Integumentary System (Skin)
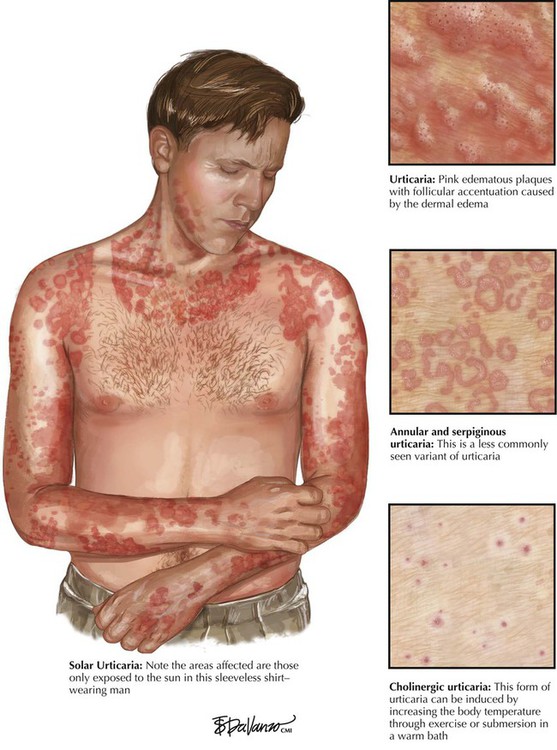
Urticaria (hives), an acute pruritic disease of short duration, is caused by a type I immune reaction (allergic, IgE-mediated) that results in local accumulation and degranulation of mast cells with histamine release and edema (pruritic nodule, edematous swelling and plaques, formation of bullae). Urticaria is caused by substances such as drugs, household stuffs, insect bites, and foods that elicit a type I immune reaction. Chronic urticaria lasting more than 6 weeks suggests persistent exposure to food additives, dyes, drugs, dust, or diseases such as thyroiditis or systemic lupus erythematosus. Acute eczematous dermatitis is characterized by erythema, edema, and vesicle formation. In later stages, oozing lesions may become crusted with scaling plaques. The etiopathogenesis is similar to urticaria (IgE-dependent immune reaction), but microscopy shows distinct eosinophilia and epidermal spongiosis. Fungal infection (dermatophytosis) must be excluded in the differential diagnosis.
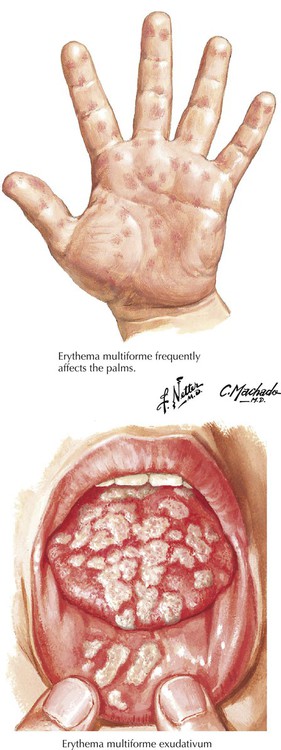
Erythema multiforme (EMF), a common hypersensitivity syndrome with associated vasculitis, may coincide with other diseases (e.g., various infections). EMF may occur after the administration of certain drugs (sulfonamides, barbiturates, salicylates) or may accompany malignant diseases (carcinoma, lymphoma) and collagen-vascular disorders (e.g., systemic lupus erythematosus). It represents a hypersensitivity reaction (CD8+ cellular immune reaction), although the immediate causative agent is unknown. Skin eruption is frequently preceded by malaise, fever, and itching or burning sensations. Typical skin changes consist of target lesions with centrifugal growth, dusky red plaques, and macules and papules on the feet and the extensor surfaces of the arms and legs. Individual lesions heal within 1 to 2 weeks and show variable hyperpigmentation and hypopigmentation. Urticarial changes may add to the polymorphism (hence the term multiforme).
