Chapter 13 Intervertebral Discography
Concepts of discography
Discography is a procedure that is used to characterize the pathoanatomy/architecture of the intervertebral disc and to determine whether it is a source of chronic spinal pain. It consists of the opacification of the nucleus pulposus of an intervertebral disc to render it visible under radiographs. An implicitly invasive diagnostic test, discography should be used only in those patients with chronic spinal pain in whom one suspects a discogenic etiology [1].
The commonly practiced technical and evaluative components of discography are as follows:
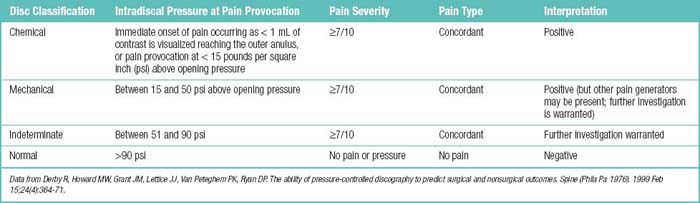
The following four classes of discs are identified during a pain-provocative discogram:
Terms Related to Discography
The following terms are used in discography:
Concepts of internal disc disruption
In 1970, Crock and associates [2] described internal disc disruption (IDD) as a condition marked by alteration in the internal structure and metabolic functions of the intervertebral disc, usually preceded by injuries. Anular tears, including radial and circumferential tears, are the major forms of IDD.
The natural history of untreated single-level IDD confirmed by discography over 3 years was described in a study by Smith and associates [3], who summarized outcomes as follows:
Indications
Cervical discography is indicated for patients with the following features:
 Patients with persistent neck and/or cervical radicular pain in whom traditional diagnostic modalities, such as magnetic resonance imaging, CT, and electromyography (EMG), have failed to identify the cause of the pain.
Patients with persistent neck and/or cervical radicular pain in whom traditional diagnostic modalities, such as magnetic resonance imaging, CT, and electromyography (EMG), have failed to identify the cause of the pain. Patients in whom findings identified on traditional diagnostic modalities, such as bulging cervical discs, are equivocal (to determine whether such abnormalities are, in fact, responsible for the pain).
Patients in whom findings identified on traditional diagnostic modalities, such as bulging cervical discs, are equivocal (to determine whether such abnormalities are, in fact, responsible for the pain). Patients who have previously undergone fusion of the cervical spine (to help determine whether levels above and below the fusion are causing persistent pain).
Patients who have previously undergone fusion of the cervical spine (to help determine whether levels above and below the fusion are causing persistent pain). Patients in whom traditional imaging techniques cannot distinguish recurrent disc herniation from scar tissue.
Patients in whom traditional imaging techniques cannot distinguish recurrent disc herniation from scar tissue.The following groups of patients should undergo thoracic discography:
 Patients with persistent thoracic radicular or myelopathic pain in whom traditional diagnostic modalities, such as magnetic resonance imaging, CT, and electromyography, have failed to identify the cause.
Patients with persistent thoracic radicular or myelopathic pain in whom traditional diagnostic modalities, such as magnetic resonance imaging, CT, and electromyography, have failed to identify the cause. Patients in whom equivocal findings, such as bulging thoracic discs, are identified by traditional diagnostic modalities (to determine whether such abnormalities are, in fact, responsible for the pain).
Patients in whom equivocal findings, such as bulging thoracic discs, are identified by traditional diagnostic modalities (to determine whether such abnormalities are, in fact, responsible for the pain). Patients who are to undergo instrumentation and fusion of the thoracic spine (in whom discography may help identify which levels need to be fused).
Patients who are to undergo instrumentation and fusion of the thoracic spine (in whom discography may help identify which levels need to be fused). Patients who have previously undergone instrumentation and fusion of the thoracic spine (to help determine whether levels above and below the fusion are responsible for persistent pain).
