CHAPTER 14 Instability with Bone Loss
PREOPERATIVE CONSIDERATIONS
Bone loss is frequently associated with chronic traumatic glenohumeral instability on the glenoid side or humeral side.1–4 Significant bone loss, often characterized by an inverted pear glenoid or engaging Hill-Sachs lesion, is believed to be a main cause of failure after arthroscopic stabilization.5–7
According to a three-dimensionally reconstructed computed tomography (CT) study with the humeral head digitally subtracted, the prevalence of glenoid bone defect has been reported as high as 90% in shoulders with chronic recurrent traumatic anterior instability.8 In addition, a bony fragment is present at the anteroinferior portion of the glenoid neck in about half of shoulders with glenoid bone loss.8 Furthermore, bone loss in shoulders associated with a bony fragment is relatively significant compared with that in shoulders with attritional glenoid loss without a bony fragment.8,9
ANATOMY AND PATHOANATOMY
Lo and colleagues7 and Burkhart and associates10 have defined the inverted pear glenoid as more than 25% to 30% loss of diameter in the inferior glenoid circle. Burkhart and DeBeer5 have recommended a bone grafting procedure for these shoulders based on their clinical outcome after arthroscopic soft tissue repair.
We have investigated a consecutive series of 121 glenoids in shoulders with chronic recurrent traumatic anterior instability, including 97 males and 24 females with an average age of 24 years (range, 13 to 54 years), using three-dimensional CT.11 The percentage defect of the glenoid was defined as a ratio of defect width against the diameter of the assumed circle based on the inferior portion of each glenoid (Fig. 14-1).9 The results demonstrated that 19 out of 121 glenoids (15.7%) were measured and showed more than 25% bone loss, with a mean percentage defect of 30.2% (range, 25.0% to 43.8%). Interestingly, a bone fragment was confirmed in 18 out of 19 glenoids in these shoulders (94.7%). Furthermore, in 9 glenoids (7.4%) that were measured and demonstrated more than 30% bone loss with 35.6% mean percentage defect (range, 30.6% to 43.8%), a bone fragment was confirmed in all shoulders. Therefore, it was concluded that most shoulders with a large glenoid bone defect, which corresponds to the so-called inverted pear glenoid,7 retain an associated bone fragment (Table 14-1).11
TABLE 14-1 Presence of Bone Fragment in Large Glenoid Bone Defect
| Bone Defect of the Glenoid | ||
|---|---|---|
| Parameter | 25% and more | 30% and more |
| No. of glenoids* | 19 (15.7%) | 9 (7.4%) |
| Mean percentage defect (range) | 30.2% (25.0%-43.8%) | 35.6% (30.6%-43.8%) |
| No. of attritional glenoids* | 1 (5.3%) | 0 (0%) |
| No. of glenoids with a bony fragment* | 18 (94.7%) | 9 (100%) |
* The values are given as the number of glenoids, with percentage in parenthesis.
HISTORY AND PHYSICAL EXAMINATION
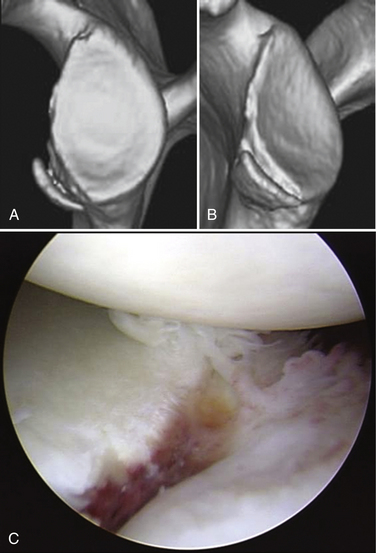
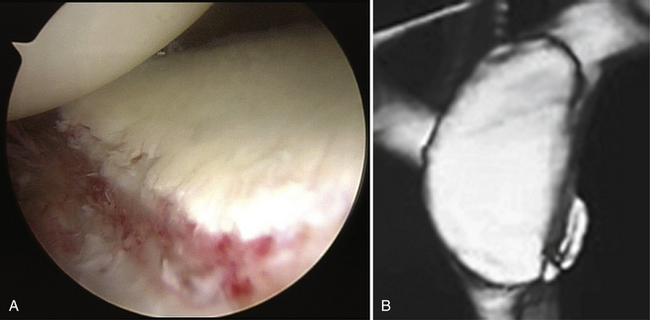
The diagnosis of recurrent traumatic anterior glenohumeral instability is usually made easily on the basis of the history of distinct dislocation or subluxation and the positive apprehension sign. However, when collision athletes are seen, care should be taken because they may not experience clear dislocation or subluxation and only complain of pain or weakness when they bring their arm to maximum external rotation in abduction. In addition, many collision athletes do have a minimally displaced bony Bankart lesion, often without a concomitant Hill-Sachs lesion, in which the arthroscopic finding demonstrates clear evidence of anteroinferior instability, but without dislocation or subluxation (Fig. 14-2).
