51 Intercostal Nerve Block
Twelve pairs of intercostal nerves lie within or near the inferior groove of each corresponding rib. These nerves supply the skin and chest wall skeletal muscles. An intercostal artery and vein accompany each nerve and lie superior to it. Intercostal nerves are difficult to image with ultrasound because they are small and often covered by the caudal edge of the corresponding rib.1 Proximal intercostal nerves are found in the classic subcostal position in 17%, in the midzone in 73%, and in the inferior supracostal position in 10% of anatomic specimens. The intercostal nerves migrate away from the ribs near the midaxillary line. Doppler ultrasound has been used to locate intercostal arteries for intercostal block.2 Intercostal arteries are 3 to 4 mm in diameter and can be detected in an acoustic window 4 cm from the midline.3 Doppler measurements of the intercostal arteries are possible from T4 and lower. Ultrasound-guided intercostal nerve block has been used for acute and chronic pain management.4 Intercostal nerve blocks can be used for breast surgery and are best placed at T3, T4, and T5 for this procedure. Another common application is for thoracic trauma and chest tube placement.5
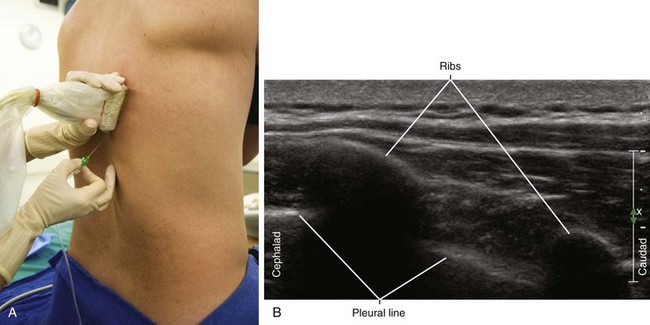
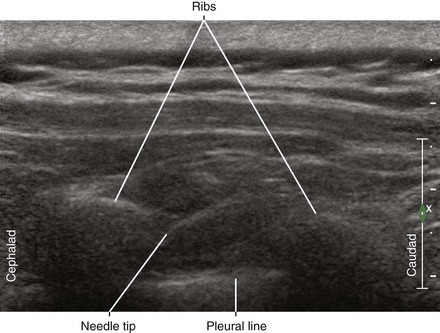
Suggested Technique
Sonograms can sometimes demonstrate three layers of the intercostal muscles (external, internal, and innermost) covering the pleural line.6 The neurovascular bundle lies between the internal and innermost intercostal muscles. Intercostal interspaces have a flying-bat appearance on sagittal ultrasound scans because of acoustic shadowing of the ribs.7
Clinical Pearls
• The easiest patient position to perform the block is prone, but lateral or sitting is also possible.
• Intercostal blocks are best performed near the posterior angulation of the ribs. In this location the nerves are shallow and relatively centrally located before branching.
• Both transverse and longitudinal in-plane approaches to intercostal injection result in similar distributions toward the paravertebral space.8
• With intercostal nerve blocks, rapid and high peak plasma levels of local anesthetic are expected. Therefore, careful attention to drug dosing is essential.
• Even with needle puncture of the pleura, the chance of pneumothorax is about 50%. This chance depends on the amount of aerated lung tissue traversed by the needle. The lung is particularly fragile in patients with chronic obstructive lung disease and emphysema.
• The tracking between the lower border of the ribs and the neurovascular bundle is not always perfect. Discrepancies are sometimes seen along the course of the rib.
• One of the benefits of ultrasound guidance for intercostal block is the avoidance of arterial puncture. This complication can result in hemothorax.
1 Eichenberger U, Greher M, Curatolo M. Ultrasound in interventional pain management. Tech Reg Anesth Pain Manag. 2004;8:171–178.
2 Vaghadia H, Jenkins LC. Use of a Doppler ultrasound stethoscope for intercostal nerve block. Can J Anaesth. 1988;35:86–89.
3 Koyanagi T, Kawaharada N, Kurimoto Y, et al. Examination of intercostal arteries with transthoracic Doppler sonography. Echocardiography. 2010;27(1):17–20. Epub 2009, Aug 31
4 Byas-Smith MG, Gulati A. Ultrasound-guided intercostal nerve cryoablation. Anesth Analg. 2006;103:1033–1035.
5 Stone MB, Carnell J, Fischer JW, et al. Ultrasound-guided intercostal nerve block for traumatic pneumothorax requiring tube thoracostomy. Am J Emerg Med. 2011;29(6):697.e1–697.e2. Epub 2010, Aug 13
6 Sakai F, Sone S, Kiyono K, et al. High-resolution ultrasound of the chest wall. Rofo. 1990;153:390–394.
7 Lichtenstein DA, Mezière G, Lascols N, et al. Ultrasound diagnosis of occult pneumothorax. Crit Care Med. 2005;33:1231–1238.
8 Paraskeuopoulos T, Saranteas T, Kouladouros K, et al. Thoracic paravertebral spread using two different ultrasound-guided intercostal injection techniques in human cadavers. Clin Anat. 2010;23(7):840–847.