Interventions for clients with movement limitations
DARCY A. UMPHRED, PT, PhD, FAPTA, NANCY N. BYL, PT, MPH, PhD, FAPTA, ROLANDO T. LAZARO, PT, PhD, DPT, GCS and MARGARET L. ROLLER, PT, MS, DPT
After reading this chapter the student or therapist will be able to:
1. Appreciate the complexity of motor responses, and discuss methods used to influence body systems and their effects on functional behaviors.
2. Outline the differences in recovery related to healing, compensation, substitution, habituation, and adaptation.
3. Analyze the similarities and differences among impairment training of specific body systems, functional training, augmented feedback training, and learning-based sensorimotor retraining.
4. Select appropriate intervention strategies to optimize desired outcomes.
5. Analyze variables that may both positively and negatively affect complex motor responses and a patient’s ability to participate in functional activities.
6. Identify procedures and sequences required to attain the most successful therapeutic outcome that best meets the needs and goals of the client and the family.
7. Consider the contribution of the client, the client’s support systems, research evidence, neurophysiology, and the best practice standards available to optimize outcomes.
Before discussing therapeutic intervention procedures, the therapist must identify the learning environment within which the client will perform. As discussed in Chapter 1, that environment is made up of the therapist and the client, all internal body control mechanisms of the client, and the external restraints and demands of the world. Although this text focuses on relearning functional movement, the reader must always consider all aspects of the client including how other organs or body systems will be affected by or will affect the therapeutic outcome both during rehabilitation and in relation to long-term quality of life. An examination and evaluation (see Chapter 8) are performed before intervention to establish movement diagnoses. These examinations lead to movement diagnoses that must link to functional limitations or restrictions in activities and their causations (body system problems). Movement diagnoses and the degree and extent of the system or subsystem dysfunction or impairments determine prognosis of the outcomes on the basis of the client’s potential for functional improvement. Factors such as motivation, family support, financial support, and cultural biases must be considered as part of the prognosis.1 This process guides the selection of intervention strategies. Although it could be assumed that some of these impairments would be directly correlated to the central nervous system (CNS) trauma experienced by the client, it must also be determined whether some or most of these impairments have developed over a lifetime as a result of small traumas and adjustments to life. This insidious cause of impairments needs to be differentiated from acute causation of activity limitations because goal setting and expectations related to prognosis and recovery can be different.
Both the American Occupational Therapy Association (AOTA) and the American Physical Therapy Association (APTA) have developed guides to practice that help to direct therapists entering the professions and should help to guide practice throughout their working lives.2,3 APTA, through the initiation of the California Physical Therapy Association, has been collecting and classifying evidence-based articles through the Hooked on Evidence project.4 Through the use of current evidence-based practice; sensorimotor processing, motor control, motor learning, and neuroplasticity theories (see Chapter 4); and body systems models, the therapist must determine the flexibility or inherent motor control the client demonstrates while executing functional activities and participating in life. This chapter or other chapters in the book cannot establish for the reader the exact treatment sequence that should be used for every patient, but an example of a decision-making pathway has been given in Box 9-1. Functional goals must be established that lead to the client’s ability to participate in life within his or her environment and whenever possible lead to or maintain the quality of life desired by the client. Similarly, the therapist must differentiate whether the observed motor problems are based on acute or longstanding impairments before establishing timelines for prognosis.
Before beginning any intervention, the therapist must determine the treatment strategies that will be used to help the client attain the desired functional outcomes. The specific environment used by the therapist to optimize patient performance will depend on the functional level and amount of motor control exhibited by the patient. The following classifications can be used to document the specific role of the therapist within the training session (refer to Chapter 4 for additional detail):
Functional training: Practice of a functional skill that is meaningful, goal directed, and task oriented. Patient will experience errors and self-correct as the program becomes more automatic and integrated. An example would be gait training on a tile surface, rugs, inclined surfaces, compliant surfaces such as grass, and so on to practice ambulation.
Body system or impairment training: Treatment focus is on correcting a body system problem during an activity (e.g., pure muscle strengthening, stretching, sensory training, endurance training).
Augmented feedback training: Patient needs external feedback (auditory, visual, kinesthetic) and control over the motor program running the target task. This will limit the response patterns (e.g., reducing degrees of freedom, reduction or enhancement of tone) for successful performance of the desired movement (e.g., handling techniques, body-supported treadmill training, constraint-induced training).
Learning-based sensorimotor retraining: Treatment focus is placed on improving sensory discrimination dysfunction as a consequence of somatosensory, premotor, and motor cortical disorganization resulting from trauma, degeneration, or overuse.
The reader must also remember that intervention encompasses multiple interactive environments where intervention decisions are often made moment by moment during any treatment period. The challenge to the educated clinical professional is to determine what is being done, why it is working, how to continue its effectiveness, and how to determine the progress of the successful intervention. The clinician must also determine how to empower the client (emotionally, cognitively, and motorically) to take over the intervention with inherent, automatic mechanisms that lead to fluid, flexible, functional outcomes independent of both the therapist and the environment within which the activity is occurring. It is not until clinicians can determine effective treatment outcomes from various interventions that efficacy within a research laboratory can be studied without speculation and hypothesis formation based on speculation.1 Effectiveness is the first way to determine evidence-based practice. Once effectiveness has been established through case studies and larger controlled studies within the clinical environment, researchers can begin to tease out separate variables and establish efficacy as part of evidence to justify clinical decision making.
History of development of interventions for neurological disabilities
During the decade or two before the 1960s, some talented and intelligent clinicians began to question the traditional intervention strategies used by the OT and PT. These pioneers5–29 in neurological rehabilitation set the stage for the development of new concepts that allowed basic science to infiltrate the clinical arena. The intervention strategies of Jean Ayers, Berta Bobath, Signe Brunnstrom, Margaret Johnstone, Susanne Klein-Vogelbach, Margaret Knott, Dorothy Voss, Margaret Rood, and others became popular. Colleagues observed these master clinicians and could easily see that the “new” interventions were much more effective and provided better outcomes than previous interventions. Each approach focused on multisensory inputs introduced to the client in controlled and identified sequences. These sequences were based on the inherent nature of synergistic patterns5,21,30,31 and motor patterns observed in humans5,7,32 and lower-order animals33 or a combination of the two.19,21 Each method focused on the individual client, the specific clinical problems, and the availability of alternative treatment approaches within an established framework. Some of these approaches focused on specific neurological medical diagnoses. The treatment emphasis was then on specific patients and their related movement disorders. Children with cerebral palsy and head injuries7,23,28 and adults with hemiplegia8,9,21,32 were the three most frequently identified medical diagnostic categories. In 1968 at Northwestern University a large conference was held and laid the foundation for the first STEP conference (Northwest University Special Therapeutic Exercise Project [NUSTEP]). Most of these master clinicians, along with research scientists of the day, came together to try to (1) identify the commonalities and differences between these approaches, and (2) integrate and use the neuroscience of the day to explain why these approaches worked.34 Since the 1970s, substantial clinical attention has also been paid to children with learning and language difficulties.5,13,35 Now these concepts and treatment procedures have been applied across the age spectrum for all types of medically diagnosed neurological problems seen in the clinical setting (refer to Section II of this text). This expansion of the use of any of the methods for any pathological condition manifested by insults from disease, injury, or degeneration of the brain seems to be a natural evolution given the structure and function of the CNS and commonalities in system problems and activity limitations that take the individual away from participating in life.
Fortunately, most dogmatism no longer persists with respect to territorial boundaries identified by clinicians using some specific intervention methods. A conference in 199036 played a significant role in challenging the relevance of these territorial boundaries and stressed the adoption of a systems model when looking at impairments, activity limitations, and participation in life interactions.37 As the boundaries for interventions began blurring, intervention approaches such as proprioceptive neuromuscular facilitation (PNF) were then integrated into the care of clients with orthopedic problems and patients with neurological impairments. Today, few universities within the United States teach separate sections or units on specific approaches, but rather teach students to identify problems, when they are occurring in functional programs, and what bodily systems might be the cause of those activity limitations.
For example, assume that a client with hemiplegia exhibited signs of a hypertonic upper-extremity pattern of shoulder adduction, internal rotation, elbow flexion, and forearm pronation with wrist and finger flexion. Brunnstrom8 would have identified that pattern as the stronger of her two upper-extremity synergies. Michels,21 although using an explanation similar to Brunnstrom’s to describe the pattern, would have elaborated and described additional upper-extremity synergy patterns. Bobath would have asserted that the client was stuck in a mass-movement pattern resulting from abnormal postural reflex activity.30 Although the conceptualization of the problem certainly determined treatment protocols, the pattern all three clinicians would have worked toward was shoulder abduction, external rotation, elbow extension, forearm supination, and wrist and finger extension. The rationale for the use of this pattern within an intervention period would vary according to the philosophical approach. One clinician might describe the pattern as a reflex-inhibiting position (Bobath).31 Another would describe the pattern as the weakest component of the various synergies (Brunnstrom),8 whereas still another might identify the pattern as producing an extreme stretch and rotational element that inhibited the spastic pattern (Rood).25 How those master clinicians sequenced treatment from the original hypertonic pattern to the opposite pattern and then to the goal-directed functional pattern would vary. Some would facilitate push-pull patterns in the supine and side-lying positions and rolling. Others would look at propping patterns in sitting clients or at weight-bearing patterns of clients in the prone position, over a ball or bolster, or in partial kneeling. All have the potential of improving the functional pattern of the upper extremity and modifying the hypertonic pattern. One method may have been better than the others given a particular patient, but in truth improved patient performance may have stemmed not from the method itself, but rather from the preferential CNS biases of the client and the variability of application skills among the clinicians themselves. That is, when a therapist intentionally uses specific augmented feedback to modulate the motor system’s response to an environment but does not identify the other external feedback present within that environment (e.g., lighting, sound, touch, environmental constraints), therapeutic results will vary. Because of variance, efficacy of intervention is often questionable, although the effectiveness of that therapist may be easily recognized.