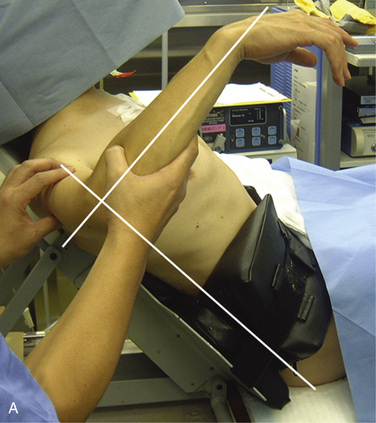
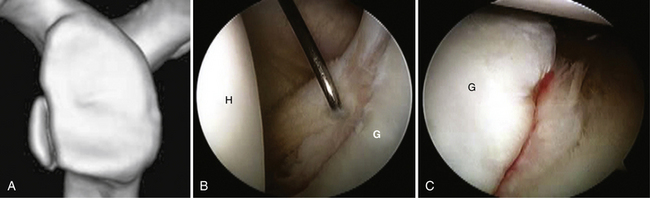
The anterior apprehension test is done with the patient in the supine position. In this test, the shoulder is moved passively into maximum external rotation with the arm at the side in 30, 60, 90, 120, and 150 degrees of abduction and maximum flexion. At the same time, the posterior apprehension test is done, with the arm at maximum internal rotation in 90 degrees of abduction. The feeling of apprehension is reported in each arm position. However, the most important and reliable physical examination can usually be done with the patient under anesthesia, comparing stability testing with the contralateral extremity (Fig. 14-3).
DIAGNOSTIC IMAGING
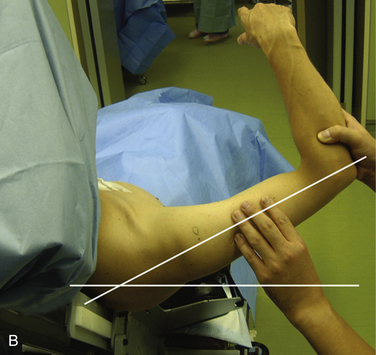
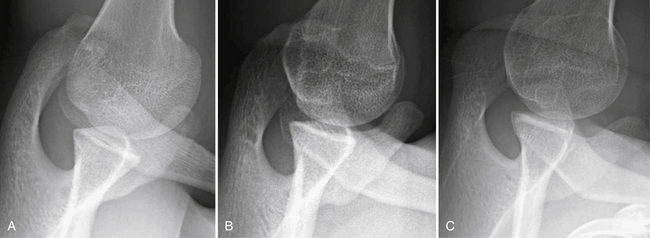
X-ray images are sometimes helpful for detecting the Hill-Sachs lesion and the anterior glenoid rim lesion,3 especially during the first patient visit. Bernageau12 has described a unique method for detecting an anterior glenoid rim lesion with the patient in the standing position. However, this technique requires fluoroscopic control to obtain optimal diagnosable images and, therefore, radiation exposure is an issue that cannot be ignored.13 Our group has developed a modified Bernageau method with the patient lying on the axilla in the most relaxed position (Fig. 14-4). In this method, clear x-ray images can be obtained more easily with a high probability of ascertaining bony pathology without using fluoroscopic imaging (Fig. 14-5).
