27 Interscalene and Supraclavicular Blocks
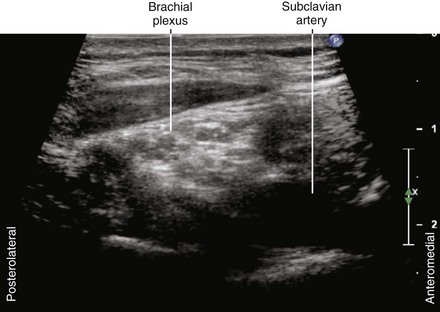
The first use of ultrasound to guide regional block was for brachial plexus block above the clavicle.1 These pioneers used an offline Doppler technique to mark the position of the subclavian artery as a surrogate landmark of the brachial plexus. Although today there may be many criticisms of this technique, their results were impressive: a 98% success rate with no complications.
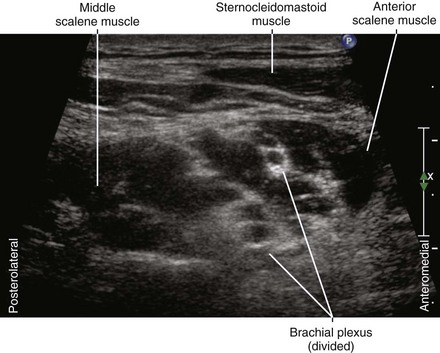
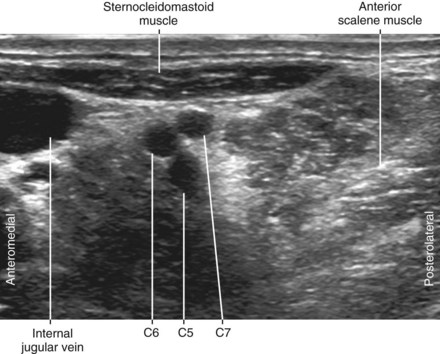
Variations in brachial plexus anatomy with respect to the scalene muscles are common. The cephalad components of the plexus (in particular, the C5 and C6 ventral rami) often pass over or through the anterior scalene muscle. This may pose a problem for nerve stimulation–based approaches to brachial plexus blocks above the clavicle. The incidence of scalene muscle anomalies is similar for sonography of volunteers and in cadaveric dissections, suggesting that ultrasound can accurately detect these anomalies.2
Cervical ribs are relatively uncommon, occurring in about 0.5% of the population.3,4 Most cervical ribs are partial (incomplete) and therefore do not pose a problem. However, if the cervical rib is sufficiently large, transducer manipulation can be difficult, and acoustic shadowing by the bone obscures imaging of the brachial plexus.
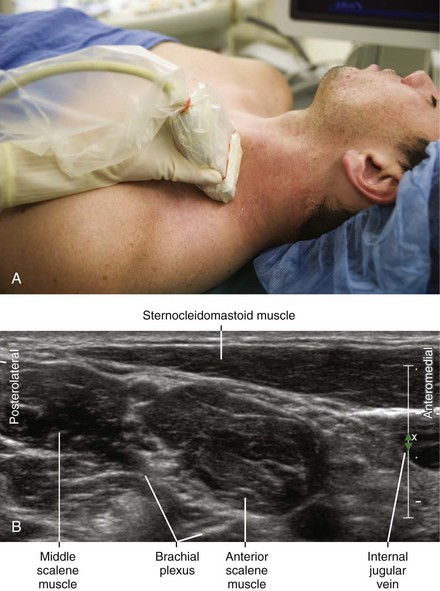
Suggested Technique
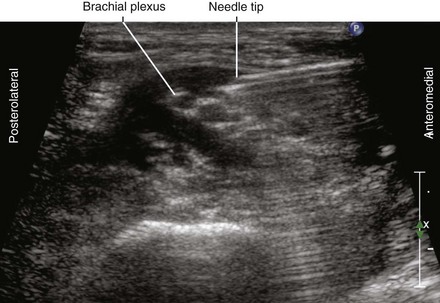
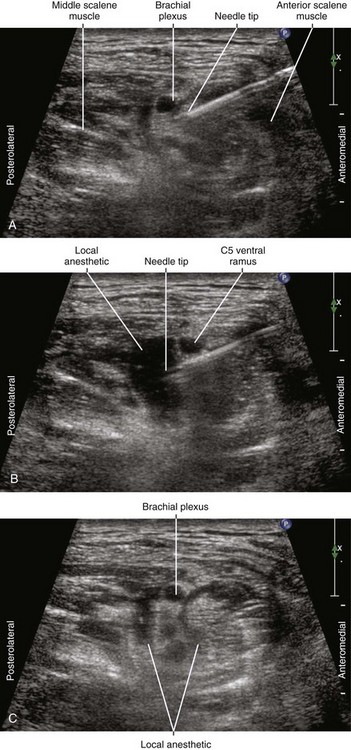
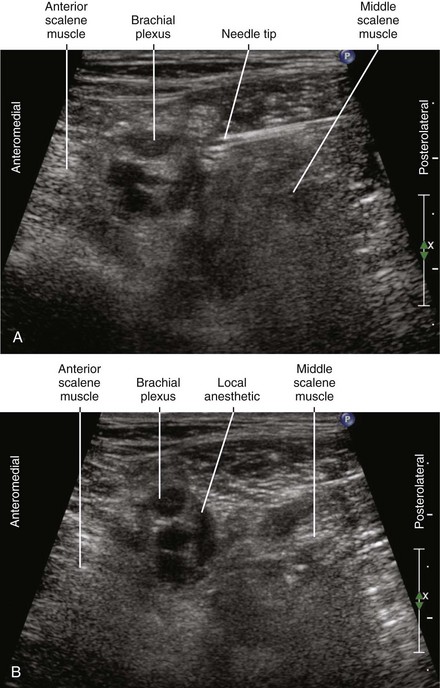
Most authors recommend a multiple injection technique to ensure complete plexus anesthesia. With this approach the initial aim of the needle is deep (under the more caudal elements of the plexus) so that the brachial plexus rises closer to the skin surface with the injection of local anesthetic. This makes the subsequent needle passes easier to perform. The needle tip should be positioned adjacent to the components of the brachial plexus for injection within the interscalene groove.5 Inferior trunk sparing occurs less often with this multiple injection ultrasound technique compared with nerve stimulation–based approaches to interscalene block.6
