Limited to bowel ± mesenteric nodes

 in the mesentery. The metastases subsequently resulted in an intussusception.
in the mesentery. The metastases subsequently resulted in an intussusception.
 . One of the bowel wall metastases served as the lead point of the intussusception.
. One of the bowel wall metastases served as the lead point of the intussusception.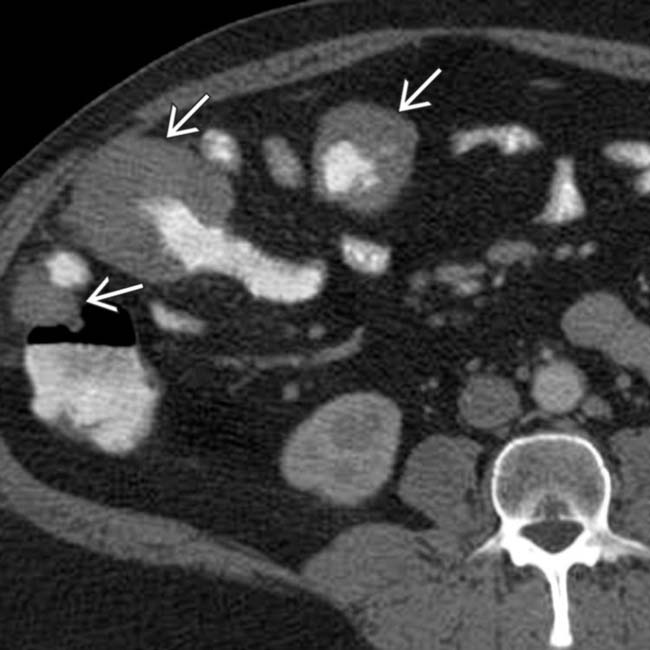
 .
.
 and encasement of the mesenteric vessels, but no bowel or vascular obstruction. Multifocal masses of lymphoma
and encasement of the mesenteric vessels, but no bowel or vascular obstruction. Multifocal masses of lymphoma  are also seen.
are also seen.IMAGING
Radiographic Findings
• Barium-enhanced fluoroscopic studies (upper GI, SB follow-through, barium enema)
CLINICAL ISSUES
Presentation
Natural History & Prognosis
• Intestinal metastases

 and lymph nodes
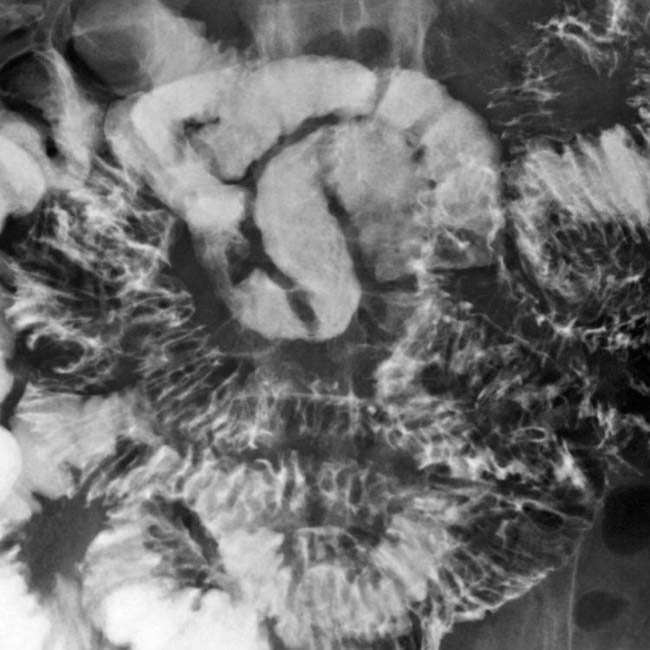
and lymph nodes  . The gastric wall metastases may ulcerate, leading to the classic “target” or bull’s-eye appearance.