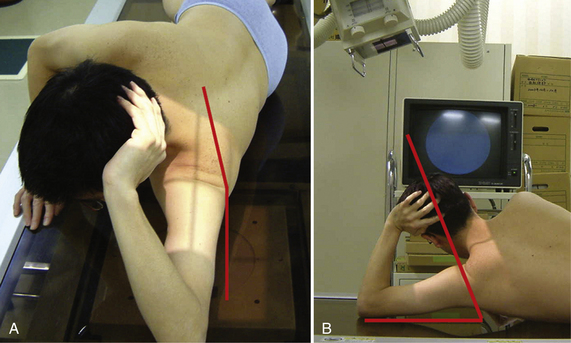
FIGURE 14-4 Modified Bernageau method. The patient lies on his or her axilla in the most relaxed position. A, In this position, the scapula needs to incline 5 degrees to the vertical line. B, Then the incident x-ray needs to be aimed craniocaudally with15 to 20 degrees of inclination to the vertical line.
Although plain magnetic resonance imaging (MRI) provides only limited information, MR arthrography is helpful when detecting a soft tissue lesion such as a Bankart lesion, capsular pathology, and/or a HAGL (humeral avulsion of the glenohumeral ligament) lesion.14 However the final diagnosis of soft tissue pathology can be made most accurately through diagnostic arthroscopy.
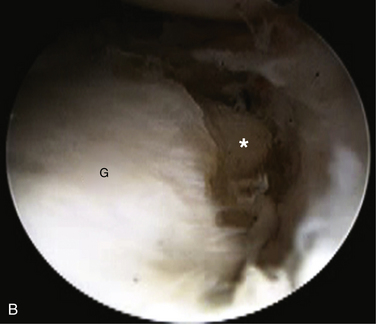
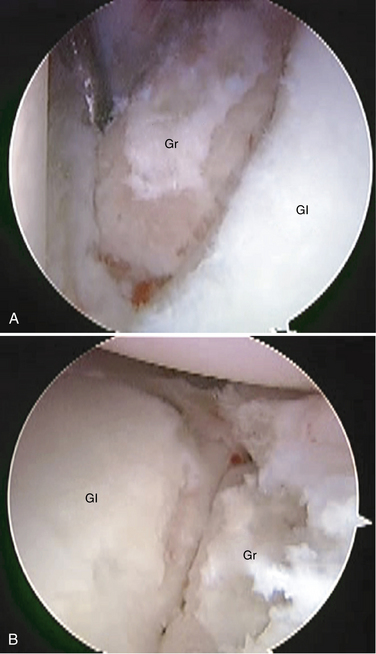
Three-dimensional CT is the most important imaging study for assessing glenoid morphology accurately.8 The arthroscopic glenoid view sometimes makes surgeons overestimate the bone defect because normally the cartilage damage is more extensive than the bony lesion (Fig. 14-6). Furthermore, in a shoulder with a bony Bankart lesion, detecting accurate configuration of the bony fragment is not easy because the bone fragment is covered by the surrounding soft tissue. Through preoperative three-dimensional CT, surgeons can determine whether the glenoid is attritional or if a bony Bankart lesion is present. They can also quantify bone loss with attritional glenoids and detect the size and shape of the bony fragment in shoulders with a bony Bankart lesion.8,9,11,15
Arthroscopic Treatment
If a bone fragment is present with three-dimensional CT, an arthroscopic bony Bankart repair, in which the fragment is incorporated into the Bankart repair, is indicated, regardless of the severity of bone loss.9,16,17 Therefore, most shoulders with a large glenoid bone loss can be treated arthroscopically using this technique.11 For shoulders with significant bone loss associated with the attritional glenoids in young and active patients, although the number of such patients is limited, open or arthroscopic bone grafting procedures are indicated. My preference is an arthroscopic iliac bone grafting in combination with an anterior-inferior capsulolabral repair (see later).18–20
Arthroscopic Bony Bankart Repair
Most bony Bankart lesions are displaced and represent a partly malunited chronic avulsion–type fracture, and the bony fragment is firmly connected to the adjacent labrum or soft tissue. These characteristics of chronic bony Bankart lesions make arthroscopic bony reconstruction feasible.9,16 Normally, bony Bankart lesions are never completely healed to the glenoid neck because the fragment is displaced from its original location while the adjacent glenohumeral ligament is not functioning. Therefore, most of the bony fragments associated with a bony Bankart lesion can be easily separated from the glenoid neck using a standard straight rasp. The gap between the fragment and original glenoid is usually well demarcated in most shoulders, but if this is not the case, careful palpation or information from a preoperative three-dimensional CT scan can assist in delineating the gap.
