CHAPTER 9 Instability of the Ankle and Subtalar Joints
Ankle sprains are the most common sports-related injuries, and they account for almost 10% of emergency department visits. Most ankle sprains are inversion-type sprains that injure the lateral ankle ligaments. Chronic lateral ankle instability develops in 20% to 30% of patients after acute ankle sprains despite adequate nonoperative treatment.1 The cause of chronic lateral ankle instability after ankle injury is not well understood and is probably multifactorial. Symptoms may result from inadequately healed torn ligaments or ligaments that have healed in a stretched manner.2 Generalized hyperlaxity, strength and proprioception deficits are likely contributing factors.
ANKLE INSTABILITY
Anatomy and Physiology
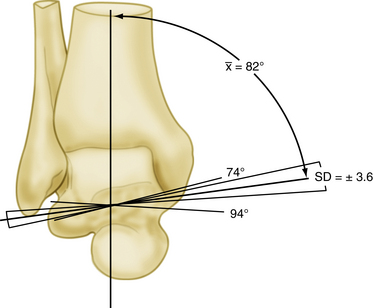
Stability of the ankle joint depends on the contributions of bony architecture, ligamentous attachments, and the dynamic stability provided by muscles around the ankle.3 The ankle is a composite joint that includes the distal tibiofibular syndesmosis and a diarthrodial mortise between the distal tibia and fibula and the talus. The subtalar joint provides sagittal rotation about a single oblique axis, from the neck of the talus to the lateral wall of the calcaneus. In the coronal plane, the axis of the ankle runs medial cephalad to lateral caudad, with a mean angulation of 82 ± 4 degrees in relation to the tibia (Fig. 9-1).
The ankle joint axis tends to change throughout the functional arc range of motion from dorsiflexion to plantar flexion. The distal fibula moves distally with weight bearing, deepening the mortise and increasing ankle stability. The talus is not as well contained by the mortise during plantar flexion compared with dorsiflexion, because the talus is wider anteriorly than posteriorly. The dorsal surface of the talus has a slight longitudinal groove that corresponds to a longitudinal ridge on the tibial plafond. The ridge and groove help to confer transverse plane stability to the tibiotalar joint. The distal fibula gives attachment to the lateral ligaments of the ankle joint, and its posterior aspect is grooved to accept the tendons of the peroneus longus and peroneus brevis muscles.4 Bony anatomic variations may contribute to increased ankle instability. For example, Scranton and colleagues showed that the fibula is located more posterior in patients with instability.5 One study compared hindfoot varus measurements on computed tomography (CT) scans of patients with lateral ankle instability to those of patients without instability and found a statistically significant increased amount of varus in patients with instability.6
The ankle ligaments provide supplemental stability to the ankle and also contribute to hindfoot stability. Ligaments of the ankle joint include the syndesmotic ligaments, the deltoid ligament complex, and the lateral collateral ligaments. The syndesmotic ligaments include the anterior inferior and posterior inferior tibiofibular ligaments and the strong interosseous ligament.
The deltoid ligament is formed by four to six main ligaments on the medial side. Four of these are always constant; from anterior to posterior, they are the anterior tibiotalar ligament (ATTL), the tibionavicular ligament (TNL), the calcaneotibial ligament (CTL), and the posterior tibiotalar ligament (PTTL). Occasionally, calcaneonavicular and tibiospring ligaments can be part of the deltoid ligament. The deltoid ligament includes superficial and deep parts. The superficial ligaments cross two joints, namely the ankle and the subtalar joints. The deep ligaments cross only the ankle joint, though the demarcation is not always absolutely clear.3,7 The deltoid ligament is the primary restraint against pronation and abduction of the talus, with the superficial and deep components equally effective.7