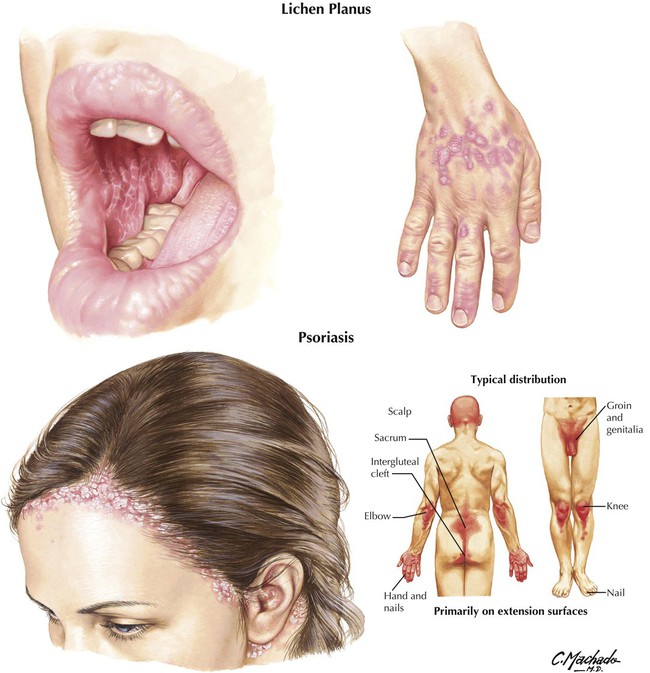
Lichen planus (LP) is a papulosquamous dermatosis. LP affects skin and mucous membranes and consists of small (2-10 mm) polygonal, white to pink, flat pruritic papules with a crisscrossed surface (Wickham striae). Externally, the papules are located on the flexor surfaces of the wrists, arms, and legs; internally, they appear on the tongue and buccal mucosa as nonerosive or erosive plaques. Malignant transformation of oral LP to SCC has been reported. Microscopy shows liquefaction degeneration of basal cells with subepithelial lymphocytic infiltration. Rete pegs are elongated with hyperparakeratosis, fissures, and single cell keratinization (Civatte bodies). LP is a cellular immune reaction against unidentified epithelial antigens. Psoriasis is a chronic inflammatory dermatosis of epidermis and dermis with epidermal hyperplasia and hyperkeratosis and parakeratosis. A deregulated epidermal cell proliferation with disturbed microcirculation has been hypothesized. Skin lesions are large (4-5 cm), demarcated, pink plaques with silver-white keratotic scales showing pinpoint hemorrhages (Auspitz sign). Microscopy shows epidermal thickening with elongated rete pegs (acanthosis), loss of the stratum granulosum and parakeratosis, thinning of suprapapillary plates with hyperemic vessels in dermal papillae, and a mixed cellular subepidermal-epidermal inflammatory infiltrate.
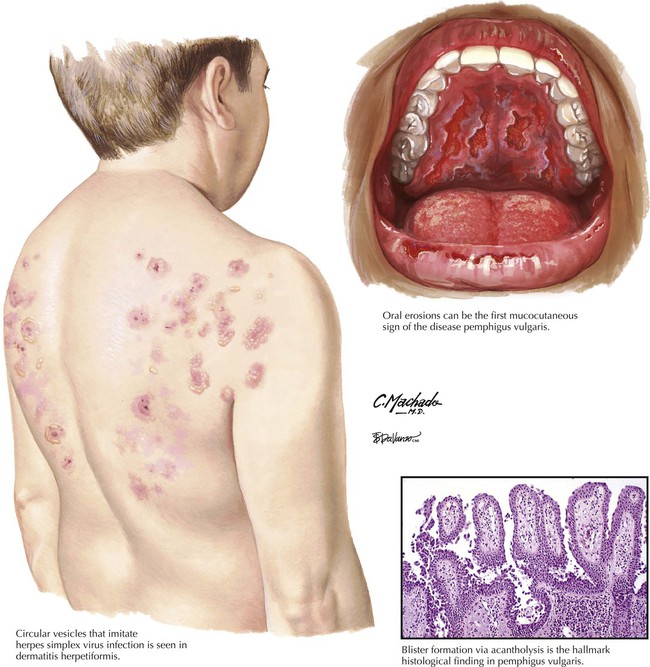
Dermatitis herpetiformis is a pruritic vesicular dermatosis often related to gluten-sensitive enteropathy (celiac disease). Burning and itching lesions on the extensor surfaces, the knees and elbows, the back, and the buttocks show a herpeslike (herpetiform) pattern. Microscopy shows subepidermal cleft formation with dense neutrophilic infiltration and microabscess formation. Dermoepidermal separation causes blister