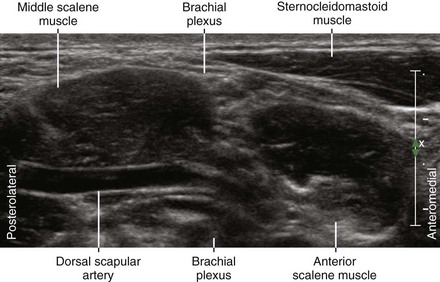
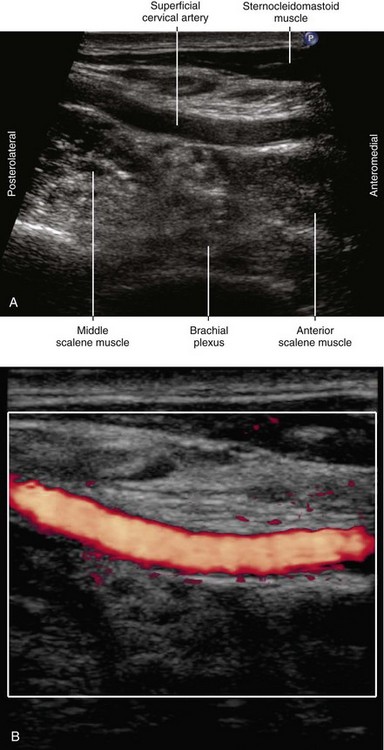
The anatomy of the posterior triangle of the neck is complex. Nerves close to the brachial plexus, and therefore potentially in the needle path, include the phrenic nerve, dorsal scapular nerve, and spinal accessory nerve. The phrenic nerve lies medial to the brachial plexus and travels over the anterior scalene muscle toward the midline as it descends into the chest. The dorsal scapular nerve is a branch of the brachial plexus that is often observed lateral to the brachial plexus within the middle scalene muscle. The spinal accessory nerve is difficult to image but lies lateral to the brachial plexus within the posterior triangle of the neck.7
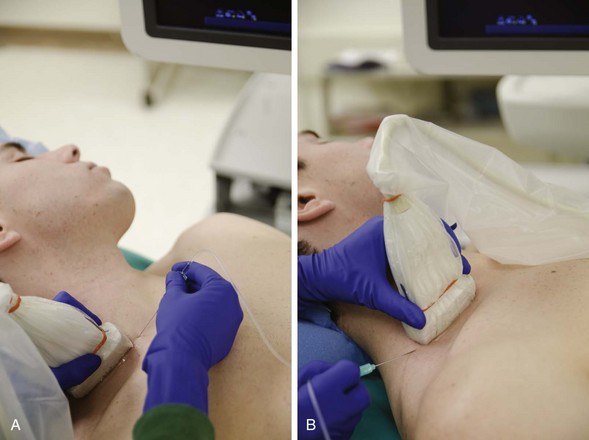
A sterile transparent dressing (Tegaderm; 3M Health Care, St. Paul, Minn) can be used to cover the hockey-stick transducer for better external visualization of the probe position and therefore easier line-ups.8 For this technique the adhesive dressing is applied directly to the transducer without acoustic coupling gel. Sterile gel is used between the covered probe and the skin. Not all sterile adhesive dressings have favorable acoustic properties for this purpose.
The subclavian artery and the transverse cervical artery are the primary vascular puncture risks of this procedure. Transverse cervical arteries are frequently observed running over or through the brachial plexus in the neck.9
Clinical Pearls
• The needle tip should be positioned adjacent to the ventral rami of C5, C6, and C7 to ensure complete plexus anesthesia with a multiple-injection technique.6
• Arteries that traverse the interscalene brachial plexus can divide it into separate compartments. The deep cervical artery (the dorsal scapular artery) usually runs between the seventh and eighth cervical roots. This artery continues between the middle and the lower trunks of the brachial plexus. Multiple injections may be necessary to obtain complete plexus anesthesia when this anatomy is present.