Setup and Arthroscopic Evaluation.
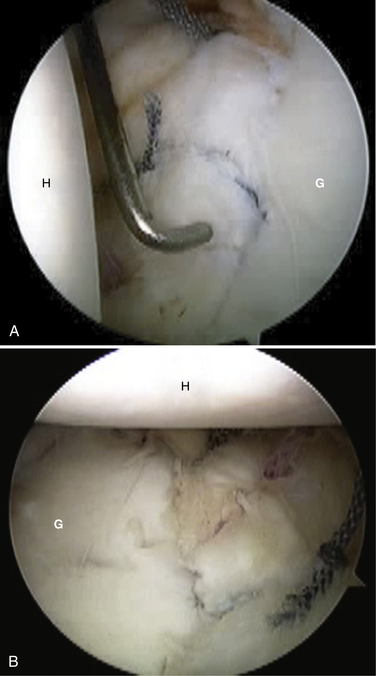
All patients are seated in the beach chair position under general anesthesia and joint laxity is assessed by examination of both shoulders prior to surgical intervention. A 4-mm arthroscope is introduced through a standard posterior portal and a diagnostic arthroscopy is performed. I then create an anterior portal just superior to the subscapularis tendon and lateral to the conjoined tendon using an outside-in technique to facilitate instrument insertion without cannulas.21 Inserting the arthroscope through the anterior portal can also help confirm a bony Bankart lesion (Fig. 14-7).
Mobilization of the Complex.
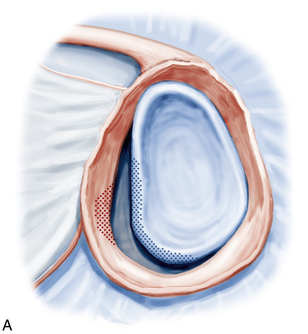
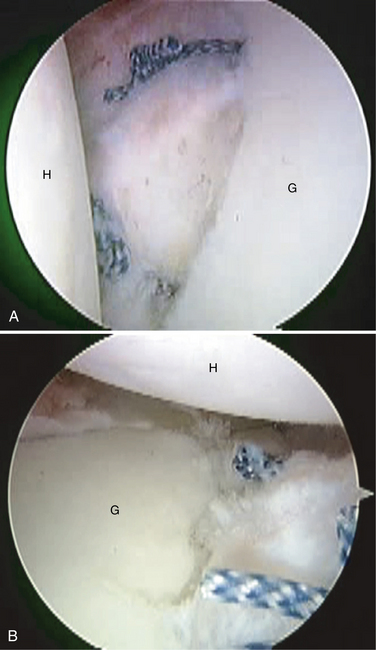
After inspection from the anterior portal, separation and mobilization of the labroligamentous complex, together with the bony fragment from the glenoid neck, is performed using an elevator, straight and curved rasps, scissors, shavers, and a radiofrequency instrument through a cannula-less anterior portal. This step is a vital part of this procedure. First, a straight rasp is inserted from the anterior portal and placed in the small gap between the fragment and glenoid neck. Then, the gap is expanded by tapping the handle of the rasp. After separating the fragment from the glenoid neck, the mobilization of the labroligamentous complex is performed up to the 7:30 o’clock position in the right shoulder until the complex and fragment become completely free. This is done in the same way as one would mobilize a Bankart lesion without a bony fragment using the instruments described. Once mobilization of the fragment and complex are completed, the glenoid is prepared by removing scar tissue from the glenoid neck and exposing the bony surface using a shaver and abrader. Articular cartilage on the edge of the glenoid is also removed to promote tissue healing after repair (Fig. 14-8). Normally, the separation of the fragment from the neck can be readily accomplished using only elevators and rasps. If the separation of the fragment is difficult and the fragment is united firmly, a small chisel can be introduced from the anterior portal to separate it from the glenoid neck. An anterosuperior portal is established at the anterosuperior margin of the rotator interval using an outside-in technique. This becomes the second working portal. In shoulders with superior labral detachment, a lateral acromial portal, established just lateral to the midpoint of the acromion through the muscle-tendon junction of the infraspinatus, is used instead of the anterosuperior portal.22
Repair of Inferior Labrum Adjacent to the Osseous Fragment.