Patients who have previously undergone instrumentation and fusion of the thoracic spine (to help determine whether levels above and below the fusion are responsible for persistent pain). Patients in whom recurrent disc herniation cannot be distinguished from scar tissue with traditional imaging techniques.
Patients in whom recurrent disc herniation cannot be distinguished from scar tissue with traditional imaging techniques.Indications for lumbar discography are as follows:
 Further evaluation of demonstrably abnormal discs (to help assess the extent of abnormality or correlation of the abnormality with the clinical symptoms; such symptoms include recurrent pain from a previously operated disc and lateral disc herniation.
Further evaluation of demonstrably abnormal discs (to help assess the extent of abnormality or correlation of the abnormality with the clinical symptoms; such symptoms include recurrent pain from a previously operated disc and lateral disc herniation. Patients with persistent, severe symptoms in whom other diagnostic tests have failed to clearly confirm that a suspected disc is the source of pain.
Patients with persistent, severe symptoms in whom other diagnostic tests have failed to clearly confirm that a suspected disc is the source of pain. Assessment of patients in whom surgical intervention has failed, to determine whether there is painful pseudarthrosis or a symptomatic disc in a posteriorly fused segment and to help evaluate possible recurrent disc herniation.
Assessment of patients in whom surgical intervention has failed, to determine whether there is painful pseudarthrosis or a symptomatic disc in a posteriorly fused segment and to help evaluate possible recurrent disc herniation. Assessment of discs before fusion to determine whether (1) the discs within the proposed fusion segment are symptomatic and (2) discs adjacent to this segment are normal.
Assessment of discs before fusion to determine whether (1) the discs within the proposed fusion segment are symptomatic and (2) discs adjacent to this segment are normal. Assessment of candidates for minimally invasive surgical intervention to confirm a contained disc herniation or to investigate dye distribution pattern before chemonucleolysis or percutaneous procedures.
Assessment of candidates for minimally invasive surgical intervention to confirm a contained disc herniation or to investigate dye distribution pattern before chemonucleolysis or percutaneous procedures.Crock HV [2] have offered the following indications for lumbar discography:
 Evaluation of patients with unremitting spinal pain, with or without extremity pain, that has lasted longer than 4 months and has been unresponsive to conservative therapy.
Evaluation of patients with unremitting spinal pain, with or without extremity pain, that has lasted longer than 4 months and has been unresponsive to conservative therapy. Evaluation of patients with persistent symptoms in whom other diagnostic tests have failed to clearly confirm that a suspected disc is the source of pain.
Evaluation of patients with persistent symptoms in whom other diagnostic tests have failed to clearly confirm that a suspected disc is the source of pain. Evaluation of persistent pain in the postoperative patient whose symptoms may be arising from intervertebral disc degeneration, recurrent herniation, or pseudarthrosis of a spinal fusion.
Evaluation of persistent pain in the postoperative patient whose symptoms may be arising from intervertebral disc degeneration, recurrent herniation, or pseudarthrosis of a spinal fusion. To determine the number of levels to be fused in spinal surgery and/or to identify the primary symptomatic disc.
To determine the number of levels to be fused in spinal surgery and/or to identify the primary symptomatic disc. In the patient who prima facie has satisfied the criteria for treatment by intradiscal electrothermal therapy (IDET), in whom pain is provoked to detect discogenic pain. In such a patient, CT discography may be undertaken to assess disc morphology to determine whether or not an IDET electrode can be navigated in the disc and, if so, where it should be placed.
In the patient who prima facie has satisfied the criteria for treatment by intradiscal electrothermal therapy (IDET), in whom pain is provoked to detect discogenic pain. In such a patient, CT discography may be undertaken to assess disc morphology to determine whether or not an IDET electrode can be navigated in the disc and, if so, where it should be placed.Contraindications
Absolute contraindications to intervertebral discography are as follows:
Relative contraindications to intervertebral discography are as follows:
Preoperative preparation
The characteristic patient complaints indicating discography are as follows:
 Unexplained cause or undetermined level of suspected discogenic axial or radicular pain that needs interventional pain management
Unexplained cause or undetermined level of suspected discogenic axial or radicular pain that needs interventional pain managementMedication given before discography consists of antibiotics for prophylaxis against infection (Tables 13.1 and 13.2).