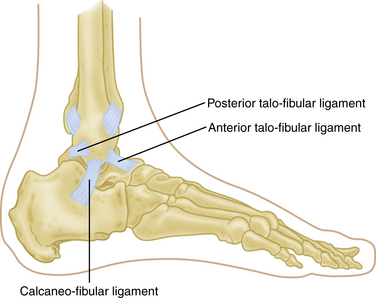
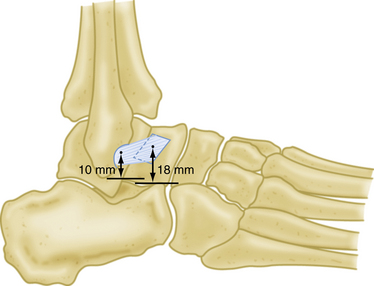
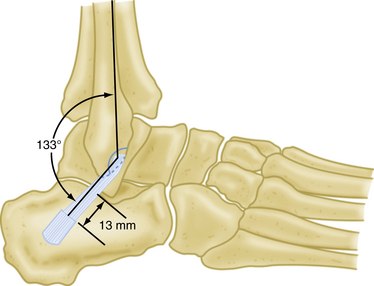
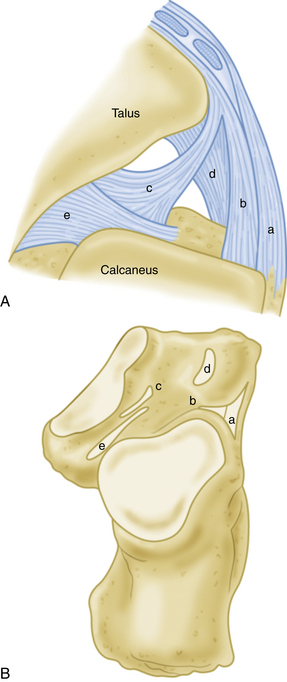
The lateral ankle joint ligamentous complex provides primary restraint to inversion and consists primarily of three structures: the anterior talofibular ligament (ATFL), the calcaneofibular ligament (CFL), and the posterior talofibular ligament (PTFL) (Fig. 9-2). Intimate knowledge of the anatomy is paramount to the success of surgical reconstruction. The ATFL, which is possibly a thickening of the joint capsule, is the most anterior structure. It averages about 24.8 mm in length and 7 mm in width and is the weakest and most easily injured of the ankle ligaments (Fig. 9-3). It originates about 10 mm proximal to the tip of the fibula and inserts on the lateral aspect of the talus, on average 18 mm superior to the subtalar joint.3,7,8 The ATFL courses obliquely from posterolateral to anteromedial with respect to the tibiotalar joint. It resists internal rotation of the talus as well as anterior translation. The CFL is a round, cordlike, extracapsular structure that originates from the inferior medial surface of the distal fibula. It extends posteroinferiorly, deep to the peroneal tendons, and attaches on a small tubercle on the lateral calcaneal surface, on average 13 mm inferior to the subtalar joint and posterior to the long axis of the fibula.3 It is about 35.8 mm long and 5.3 mm wide (Fig. 9-4). The CFL is vertical and coplanar with the fibula at 10 to 20 degrees of ankle dorsiflexion. In that position, it resists inversion and becomes the primary ankle stabilizer and a secondary subtalar joint stabilizer.8,9
Isolated rupture of the PTFL is rare because it is the strongest and least vulnerable of the lateral ankle ligaments. The PTFL originates from the posterior portion of the distal fibula and inserts onto the lateral tubercle of talus posteriorly. It may be injured in combination with rupture of the ATFL and CFL in severe ankle sprains and ankle dislocations.7,10 The lateral subtalar joint is further stabilized by the interosseous talocalcaneal ligament (ITCL), the cervical ligament, the inferior extensor retinaculum, and the lateral talocalcaneal ligament (LTCL) (Fig. 9-5). In a biomechanical study, Tochigi and Amendola showed the ITCL to be the main stabilizer of the subtalar joint.11
The musculotendinous units that cross the ankle joint provide secondary or dynamic stability to the ankle and hindfoot. The most important of these are the laterally positioned peroneal tendons, which are the primary evertors of the ankle12; the tibialis posterior tendon; and the toe flexors medially. In a cadaveric study, Hatch and Labib demonstrated that the peroneal tendons, along with the superior peroneal retinaculum (SPR), provide static resistance to anterior talar displacement with the ankle in neutral position. In that study, sectioning of the retinaculum and removal of the tendons caused an average increase of 15% in anterior ankle displacement, indicating that the peroneal tendons may impart some static stability to the ankle joint.13 This finding may explain the increased incidence of peroneal tendon problems in patients with chronic ankle instability.