formation. Immunofluorescence shows granular or fibrillar IgA deposits in dermal papillae, and antiendomysial IgA antibodies can be demonstrated. Pemphigus vulgaris, a potentially lethal autoimmune dermatosis, involves skin and mucous membranes, primarily in older patients. It occurs everywhere on the skin except the palms and soles, with blisters that can be laterally dislocated (Nikolsky sign). Healing occurs with hyperpigmentation and scarring. Microscopy shows vesicle formation within the stratum spinosum with acantholytic epithelial cells and few lymphocytes, macrophages, or eosinophils. Serum IgG autoantibodies against desmoglein III (intercellular desmosomal component) can be demonstrated. Death occurs in approximately 10% of cases.
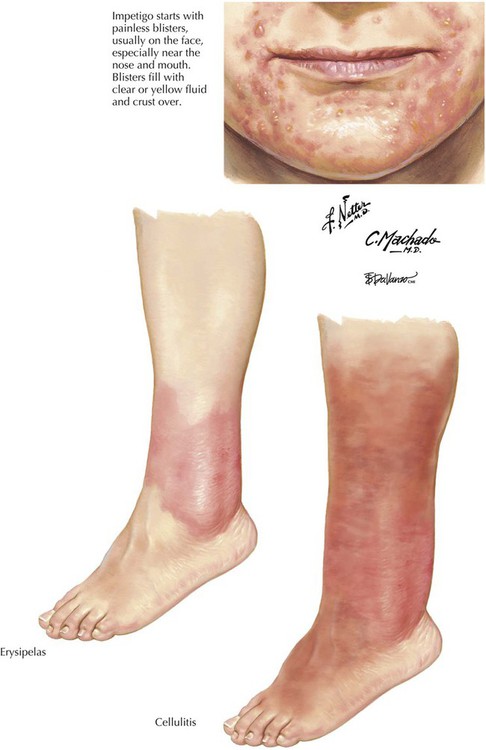
Impetigo, a superficial staphylococcal infection of the skin, occurs after minor injury. Lesions consist of pustular, vesicular, or bullous eruptions with surrounding erythema and development of honey-yellow adherent crusts. The infection usually heals within a few weeks or months. Cellulitis is an acute streptococcal infection of the deeper dermis and subcutaneous tissue that can spread to cover a large area of skin. Lesions consist of poorly demarcated painful erythematous swellings, occasionally complicated by blisters, hemorrhage, or abscess formation. Cellulitis often occurs in patients with impaired host defense from diabetes mellitus, liver cirrhosis, renal failure, chronic alcoholism, or human immunodeficiency virus (HIV). Erysipelas is an acute superficial form of cellulitis with demarcated margins and prominent lymphangitis usually caused by type A streptococci. Patients experience malaise, anorexia, fever, and chills. Blood culture results may be positive in cases with high fever. Lesions clear within 2 to 3 weeks, with frequent recurrences in immunocompromised patients.
