CHAPTER 15 Interscalene block
Clinical anatomy
The cervical nerves exit from the cervical spine through gutters in the transverse processes that run in an anterolateral direction, immediately posterior to the vertebral artery. The cervical nerves enter a facial space in the posterior triangle of the neck between the anterior and middle scalene muscles called the interscalene compartment (Fig. 15.1). The interscalene block is performed at the level of the cricoid cartilage (C6). Important anatomic relations (Fig. 15.2) include the external jugular vein, which crosses the posterior border of the sternocleidomastoid muscle at this point, the phrenic nerve on the anterior scalene muscle, and the vertebral artery.
Surface anatomy
The main landmarks for the interscalene block (Fig. 15.3) include clavicle; sternal notch; cricoid cartilage; sternal and clavicular heads of the sternocleidomastoid muscle – these can be accentuated by asking the patient to perform a head lift; interscalene groove – both scalene muscles descend to the first rib and can be identified by asking the patient to inhale deeply, because they contract before the sternocleidomastoid muscle; and the external jugular vein –which can be accentuated by asking the patient to perform a Valsalva maneuver. A skin marker should routinely be used to delineate the anatomic structures before performing the block.
Sonoanatomy
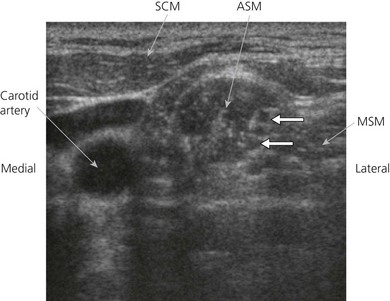
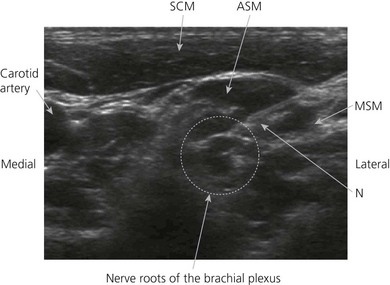
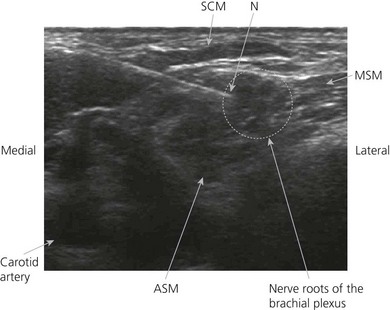
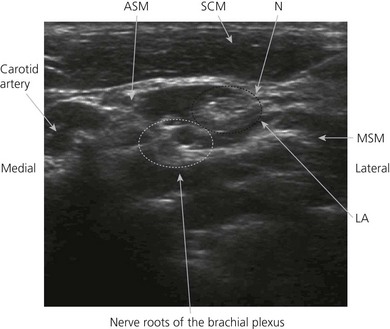
Perform a systematic anatomical survey from medial to lateral and superficial to deep. The carotid artery and internal jugular vein are seen medially. Medial to the vessels, the thyroid and trachea are identified. The ultrasound-guided intrascalene block is performed at the lateral border of the clavicular head of the sternocleidomastoid at the level of the cricoid cartilage. Here the brachial plexus is a superficial structure and a high frequency ultrasound transducer (6 to 13 MHz) is used. A high frequency transducer allows good visualization of structures to a depth of 4–5 cm. The ultrasound transducer is placed in an axial oblique plain (Fig. 15.4) and the most superficial structure consistently encountered is the sternocleidomastoid muscle. This appears as a triangular structure with the apex pointing laterally. Immediately deep to the sternocleidomastoid muscle are the anterior and middle scalene muscles. These can be accentuated by asking the patient to sniff. The roots of the brachial plexus appear between these two muscles in the interscalene groove. At this level it is common to identify between one and five hypoechoic structures (roots or trunks) and, depending on the position of the ultrasound transducer, these may appear oval or round. The brachial plexus at this level lies at a depth of around 1 cm from the skin (Fig. 15.5).
Technique
Landmark-based approach
The patient is placed in the supine position with the head facing away from the side to be blocked. The patient is asked to elevate the head slightly to bring the clavicular head of the sternocleidomastoid muscle into prominence. The palpating finger is placed behind the sternocleidomastoid muscle and the patient is instructed to end the head lift (Fig. 15.6). The finger now lies on the belly of the anterior scalene muscle, and with lateral movement of the finger to the lateral edge of this muscle, the groove between the anterior and middle scalene muscles (interscalene groove) is encountered (Fig. 15.7). The injection site in the interscalene groove lies at the level of the cricoid opposite the transverse process of C6 (Chassaignac tubercle).

Figure 15.6 Locating the interscalene groove. The palpating fingers are placed deep to the sternocleidomastoid muscle.
The needle insertion point is infiltrated with local anesthetic using a 25-G needle. A 35–50-mm 21-G insulated needle is used. The index and middle fingers of the palpating hand should be firmly seated in the interscalene groove. To assure stability of both hands, all fingers not in use should be resting on the neighboring structures. The direction of needle insertion runs inward, slightly dorsally, and 30–40° caudally (backward, inward, and downward; Fig. 15.8). This needle direction takes into account the orientation of the gutter of the transverse processes of the cervical vertebrae, on which the cervical roots lie. It also acts as a safety technique to decrease the risk of intervertebral needle insertion. The stimulating current is set at 1.0 mA, 2 Hz, and 0.1 ms. The needle is advanced slowly until the appropriate muscle response is obtained: shoulder, elbow, index finger, or thumb movement. The needle position is adjusted while decreasing the current to 0.35 mA with maintenance of the muscle response.