. The gastric wall metastases may ulcerate, leading to the classic “target” or bull’s-eye appearance.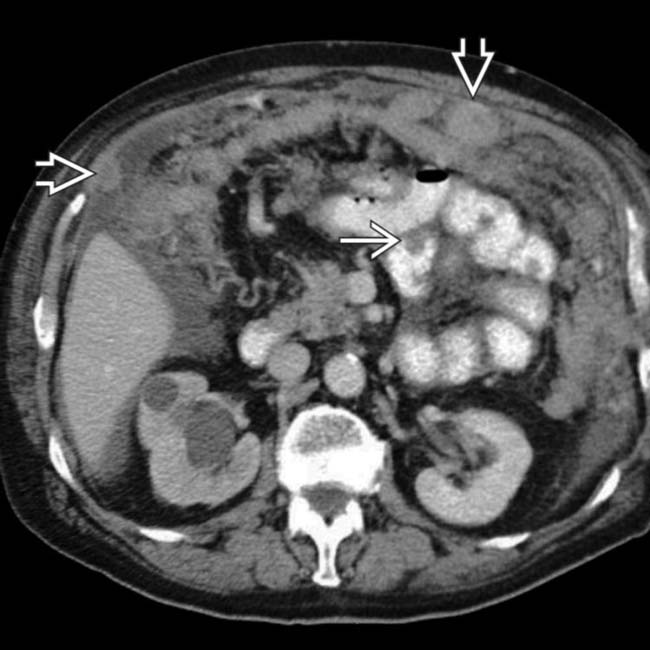
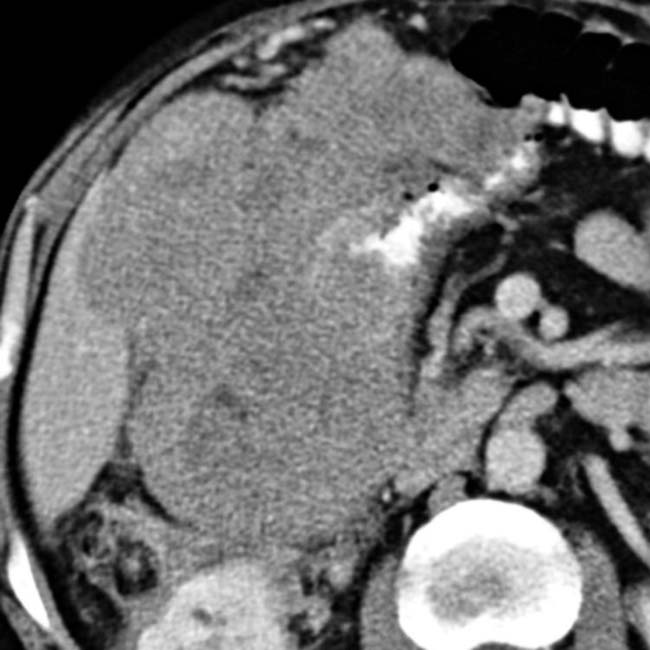
 , lymph nodes, and omentum
, lymph nodes, and omentum  , with both nodular and diffuse metastases seen. The right ureter was obstructed due to a ureteral metastasis.
, with both nodular and diffuse metastases seen. The right ureter was obstructed due to a ureteral metastasis.
 enveloping, but not obstructing, small bowel and mesenteric vessels.
enveloping, but not obstructing, small bowel and mesenteric vessels.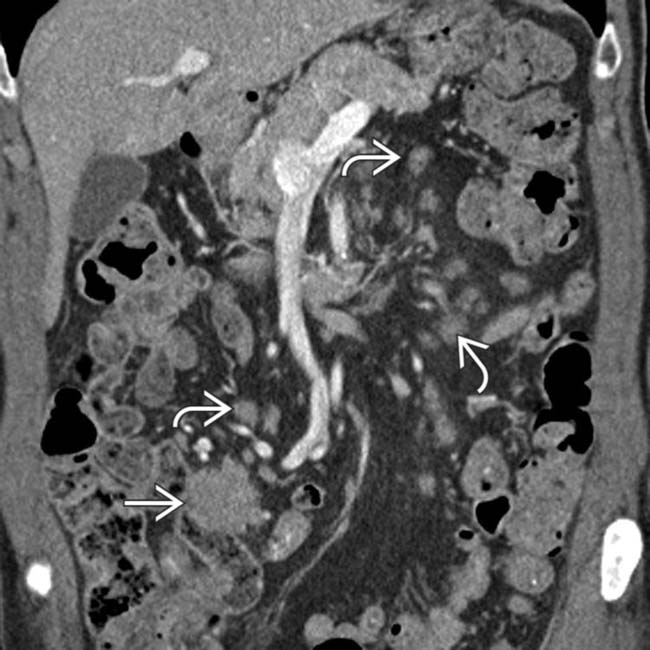
 along with extensive mesenteric lymphadenopathy
along with extensive mesenteric lymphadenopathy  . Non-Hodgkin lymphoma was confirmed.