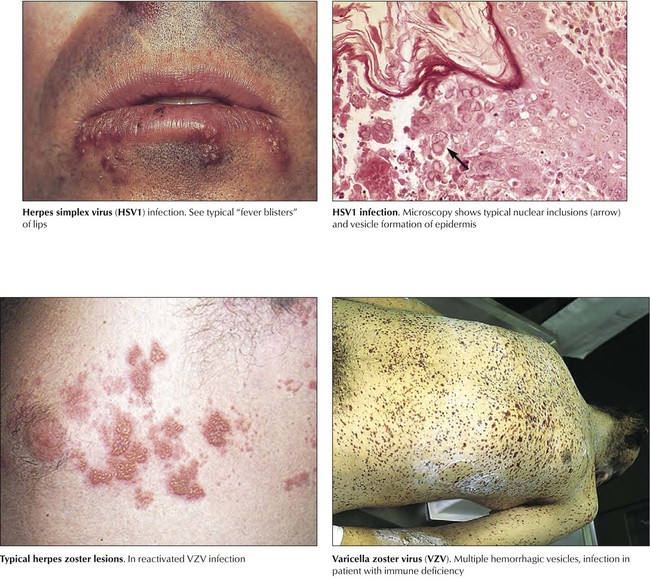
Along with varicella zoster virus and herpes genitalis, herpes simplex virus is among the more common viruses causing acute vesicular dermatitis. Acute primary infection by respiratory droplets or direct contact causes transient stomatitis and pharyngitis associated with mild lymphadenopathy. Grouped vesicles on an erythematous background appear at various sites, including the mucous membranes. Lesions heal spontaneously without scarring within 2 to 6 weeks. Some areas show only erythematous spots or plaques. Reactivated herpes simplex or varicella zoster in immunodeficient patients can cause severe systemic herpes with generalized necrotic and hemorrhagic lesions and life-threatening internal disease (hemorrhagic enteritis and encephalitis, necrotizing and hemorrhagic hepatitis).
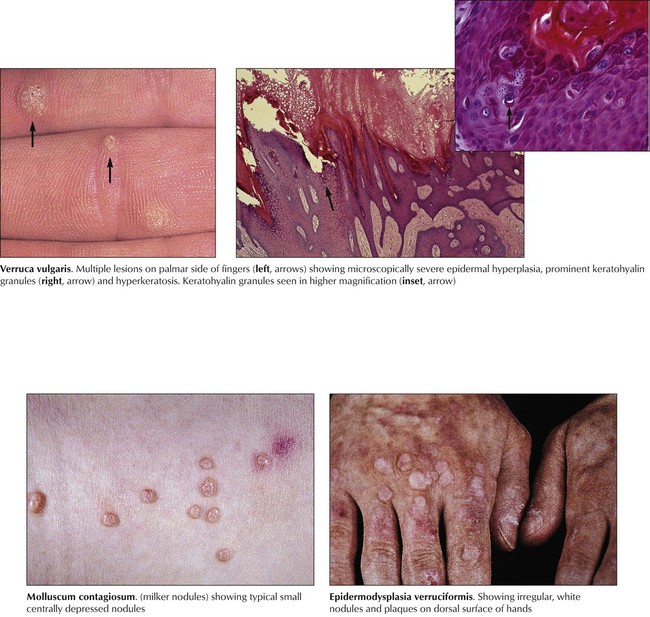
Other viral infections of the skin produce a proliferative epidermal reaction with or without overt inflammatory response. These include verrucae vulgares (common warts) and condylomata acuminata (genital warts) caused by human papillomavirus (HPV) and molluscum contagiosum (Milker nodule) caused by an unclassified poxvirus. There are more than 70 subtypes of HPV, some of which may be oncogenic, including HPV-5, implicated in epidermodysplasia verruciformis; HPV-6, in genital warts; HPV-16, in penile carcinoma; HPV-16 and HPV-18, which in a subset of cases may lead to the development of dysplasia (cervical intraepithelial neoplasia) or carcinoma. The occurrence of proliferative viral infections and their malignant sequelae increase significantly in immunodeficient patients.