Mechanisms of Chronic Lateral Ankle Instability
When the ankle is dorsiflexed, the talus fits snuggly into the mortise and the ATFL is loose, but when the foot is plantar flexed, the ATFL becomes vertical and serves as the primary stabilizing structure of the ankle in inversion. Injury to the ATFL occurs with inversion of a plantar-flexed ankle with or without internal rotation. Commonly, the CFL is injured in combination with injury to the ATFL. Injures to the CFL occur with inversion of a dorsiflexed ankle. Subtalar ligament injury may be in continuum with a CFL injury. It has been shown that rupture of the ATFL occurs as an isolated injury in 50% to 75% of cases. With increasing force, the CFL also is ruptured. A rupture of the ATFL and the CFL occurs in 15% to 25% of cases. Isolated rupture of the CFL happens in approximately 1% of patients, and injury to the PTFL is extremely rare.8–10,14 Isolated ligament injuries of the deltoid ligament are infrequent.
Chronic lateral ankle instability results when the injured ligaments do not regain the mechanical integrity necessary to stabilize the ankle against physiologic stress. Possible risk factors for ankle instability that have been implicated in the literature include (1) environmental factors, such as the condition of the playing field, the level of neuromuscular training, the position an athlete plays, and the available equipment15 and (2) a patient’s unique anatomy, including variations in ankle anatomy, multiligamentous laxity, limitation of ankle range of motion, a history of recurrent ankle sprain, diminished muscle strength, poor postural control and proprioception, and delayed muscle reaction time.16 A varus tibial plafond alignment, a varus hindfoot alignment, and a posterior fibular position have also been proposed as possible predisposing factors in chronic ankle instability.17
Chronic lateral instability of the ankle usually manifests as a mechanical or a functional instability. Mechanical instability is objective abnormal motion of the talus relative to the ankle mortise, as measured on standardized stress radiographs or by clinical measurement of an anterior drawer sign or varus tilt.7,15 Functional instability is manifested as a symptomatic feeling of the ankle’s repeatedly giving way, combined with pain and difficulty walking on uneven terrain. Functional instability is most likely caused by increased laxity of the injured ligaments, inhibition of proprioceptive function, peroneal muscle weakness, or a combination of these factors.7,15 Some patients manifest functional instability without the mechanical components or vice-versa.
PATIENT EVALUATION
History and Physical Examination
Physical examination should include an evaluation of gait, generalized laxity, and hindfoot varus malalignment (Fig. 9-6). Proprioception testing is done by asking the patient to balance on the affected foot (single leg balance) or to perform a single leg jump-landing test with comparison to the contralateral side.18 Local ankle examination is often positive for tenderness to palpation over the affected ligaments with guarding, apprehension, and peroneal weakness.19
Clinical stress testing, including the talar tilt test and the anterior drawer test, may lead to the confirmation of a diagnosis of chronic ankle instability secondary to ligamentous insufficiency. The anterior drawer test is used to assess the ATFL. The talar tilt test evaluates the integrity of the CFL (Fig. 9-7). The talar tilt test also assesses subtalar instability in symptomatic patients. Thermann and colleagues described a provocative test for subtalar instability in which a varus stress to the calcaneus is applied with the ankle in 10 degrees of dorsiflexion and the talus locked in the ankle mortise. Subtalar pain or instability is considered a positive result.20
Diagnostic Imaging
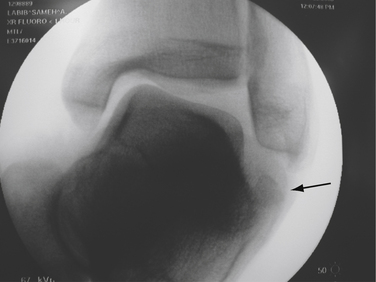
Radiographic evaluation of chronic ankle and subtalar instability is very important in ruling out the other differential diagnoses of chronic ankle pain. Plain radiographs in the standing position are used to evaluate hindfoot varus (Saltzman hindfoot view),21 talus osteochondral lesions, or concomitant fractures. The Os subfibulare is nonunion of a distal fibula avulsion fracture of the ATFL insertion that may require repair (Fig. 9-8).