Because of the overlap of treatment methods and the infiltration of therapeutic management into all avenues of neurological dysfunction, various multisensory models were developed during the early 1980s.13,38–41 These have continued to evolve into acceptable methods in today’s clinical arena. Although these models attempted to integrate existing techniques, in reality they have created a new set of holistic treatment approaches. In July 2005 the III STEP conference42 was held in Utah to again bring current theories and evidence-based practice into today’s clinical environment. The history of the three STEP conferences demonstrates the evolution of evidence-based practice from the first conference, where basic science was the only evidence to justify treatment, to the second conference, where evidence in motor learning and motor control began to bring efficacy to intervention. By the time the third conference was held, the research in neuro/movement science regarding true efficacy within practice and the reliability and validity of our examination tools set the stage for standards in practice.43 Where the next conference will take the professions and how soon that will occur is up to colleagues in the future. No proceedings from that third conference were published, but over the preceding years articles covering most of the presentations had been published in the Journal of Physical Therapy. The ultimate goal would be to develop one all-encompassing methodology that allows the clinician the freedom to use any method that is appropriate for the needs and individual learning styles of the client as well as to tap the unique individual differences of the clinician. Although intervention today is based on an integrated model, the influence of third-party payers, the need for efficacy of practice, and time constraints often factor into the therapist’s choice of intervention. Visionary and entrepreneurial practice ideas that have the potential to be effective will always be a challenge to future therapists. Those ideas generally originate within the clinical environment and not the research laboratory. For that reason, clinicians need to communicate ideas to the researcher, and then those researchers can develop research studies that test the established efficacy or refute that effectiveness. Few researchers are master clinicians, and few clinicians are master researchers; thus collaboration is needed as the professions move forward in establishing evidence-based practice.
Today’s therapists have replaced many of the existing philosophical approaches with patient-centered therapeutic intervention. Patient performance, available evidence, and the expertise of the clinician often play a key role in the specific decision regarding an intervention. When confronted with an abnormal upper-extremity pattern, today’s therapist may choose to work on improving the movement pattern using a functional activity. Control of the combination of movement responses and modulation over specific central pattern generators or learned behavior programs will allow the patient opportunities to experience functional movement that is task oriented and environmentally specific. With goal-directed practice of the functional activity, neuroplastic changes, motor learning, and carryover can be achieved.44 With a better scientific basis for understanding the function of the human nervous system, how the motor system learns and is controlled, and how other body systems, both internal and external to the CNS, modulate response patterns, today’s clinicians have many additional options for selection of intervention strategies.45–54 Whether a patient would initially benefit best from neuromuscular retraining, functional retraining, or a more traditional augmented or contrived treatment environment is up to the clinician and is based on the specific needs identified during the examination and evaluation process.
A problem-oriented approach to the treatment of any impairment or activity limitation implies that flexibility and neural adaptation are key elements in recovery. However, adaptation should not be random, disjointed, or non–goal oriented. It should be based on methods that provide the best combination of available treatment alternatives to meet the specific needs of the individual. Development of a clinical knowledge bank enables the therapist to match treatment alternatives with the patient’s impairments, activity limitations, objectives for improved function, and desired quality of life. A professionally educated therapist no longer bases treatment on identified approaches, although specific aspects of those approaches may be treatment tools that will meet the client’s needs and assist him or her in regaining functional control of movement. Treatment is based on an interaction among basic science, applied science, the therapist’s skills, and the client’s desired outcomes.49–52,55,56 In most cases, multiple intervention strategies must be included, but the therapist needs to be able to identify why those selected treatments will lead to system improvement as well as documenting those findings using reliable standardized and acceptable clinical methods and terminology. These intervention strategies must be dynamic yet also understandable and repeatable. As new scientific theories are discovered, new information must be integrated to continue to modify treatment approaches.
Intervention strategies
Functional training
In Chapter 8 the steps involved in the examination process are explained in detail. The intricate relationship of body system problems, impairments, and functional limitations that decrease participation in the rehabilitation process are discussed. Functional training can be implemented once the clinician has identified the client’s activity limitations. The clinician must first answer the questions “What can the client do?” “What limitations does the client have when engaging in functional activities?” “Are there motor programs that are being used to substitute for normal motor function?” and “Can the therapist use functional training to improve body system problems within the context of the functional skill?” Once the therapist has an understanding of the reasons for any activity limitation and can alleviate substitution and compensation for the deficit, functional tasks should be identified and practiced.
The effect of functional training on task performance and participation
An intervention approach in the early 1990s that evolved as an offshoot of functional training was labeled clinical pathways. These pathways were established by health care institutions to improve consistency of management of patients who met specific medical diagnostic criteria. It has been proven that the implementation of these pathways reduces variability in clinical practice and improves patient outcomes.67 Health care practitioners also became aware that some individuals do not fall into these pathways and need to be treated according to the specific clinical problems that the patients were presenting.
Conclusion
One important variable that has clearly been identified with respect to functional training is “task specificity.”47,68–76 Although it is important that a patient be independent in as many ADLs as possible, often the therapist, the patient, and the family need to prioritize which activities are most important to the quality of life of the patient. If walking into the mountains to do “birdwatching” is one important goal to the patient, then creating an environment that would closely resemble the environment of that activity is crucial. Similarly, practice within that environment is a key to successful carryover (see Chapter 4). If the patient wants to walk into the mountains and the family expects the patient to walk into his or her old job, a therapist must accept that motivation will drive behavior and task specificity will drive learning. Carryover into any other functional activity such as walking into the office building in order to go back to work may not be the motivating factor that will guide that individual’s desire to perform that motor task. Whether the patient ever goes back to work is not the variable that should be used as part of the motivational environment for task-specific gait training geared to walking in the mountains and is not a decision for which the therapist is responsible. Therapists need to allow the patient to tell them what will be the most important task and the specificity of that task to optimize motor learning and functional recovery.
Body system and impairment training
As mentioned in Chapter 8, the therapeutic examination results in the identification of activity limitations and possible body system and subsystem impairments that are causing the functional movement disorders. Impairment training is another intervention strategy that involves the correction of impairments with the expectation that improving these impairments will result in a corresponding improvement in function. For example, when a client has the inability to stand up without assistance (activity limitation) and the clinician determines the cause to be lower-extremity weakness, an appropriate approach may be to strengthen the lower extremities (impairment training). Numerous studies have shown the effectiveness of impairment training in improving the functional performance of individuals with neurological conditions such as cerebral palsy,77,78 stroke,79–87 multiple sclerosis,88–93 Parkinson disease,94–98 and other neuromuscular diagnoses.99–110 The strengthening intervention selected should reflect the task and the environment within which the impairment was identified. The clinician should attempt to create a training situation so that the client may be able to run the necessary motor programs with all the required subsystems in place. For example, training sit to stand with weakness in the hip and knee extensors is much less likely to automatically result in the improvement of sit-to-stand function if the therapist begins the activity in sitting where generation of extension is most difficult, than if the strengthening training was performed with repetition of practice starting in standing and going to sit and back again to stand. By decreasing the degrees of freedom of the eccentric control of the hips and knees when going from stand to sit, the functional training activity has turned into specific impairment training. The therapist can ask the patient to eccentrically lengthen the extensors only in a limited range and then concentrically contract back to standing. As the power increases, the degrees of freedom can also be enlarged until the patient is able to complete the task of stand to sit while simultaneously regaining the sit to stand pattern. In pure impairment training a patient might also be asked to straighten the knee when sitting or to extend the hip when prone. These three exercises have the potential of training impaired strength, but only the first example forces the training within a functional pattern. Similarly, the therapist could train the sit-to-stand pattern using various seat heights that encompass many of the components that force the use of normal movement synergies and postural control, using the environment in which that activity is typically performed, versus performance of strengthening exercises against resistance in an open chain exercise program.
Augmented therapeutic intervention
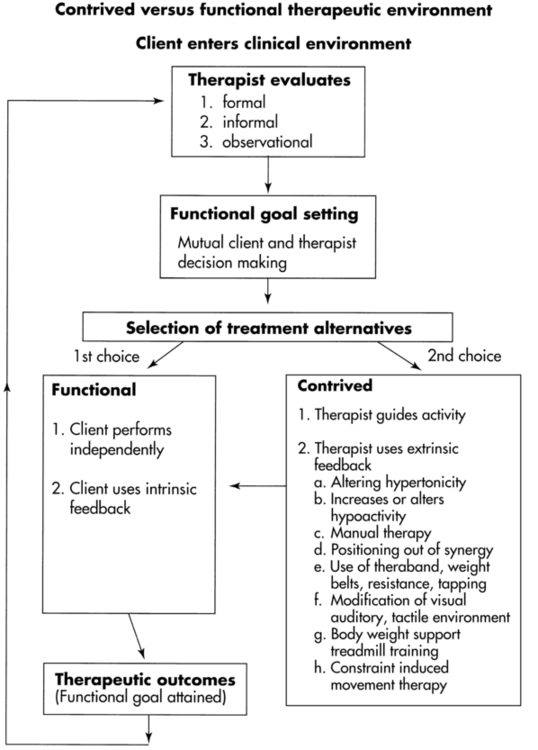
These augmented techniques make up a large component of the therapist’s specific interventions tool box. The difference between augmented and functional training might be the need for the therapist or piece of equipment to be part of the client’s external environment for the client to succeed at the task. For example, in BWSTT a harness is used to take away the demand of gravity on the limbs during gait and the demand of the postural trunk and hip muscles for stability. Before the therapist or the patient can consider the movement as independent, those aspects must be removed from the environment. In the previous example, the individual needs to transition from maximal body weight support during ambulation to not needing any external support during ambulation. The client must assume total ownership of the functional responses. Then and only then has independence been achieved. At that time, functional retraining can be used with the intent of enlarging the environmental parameters to allow for maximal independence. Figure 9-1 illustrates this concept of functional versus contrived intervention, which must be constantly considered throughout any treatment session. Augmented techniques are often the early choices for treatment of patients who have neurological insults. It cannot be emphasized enough that once the client has the ability to perform without augmented methods and does so in functional, efficient ways, those augmented techniques need to be selectively eliminated.
Once a clinician has chosen to augment the clinical environment, the client needs to learn efficient motor behaviors within the limitations of that environment. The client influences the therapist’s decision-making strategies by selecting inefficient or ineffective motor responses to a given task demand. If the response is effortless, efficient, and noninjurious to any part of the body and meets the client’s expectations and goals, then the therapist knows the strategies selected were effective even if the therapist augmented the intervention. If the movement itself is available to the client, then there is a high probability that the client will be able to regain that movement control, regardless of the need for early augmentation to achieve the skill. If the response does not meet the desired goal for any reason, then the therapist must determine why. Often, it is because the therapist did not identify the correct body system problems. Many correct solutions may answer the question. Which solution is best may be more client than approach dependent. Yet if flexibility means that the therapist selects any component of any method that helps the client reach an objective, then the therapist is confronted with hundreds—if not thousands—of various treatment choices. If the treatment procedures used introduce information to the client through sensory systems, then from a neurological perspective a limited number of input systems or modalities are available. The myriad treatment procedures are transformed into neurochemical and electrophysiological responses that must travel along a limited number of pathways in the nervous system. Thus, many different treatment procedures may produce similar types of neurotransmission. The temporal and spatial sequencing or timing of the input will vary according to the technique and the specific application. The clinician has little basis for decision making without a comprehensive understanding of the neurophysiological mechanisms of (1) the various techniques introduced to modify input, (2) where that information will be processed and how that might affect motor output, (3) prior learning and the ability for new learning, and (4) the client’s willingness and motivation to adapt. The reader is referred to Chapter 1 (Figure 1-1); Chapter 4 on motor control, motor learning, and neuroplasticity; and Chapter 5 for a discussion on motivation.