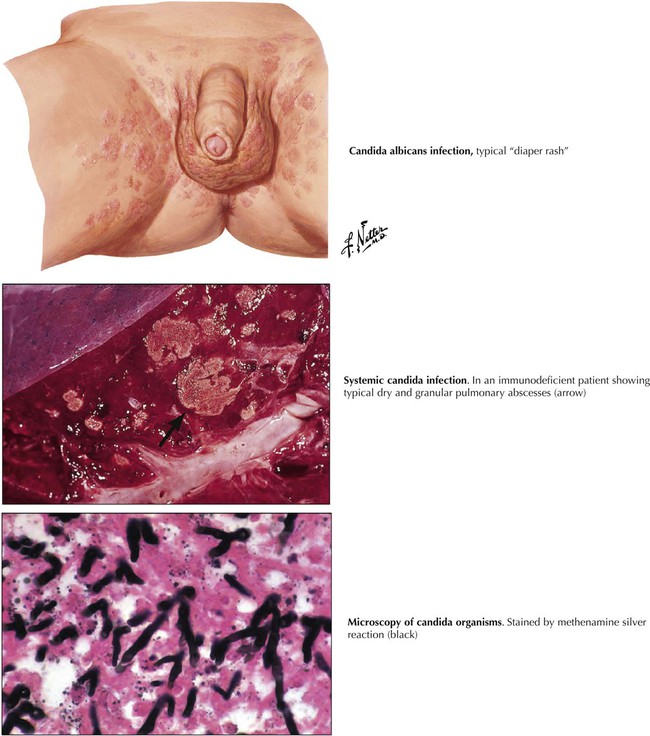
Dermal candidiasis is a fungal infection that occurs frequently in patients with metabolic or immunodeficiency disorders (e.g., diabetes mellitus, long-standing steroid or antibiotic treatment, HIV, inherited immune deficiency). Yeasts, such as Candida species, belong to the normal flora of skin and mucous membranes close to the skin (oral cavity, vagina, anus). If the host defense is disturbed, these organisms become pathogenic, causing mucositis and eventual hematogenous spread. Initially, warm, moist areas, such as the axillae, the groin, and other intertriginous regions, show moist erythematous plaques and papules with red denuded areas and glistening, cigarette paper–like scaling. Fungal organisms can be scraped from lesions and shown with histologic stains or by cultivation.
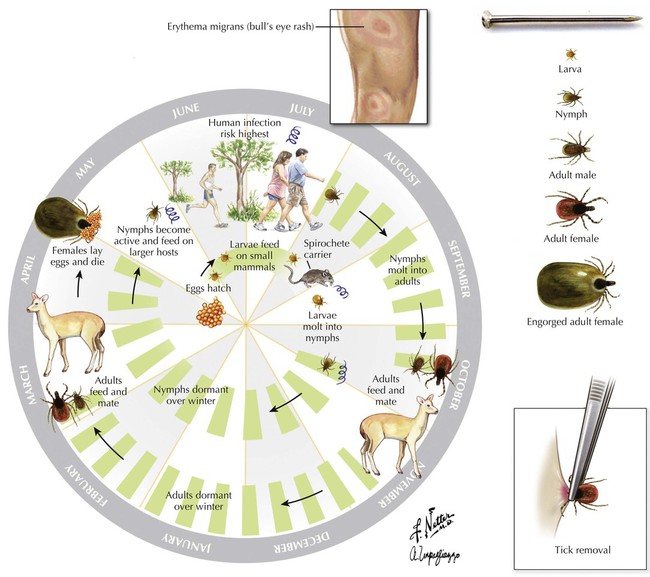
Lyme disease is caused by the spirochete Borrelia burgdorferi, which is acquired through tick bites. Ticks invade the skin, causing erythema migrans. Starting at the site of the tick bite, erythemalous patches develop and spread in an irregular pattern while the center will return to normal. Lyme disease progresses through several stages, including an acute influenzalike illness, cardiac and neurologic symptoms, and, finally, arthritis and persistent neuropsychiatric disorders.