Table 13.1 Dosages of Antibiotics Recommended for Prophylaxis in Patients Undergoing Spinal Surgery
| Antibiotic | First Dose in Adults (In Children) | Subsequent Doses in Adults (In Children)* |
|---|---|---|
| Cephradine | 1 g (25 mg/kg) | 500 mg (12.5 mg/kg) |
| Cefazolin | 1 g (25 mg/kg) | 500 mg (12.5 mg/kg) |
| Cefuroxime | 1.5 g (25 mg/kg) | 750 mg (12.5 mg/kg) |
| Cefamandole | 1 g (25 mg/kg) | 500 mg (12.5 mg/kg) |
| Vancomycin | 1 g (15 mg/kg) | 500 mg (7.5 mg/kg) |
| Teicoplanin | 800 mg (10 mg/kg) | 400 mg (5 mg/kg) |
| Gentamicin | 3 mg/kg (2 mg/kg) | 1.5 mg/kg (1.5 mg/kg) |
| Clindamycin | 600 mg (10 mg/kg) | 300 mg (5 mg/kg) |
* Administered at 4-hour intervals (8-hour intervals for glycopeptides and gentamicin) for surgical procedures lasting ≥4 hours (or ≥8 hours if patient is receiving a glycopeptide/aminoglycoside regimen). Gentamicin and vancomycin must be used with caution in patients who have impaired renal function or who are otherwise at risk of toxicity from these drugs. From Brown EM, Pople IK, de Louvois J, Hedges A, Bayston R, Eisenstein SM, Lees P. British Society for Antimicrobial Chemotherapy Working Party on Neurosurgical Infections. Spine update: prevention of postoperative infection in patients undergoing spinal surgery. Spine (Phila Pa 1976). 2004;29(8):938-45.