The number of available contrived or augmented feedback techniques is almost infinite. This section presents an overview of a classification system that can be used to help the reader develop a greater understanding of why certain responses occur and why the selection of certain techniques is appropriate and should positively affect the desired motor responses. This section focuses on intervention strategies that have been accepted, have been used within the traditional Western health care model, and are efficacious. Some alternative approaches to intervention that are not necessarily classified as traditional within this chapter are introduced in Chapter 39. There are other classification systems a clinician might use when analyzing movement problems seen in patients with neurological dysfunction. For example, a therapist may see in a patient a problem primarily with tone, such as hypertonicity, hypotonicity, rigidity, dystonia, flaccidity, intentional and nonintentional tremors, ataxia, and combinations of or fluctuations in the total movement strategies. Given this specific classification schema, one still uses the available treatment strategies or uses an input modality that may modify the specific tone problem that was causing the movement dysfunction.
The primary goal of this section is to help the reader develop a classification system based on the primary input modality used when introducing an augmented treatment technique to facilitate a sensory system and provide feedback to the CNS in order to help a client learn or relearn motor control. The reader has been provided with an in-depth reference to the specific neurophysiological approaches in the past also discussed in Chapter 1, and only a brief overview has been included within this chapter. In-depth discussion of some basic treatment strategies, explanations of less familiar techniques, and current approaches gaining popularity within the clinical area of movement analysis are found within the body of this section.
When the primary input system for a technique is identified, at no time do we suggest that it is the only input system affected. For example, when a proprioceptive technique is introduced, tactile cutaneous receptors are also simultaneously firing. If there is a “noise” component (such as with vibration or tapping with the fingers), then auditory input has been triggered as well. There is evidence that a given sensory modality may “cross over” or fuse with a completely different modality, helping in the synthesis of motor responses. In addition, there is evidence that the principles of neuroplasticity are applicable across modalities (e.g., auditory, visual, vestibular, somatosensory). Sometimes responses occur in a modality that does not appear to be related. For example, olfaction may improve tactile sensitivity of the hand. This concept is called cross-modal training or stimulation.111,112 Yet a classification schema based on a primary modality promotes logical problem solving because the therapist can select from available treatment procedures that theoretically provide similar information to the CNS and help in the organization of appropriate motor responses. The motor system and its various motor programmers adapt to the environment to achieve functional motor output toward a goal. Both external and internal feedback are critical for adaptation and change. External feedback in this chapter is considered a mechanism to help the client’s CNS optimally learn and adapt. Obviously, as the patient learns, internal feedback will allow the person to run feed-forward motor programs without the need for external feedback for control. External feedback will, it is hoped, be used only when the outside surrounding needs the feed-forward program to change to adapt to a new environment (refer to the Chapter 4 section on motor learning). Therapists must realize that even if the primary goal may be to facilitate or dampen a motor system response, diverging pathways may also connect with endocrine, immune, and autonomic systems. According to motor control theory, the clinical picture is a consensus of all interacting body systems (see Chapter 4). Research tools are not yet available to measure those systems interacting simultaneously, although functional magnetic resonance imaging (fMRI) studies are beginning to help researchers and clinicians identify what happens to the nervous system with input from the environment and how that information is processed. Efficacy using reliable and valid measurement tools must then be based on outcomes, with an understanding of the best available scientific knowledge as a rationale for why the outcome is present.
This classification system is based on identified input, observed responses, current research on the function of the CNS, and the various systems involved in the control and modification of responses. An understanding of normal processing of input and its effect on the motor systems helps the clinician evaluate and use the intact systems as part of treatment. Research with fMRI is now allowing greater insight into specific brain regions that are being used during various cognitive and motor activities.113–128 Yet the specific interactive nature of multisensory input, memory, motivation, and motor function is still unknown. When the response to certain stimuli does not help the client select or adapt a desired motor response, then the classification schema for augmented input provides the clinician with flexibility to select additional options. This can be done by spatially summating input, such as using stretch, vibration, and resistance simultaneously, or temporally summating input, such as increasing the rate of the quick stretch or increasing the time between inputs to give the system ample time to respond.
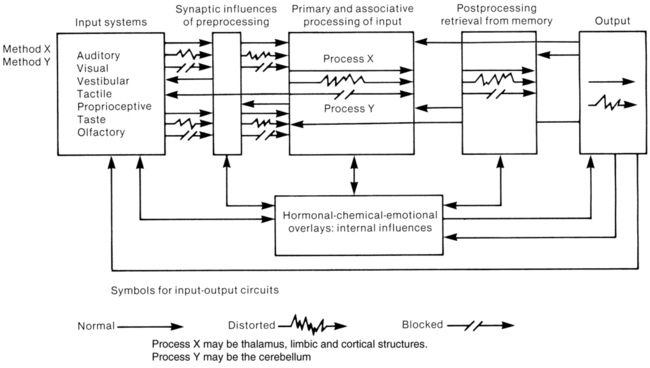
Many factors can influence motor behavior, such as the methods of instruction, the resting condition of the nervous system, synaptic connections, cerebellar or basal ganglia or cortical processing, retrieval from past learning, motor output systems, or internal influences and neuroendocrine balance. Figure 9-2 illustrates and simplifies this total system. Its clinical implications become clearer if the therapist retains a visual image of the client’s total nervous system, including afferent input, intersystem processing, efferent response, and the multiple interactions on one another. At any moment in time, multiple stimuli are admitted into a client’s input system. Before that information reaches a level of primary processing, it will cross at least one if not many synaptic junctions. At that time the information may be inhibited, excited, changed or distorted, or allowed to continue without modification. If the information is at the first synapse, the patient will have no sensation. If it is inhibited at the thalamus, again the patient will not perceive sensation, but that does not mean other areas of the brain will not be sent that information, because sensory information is also sent to a variety of areas after that initial synapse. Research studies have found that sensory input information may even affect gait and other movement patterns even if the patient has no perception of the input.129,130 If the input is changed, then the processing of the input will vary from the one normally anticipated. The end product after multiple system interactions will be close to, will be farther away from, or will seem to have no effect on the desired motor pattern. Furthermore, sensory processing can take place at many segments of the nervous system. Although the CNS is not hierarchical, with one level in total control over another, certain systems are biased to affect various motor responses. At the spinal level the response may be phasic and synergistic. Brain stem mechanisms may evoke flexor or extensor biases, depending on various motor systems and their modulation. Cerebellar, basal ganglia, thalamic, and cortical responses may be more adaptive and purposeful.130–133 Thus the therapist must try to discern where the input or the feedback is being affective or short circuited.
Remembering input as a possible option for intervention will always allow the therapist to differentiate the same five alternatives—no response, facilitating (heightening), inhibiting (dampening), distorting, or normal processing. These alternatives can occur anywhere in the system at synaptic junctions. Finally, motor output is programmed and a response is observed. If the response is considered normal, the clinician assumes that the system is intact with regard to the use and processing of the inputs. If the response is distorted or absent, little is known other than there is a lack of the normal processing somewhere in the CNS or an insufficient amount of input was used. One way to differentiate motor problems from problems with other systems is to use other functional activities that have programs similar to the body system program identified as impaired. If a program, such as posture, demonstrates deficiencies in one functional pattern, then the therapist must determine if it is also deficient in other patterns. If the postural motor problem affects all motor performance, then the therapist had determined that a motor program deficit exists and will have to determine how to correct that problem. If, on the other hand, the program runs smoothly and effortlessly when certain demands are taken away, such as resistance from gravity, position in space, need for quick responses, and so forth, then it may be that the problem is within another subsystem such as cognition, perception, the biomechanical system, or the cardiopulmonary system or is a power-production problem that can be corrected by slowly increasing the demand on the postural system through repetitive practice using various additional input interventions. Differentially screening motor impairments as pure CNS motor problems (muscle recruitment, firing rate, balance) versus problems with another system (perception of vertical) becomes critical in a managed-care system that funds only a certain number of treatment sessions. Internal influences also need to be considered because they affect each aspect of the system. Once normal processing has been identified, understanding of deficit systems and potential problems can be analyzed more easily. To reiterate, this requires awareness of the totality of the individual—that is, the client’s personal preference of stimuli and the uniqueness of processing and internal influences. A systems model requires simultaneous processing of multiple areas, with interactions being relayed in all directions. A client’s CNS and peripheral nervous system (PNS) are doing just that, and the therapist must develop a sensitivity toward the client as a whole while interacting with specific components (see Chapters 1, 4, 5, 6, and 39 for additional information). With input from the client and family, it is the therapist’s responsibility to select methods most efficacious and effective for each client’s needs in relation to that person’s specific neurological problems. (See all clinical chapters in Section II.) This viewpoint, based on a variety of questions, leads to a problem-oriented approach to intervention. Because the output or response pattern is based on alpha motor neuron discharge and thus extrafusal muscle contraction, the first question is posed: what can be done to alter the state of the alpha motor neuronal pool or motor generators? Second, what input systems are available, either directly or indirectly, that will alter the state of the motor pool? Third, which techniques use these various input systems as their primary modes of entry into the CNS? Fourth, what internal mechanisms need modification or adaptation to produce a desired behavior response from the client? Fifth, which input systems are available to alter the internal mechanism and what outcomes are expected? Sixth, what combination of input stimuli will provide the best internal homeostatic environment for the client to learn and rehearse a more optimal response pattern? For example, assume that a client with a residual hemiplegia resulting from an anterior cerebral artery problem has a hypertonic lower extremity that produces the pattern of extension, adduction, internal rotation of the hip, extension of the knee, and plantarflexion inversion of the foot. The answers to the first two questions are based on the knowledge that the proprioceptive and exteroceptive systems can drastically affect spinal central pattern generators and that these input systems are intact at spinal, brain stem, cerebellum, and thalamic levels and may even project to the cortex.