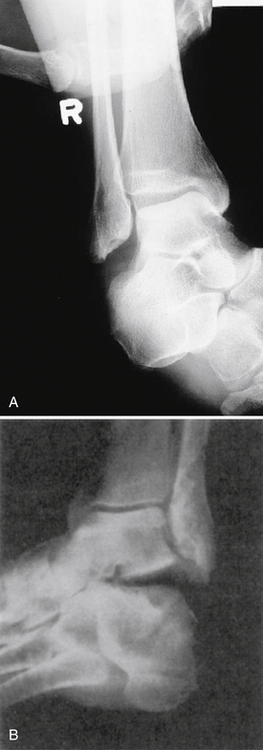
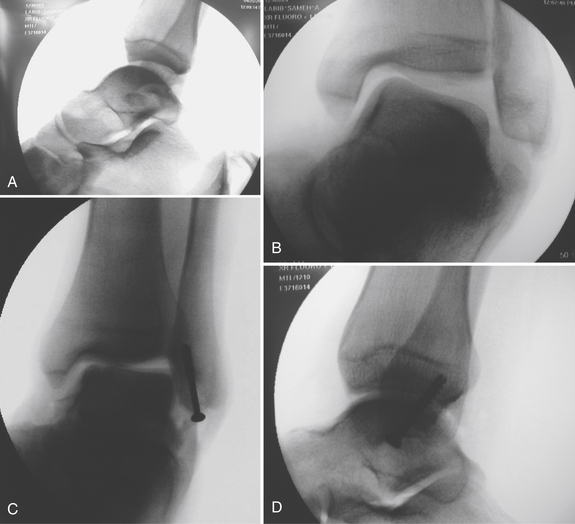
Radiographic tests of laxity demonstrating lateral instability (talar tilt test) and anterior instability (anterior talar translation tests) are pivotal in the objective assessment of ankle instability. These become even more pronounced and informative when performed with the patient under anesthesia (Fig. 9-9AR). How much talar translation or varus tilt is abnormal is a subject of much debate, with a wide range of values described in the literature.4,22 However, a reasonable guideline is an absolute tibiotalar anterior translation of greater than 10 mm, or greater than 3 mm more than the opposite normal ankle. A varus talar tilt angle greater than 15 degrees on the affected side, or 10 degrees more than the normal side, is considered positive for chronic ankle instability.4 A 30-degree cephalad view of a talar tilt stress test or a Broden view is used to assess subtalar instability (see Fig. 9-9). MRI examination has proved essential in the preoperative evaluation of ankle instability and ligament visualization. Concomitant talus osteochondral lesions, intra-articular impingement, or peroneal tendon injuries are common MRI findings that need to be addressed at the time of surgery.23
TREATMENT
Indications and Contraindications for Surgical Treatment
Not all patients with ligamentous laxity require surgery. The principal indication for surgical intervention is recurrent giving-way or instability despite proprioceptive training in patients who have mechanical laxity. Relative contraindications to surgery include instability caused by collagen disease, coalitions of the tarsal bones, and functional instability without mechanical instability.4,15,17 Absolute contraindications include advanced ankle arthritis, Charcot’s neuroarthropathy, and neurologic conditions leading to muscle imbalance or paralysis.
Management of Chronic Lateral Ankle Instability
Before surgical treatment of chronic lateral ligament insufficiency is considered, a supervised rehabilitation program that is based on peroneal muscle strengthening and proprioception training should be completed. Ankle bracing is also beneficial.16
Although an all-arthroscopic procedure for lateral ankle instability is possible,24 open repair remains the standard of care for ankle and subtalar instability.16 Concomitant arthroscopy of the ankle joint followed by reconstruction of the ligaments is now common practice. This is particularly important because of the association of ankle instability with concomitant intra-articular pathology.25
Several procedures have been described for the treatment of ankle instability, and the success rate varies from 50% to more than 90% in most series in the literature.17 These surgeries can be divided into secondary “native” ligament repair and imbrications (anatomic) and ligament reconstructions with free tendon grafts or transfers (nonanatomic). Three classic nonanatomic repairs—the Evans, Watson-Jones, and Chrisman-Snook techniques—were widely used in the past, with variable short- and long-term results.15,16 Major disadvantages of nonanatomic techniques are the sacrifice of normal, well-functioning anatomic structures around the ankle joint (e.g., peroneal tendons) and the limitation of ankle motion with alteration of normal kinematics of the ankle, which leads to joint degeneration and skin- and nerve-related complications. Late deterioration is common with these procedures and results in increasing laxity, reduction of ankle function, and increased pain.7,15,16,26
Because of the drawbacks associated with nonanatomic procedures, anatomic reconstruction of the lateral ankle ligaments is regarded as the surgical treatment of choice for patients with chronic ankle instability. However, nonanatomic repair does still play a role in certain situations, such as in cases of failed surgical stabilization, absence of adequate ligament tissue, and joint hyperlaxity.7 Anatomic reconstruction of the ankle ligaments involves suturing of the remnants of the original ligaments (as described by Brostrom) or reconstruction of the original ligament ends with reinforcement using adjacent tissues, including the periosteum or inferior extensor retinaculum (Gould modification of the Brostrom procedure).27–29 Satisfactory long-term functional results after anatomic reconstruction using the Gould modification have been published.29,30 The damaged or elongated remnants of the ATFL and CFL are divided, shortened 3 to 5 mm, and imbricated or reinserted into bone.