. Non-Hodgkin lymphoma was confirmed.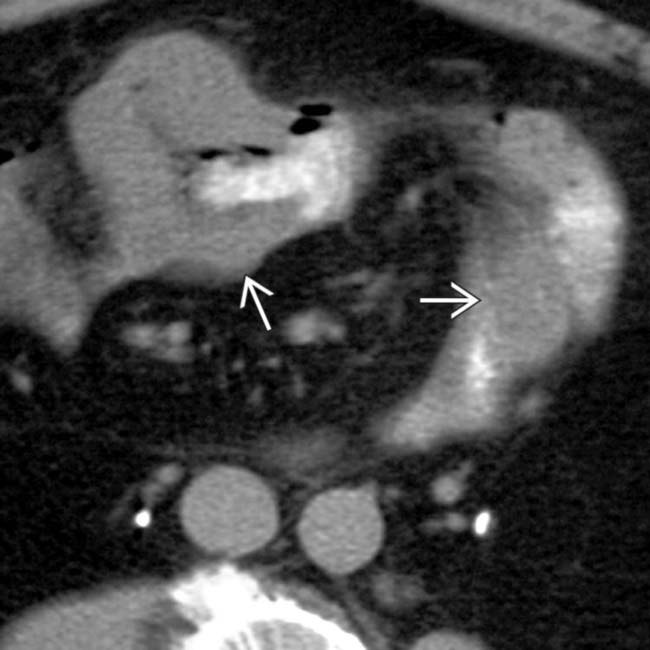
 with aneurysmal dilation of the small intestine lumen; however, no intestinal obstruction is seen.
with aneurysmal dilation of the small intestine lumen; however, no intestinal obstruction is seen.
 . An intramural mass is constricting the lumen of the duodenum. At surgery, metastatic breast cancer was confirmed.
. An intramural mass is constricting the lumen of the duodenum. At surgery, metastatic breast cancer was confirmed.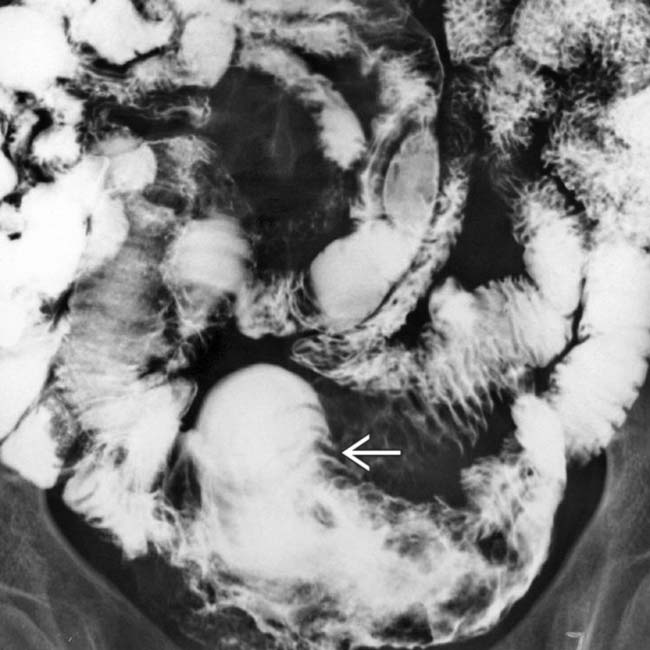
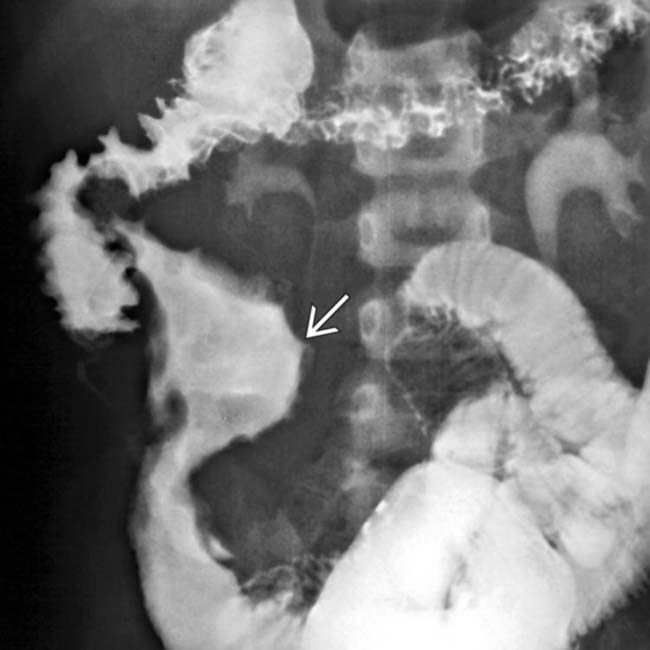
 and mucosal destruction of the distal SB segment in this patient with melanoma.