Appropriate selection of specific techniques—such as prolonged stretch using the tendon organ to modulate the hypertonic pattern, quick stretch or light touch to the antagonistic muscle, or any other treatment modality within the classification schema—will provide viable treatment alternatives. Awareness that a client’s response pattern is an inherent synergistic pattern and that it is further elicited by pressure to the ball of the foot leads to a better understanding of the clinical problem. Knowing that the client is unable to combine the alternative patterns, such as hip flexion with knee extension needed for the late stage of swing phase through the early aspects of stance phase during gait, the therapist can use the other inherent processes to elicit these and other patterns. BWSTT is an example of an augmented treatment intervention in which the clinician assists the patient to place the leg and foot with each step while the apparatus controls balance and posture to provide an experience of normal gait while requiring the patient to have only the strength to manage partial body weight.134–139 Finally, techniques such as combining standing and walking with the application of quick stretch, vibration, or rotation, or having the client reach for a target or follow a visual stimulus while walking, provide a variety of combinations of therapeutic procedures to help the client learn or relearn normal response patterns. Furthermore, combining techniques gives the clinician a choice of various procedures and promotes a learning environment that is flexible, changing, and interesting. The therapist must, again, make the transition from applying contrived therapeutic procedures during functional tasks to allowing the client to practice the task without the therapist interceding and without external feedback.140 In that way the client uses inherent feedback to self-correct feed-forward motor programming and then to continue running the appropriate movement strategies. This self-correction leads to independence, adaptability, and long-term learning (see Figure 9-2).
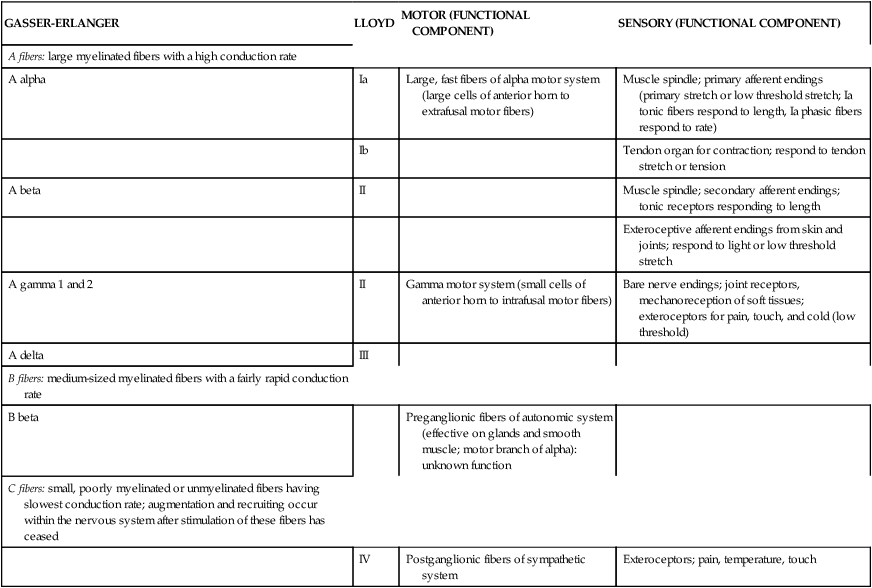
To avoid confusion about which peripheral sensory nerve fiber coming from the surface of the body or extremities is being discussed, the two primary methods of classifications (Gasser-Erlanger and Lloyd), along with a description of the functional component, have been included in Table 9-1 for easy referral. The other sensory systems will be presented separately to help the reader establish an appropriate classification scheme. The primary sensory input systems presented include proprioception, exteroception, vestibular, vision, auditory, taste, and smell. These sensory inputs have the potential to influence CNS structures including the thalamus, sensory and motor cortices, the cerebellum, the reticular formation, and the basal ganglia and thus to affect the descending fibers under their control.
TABLE 9-1 
CLASSIFICATIONS OF PERIPHERAL NERVES ACCORDING TO SIZE
| GASSER-ERLANGER | LLOYD | MOTOR (FUNCTIONAL COMPONENT) | SENSORY (FUNCTIONAL COMPONENT) |
| A fibers: large myelinated fibers with a high conduction rate | |||
| A alpha | Ia | Large, fast fibers of alpha motor system (large cells of anterior horn to extrafusal motor fibers) | Muscle spindle; primary afferent endings (primary stretch or low threshold stretch; Ia tonic fibers respond to length, Ia phasic fibers respond to rate) |
| Ib | Tendon organ for contraction; respond to tendon stretch or tension | ||
| A beta | II | Muscle spindle; secondary afferent endings; tonic receptors responding to length | |
| Exteroceptive afferent endings from skin and joints; respond to light or low threshold stretch | |||
| A gamma 1 and 2 | II | Gamma motor system (small cells of anterior horn to intrafusal motor fibers) | Bare nerve endings; joint receptors, mechanoreception of soft tissues; exteroceptors for pain, touch, and cold (low threshold) |
| A delta | III | ||
| B fibers: medium-sized myelinated fibers with a fairly rapid conduction rate | |||
| B beta | Preganglionic fibers of autonomic system (effective on glands and smooth muscle; motor branch of alpha): unknown function | ||
| C fibers: small, poorly myelinated or unmyelinated fibers having slowest conduction rate; augmentation and recruiting occur within the nervous system after stimulation of these fibers has ceased | |||
| IV | Postganglionic fibers of sympathetic system | Exteroceptors; pain, temperature, touch |
Proprioceptive system integration of stretch, joint, and tendon receptors
Proprioception as an input system has a direct effect on program generators at the spinal level.141 Because of its importance in motor learning and motor adaptation to new or changing environments, however, proprioception also has significant connections to the cortical and cerebellar neural networks. Its divergent pathways have synapses within the brain stem, diencephalon, and spinal system. Proprioceptive input can potentially influence multiple levels of CNS function, and all those levels can potentially modulate the intensity or importance of that information through many different mechanisms.141,142 Proprioceptors are found in three peripheral anatomical locations: the stretch receptors, the tendon, and the joint. The afferent receptors responsible for relaying sensory information through those sites are discussed in the following subsections.
Muscle stretch receptors
Stretch.
Stretch, quick stretch, and maintained stretch are all sensory input systems that use the stretch receptors in the muscles and heighten the motor pool.143–145 Stretch simultaneously heightens both the muscle response to that stretch and potentially heightens the sensitivity of the agonistic synergy. It will also lower the excitation of the antagonistic muscle and those muscles that are part of the antagonistic synergy. Stretch information will be sent to higher centers for sensory integration and perception. The cerebellum uses this incoming feedback to maintain and/or regulate motor nuclei in the brain stem that will influence the state of the alpha and gamma motor neurons. This allows for cerebellar feed-forward regulation (refer to Chapter 21). There are many ways to apply stretch to the muscles. The therapist can use (1) the hands and their respective muscle power to apply a stretch, (2) a manual weight system of some sort that maintains the stretch through the range, (3) a suspension system such as used in Pilates exercises (see Chapter 39), (4) the patient’s own body weight against gravity, (5) a complex robotic system that computerizes the amount of stretch depending on the individual’s specific data (see Chapter 38), or many other creative ways to apply stretch to muscle fibers within the belly of the muscle tissue. As stated previously, stretch can also be applied to the antagonist muscle or muscle synergy in order to dampen agonist function. Thus stretch can be used to enhance tone in the agonist or to decrease tone of the agonist through the antagonist. The therapist should always remember that even though a response may not look obvious, as long as the peripheral nerves and motor neurons within the spinal system are intact, these approaches will change the state of the motor pool.
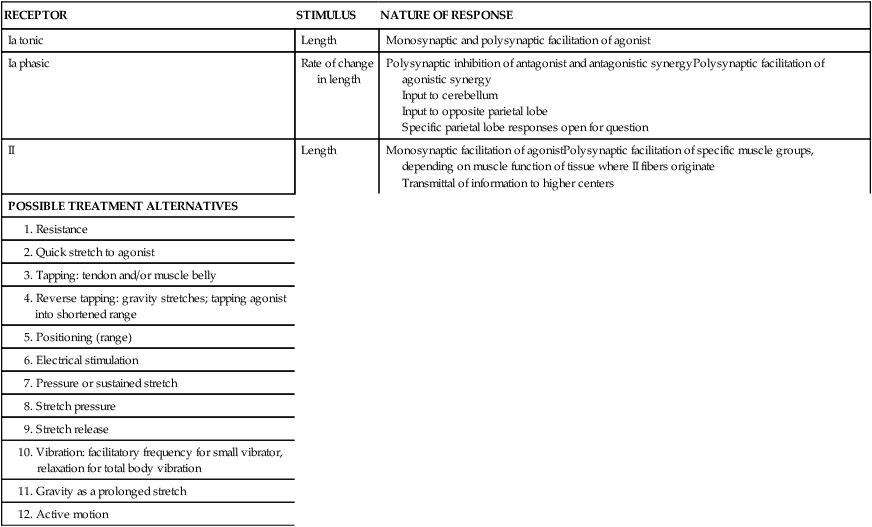
Table 9-2 lists a variety of treatment procedures believed to use proprioceptive input from the muscles as a primary mode of sensory stimulation. The varying intensity, amount of tension, or rate of the stimuli, in addition to the original length of the muscle before application of the stimulus, will determine its firing. Remember, afferent information is projecting to many areas above the spinal system, and the result will be regulation or modulation, ultimately affecting activity.141
TABLE 9-2 
PROPRIOCEPTIVE STRETCH RECEPTORS
| RECEPTOR | STIMULUS | NATURE OF RESPONSE |
| Ia tonic | Length | Monosynaptic and polysynaptic facilitation of agonist |
| Ia phasic | Rate of change in length | Polysynaptic inhibition of antagonist and antagonistic synergyPolysynaptic facilitation of agonistic synergy Input to cerebellum Input to opposite parietal lobe Specific parietal lobe responses open for question |
| II | Length | Monosynaptic facilitation of agonistPolysynaptic facilitation of specific muscle groups, depending on muscle function of tissue where II fibers originate Transmittal of information to higher centers |
| POSSIBLE TREATMENT ALTERNATIVES | ||
Resistance and strengthening.