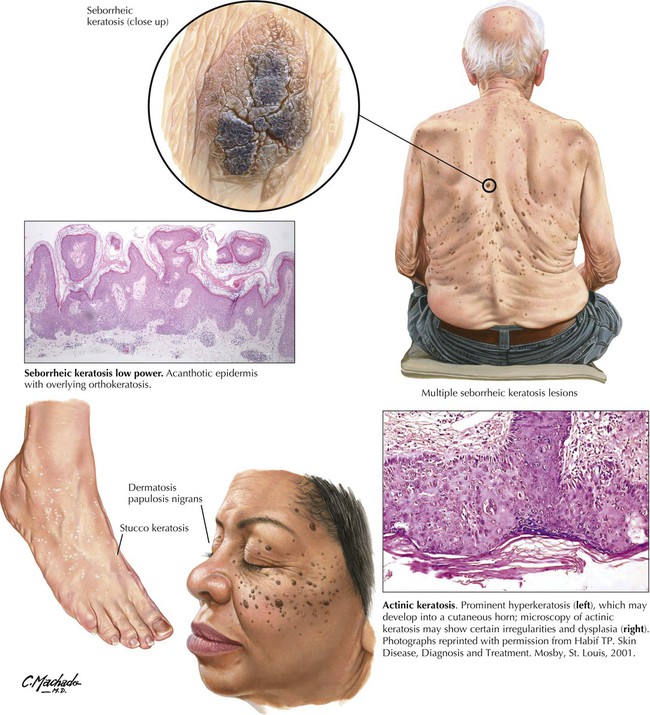
Seborrheic keratosis is a common, benign, sharply demarcated, flat or raised, epidermal proliferation with a pink to brownish-black, pigmented, smooth or lobulated surface. A sudden outgrowth of multiple seborrheic keratoses may be associated with malignancies of internal organs (Leser-Trélat sign). Microscopy shows epidermal thickening by multiple layers of small basaloid cells and various degrees of melanin pigmentation and hyperkeratosis. Some pigmented lesions must be distinguished from MM. AK is a benign lesion that may eventually progress to SCC. Excessive keratinization frequently produces cutaneous horns. AK develops at sites of chronic sun exposure and shows progressive epithelial dysplasia. Some may be pigmented (spreading pigmented actinic keratosis) and are difficult to distinguish from lentigo maligna or superficial spreading MM.
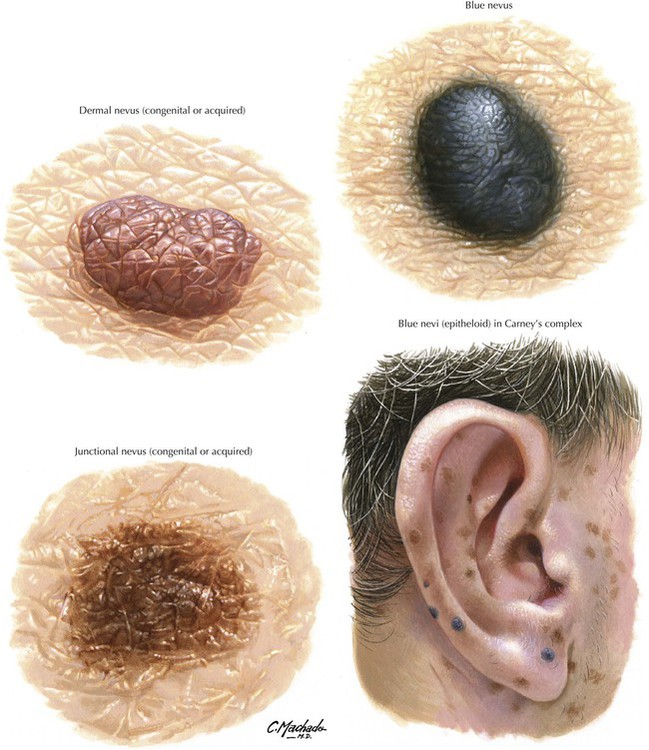
Nevi (common moles) are benign skin tumors of melanocytic origin. Dysplastic nevi describe nevi with cellular atypia without invasion. Nevi erupting de novo in areas of the body not exposed to the sun and occurring after the age of 30 years should always be evaluated for malignancy. Microscopy shows bands or nests of melanocytes in the epidermis (epidermal) or epidermal junction (junctional nevus) or both (compound nevi). Dermal nevi do not show epidermal involvement. Deep dermal nevi are referred to as blue nevi. A gross change to asymmetry and partial poor demarcation with spread and discoloration may indicate malignant transformation.