Table 13.2 Antibiotic Penetration into Discs
| Antibiotic | Experimental subject |
|---|---|
| Clindamycin | Rabbit |
| Gentamicin | Human and rabbit |
| Tobramycin | Rabbit |
| Vancomycin | Rabbit |
| Teicoplanin | Rabbit |
| Vancomycin | Rabbit |
Procedures
Cervical Discography
Cervical discography is performed as follows:
Thoracic Discography
Thoracic discography is performed as follows:
Lumbar Discography
Lumbar discography is performed as follows:
Related anatomy and physiology
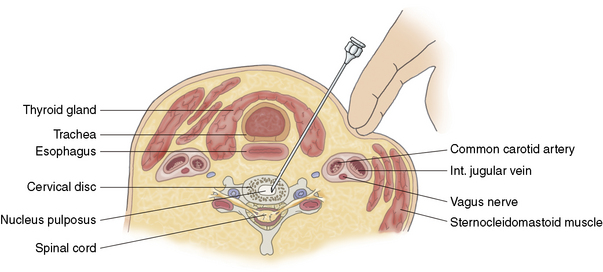
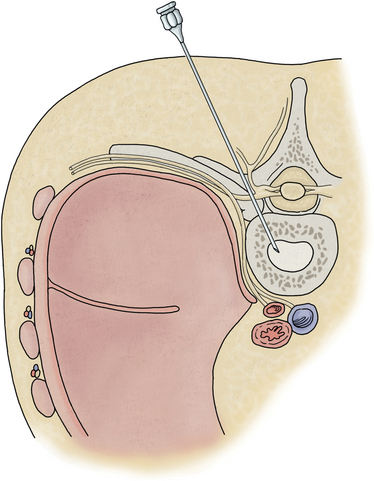
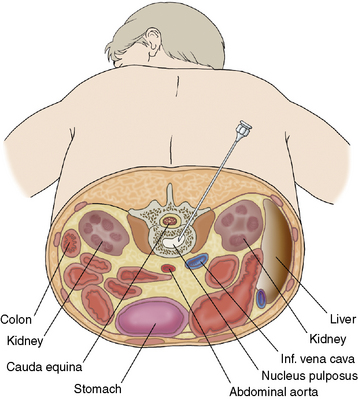
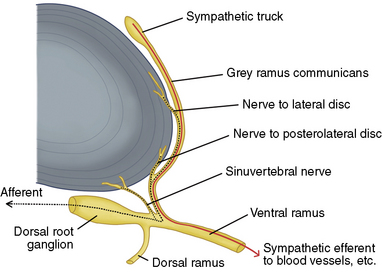
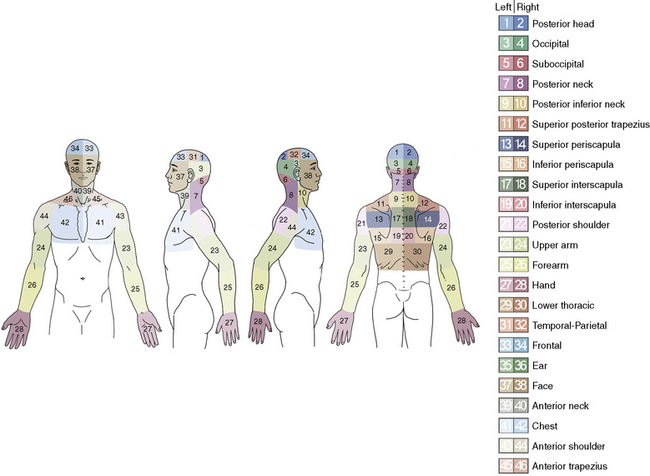
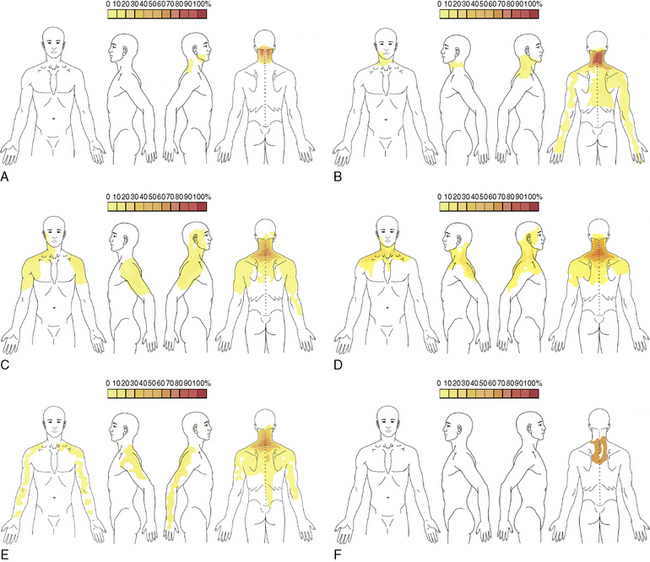
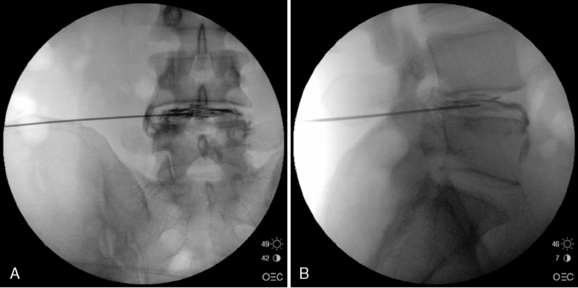
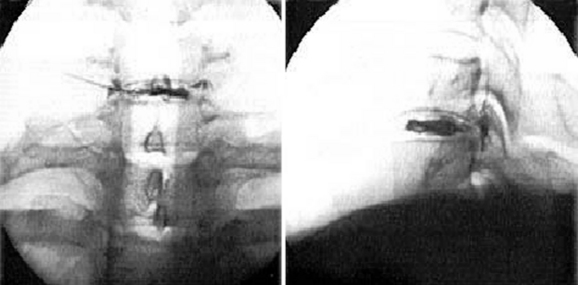
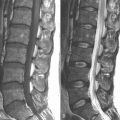
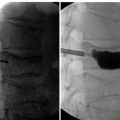
The anatomy and physiology related to the performance of discography are listed in Table 13.3 and illustrated in Figures 13-1 and 13-3 through 13-6.