Preferred Surgical Treatment
The Gould modification of the Brostrom procedure for reconstruction of chronic lateral ankle instability is preferred. We prefer to perform an initial diagnostic arthroscopy before undertaking the repair of the lateral ankle ligaments. Chronic lateral ankle instability is associated with intra-articular pathology in up to 93% of cases, as described by Ferkel and others.25,31,32 These intra-articular abnormalities include loose bodies, osteochondral defects, synovitis, adhesions, chondromalacia, and osteophytes. Failure to recognize or appreciate these abnormalities could compromise results of ankle instability repair.
Surgical Procedure
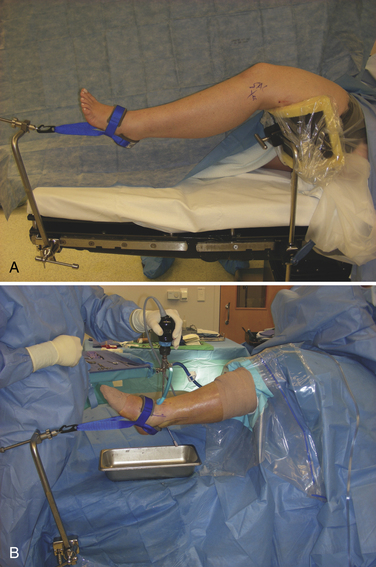
The patient is positioned supine on the operating table, and intravenous antibiotics are administered. A bump is placed under the hip of the operative side. An examination under anesthesia (EUA) with specific use of fluoroscopy is performed, to further document positive findings on the anterior drawer and talar tilt tests (see Fig. 9-9). After a proximal thigh tourniquet is placed, a thigh holder is positioned under the operative side with hip flexion at 60 degrees. To avoid compression of the neurovascular structures, the holder should not impinge on the popliteal fossa when the leg is flexed at the knee (Fig. 9-10). Skin preparation is then performed in a standard fashion.
After the extremity is draped, the medial and lateral malleoli, anterior tibialis tendon, superficial peroneal nerve, and standard arthroscopic portals are marked out. An Esmarch bandage or ace wrap is used to exsanguinate the leg, and the tourniquet is inflated. The leg is then placed in a Guhl noninvasive ankle distractor set (Smith and Nephew), and the appropriate tension is dialed to distract the joint. A 21-point diagnostic arthroscopic examination of the ankle is performed to ensure a thorough evaluation of the joint.25 The arthroscopic procedure is described in other chapters of this text. Appropriate treatment of incidental lesions can be undertaken before the ligamentous repair. Care is taken to minimize fluid extravasations during the procedure. This is best accomplished with the use of low-pressure arthroscopy done in an expeditious manner. In our hands, the average ankle arthroscopy takes between 15 and 20 minutes.
Brostrom-Gould Repair
After the diagnostic arthroscopy, the leg is removed from the Guhl distractor, and the thigh holder is removed before the Brostrom-Gould repair is commenced (video 1). With the patient still lying supine, attention turned to the lateral ankle. At this time, the appropriate landmarks are marked out, including the distal fibula and superficial peroneal nerve (SPN). The skin incision depends on the planned surgical procedure. For a classic Brostrom repair, a curvilinear incision just anterior to fibula is used (Fig. 9-11A). This incision should start at the ankle joint line, 1 cm anterior to the distal fibula, and extend in a curvilinear fashion just inferior and posterior to the tip of the fibula, almost like a C shape for the left ankle and a backward C shape for the right ankle. If hindfoot varus correction with a valgus (Dwyer) calcaneal osteotomy will be necessary, a second incision is made posterior to the fibula and parallel to the peroneal tendons (see Fig. 9-11B). In the case of concomitant peroneal tendon involvement, the initial incision is changed to an extended, posteriorly based, lateral incision following the peroneal tendons. With this incision, an anterior flap is raised to expose the capsule and extensor retinaculum (see Fig. 9-11C). Care is taken to elevate full-thickness tissue flaps anteriorly, to expose the ATFL and the inferior extensor retinaculum, and inferiorly, to expose the peroneal tendons and the calcaneal tuberosity. It is important to identify and protect the intermediate dorsal cutaneous branch of the superficial peroneal nerve as it courses over the extensor retinaculum anterior to the fibula. We extend the skin incision and subcutaneous dissection posterior to the fibula to expose the calcaneus, because the CFL attachment is relatively posterior on the calcaneus. The lateral extent of the inferior extensor retinaculum is identified and mobilized for later reconstruction to the fibula (Fig. 9-12).