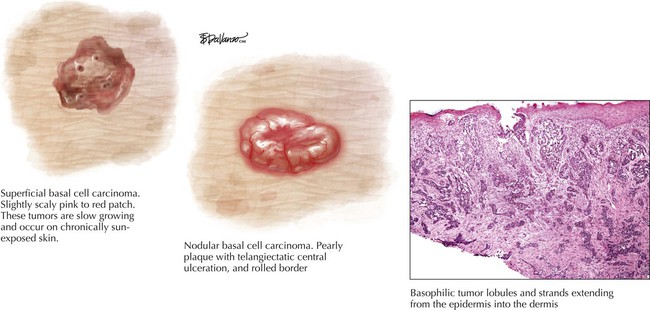
Basal cell carcinoma is a primary epidermal malignancy that does not metastasize but shows progressive invasion without sparing even skull bones (ulcus rodens). BCC is frequent in the skin of the face, scalp, ears, and neck. In addition, there exists a rare familial basal cell nevus syndrome with multiple tumors on the back and other non–sun-exposed sites. BCC appears as flat, yellowish-pink circumscribed nodules (“pearly” appearance) with prominent telangiectasia and occasional white keratotic scaling. Microscopy shows the replacement of regular squamous epithelium with atypical basal cells with peripheral palisading and signs of invasion. After surgical removal, 92% of patients with primary tumors and 60% with recurrences achieve 5-year survival.
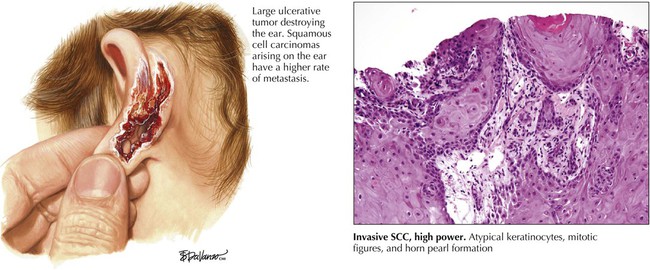
Squamous cell carcinoma, derived from keratinocytes, is one of the most common malignant tumors in the sun-exposed skin (head, neck, hands) of older people. Chemical carcinogens in tars, oils, arsenicals, and ionizing radiation also may cause SCC. Primary SCC appears as sharply circumscribed, soft or firm red nodules with a “crusted” hyperkeratotic or eroded center spreading within the skin and extending into the dermis along perivascular or perineural spaces (conduit spread). Ultimately, tumors metastasize to regional lymph nodes. Microscopy shows variable differentiation and keratinization of squamous cells, with disorganized growth and single cell keratosis, focal or total loss of stratification, and overt invasion. Tumors larger than 2 cm in diameter with deep (0.4 cm) dermal invasion are at risk for metastasis, which occurs in approximately 2% to 6% of tumors in well-vascularized regions and 20% to 30% in other areas (lips, ears, scar tissue). The 5-year mortality in patients with regional metastases is approximately 50%.