| Discography Region | Anatomic Structures Visualized |
|---|---|
| Cervical |
Interpretation of discography
Scoring System for Response to Disc Stimulation
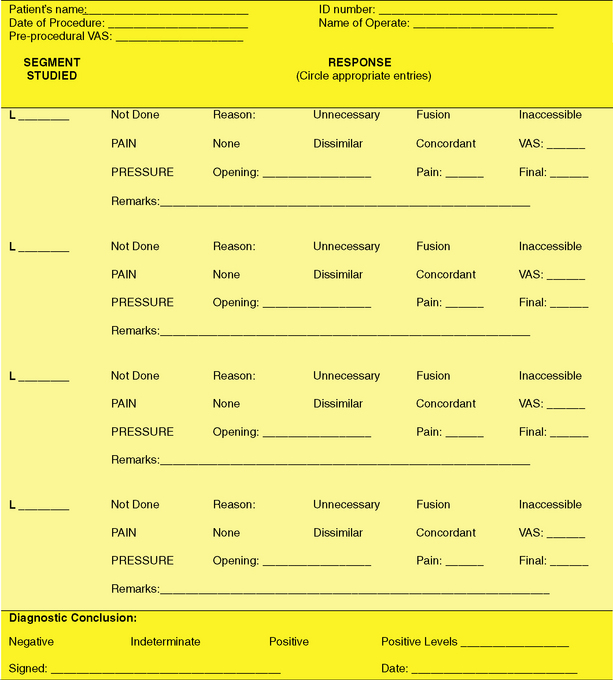
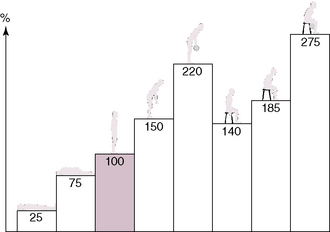
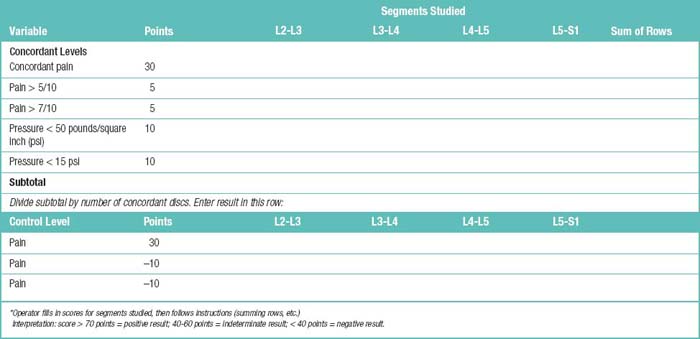
For practitioners who are uncertain whether a particular pattern of response to disc stimulation constitutes a positive result, a scoring system may be used to derive a numerical score that can then be interpreted. This scoring system does not replace clinical judgment; it is designed to assist in the interpretation of borderline or confusing responses. The scoring system requires a table to be completed (Table 13.4; see Fig. 13-2).
