosa. Because of the mechanical insertion into the intestinal wall, patients lose weight rapidly as a result of malabsorption and fluid loss. Long-term infections lasting weeks to months may result in death attributable to a severe loss of electrolytes, particularly potassium (hypokalemia), and associated organ failure. See Table 51-1 for a summarized detail of associated diseases.
Hookworms
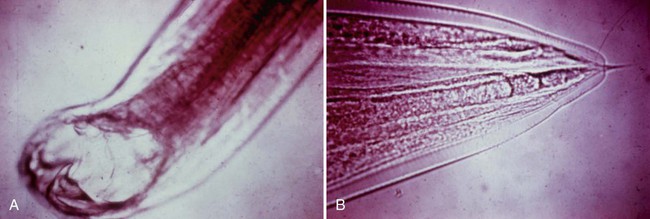
Hookworms are known to have a worldwide distribution with two species known to infect humans, Ancylostoma duodenale (Figure 51-13) and Necator americanus (Figure 51-14). They are the second most common helmintic infection reported in humans. The eggs and rhabditiform larvae of the two species are indistinguishable. Differentiation of the species is based on the morphology of the buccal capsule and the adult male copulatory bursa (see Figure 51-14, B).
Ancylostoma Duodenale
General Characteristics
A. duodenale, Old World hookworm, is prevalent in southern Europe, northern Africa, Southeast Asia, and South America. The adult male tends to be larger than the adult male of N. americanus. They attach to the intestinal mucosa by well-developed mouthparts, especially teeth (see Figure 51-13).
Necator Americanus
General Characteristics
N. americanus, New World hookworm, is prevalent in Africa, Southeast Asia, and South and Central America as well as the southeastern United States. They attach to the intestinal mucosa by well-developed cutting plates (see Figure 51-14, A).
Laboratory Diagnosis
Hookworms are typically diagnosed by the presence of eggs or rhabditiform larvae found in stool specimens. The eggs and larvae of the two species are indistinguishable. The eggs are oval and thin-shelled and contain a clearly visible four- to eight-cell stage embryo. There is a characteristic clear space between the shell and the developing embryo (see Figure 51-14). Recovery and identification of eggs on direct smear or from concentration methods is recommended. Eggs may appear distorted on permanently stained smears. The rhabditiform larvae are typically 250 to 300 µm with a long buccal capsule and an inconspicuous genital primoridum (Figures 51-15 and 51-16). The larger filariform larvae are approximately 500 µm, with a pointed tail and a esophageal to intestinal ratio of 1 : 4. Both the rhabditiform and filariform larvae must be differentiated from S. stercoralis.