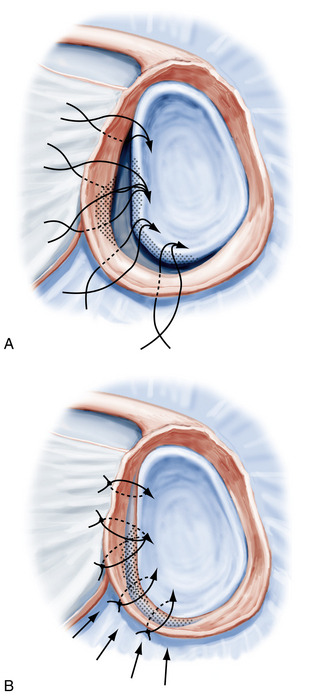
In total, four bioabsorbable suture anchors loaded with no. 2 high-strength suture are inserted on the surface of the glenoid at the 6 o’clock position using a drill guide introduced through the anterior portal. Because this portal has no cannula, the angle of approach of the guide can be adjusted, easily allowing optimization of the angle to the glenoid.21 After the first anchor insertion, a looped 2-0 nylon suture is placed into the labrum at the 6:30 o’clock position using a low profile 7-mm punch or a suture hook. A suture relay is then performed intra-articularly.21 The second anchor in inserted into the face of the glenoid at the 4:40 o’clock position, followed by suture placement in the labrum adjacent to the inferior side of the bony fragment using the same technique. After completion of the suture placement of the inferior two anchors, knot tying is performed using a self-locking sliding knot through a 5-mm cannula inserted through the anterior portal. To accomplish secure knot tying, the complex, together with the fragment, is held upward and laterally on the glenoid surface by a grasper introduced through the anterosuperior portal to reduce tensile force on the suture.
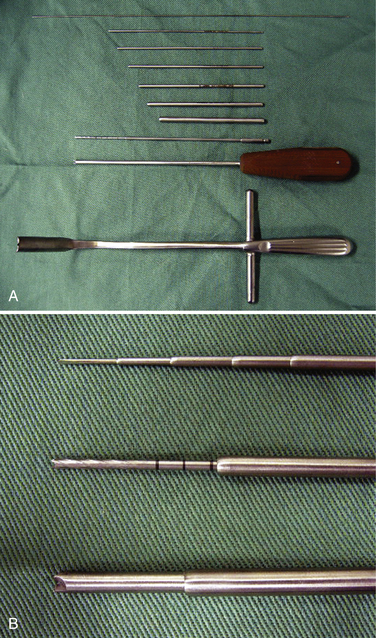
Osseous Fragment and Superior Labrum Repair.
The next step is the suturing of the osseous fragment itself by passing the suture through the fragment or by penetrating it using a bone-penetrating tool, such as a Suture Leader (DePuy Mitek, Raynham, Mass), Ideal Suture Grasper (DePuy Mitek), an originally developed bone penetrator with a stiff shaft and large handle, a Bone Stitcher (Smith & Nephew, Andover, Mass), or by passing suture around the fragment using a suture hook (Conmed Linvatec, Largo, Fla) or Suture Leader.16,23,24 It is very important to characterize the fragment shape and size preoperatively by three-dimensional CT evaluation to decide whether passing through or passing around the fragment is most appropriate.16 This procedure is facilitated when the bony fragment is reduced and stabilized by grasping the labrum adjacent to the superior portion of the fragment with a grasper while the first knot is tied (see earlier). Although the number of suture anchors used is dependent on the size and shape of the osseous fragment, normally one or two suture anchors are used for this part of the stabilization procedure (Fig. 14-9).16 Knot tying is performed after placing the sutures through the fragment. The final step is to suture the labrum adjacent to the superior side of fragment to augment the stability of the entire complex. Normally, four suture anchors with simple sutures are used to reconstruct the entire labroligamentous complex (Fig. 14-10).