Other
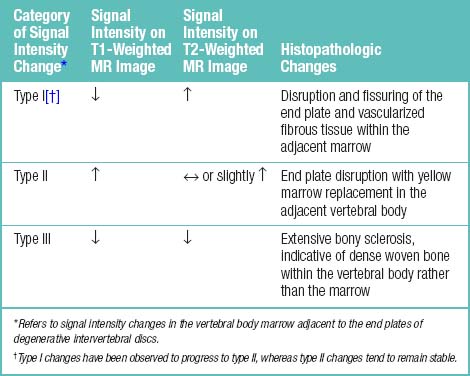
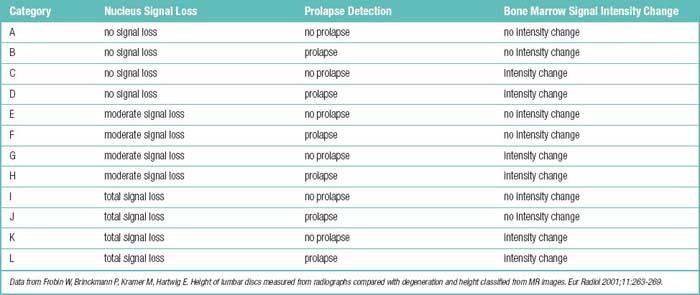
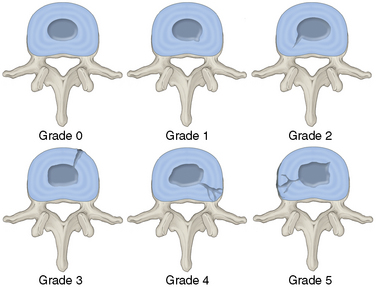
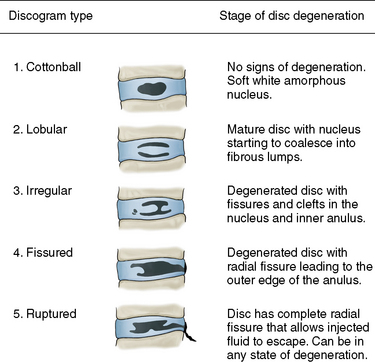
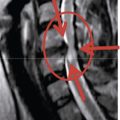
Other classification systems and criteria for rating degenerative disc disease are presented in Tables 13.5 to 13.10 and Figures 13-7 to 13-12.
| Unequivocal discogenic pain |
.
.
.
Data from Bogduk B: Proposed discography standards. ISIS Newsletter, Volume 2, Number 1. Daly City, California, International Spinal Injection Society, 1994. pp 10-13.Derby R: A second proposal for discography standards. ISIS Newsletter, Volume 2, Number 2. Daly City, California, International Spinal Injection Society, 1994. pp 108-122.
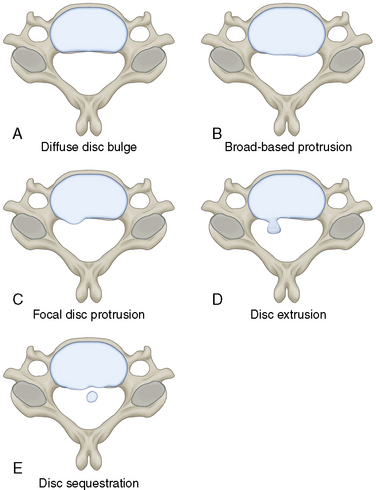
Table 13.9 Classification of CT Discographic Findings
| Type 1 | The discogram is normal manometrically, volumetrically, and radiologically, and produced no pain. The CT discogram shows contrast agent to be centrally located in both axial and sagittal projections. |
| Type 2 | Identical to type 1 except it is positive for pain reproduction. |
| Type 3 | The anular tears lead to a radial fissure. This group can be further subdivided into: |
| 3a The radial fissure is posterior | |
| 3b The fissure radiates posterolaterally | |
| 3c The fissure extends lateral to a line drawn from the center of the disc tangential to the lateral border of the superior articulating process | |
| Type 4 | When the radial fissure reaches the periphery of the anulus fibrosus, nuclear material protrudes, causing the outer anulus to bulge. |
| Type 5 | When the outer anular fibers rupture, nuclear material may extrude beneath the posterior longitudinal ligament, directly contacting either the dura or a nerve root. |
| Type 6 | When the extruded fragment is no longer in continuity with the interspace, it is said to be sequestrated. Manometrically, volumetrically, and radiologically, the discogram is always abnormal. Concordant pain may be reproduced only if enough pressure is generated against the free fragment to cause stimulation of pain-sensitive structures. |
| Type 7 | The end stage of the degenerative process is internal disc disruption, in which multiple anular tears occur. The discograms are abnormal manometrically and volumetrically, and familiar pain may or may not be reproduced. The contrast agent usually fills the entire interspace in a chaotic fashion. The CT discogram shows extravasation of contrast agent throughout multiple anular tears. |