Resistance is often used to facilitate intrafusal and extrafusal muscle contraction. Resistance can be applied manually, mechanically, and by the use of gravity. Resistance recruits more motor units in the target muscles. Although muscles can contract both in an isometric and an isotonic fashion, most contractions consist of a mixture of the two. Certain muscle groups, such as the flexors, benefit from isometric exercise, as well as isotonic exercise in both eccentric and concentric modes. Under normal circumstances, the flexors are used for repetitive or rhythmical activities. The extensors, on the other hand, usually remain contracted in an effort to act against the forces of gravity. Therefore the extensor groups benefit best from isometric and eccentric resistance.146
When resistance is applied to a voluntary muscle, spindle afferent fibers and tendon organs fire in proportion to the magnitude of the resistance. Resistance is more facilitative to an isometrically contracted muscle than in an isotonic contraction.35 As isometric resistance is increased or continued, more motor units are recruited, thereby increasing the strength of extrafusal contraction.26 Eccentric isotonic contraction refers to the lengthening of muscle fibers with resistance added to the distal segment, as in lowering the arms while holding a heavy weight. Eccentric contraction uses less metabolic output and promotes strength gains in less time.26 However, all types of muscle contraction will promote increased strength. Resistance is an important clinical treatment and has been used and will continue to be used by clinicians within multiple treatment philosophies over the next millennium.8,19,25,29,77,147–153 The complexity of neural adaptation after resistive exercises may lead to a different training environment depending on age, athletic status, and specific body system deficits.154 Combining resistive training with guided imagery or other types of adjunct interactions has conflicting results.154–156 Yet there are still questions regarding optimal resistive training and whether one resistive technique is better than another.157,158 Research certainly has shown that resistance training does enhance functional abilities across age groups,150,159,160 but again the specifics regarding resistive training techniques are often not identified. The terms resistive training, weight training, and strength training are often used synonymously, and thus specifics are yet to be identified in the research. How all these uses of resistive exercises will play out in the future is up to future researchers in the field of movement science. Very costly high-technology tools have been added to aid in resistive training (see the discussion of Pilates in Chapter 39 and robotics in Chapter 38).161,162 Given the needs of individuals after neurological insults, cost becomes a major factor, and finding creative and cost-efficient ways to apply resistance may become a common research question in the future.
Tapping.
Three types of tapping techniques are commonly used by therapists. Tapping of the tendon is a fairly nondiscriminatory stimulus. Physicians use this technique to determine the degree of stretch sensitivity of a muscle. A normal response would be a brisk muscle contraction. Because of the magnitude of the stimulus and the direct effect on the alpha motor neuron, this technique is not highly effective in teaching a client to control or grade muscle contraction.163 Instead, tapping of the muscle belly, a lower-intensity stimulus, is more satisfactory. Reverse tapping is a less frequently described technique, but it can be used. The extremity is positioned so gravity promotes the stretch, instead of the therapist manually tapping or actively inducing muscle stretch. Once the muscle responds, the therapist taps or passively moves the extremity to help the muscle obtain a shortened range. An example of reverse tapping would be tapping the triceps muscle when the client is bearing weight on the extended elbow and actively trying to achieve full elbow extension. Gravity quickly stretches the triceps. Timing of this technique is important. If the therapist taps the elbow toward extension when the flexors’ motor neurons are sensitive, then those flexor muscles may respond to the stretch and contract, taking the arm farther into flexion. If the timing follows the quick stretch to the extensor, then the flexors will be dampened and active extension more likely a motor response.
Positioning (range).
The concept of submaximal and maximal range of muscles is highly significant to clinical application. Bessou and colleagues164 monitored the neuronal firing of muscle spindles at different ranges of motion. Upper motor neuron lesions can alter the sensitivity of the spindle afferent reflex arc fibers by not using presynaptic inhibition to normally dampen incoming afferent activity.165 Therefore ROM should be carefully assessed on an individual basis, particularly in a patient with an upper motor neuron lesion, to determine the maximal or submaximal range for an individual. Therapists always need to determine whether the difference between optimal range and functional ROM is different. If a patient will never need to use full ROM, then spending long periods of time trying to stretch a shoulder or hip may not be the best decision with regard to intervention. As well as the ROM itself, therapists need to carefully evaluate excessive range resulting from hypermobility and hypotonicity. In those situations, external support of the affected joint or limb needs to be considered in all functional positions in order to prevent complications such as pain.166–168
Electrical stimulation.
For an in-depth discussion of the use of electrical stimulation both as an evaluation and a treatment modality, see Chapter 16 and Chapter 33. Electrical stimulation has the potential to be an excellent muscle spindle facilitatory technique, especially if additional therapeutic tools, such as resistance, are included. Electrical stimulation delivered to create muscle contraction is beneficial, but electrical stimulation as a sensory stimulus is less effective as a learning tool because there are no sensory receptors for electrical currents and thus they are not represented as a unique stimulus on the somatosensory cortex. Functional electrical stimulation (FES) is a technique that applies electrical stimulation during functional movement. Chapter 16 discusses this technique with traumatic spinal cord injury, but the application has gone beyond those individuals diagnosed with spinal injury. Individuals poststroke have also been studied using FES. The results were inconsistent. Some studies showed there was no difference in the stroke groups during or directly after intervention but that the long-term effect remained with those individuals who received FES, whereas those who did not regressed in function.169,170 Studies have shown that FES training increased walking ability and speed during and after the training.171,172 Studies that have looked at other neurological problems have also used FES and certainly are showing that this type of intervention may become a standard of practice in the future.173–175 Combined modulation of voluntary movement, proprioceptive sensory feedback, and electrical stimulation might play an important role in improving impaired sensorimotor integration by power-assisted FES therapy.176 The use of FES over acupressure points has been shown to significantly reduce pain.177
Stretch pressure.
The muscle belly is the stimulus focus of stretch pressure. The therapist slowly applies pressure to the muscle belly. It is used to decrease or release tone in the target muscle, allowing for the (temporary) recovery of voluntary movement.111,178 Generally this type of stimulus is applied and maintained for a period of time (e.g., 5 to 10 seconds). It is not a quick stimulus and may be using the tendon organ to dampen tone. This type of pressure technique is also used in a variety of complementary approaches (see Chapter 39).
Vibration.
There are two types of vibratory methods used therapeutically. The first deals with the use of a handheld vibrator to facilitate Ia receptors to enhance agonistic muscle contraction in hypotonic muscles or to facilitate Ia receptors of antagonistic muscle fibers to inhibit hypertonic agonists. Currently the use of vibration to facilitate Ia responses within specific muscle function has been used to show how proprioception can be used to alter upright standing.179,180 The second type of vibratory method is a total-body vibration to facilitate postural tone and balance and is applied through the feet in a standing position.181–184
Bishop185,186 wrote an excellent series of articles on the neurophysiology and therapeutic application of vibration in the 1970s. High-frequency vibration (100 to 300 Hz or cycles per second) applied to the muscle or tendon elicits a reflex response referred to as the tonic vibratory response. Tension within the muscle will increase slowly and progressively for 30 to 60 seconds and then plateau for the duration of the stimulus.187 Some researchers found that at cessation of the input the contractibility of the muscle was enhanced for approximately 3 minutes.187,188 The discrepancy in the research may reflect the way the individual is using the input, both from a direct effect on the motor generator and from supraspinal modulation over the importance of the input, which may affect the overall learning and plasticity of the CNS. To facilitate hypotonic muscle, the muscle belly is first put on stretch, and then vibratory stimuli are applied.189 To inhibit a hypertonic muscle, the antagonistic muscle could be vibrated.185,189 The use of vibration can be enhanced by combining it with additional modalities such as resistance, position, and visually directed movement. Vibration also stimulates cutaneous receptors, specifically the Pacinian corpuscles, and thus can also be classified as an exteroceptive modality.190 Because of its ability to decrease hypersensitive tactile receptors through supraspinal regulation, local vibration is considered an inhibitory technique (it is also discussed later in the section on exteroceptor-maintained stimulus). Therapists have reported that vibration over acupressure points can modulate localized pain syndromes. It seems to trigger A delta exteroceptive fibers, which in turn dampen the effect of C fibers. (See Chapter 32 for more information on the treatment of pain.)
Farber111 summarized the use of vibration and clearly identified precautions that must be taken. Frequencies greater than 200 Hz can be damaging to the skin. We have found frequencies greater than 150 Hz to cause discomfort and even pain. Therefore it is recommended that vibrators registering 100 to 125 Hz be used. Most battery-operated hand vibrators function at 50 to 90 Hz.11 Frequencies less than 75 Hz are thought to have an inhibitory effect on normal muscle,187 although a study showed that some muscle groups, especially the lateral gastrocnemius, do respond positively to frequencies of 40 to 60 Hz.191 Another researcher192 studying vibration found similar results that frequencies of 50 Hz generated more neuromuscular facilitation than lower frequencies (30 Hz) when studying improvements in upper body resistance exercise performance. Cutaneous pressure is also known to cause inhibition, so if it is combined with a vibration technique that is being used to augment a muscle contraction, it can only serve to cancel the desired effects.
Amplitude or amount of displacement must also be considered when vibration is analyzed as a modality. It has been reported that high amplitude causes adverse effects, especially in clients with cerebellar dysfunction.186 Vibration is not recommended for infants because the nervous system is not yet fully myelinated and the vibration might cause too much stimulation. The reader is also cautioned about using vibration over areas that have been immobilized because of the underlying vascular tissue potential for clotting. Vibration on or near these blood vessels could dislodge a clot, causing an embolism. Vibration also needs to be used cautiously over skin that has lost its elasticity and is thin (e.g., that in older persons) because the friction itself from the vibration can cause tearing. The therapist must always keep in mind the environment and the functionality of an intervention procedure. The use of vibration may assist the client in contractions and somatosensory awareness, but it is an unnatural way to facilitate either system and thus needs to be removed as part of an intervention as soon as the patient demonstrates some sensory awareness and/or volitional control over a movement component.
Within the last decade the use of vibration of specific muscle groups of the neck has been studied in order to determine its effect on upright standing and the interaction with and without eyes open.179,180 These studies showed that by vibrating specific muscle groups, those muscles would actively contract and change the position of the head in space but that with eyes open the effect was minimized in relation to global postural control. A similar study examined the effect of vibration on various muscles within the lower extremities and how that affected various postural responses.191,193 These researchers found that different frequencies affected different muscle groups. The one consistent thing all studies have shown is that vibration does facilitate Ia muscle fibers, which in turn affect muscle contraction of the agonist receiving the vibration. Other sensory systems can assist or override the effect of vibration, but that is because of superspinal influence over motor generators.
Total-body vibration is currently being used to determine if it affects motor performance. Studies have shown that whole-body vibration can enhance motor performance in high-level athletes performing sprints and jumps,181,182 as well as improve trunk stability, muscle tone, and postural control in individuals after stroke while in geriatric rehabilitation.184 Its application for individuals with neurological dysfunction is inconclusive.194,195 Studies specifically directed toward the elderly again show promise, but further research is needed for specificity.196,197 Future research will need to determine the effect of total-body vibration when introduced to all populations of individuals with neurological dysfunction. At that time both amplitude and magnitude will need to be identified in order to replicate studies. Total-body vibration certainly falls under primarily proprioception but also could be classified under combined proprioceptive techniques or multisensory classification techniques because the input affects the muscle spindles, the joints, the vestibular system, and possibly the auditory system with the low frequency noise. And every time vibration is applied, the skin receptors will initially fire although most will adapt quickly to prolonged use of any stimuli.