Management of the Associated Pathology.
In shoulders with a capsular tear, a capsular repair using two to three side to side stitches is performed prior to the bony Bankart repair. Furthermore, in shoulders with a superior labral detachment, arthroscopic reattachment is performed after the Bony Bankart repair is completed, using a lateral acromial portal instead of the anterosuperior portal.22
Rotator Interval Closure.
The rotator interval closure is performed as an augmentation in patients with relatively high-risk shoulders, such as contact athletes, young individuals with joint laxity, and those with a large Hill-Sachs lesion (Rowe25 grade III). 26-28 In these patients, the rotator interval is closed by suturing the superior margin of the subscapularis tendon to the superior glenohumeral ligament with the arm held at the side and in maximum external rotation using no. 2 high-strength sutures.29
PEARLS& PITFALLS
Arthroscopic Iliac Bone Grafting
For shoulders with significant bone loss in the attritional glenoid category, many surgeons prefer to use the coracoid transfer procedure.5,15,30 I believe that the coracoid process should be preserved because it plays an important role in shoulder function. In addition, an arthroscopic coracoid transfer normally requires an anterior capsular resection despite the fact that the capsule is important for proprioception of the glenohumeral joint.31–33 Therefore, I prefer an arthroscopic technique using a tricortical bone graft, which is harvested from the iliac crest, in combination with an anterior-inferior capsulolabral repair.
Harvesting the Iliac Bone Graft.
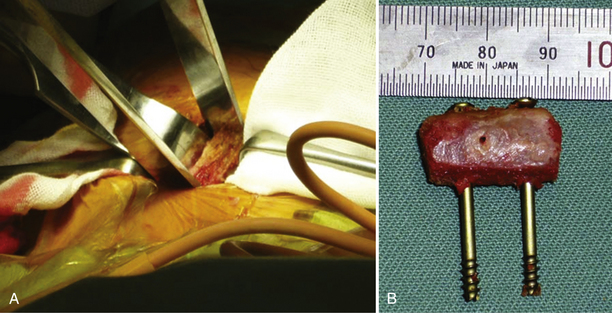
An iliac tricortical bone graft 20 mm in length and 10 mm in depth is harvested from the iliac crest with the patient in the supine position prior to arthroscopy. The graft is then prepared for insertion to fit the configuration of the anteroinferior portion of the native glenoid demonstrated by preoperative three-dimensional CT. Two drill holes are created to accommodate a 3-mm cannulated screw inserted into the graft; another two small holes are also created in the center of the graft for sutures from the suture anchor for temporary graft fixation (Fig. 14-11).
Arthroscopic Evaluation and Mobilization of the Complex.
All patients are seated in the beach chair position under general anesthesia and joint laxity is assessed prior to surgery. A 4-mm arthroscope is introduced through a standard posterior portal and a diagnostic arthroscopy is performed. I then create an anterior portal in the same manner as that for a bony Bankart repair. After inspection from the anterior portal, separation and mobilization of the labroligamentous complex from the glenoid neck are performed up to the 7:30 o’clock position in the right shoulder until the complex becomes completely free. Then, an anterosuperior portal is established at the anterosuperior margin of the rotator interval as the second working portal.
Iliac Graft Fixation.
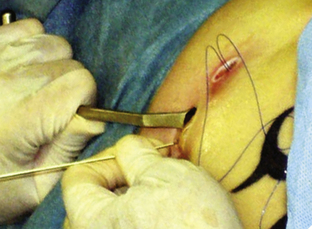
An anteroinferior portal is then created 3 cm inferior and 1cm medial to the anterior portal with a 2-cm longitudinal skin incision. The conjoined tendon and coracoid process are palpated manually with the index finger, and the conjoined tendon retractor, inserted from the anteroinferior portal, is placed lateral to the tendon at a point 2 to 3 cm below the coracoid process. The conjoined tendon is then retracted medially to obtain an optimal angle to the glenoid. Next, a cannulated guidewire inserter is introduced from the anteroinferior portal into the joint by penetrating the subscapularis muscle to line up the drill hole created in the graft in advance (Fig. 14-12). A guidewire is inserted through this cannulated guide and drilled to the optimal position of the glenoid neck. The cannulated guide is then replaced by one with a larger diameter to fit the cannulated drill and screw (Fig. 14-13). After drilling, a 3-mm diameter cannulated cancellous screw, 30 mm long (Synthes, West Chester, Pa), is inserted through this cannula to the superior portion of the graft. The same procedure is then repeated to insert another screw into the inferior portion of the graft. The guidewire, cannulated guide, and conjoined tendon retractor are then removed (Fig. 14-14).