Data From Bernard TN Jr: Lumbar discography followed by computed tomography. Refining the diagnosis of low-back pain. Spine 15: 690-707, 1990.Sachs BL, Vanharanta H, Spivey MA, Guyer RD, Videman T, Rashbaum RF, Johnson RG, Hochschuler SH, Mooney V. Dallas discogram description. A new classification of CT/discography in low-back disorders. Spine (Phila Pa 1976). 1987 Apr;12(3):287-94.
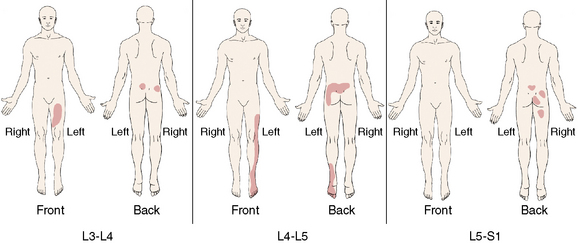
Table 13.10 Patterns of Pain Provocation for Positive Discograms
| Discogram or Finding | Positive Pain Provocation Referral Patterns |
|---|---|
| L3-L4 injections | The lumbar region with radiation into the anterior but not posterior thigh (71.4%) |
| L4-L5 injections | The lumbar pain with more equivalent proportions of anterior and posterior thigh pain (>63%) |
| L5-S1 injections | The lumbar region with posterior thigh or leg pain (>75%). |
| Absence of disc pathology | Pain limited to the low back and buttocks (58.3%) |
Data from Ohnmeiss DD, Vanharanta H, Ekholm J. Degree of disc disruption and lower extremity pain. Spine (Phila Pa 1976). 1997 Jul 15;22(14):1600-5.
Postoperative follow-up
After discography, the patient should be advised as follows:
 “Stress-bearing” or “strenuous” activities should be limited for 24 hours because of expected postprocedure discomfort.
“Stress-bearing” or “strenuous” activities should be limited for 24 hours because of expected postprocedure discomfort.Caveats
 Intervertebral discography should be performed only when the source of the spinal pain remains unknown after various imaging and electrodiagnostic studies and an interventional procedure such as intradiscal electrothermal therapy (IDET), nucleoplasty, or fusion is to be scheduled.
Intervertebral discography should be performed only when the source of the spinal pain remains unknown after various imaging and electrodiagnostic studies and an interventional procedure such as intradiscal electrothermal therapy (IDET), nucleoplasty, or fusion is to be scheduled. Because the intervertebral disc is the largest avascular organ in the body, it is essential that the risk of discitis be minimized.
Because the intervertebral disc is the largest avascular organ in the body, it is essential that the risk of discitis be minimized.1 Guyer R.D., Ohnmeiss D.D. NASS: Lumbar discography. Spine J. 2003;3:11S-27S.
2 Crock H.V. A reappraisal of intervertebral disc lesions. Med J Aust. 1970;1(20):983-989.
3 Smith S.E., Darden B.V., Rhyne A.L., Wood K.E. Outcome of unoperated discogram-positive low back pain. Spine. 1995;20:1997-2000. discussion 2000–2001