Incremental injections of local anesthetic (40 mL) are made with repeated aspiration. This volume is sufficient for an adequate block of the brachial plexus and the caudal part of the cervical plexus (Fig. 15.9). Digital pressure is applied proximal to injection (Fig. 15.10) to promote distal spread of local anesthetic; this is to facilitate reaching the lower roots of the plexus. The lower roots of the plexus may not be anesthetized due to the proximal injection site with this technique.
Ultrasound-guided approach
Intravenous access, electrocardiogram (ECG), pulse oximetry and blood pressure monitoring are established. Maximized comfort for the operator and patient is an important step in pre-procedure preparation. For the ultrasound-guided interscalene block, the patient is placed in the supine position with the head turned to the side opposite that to be blocked. The operator stands or sits adjacent to the side to be blocked. The ultrasound screen, transducer, needle, and plane of imaging should all be placed in one view for the operator. For the interscalene block, the ultrasound screen is placed below the shoulder on the side to be blocked (Fig. 15.11). Room lights may be turned down to enhance image viewing. The operating lights can be used to maintain some working lighting in the background. The patient is asked to raise their head to identify the interscalene groove.
Developing and maintaining a predetermined basic scanning routine is of enormous help in improving operator confidence and success. The trachea, common carotid and internal jugular veins and sternocleidomastoid muscle are identified. The ultrasound transducer is moved laterally to identify the lateral edge of the sternocleidomastoid muscle. Beneath this muscle edge, the anterior and middle scalene muscles lie with the roots of the brachial plexus between (Fig. 15.5). The patient can be asked to sniff to identify the scalene muscles. Moving the transducer down the neck facilitates identification of the brachial plexus roots. The roots will appear as large hypoechoic (dark) structures.
A skin wheal of local anesthetic is raised at the lateral aspect of the ultrasound transducer. The needle bevel should face the active face of the transducer to improve visibility of the needle tip. A free-hand technique rather than the use of a needle guide is preferred. A 21-GA × 50-mm insulated needle (Pajunk, Geisingen, Germany; or B. Braun, Bethlehem PA) is inserted parallel to the axis of the beam of the ultrasound transducer (Fig. 15.12). The needle is attached to sterile extension tubing, which is connected to a 20-mL syringe and flushed with local anesthetic solution to remove all air from the system. The operator can slide and tilt the transducer to maintain the needle tip within the plane of imaging as much as possible. The needle tip is slowly advanced under ‘real-time’ imaging until the needle reaches the side of the target neural structures (Fig. 15.13). The operator can slide and tilt the transducer to maintain the needle tip within the plane of imaging as much as possible. Manipulation of the transducer or redirection of the block needle may be necessary to bring the needle tip into the plane of imaging.
The final needle position can be further confirmed with the use of a nerve stimulator (Stimplex; B. Braun, Bethlehem, PA). Characteristic motor activity in the forearm and hand is seen. An alternate method of needle insertion for the interscalene block can be from the medial aspect of the ultrasound transducer (Fig. 15.14). During the slow serial injection of the local anesthetic solution, the spread of the solution can be indirectly confirmed by interscalene space distention and enhanced nerve borders (Fig. 15.15). However, if appropriate local anesthetic is not visualized after a small volume of solution (0.5 to 2 mL) has been injected, the needle tip should be repositioned. Typically, smaller volumes of local anesthetic solution are required for ultrasound-guided interscalene blocks compared to non-guided techniques. The volume of solution injected is determined by the spread pattern observed. The needle is readjusted to allow complete encirclement of the nerve roots with local anesthetic. Typically in adults, 20 mL of local anesthetic solution is used. Local anesthetic appears as a hypoechoic image.
Adverse effects
Clinical pearls
Borgeat A, Ekatodramis G, Kalberer F, et al. Acute and nonacute complications associated with interscalene block and shoulder surgery: a prospective study. Anesthesiology. 2001;95:875-880.
Chan VWS. Applying ultrasound imaging to interscalene brachial plexus block. Reg Anesth Pain Med. 2003;28(4):340-343.
Kapral S, Greher M, Huber G, et al. Ultrasonographic guidance improves the success rate of interscalene brachial plexus blockade. Reg Anesth Pain Med. 2008;33(3):253-258.
Lehtipalo S, Koskinen LO, Johansson G, et al. Continuous interscalene brachial plexus block for postoperative analgesia following shoulder surgery. Acta Anaesthesiol Scand. 1999;43:258-264.
Long TR, Wass CT, Burkle CM. Perioperative interscalene blockade: an overview of its history and current clinical use. J Clin Anesth. 2002;14:546-556.
Perlas A, Chan VWS, Simons M. Brachial plexus examination and localization using ultrasound and electrical stimulation: A volunteer study. Anesthesiology. 2003;99:429-435.
Winnie AP. Interscalene brachial plexus block. Anesth Analg. 1970;49:455-466.