Anteroinferior Capsulolabral Repair.
The capsulolabral complex, which was previously mobilized, is then reattached to the native glenoid using another three to four bioabsorbable suture anchors loaded with no. 2 high-strength suture in the same manner as a Bankart repair (Fig. 14-15).
PEARLS& PITFALLS
Treatment for the Engaging Hill-Sachs Lesion
A Hill-Sachs lesion should be considered in conjunction with the glenoid bone defect.2 I believe that if the bone loss on the glenoid side is addressed by the bony Bankart repair or the iliac bone graft procedure, surgeons can ignore the Hill-Sachs lesion. In shoulders with a large engaging Hill-Sachs lesion associated with minimum glenoid bone loss, a Hill-Sachs remplissage technique can be useful.34
POSTOPERATIVE REHABILITATION PROTOCOL
The shoulders are immobilized for 3 weeks using a sling (UltraSling II, Donjoy, Carlsbad, Calif). After immobilization, passive and assisted-active exercises are initiated for forward flexion and external rotation, avoiding pain. After 6 weeks, patients begin strengthening exercises of the rotator cuff and scapular stabilizers. Three months after the operation, they are permitted to practice noncontact sports. Full return to throwing or contact sports is allowed after 6 months according to each individual’s functional recovery. The same postoperative protocol is used after the bony Bankart repair and the iliac bone grafting.
1. Bushnell BD, Creighton RA, Herring MM. Bony instability of the shoulder. Arthroscopy. 2008;24:1061-1073.
2. Yamamoto N, Itoi E, Abe H, et al Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg, 16; 2007:649-656.
3. Bigliani LU, Newton PM, Steinmann SP, et al. Glenoid rim lesions associated with recurrent anterior dislocation of the shoulder. Am J Sports Med. 1998;26:41-45.
4. Itoi E, Lee SB, Berglund LJ, et al The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: A cadaveric study. J Bone Joint Surg Am, 82; 2000:35-46.
5. Burkhart SS, De Beer JF Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy, 16; 2000:677-694.
6. Boileau P, Villalba M, Héry JY, et al. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88:1755-1763.
7. Lo IY, Parten PM, Burkhart SS The inverted pear glenoid: an indicator of significant glenoid bone loss. Arthroscopy, 20; 2004:169-174.
8. Sugaya H, Moriishi J, Dohi M, et al. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am. 2003;85:878-884.
9. Sugaya H, Moriishi J, Kanisawa I, Tsuchiya A. Arthroscopic osseous Bankart repair for chronic recurrent traumatic anterior glenohumeral instability. J Bone Joint Surg Am. 2005;87:1752-1760.
10. Burkhart SS, DeBeer JF, Tehrany AM, Parten PM. Quantifying glenoid bone loss arthroscopically in shoulder instability. Arthroscopy. 2002;18:488-491.
11. Maeda K, Sugaya H, Mochizuki T, Moriishi J. [The inverted-pear glenoid in recurrent anterior glenohumeral instability. Shoulder Joint (Katakansetsu). 2005;29:507-510.
12. Bernageau J. Imaging of the shoulder in orthopedic pathology. Rev Prat. 1990;40:983-992.
13. Edwards TB, Boulahia A, Walch G. Radiographic analysis of bone defects in chronic anterior shoulder instability. Arthroscopy. 2003;19:732-739.
14. Kon Y, Shiozaki H, Sugaya H. Arthroscopic repair of a humeral avulsion of the glenohumeral ligament lesion. Arthroscopy. 2005;21:632.