The tendon.
The tendon receptors are specialized receptors located in both the proximal and the distal musculotendinous insertions. In conjunction with the stretch receptors, the tendon plays an important role in the mediation of proprioception.141,142,198–203
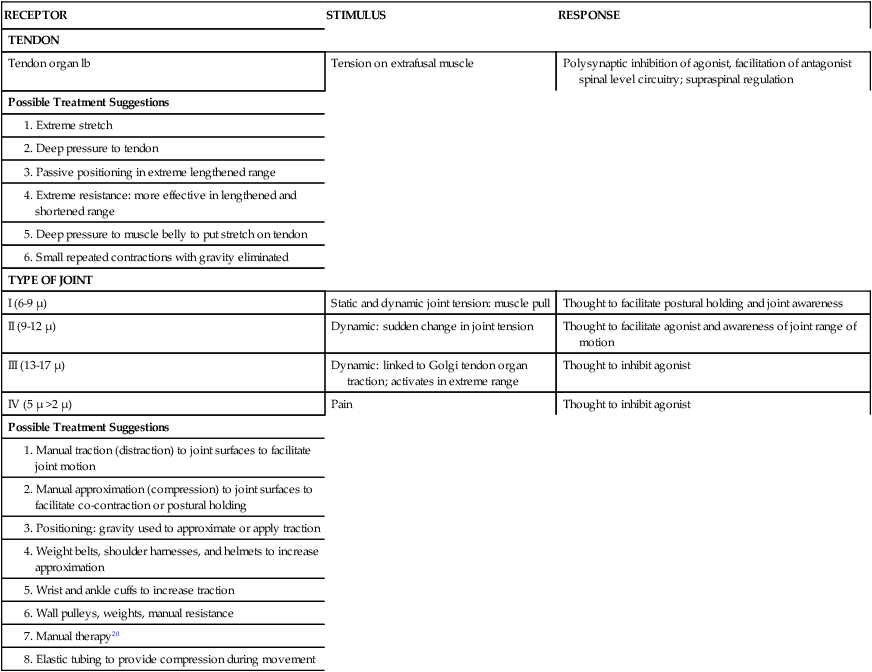
The principal role of the tendon is to monitor muscle tension exerted by the contraction of the muscles or by tension applied to the muscle itself. Research has demonstrated that the tendon is highly sensitive to tension and acts conjointly with the stretch receptors to inform higher centers of continuing environmental demands to modulate or change existing plans; these higher centers in turn regulate tonicity and the state of the motor pool.43,141 The tendon (Ib) signals not only tension but also the rate of change of tension and provides the sensation of force as the muscle is working.198 A fundamental difference between the tendon organ and the stretch receptors is that the stretch receptors detect length, whereas the tendon monitors tension and force. Sensory input from the stretch receptors and the tendon are mostly opposites.43,202 The stretch receptors regulate reciprocal inhibition, whereas the tendon modulates autogenic inhibition. Table 9-3 lists a variety of known treatment approaches that use the tendon to inform higher centers regarding needed change and regulation over spinal generators.
TABLE 9-3 
PROPRIOCEPTIVE RECEPTORS OF TENDONS AND JOINTS
| RECEPTOR | STIMULUS | RESPONSE |
| TENDON | ||
| Tendon organ lb | Tension on extrafusal muscle | Polysynaptic inhibition of agonist, facilitation of antagonist spinal level circuitry; supraspinal regulation |
| Possible Treatment Suggestions | ||
Inhibitory pressure.
Pressure has been used therapeutically to alter motor responses. Mechanical pressure (force), such as from cones, pads, or the orthokinetic cuff developed by Blashy and Fuchs,204 provided continuously is inhibitory. That pressure seems most effective on tendinous insertions. It is hypothesized that this deep, maintained pressure activates Pacinian corpuscles, which are rapidly adapting receptors. A variety of researchers have studied these receptors and their relationship to regulating vasomotor reflexes,205 modulating pain,206–210 and dampening other sensory system influence on the CNS.188,209
This inhibitory pressure technique also works when pressure is applied across the longitudinal axis of a tendon. The pressure is applied across the tendon with increasing pressure until the muscle relaxes. Constant pressure applied over the tendons of the wrist flexors may dampen flexor hypertonicity and elongate the tight fascia over the tendinous insertion (see Chapter 39 for additional information).
Pressure over bony prominences has modulatory effects. A common example is pressure on the medial aspect of the calcaneus, which dampens plantarflexors and allows contraction of the lateral dorsiflexor muscles. Pressure over the lateral aspect of the calcaneus also dampens calf muscles to allow for contraction of the medial dorsiflexor muscles.25 Localized finger pressure applied bilaterally to acupuncture points has been shown to relieve pain and reduce muscle tone.210–214 This technique has also been found to be particularly effective when used in a low-stimulus environment and when combined with deep breathing.
This combination of pressure (manually applied), environmental demands (low), and parasympathetic activity (slow, relaxed breathing) illustrates various systems interacting together to create the best motor response. The real world requires the client to respond to many environmental conditions while relaxed or under stress. Thus, once a client begins to demonstrate normal adaptable motor responses, the therapist needs to change the conditions and the stress level to allow the client to practice variability. That practice should incorporate motor error, especially error or distortions in the plan, yet still achieve the desired goal. As the client self-corrects, greater demand and variability should be introduced.215
Joint receptor approximation.
Approximation of the joint mimics weight bearing and facilitates the postural extensor system. Gravity creates approximation and its greatest force is produced down through the body in vertical postures. Approximation should help to stabilize any joint that is in a load-bearing situation by eliciting coactivation of the muscles around the joint in question. In standing, gravity creates approximation down through the entire spine, hips, knees, and ankles. When in a prone position on elbows, the load goes down again through the upper spine while simultaneous going down through the shoulder girdles of both arms. If a therapist increases that load by adding pressure down through the joints in question, then an augmented intervention has been added to the therapeutic environment. Using weight belts around the waist or a weighted vest on the trunk can facilitate the postural coactivation needed during standing or walking.216–218 At times, approximation can be used to heighten normal postural tone while simultaneously dampening excessive tone in the other leg. For example, clients who have CNS insult often have an imbalance in function within the two lower extremities. This can be very frustrating for the therapist because bringing the patient to standing to assist in regaining normal postural extension of one leg triggers the other into a strong extensor pattern, causing plantarflexion and inversion of that foot. One way to use approximation in treating both legs simultaneously might be to first bring the patient from sitting onto a high-low mat. Then the therapist can raise the mat high enough that the patient can be lowered into standing on the normal-functioning leg. At the same time the patient’s other leg can be bent at the knee, and that knee placed on a stool or chair. This allows approximation down through the entire leg that is in standing position while approximating the trunk, hip, and knee of the other leg in the kneeling position. The therapist can work on standing and weight shifting in one leg while dampening abnormal tone in the kneeling leg. As the kneeling leg starts to regain postural coactivation in its hip, postural function will often be felt in the knee and ankle.
One very effective way to apply approximation and resistance simultaneously is to use the product similar to a cut large elastic rubber band: Thera-Bands. The rubber material is attached under the heel on the right and left side; both ends of the band are brought up across the ankle and then crossed over the lower leg, once more over the back of the thigh, and then anchored onto a belt around the patient’s waist. A similar pattern can be used for the arm; the band is first placed across the palm and then crossed in the forearm and then the arm. Finally one end is brought across the upper chest and the other comes around from the back of the arm. Then the two ends of the band are tied together across the neck.These techniques can be graded by the elasticity of the material.219–221
Traction and distraction.
One or more joints are distracted by a force that causes it or them to separate or pull apart, similar to the swing phase of the leg during ambulation or the arms in a reciprocal pattern to each leg. This distraction of the joint receptors also puts stretch on the muscles, which combines to facilitate the pattern into which the limb is moving. Simultaneously, distraction dampens the antagonistic movement pattern, which allows the agonist movement to continue. A therapist will often use manual traction to get relaxation of hyperactive extensor muscles or for limited mobility.222 Often therapists do not think of the traction when applying resistance to a limb. For example, a mistake made is placing ankle weights to facilitate limbs that are ataxic. Ataxia is an imbalance in coactivation and smooth movement of both agonist and antagonist muscle groups.223 The weight itself slows down the excessive movement by the resistance. However, weight on the ankle creates traction that will facilitate only the flexor group and often creates an additional imbalance in the ataxic leg.224 When the weights are removed, the patient often is more ataxic.
Combined proprioceptive input techniques.
Many techniques succeed because of the combined effects of multiple inputs. Some of these combined techniques include jamming; ballistic movements; total-body positioning; PNF patterns; postexcitatory inhibition (PEI) with stretch, range, rotation, and shaking; heavy work patterns; Feldenkrais (see Chapter 39)225–227; and manual therapy.20,208,228
Ballistic movement.
Ballistic movements are effective because of their combined proprioceptive interaction. The client is asked to initiate a movement, such as shoulder flexion while prone over a table with the arm hanging over the side. This component is volitional, but the client then maintains a passive role. As the patient relaxes, the movement patterns become automatic. The physiology behind the automatic movement is easy to understand. As the muscle approaches the shortened range, the amount of ongoing gamma afferent activity decreases. Thus both the agonist alpha motor neuron bias and the inhibition of Ia and II receptors of the antagonistic alpha motor neurons decrease. Simultaneously, the antagonistic muscle is being placed on more and more stretch. This stretch, as well as the lack of inhibition on the antagonistic alpha motor neurons, will encourage the antagonistic muscle to begin contraction and reverse the movement pattern. The tendon organs also play a key role in ongoing inhibition. As the muscle approaches the shortened range and tension on the tendon becomes intense, the tendon organ increases its firing, thus inhibiting the agonistic muscle in the shortened range while facilitating the antagonistic muscle. This technique is highly movement oriented, and the traction applied by gravity to the shoulder joint while swinging the arm further facilitates the movement. These ballistic movements are part of the program generators within the spinal system that facilitate reciprocal movements of the limb. As the client performs the movement, there is little need for conscious attention to drive the movement; it will run automatically. The role of the Ib fibers during this open chain or movement pattern is definitely different from its role in a closed chain or weight-bearing environment.199 Supraspinal influence over programmed activity also plays a role in the effectiveness of this treatment.229 The specific rationale for why ballistic movements have functional carryover may be explained by recent research into cerebellar function and the importance of mechanical afferent input in regulation of movement (see Chapter 21).