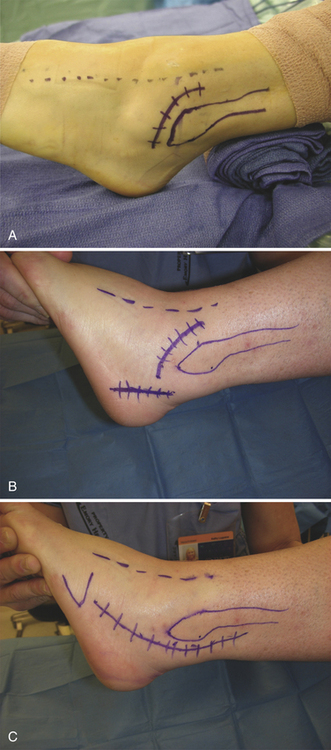
FIGURE 9-11 A, For a classic Brostrom repair, a curvilinear incision just anterior to fibula is marked out. B, If hindfoot varus correction with a valgus (Dwyer) calcaneal osteotomy will be necessary, a second incision is made posterior to the fibula and parallel to the peroneal tendons. C, In the case of concomitant peroneal tendon involvement, the initial incision is changed to an extended, posteriorly based, lateral incision following the peroneal tendons. With this incision, an anterior flap is raised to expose the capsule and extensor retinaculum.
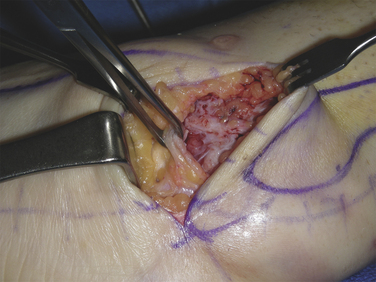
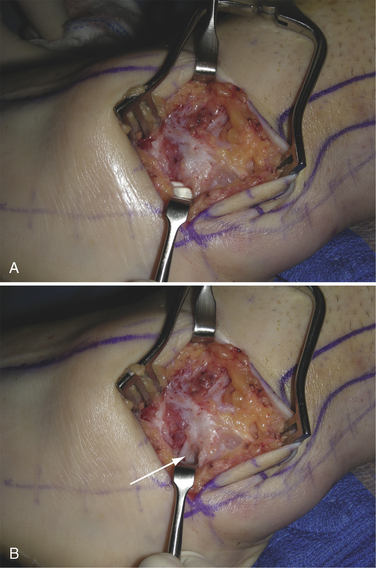
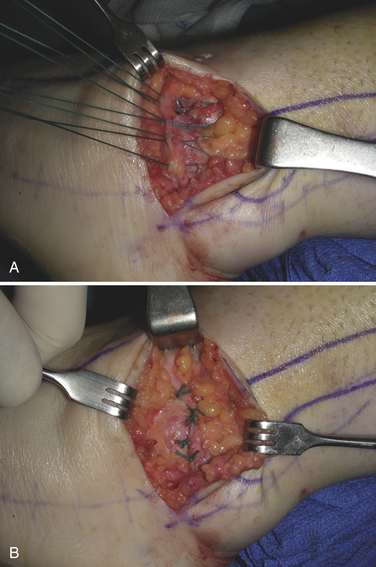
The peroneal sheath is incised, and the tendons are retracted from their sheath to expose the underlying CFL (Fig. 9-13). At this point, the torn edges of the ATFL and CFL or laxity within the ligaments can be identified. Often, the ATFL stump cannot be easily identified because it blends with the ankle joint capsule. The ATFL is usually transected during the repair as the arthrotomy is made in line with the anterolateral capsule incision at the ankle joint (Fig. 9-14). The talofibular joint space should now be visualized and inspected for any additional pathology, with care taken not to damage the underlying cartilage. The CFL is identified underneath the peroneals, and its laxity is assessed in dorsiflexion. If the remaining portions of either ligament appear too small to repair, the tissue is excised, and periosteum is elevated from the underlying fibula to create flaps for later repair to the residual ATFL and CFL.