and mucosal destruction of the distal SB segment in this patient with melanoma.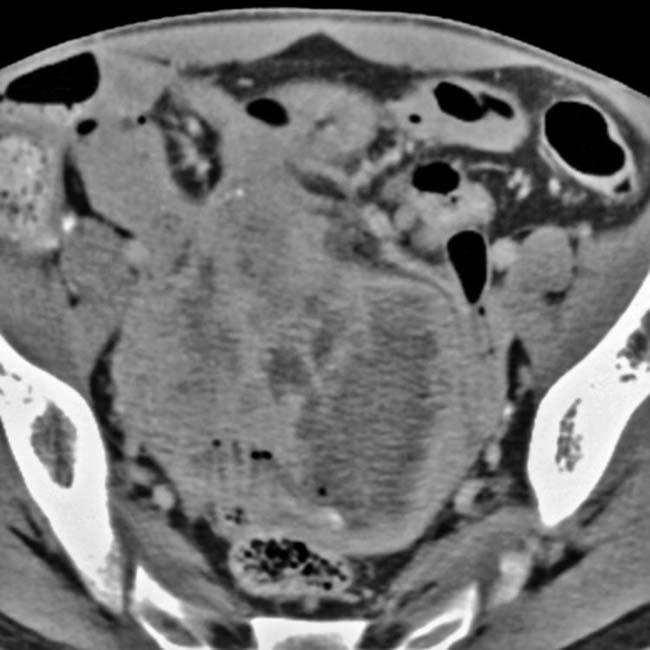
 of the lumen of the terminal ileum along with mesenteric mass effect in this patient with lymphoma.
of the lumen of the terminal ileum along with mesenteric mass effect in this patient with lymphoma.























































































 with distorted mucosa due to melanoma.
with distorted mucosa due to melanoma.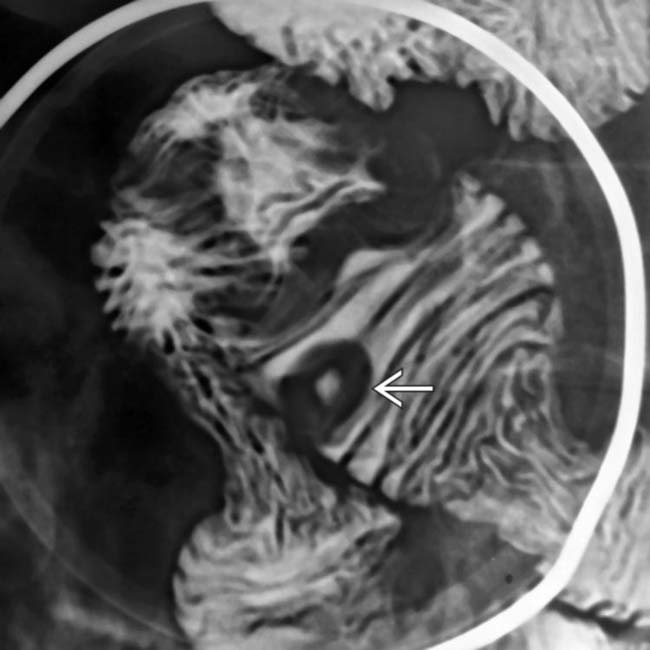
 due to metastatic melanoma.
due to metastatic melanoma.