Total-body positioning.
Total-body positioning implies the use of positioning and gravity to dampen afferent activity on the alpha motor neurons and thus cause a decrease in tone, or relaxation.230 Today, the rationale for why relaxation of striated muscle occurs after this treatment implies that the effect of the flexor reflex afferents is being dampened by a combination of input and interneuronal activity. These changes in the state of the muscle tone will not be permanent and will revert to the original posturing unless motor learning and adaptation within the central programmer occur simultaneously. Thus for this treatment to effect permanent change, a large number of systems need modification. This modification can be augmented by techniques that facilitate autogenic inhibition, reciprocal innervation, labyrinthine and somatosensory influences, and cerebellar regulation over tone.231 Changing the degree of flexion of the head also alters vestibular input and the state of the motor pool. But again, the CNS of the client needs to be an active participant and will ultimately determine whether permanent learning and change are programmed.
Proprioceptive neuromuscular facilitation.
To analyze and learn the principles, techniques, and patterns that constitute PNF, a total approach to treatment, refer to the texts by Adler,232 Voss,233 and Sullivan and colleagues.29 This approach is being used extensively for patients with musculoskeletal and neuromuscular problems, with research on this method encompassing more populations with lower motor neuron and musculoskeletal problems than upper motor neuron lesions.154,228,234–242 When proprioceptive techniques are packaged in specific movement patterns, it may be referred to as PNF. When individual proprioceptive techniques are discussed alone, the specific sensory function is being acknowledged, and these techniques can be integrated into many rehabilitation intervention strategies.
Postexcitatory inhibition with stretch, range, rotation, and shaking.
The concept of PEI is based on the action potential or electrical response pattern of a neuron at the time of stimulation and on the entire phase response until the neuron returns to normal. At the time of stimulation, the action potential will build and go through an excitatory phase. The neuron then enters an inhibitory phase or refractory period during which further stimulation is not possible. This is referred to as the PEI phase or postsynaptic afferent depolarization.111 These phase changes are extremely short and, in normal muscle, asynchronous with respect to multiple neuronal firing. In a hypertonic muscle more simultaneous firing occurs. When the muscle is lengthened, and thus tension is created, more fibers will be discharged. It is hypothesized that if the hypertonic muscle is placed at the end of its spastic range and a quick stretch is applied and held, then total facilitation followed by total inhibition will occur because of PEI. As the inhibition phase is felt, the therapist can passively lengthen the spastic muscle until the facilitatory phase sets in repolarization. At that time the clinician holds the lengthened position. Increased tone will ensue, followed by inhibition and continued lengthening. Holding the range (not allowing concentric contraction during the excitatory phase) is critical. If the muscle is held as the tone increases, the resistance and stretch are then maximal and probably further facilitate the inhibitory phase.
Feldenkrais.
The Feldenkrais concepts225,226 of sensory awareness through movement place emphasis on relaxation of muscles on stretch, and distracting and compressing joints for sensory awareness. Both techniques reflect combined proprioceptive techniques. Taking muscles off stretch slows general afferent firing and thus overload to the CNS. Compression and distraction of joints enhance specific input from a body part while simultaneously facilitating input of a lesser intensity from other body segments. This combined proprioceptive approach enhances body schema awareness in a relaxed environment. It also integrates empowerment of the client by use of visualization and asking for volitional control. (See Chapters 27 and 39 for additional information.)
Manual therapy, specifically maitland’s.
“The peripheral and central nervous systems need to be considered as one because they form a continuous tissue tract.”208,225,243–246 Manual therapy or mobilization of joint or soft tissue structures is not specific to orthopedic conditions, nor are neurological treatment principles ineffective on orthopedic patients. Regardless of the diagnosis or pathological body system leading to joint immobility, the functional consequences can be synonymous. Joint immobility can cause the peripheral nerves to lose their adaptability to change in the length of the nerve bed. This change in neural elasticity then creates additional problems in connective tissue function, which in turn may affect the function of the motor system’s control over the musculoskeletal component.228,247 For this reason alone, discussion of musculoskeletal mobilization needs to be included in this section as a component of classification.
“Pathological processes may interfere with both of these mechanisms: extraneural pathology will affect the nerve/interface relationship and intraneural pathology will affect the intrinsic elasticity of the nervous system.”247 Patient complaints of pain that limits functional movements constitute the primary reason clients are referred to a therapist for a musculoskeletal evaluation. During the physical examination, tension tests can be used to determine the degree of pain and joint limitation, to differentiate between somatic and radicular symptoms, and to identify adverse neurophysiological changes in the PNS.247 “The increased muscle tone (in a peripheral injury) is considered to be a protective mechanism for the inflamed tissue.”248 This increase in tone may be caused by a dampening of presynaptic activity of the flexor reflex afferent by supraspinal mechanisms. This same mechanism may be triggered by a CNS injury. The difference between the orthopedic patient and the neurological patient may be the trigger to the CNS. In a central lesion the motor generators are often not adequately maintained after injury, which results in hypotonicity. The hypotonicity causes peripheral instability, stretches peripheral tissue, and potentially causes peripheral damage. In both orthopedic and neurological cases, there is peripheral instability, the first the result of peripheral damage and the second the result of hypotonicity. The CNS response to the instability may be the same: an increase in muscle tone by dampening of presynaptic inhibition. A decrease in presynaptic inhibition on incoming afferents would cause an increase in spinal generator activity. With an isolated musculoskeletal problem and an intact CNS, the motor system would have the adaptability and control to modulate the spinal generators and isolate only those components in which an increase in tone might directly affect the problems. The client with CNS involvement may lose some of the flexibility of the motor system’s control over the pattern generators, and thus high-tone synergistic patterns may develop.
In either case, the peripheral system needs to be evaluated and intervention provided when necessary. Tension tests look for adverse responses to physical examination of neural tissues. These adverse responses are muscle tone increases as a result of painful provocation of sensitized neural tissue nociceptors attempting to prevent further pain by limiting the movement of the neural tissue.248 Pain increases tone and leads to limited range of passive movement.248,249 Pain-free range suggests CNS sensitivity to the large, highly myelinated alpha fibers and functions in a discriminatory manner. Pain range encompasses the degree of joint motion where neural length, as well as nociceptors in the skin, fascia, muscles, and joints, plays a primary role in CNS attention and protection. Inflammation of neural tissue can also cause the nociceptors to become hypersensitized or more reactive to mechanical or chemical changes. This is particularly true in the joint when the nociceptors react significantly to movement at the end ranges.248
Treatment will be based on the degree of immobility, the pain range, the site of the irritability, and the degree of pain. Butler228 not only looks at joint problems but also considers many joint problems as having adverse neural dynamics (tension on the PNS). Treatment still incorporates Maitland’s grades of passive movement, but with consideration across the length of the neural tissue across multiple joints.
Butler247,250 divides treatment of the joint into three categories: limitations, pain, and adverse mechanical tension. When analyzing selective nervous system mobilization as identified by Butler, the therapist needs to mobilize the nervous system and its surrounding fascia rather than stretching it. These techniques may be either gentle (grade I) or strong (grade IV), through the range (grades II and III), or at end range only (grade IV). Different disorders (irritable compared with nonirritable) will require different treatment approaches (Figure 9-3).
Exteroceptive or cutaneous sensory system
Differentiation of receptor site as augmented intervention.
A list of treatment techniques using the exteroceptive (tactile) input system as their primary mode of entry can be found in Table 9-4.
TABLE 9-4 
EXTEROCEPTIVE INPUT TECHNIQUES
| RECEPTORS | STIMULI | RESPONSE* |
| Free nerve endings: C + A fibers | Pain, temperature, touch | Seem to protect and alert, perception of temperatures, protective withdrawal |
| Hair follicles | Mechanical displacement of hair receptors | Increased tone of muscle below stimulus site |
| Merkel disk | Touch: pressure receptors | Touch identification |
| Meissner corpuscles | Discriminative touch | Postural tone; two-point discrimination |
| Pacinian corpuscles | Deep pressure and quick stretch to tissue, vibration | Position sense, postural tone and movement |
| Ruffini corpuscles | Touch mechanoreceptor | Touch and spatial discrimination |
| SUGGESTED TREATMENT PROCEDURES USING CUTANEOUS STIMULI | ||
| Quick Phasic Withdrawal | ||
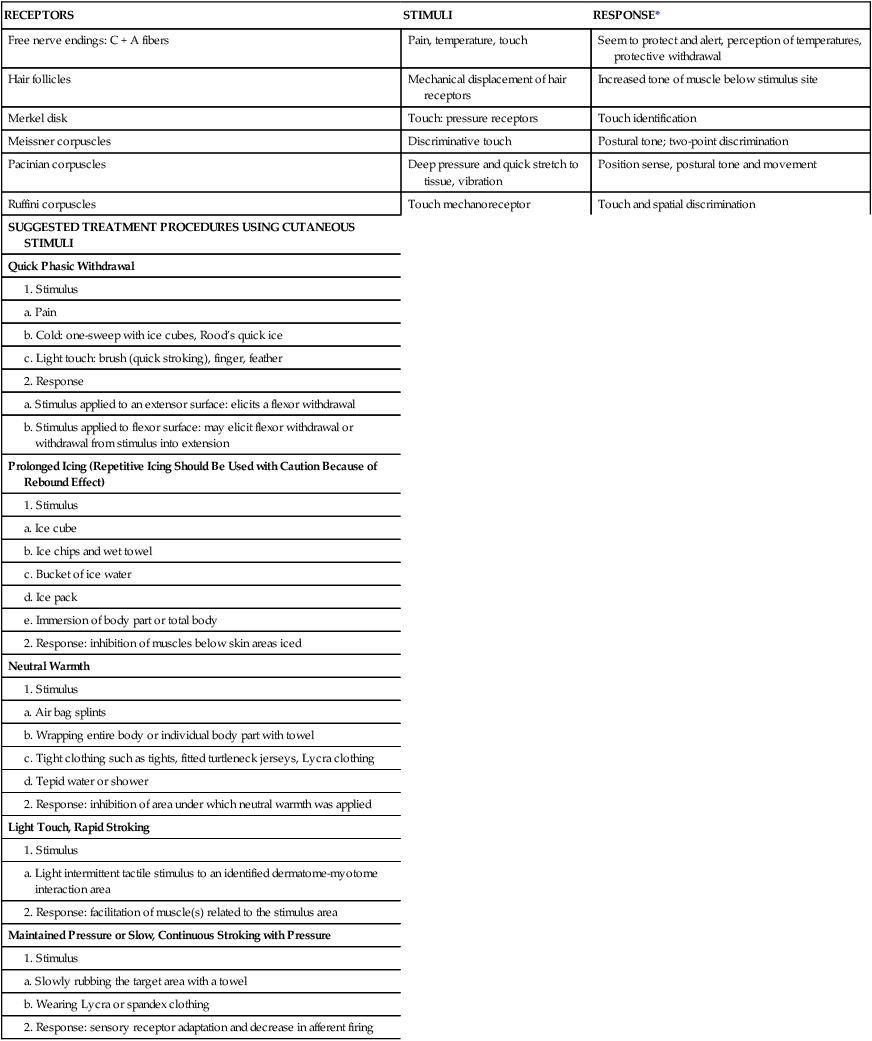
*Response: adaptation of many cutaneous receptors to stimulus, thus decreasing exteroceptive input, decreasing reticular activity, and decreasing facilitation of muscles underlying stimulated skin.