15. Chuang TY, Adams CR, Burkhart SS. Use of preoperative three-dimensional computed tomography to quantify glenoid bone loss in shoulder instability. Arthroscopy. 2008;24:376-382.
16. Sugaya H, Moriishi J, Kanisawa I, Tsuchiya A. Arthroscopic Osseous Bankart repair for chronic traumatic anterior glenohumeral instability. Surgical technique. J Bone Joint Surg Am. 2006;88(suppl 1, pt 2):159-169.
17. Mologne TS, Provencher MT, Menzel KA, et al Arthroscopic stabilization in patients with an inverted pear glenoid: results in patients with bone loss of the anterior glenoid. Am J Sports Med, 35; 2007:1276-1283.
18. Warner JJ, Gill TJ, O’Hollerhan JD, et al. Anatomical glenoid reconstruction for recurrent anterior glenohumeral instability with glenoid deficiency using an autogenous tricortical iliac crest bone graft. Am J Sports Med. 2006;34:205-212.
19. Scheibel M, Kraus N, Diederichs G, Haas NP. Arthroscopic reconstruction of chronic anteroinferior glenoid defect using an autologous tricortical iliac crest bone grafting technique. Arch Orthop Trauma Surg. 2008;128:1295-1300.
20. Scheibel M, Nikulka C, Dick A, et al. Autogenous bone grafting for chronic anteroinferior glenoid defects via a complete subscapularis tenotomy approach. Arch Orthop Trauma Surg. 2008;128:1317-1325.
21. Sugaya H, Kon Y, Tsuchiya A Arthroscopic Bankart repair in the beach-chair position: a cannulaless method using intra-articular suture relay technique. Arthroscopy, 20(suppl 2); 2004:116-120.
22. Sugaya H, Kon Y, Matsuki K, Tsuchiya A. Arthroscopic superior labrum detachment repair using lateral acromial portal. Kasnsetsukyo (Arthroscopy). 2002;27:163-167.
23. Porcellini G, Campi F, Paladini P. Arthroscopic approach to acute bony Bankart lesion. Arthroscopy. 2002;18:764-769.
24. Sugaya H, Kon Y, Tsuchiya A Arthroscopic repair of glenoid fractures using suture anchors: technical note with case series. Arthroscopy, 21; 2005:635.
25. Rowe CR, Zarins B, Ciullo JV Recurrent anterior dislocation of the shoulder after surgical repair: apparent causes of failure and treatment. J Bone Joint Surg Am, 66; 1984:159-168.
26. Treacy SH, Field LD, Savoie FH Rotator interval capsule closure: an arthroscopic technique. Arthroscopy, 13; 1997:103-106.
27. Gartsman GM, Taverna E, Hammerman SM Arthroscopic rotator interval repair in glenohumeral instability: description of an operative technique. Arthroscopy, 15; 1999:330-332.
28. Karas SG Arthroscopic rotator interval repair and anterior portal closure: an alternative technique. Arthroscopy, 18; 2002:436-439.
29. Takahashi N, Sugaya H, Matsuki K, et al. Arthroscopic rotator interval closure for recurrent anterior-inferior glenohumeral instability. Kansetsukyo (Arthroscopy). 2005;30:57-60.
30. Latarjet M. Techniques chirugicales dans le trairement de la luxation anteriointerne recidivante de l’epaule. Lyon Chir. 1965;61:313-318.
31. Lafosse L, Lejeune E, Bouchard A, et al. The arthroscopic Latarjet procedure for the treatment of anterior shoulder instability. Arthroscopy. 2007;23:1242.
32. Gelber PE, Reina F, Monllau JC, et al Innervation patterns of the inferior glenohumeral ligament: anatomical and biomechanical relevance. Clin Anat, 19; 2006:304-311.
33. Jerosch J, Castro WH, Halm H, Drescher H. Does the glenohumeral joint capsule have proprioceptive capability. Knee Surg Sports Traumatol Arthrosc. 1993;1:80-84.
34. Purchase RJ, Wolf EM, Hobgood ER, et al Hill-sachs “remplissage”: an arthroscopic solution for the engaging hill-sachs lesion. Arthroscopy, 24; 2008:723-726.