• The seventh cervical ventral ramus is usually the largest, with progressively smaller cephalad and caudad ventral rami. These size differences tend to equalize the size of the three trunks that form the brachial plexus.
• Both the medial to lateral and lateral to medial approaches to supraclavicular block have similar efficacy and safety profiles.10
1 La Grange P, Foster PA, Pretorius LK. Application of the Doppler ultrasound bloodflow detector in supraclavicular brachial plexus block. Br J Anaesth. 1978;50:965–967.
2 Kessler J, Gray AT. Sonography of scalene muscle anomalies for brachial plexus block. Reg Anesth Pain Med. 2007;32:172–173.
3 Tubbs RS, Louis RG, Jr., Wartmann CT, et al. Histopathological basis for neurogenic thoracic outlet syndrome: laboratory investigation. J Neurosurg Spine. 2008;8:347–351.
4 Mangrulkar VH, Cohen HL, Dougherty D. Sonography for diagnosis of cervical ribs in children. J Ultrasound Med. 2008;27:1083–1086.
5 Sinha SK, Abrams JH, Weller RS. Ultrasound-guided interscalene needle placement produces successful anesthesia regardless of motor stimulation above or below 0.5 mA. Anesth Analg. 2007;105:848–852.
6 Kapral S, Greher M, Huber G, et al. Ultrasonographic guidance improves the success rate of interscalene brachial plexus blockade. Reg Anesth Pain Med. 2008;33:253–258.
7 Kessler J, Gray AT. Course of the spinal accessory nerve relative to the brachial plexus. Reg Anesth Pain Med. 2007;32:174–176.
8 Tsui BC, Twomey C, Finucane BT. Visualization of the brachial plexus in the supraclavicular region using a curved ultrasound probe with a sterile transparent dressing. Reg Anesth Pain Med. 2006;31:182–184.
9 Weiglein AH, Moriggl B, Schalk C, et al. Arteries in the posterior cervical triangle in man. Clin Anat. 2005;18:553–557.
10 Subramanyam R, Vaishnav V, Chan VW, et al. Lateral versus medial needle approach for ultrasound-guided supraclavicular block: a randomized controlled trial. Reg Anesth Pain Med. 2011;36(4):387–392.