Treatment alternatives using the exteroceptive system.
Quick phasic withdrawal.
The human organism reacts to painful or noxious stimuli at both conscious and unconscious levels. If the stimulus is brief and of noxious quality, it will elicit a protective reaction of short duration with use of the long-chain spinal reflex loops. Simultaneously, afferent impulses ascend to higher centers to evoke prolonged emotional-behavioral responses. Stimuli such as pain, extremes in temperature, rapid movement, light touch, and hair displacement are the most likely to cause this reaction by activating free nerve endings. These stimuli are perceived as potentially dangerous and communicate directly with the reticular-activating system and nonspecific thalamic nuclei. These structures have diffuse interconnections with all regions of the cerebral cortex, ANS, limbic system, cerebellum, and motor centers in the brain stem. Research has shown that children who exhibit hyperactive withdrawal reactions also develop negative emotional reactivity and show significantly more avoidance behavior and in time show right frontal asymmetry.251 These alerting stimuli have been linked to motor seizures in critically ill patients.252 As indicated by these research studies, therapists need to be aware of these potential responses, especially in patients with severe neurological insult that has resulted in a lower level of consciousness. These low-functioning clients cannot express their feelings nor how their nervous system is reacting to the input. Thus therapists need to be very aware of any motor response a patient may express and try to avoid using stimuli that might trigger these avoidance behaviors. From observance of the behavior of clients with chronic pain, these responses seem to become habitual and may lead to somatosensory remapping, making it hard to differentiate protective from discriminatory information. Thus, any movement or touch triggers pain. Patients need to be taught to discriminate between tightness and true pain, and therapists need to feel when the muscle response has shifted from muscle gliding to muscle restriction. Therapists need to gain trust, and one way is to not elicit a lot of pain. For example, if a therapist tells a patient to say something when it hurts, and the patient says, “Now,” the therapist should never respond with “Well, just a little more.” In that instant the patient has learned that the therapist lied (because the patient was told to tell the therapist when it hurt, suggesting that the therapist would stop then) or that the therapist is a masochist. If the therapist had stopped when the patient said that it hurt, the patient would then know that he does not need to tell the therapist to stop 10 degrees before it hurts because the therapist is not going to range him that 10 extra degrees. Often the therapist will find that without any effort the patient now has that extra range and has no need to splint the limb because it is not going to hurt to have therapy.
There are some real therapeutic limitations to using stimuli that “load” the spinothalamic system. A painful stimulus will be excitatory to the nervous system and produce a prolonged reaction after discharge. According to Wall’s gate-control theory,253–257 all sensory afferent neurons converge and synapse in the dorsal horn in an area called the substantia gelatinosa. Curiously, the large, more discriminatory fibers do outnumber the small fibers.258 Therefore, physical activity, frequent positioning, deep pressure, and proprioceptive and cutaneous stimulation should cause enough impulses to converge on cells within the substantia gelatinosa to close the gate and thus block transmission of pain messages to the brain. Studies have demonstrated that physical activity (types of physical stress) stimulates the production of endorphins, which in turn release opiate receptors and act as the body’s own morphine for pain control20,212,259–262 (see Chapters 18 and 32).
Short duration, high-intensity icing.
Cold is another stimulus that the nervous system perceives as potentially dangerous. The use of ice as a stimulus to elicit desired motor patterns is an early technique developed by Rood. Her technique was referred to as repetitive icing. An ice cube is rubbed with pressure for 3 to 5 seconds or used in a quick-sweep motion over the muscle bellies to be facilitated. This method activates both exteroceptors and proprioceptors and causes a brief arousal of the cortex. This method can produce unpredictable results. Although initially a phasic withdrawal pattern generator response will be activated immediately after the reflex has taken place, the “rebound” phenomenon deactivates the muscle that has been stimulated and lowers the resting potential of the antagonistic muscle.263 Therefore a second stimulus to the same dermatome-myotome neural network may not elicit a second response. But, because of reciprocal innervation, the antagonistic muscle may effect a rebound movement in the opposite direction. Icing may also cause prolonged reaction after discharge because of the connections to the reticular system, limbic system, and ANS. Thus the ANS would be shifted toward the sympathetic end. Too much sympathetic tone causes a desynchronization of the cortex.264 Although the resting state of the spinal generator may be altered briefly, if the heightened state persists the cause is most likely fear or sympathetic overflow (see Chapter 5). This state is destabilizing to the system and most likely will not lead to any motor learning. Because of unpredictable response patterns to Rood’s repetitive icing, this technique is seldom used.
The therapist is cautioned not to use short-duration, high-intensity icing to the facial region above the level of the lips, to the forehead, or to the midline of the trunk. These areas have a high concentration of pain fibers and a strong connection to the reticular system.10,265
Ice should not be used behind the ear because it may produce a sudden lowering of blood pressure.266 The therapist should also avoid using ice in the left shoulder region in patients with a history of heart disease because referred pain from angina pectoris manifests itself in the left shoulder area, indicating that the cold stimulus might cause a reflexive constriction of the coronary arteries.267 In addition, the primary rami located along the midline of the dorsum of the trunk have sympathetic connections to internal organs. The cold stimulus may alter organ activity and perhaps produce vasoconstriction, causing increased blood pressure and reduced blood supply to the viscera.268,269
Brief administration of ice can have beneficial effects if the nervous system’s inhibitory mechanisms are in place. For instance, in children with learning disabilities or adults with sensorimotor delays, the application of ice to the palmar surface of the hands will cause arousal at the cortical level because of the increased activity of the reticular activating system. This arousal response presumably produces increased adrenal medullary secretions, resulting in various metabolic changes. Therefore icing should be used selectively. If the patient has an unstable ANS, icing should be eliminated as a potential sensory modality.270
Prolonged use of ice.
Physicians have used therapeutic cold for the treatment of individuals with high fever and/or intracranial pressure with the intent of reducing the body temperature or brain swelling to prevent brain damage.271 This procedure is done with cooling pans or blankets. Whole-body cryotherapy has been used to reduce inflammation and pain and overcome symptoms that prevent normal movement. This type of therapy consists of the use of very cold air maintained for 2 minutes in cryochambers. A recent study looked at this type of therapy for injured athletes. It was found that the procedure did not cause harm to the individual.272 This approach does not seem realistic for use in occupational or physical therapy clinics.
A variety of approaches that incorporate prolonged icing techniques have been used in therapy clinics for decades. The PNF approach may be the most common.19 Inhibition of hypertonicity or pain is the goal for the use of any of these methods. With prolonged cold the neurotransmission of impulses, both afferent and efferent, is reduced. Simultaneously the metabolic rate within the cooled tissue is reduced (see Chapter 32). Caution must be exercised with regard to the use of this modality. However, for effective treatment results, the client (1) should be receptive to the modality, (2) should be able to monitor the cold stimulus (sensory deficits should not be present), and (3) should have a stable autonomic system to prevent unnecessary adverse effects of hypothermia. Research of the last decade has consistently shown that cryotherapy is an effective tool for reducing pain and has helped individuals regain integration of axial musculature after neurological insults.273–276 Individuals of all ages seem to respond similarly, which allows therapists to use this therapeutic tool across generations.277
Ice immersion of the contralateral limb was used decades ago in order to get a reflexive decrease in temperature in the affected limb. It was believed that this intralimb reflex was an effective way of treating pain without directly treating the limb. Recent research has validated that belief.278
Ice massage is another form of prolonged icing and is often used to treat somatic pain problems.279 It is also used over high-toned muscles to dampen striated muscle contractions. Caution must be used when eliminating pain without correcting the problem causing pain. For example, if instability causes muscle tone and pain, then icing might decrease pain while causing additional joint instability and potential damage. The end result would be an increase, not a decrease, in pain and motor dysfunction.
Neutral warmth.
Like icing, neutral warmth alters the state of the motor generators, either directly or indirectly through afferent input. According to Farber,12 the length of application depends on the client. A 3- to 4-minute tepid bath may create the same results as a 15-minute total-body-wrapping procedure. As with any input procedure, the effects should be incorporated into the therapeutic session to maximize the results and promote client learning. The Johnstone approach uses air splints effectively as a neutral warm treatment intervention while clients work on functional activities.17 If neutral warmth is applied as an isolated intervention, the client may feel relaxation or a decrease in discomfort, but neuroplastic CNS changes are unlikely, owing to the lack of repetition, attention, and error correction by the client during activities. A recent study looked at blood pressure, heart rate, and other autonomic mechanisms in subjects using compression hose. The researchers did not look at neutral warmth as a mechanism to maintain a homeostatic state of the nervous system. Yet the use of compression hose does create a state of neutral warmth, and the link to homeostasis can easily be made.280
Maintained stimulus or pressure.
Maintained pressure approaches using elastic stockings, tight form-fitting clothing (e.g., wet suits, expanded polytetrafluoroethylene [Gore-Tex] biking clothing), air splints, and other techniques can be incorporated into a client’s daily activity without altering lifestyle. The use of TheraTogs in children with various hyperactivity conditions has become an accepted therapeutic tool. They add some resistance, some support, and maintained pressure.281 TheraTogs have also been shown to be effective in assisting individuals with hemiplegia to regain abductor control.282
Light discriminatory touch.
Once an individual can discriminate light touch both for protection and for discriminatory learning, a lot of therapeutic tools become available to the therapist. Using boxes with an opening so the individual can insert a hand and arm but cannot see what is inside, a patient can work on discriminating textures, objects, letter, numbers, and so on while working on higher-order processing. Once this touch has been integrated, the patient can also use light touch to determine balance, position in space, and various other types of perceptual tasks.283