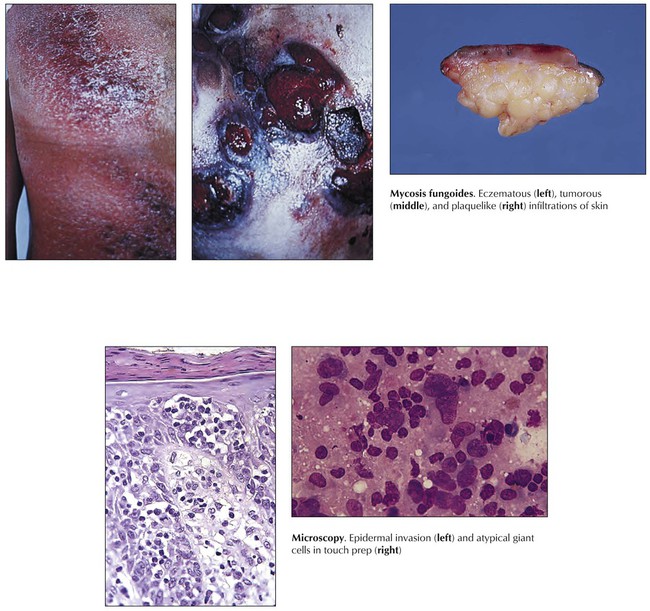
Malignant lymphomas of the skin include non-Hodgkin lymphomas and Hodgkin lymphomas. The most frequent non-Hodgkin lymphoma of the skin is the T-cell lymphoma identified as mycosis fungoides (MF), preferentially affecting people aged 30 to 50 years. MF is a distinct CD4+ T helper cell lymphoma that may secondarily involve lymph nodes and internal organs. It develops in stages from pre-MF eczematoid or psoriasislike lesions to a patch stage, a plaque stage, and a tumor stage. Microscopy shows a bandlike polymorphous dermal infiltrate with small to medium lymphoid cells, including approximately 10% to 40% atypical cells with cerebriform nuclei (MF cells) and pronounced epidermotropism. Atypical cells invade the epidermis to form small aggregates referred to as Pautrier abscesses. The median survival time is 5 years, although if lesions are ulcerated and MF invades lymph nodes, the survival time decreases to 1 year.
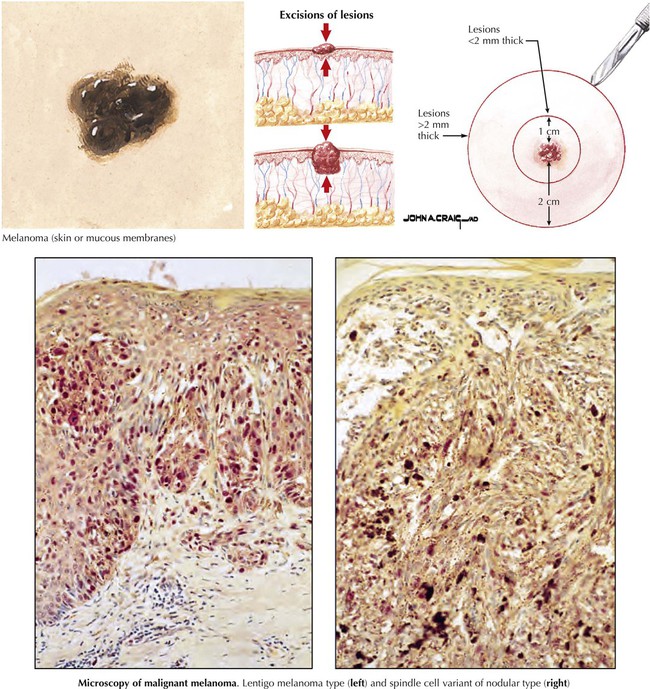
Malignant melanoma, an increasingly common melanocytic neoplasm, comprises approximately 4% of all cancers, with greatest incidence in the sun-exposed skin of red- or fair-haired persons. MM is clinically asymptomatic except for the warning signs: enlargement of a preexisting nevus with irregular border or change in color; itching and pain; or sudden development of pigmented lesions in adults in sites not often exposed to the sun. Late-stage changes are tenderness, bleeding, and ulceration. The types of MM are lentigo maligna melanoma, superficial spreading melanoma, nodular melanoma, and amelanotic melanoma. Microscopy shows poorly formed nests of nevus cells with atypia (enlarged nuclei with prominent nucleoli and mitoses), overt signs of invasion, adjacent chronic inflammatory reaction, and lymphatic spread. Size and vertical spread determine clinical staging and prognosis. After lesion removal, the 5-year survival rate is 80% to 95% in patients with early MM and less than 20% in patients with advanced disease.