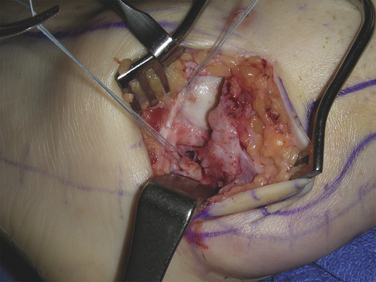
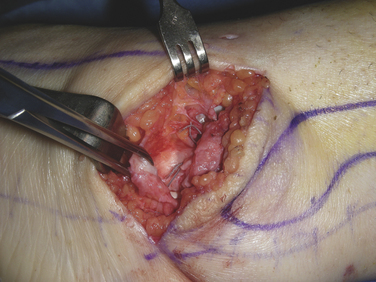
A 2-0 fortified polyester suture (Fiberwire, Arthrex, Naples, FL) is used to imbricate the ATFL and capsule in a “pants over vest” fashion. This stitch starts on the distal side and then crosses over to the proximal side with a near-far–far-near sequence (see Fig. 9-14). The CFL is imbricated in a similar manner. All sutures should be placed before any knots are tied. After all sutures are placed, the ankle is held reduced in neutral and eversion while all sutures are tied (Fig. 9-15). If the ligaments have avulsed off of the bone rather than rupturing midsubstance, they can be repaired with suture anchors (mini-corkscrew anchors) or tied over a bone bridge after a small trough is made for the ligaments. Sutures are then placed in the remaining capsular tissues and tied. We routinely perform the Gould modification in which the inferior extensor retinaculum is mobilized, advanced proximally over the area of reconstruction, and then repaired to the distal fibula periosteum with no. 0 nonabsorbable polyester suture (Fig. 9-16). To judge the adequacy of the repair, the foot is held up with the hip in full internal rotation and should maintain an everted position against gravity (i.e., negative gravity test) (Fig. 9-17). The tissues are then closed in layers with 2-0 Vicryl for the subcutaneous layer and 3-0 Monocryl for the skin. The extremity is placed in a well-padded splint after sterile dressings are applied, in a position of eversion and neutral ankle dorsiflexion.
Special Considerations
A detailed preoperative examination is extremely helpful, because comorbid conditions can change the surgical plan. For example, if the patient displays peroneal pathology (peroneal instability, peroneal tear) on examination or on MRI, the operative plan should also address these issues. In such a case, the incision would be a posterior extensile incision around the fibula (to deal with both issues) rather than an anterior incision (see Fig. 9-11C).
Another important issue to evaluate is hindfoot varus (see Fig. 9-6). We agree with other authors that, in patients with chronic ankle instability and hindfoot varus, surgical reconstruction of the lateral ligamentous complex without addressing the hindfoot varus leads to higher failure rates. We believe that hindfoot varus is a predisposing factor to inversion ankle sprains, which, in turn, lead to injury of the lateral ligamentous complex. In such cases, one would plan on performing a concomitant calcaneal lateral closing wedge (Dwyer) osteotomy. There would be two laterally based incisions for this procedure: the standard anterior curvilinear incision for the Brostrom-Gould reconstruction and an oblique lateral incision over the posterior calcaneus for the osteotomy (see Fig. 9-11B).
It is also important to be mindful of the symptomatic os subfibulare, which is an avulsion fracture of the distal fibula that resulted in a nonunion. This fracture fragment usually contains the attachment site of the ATFL, with or without that of the CFL, and can result in lateral ligament instability. Sometimes this is not evident until stress radiographs are obtained (Fig. 9-18). The treatment for this condition is open reduction and internal fixation of the fracture fragment with a partially threaded cancellous screw (video 2). If the piece of bone is too small to be captured with a screw, suture anchors may be used for the repair.
1. Garrick JG. The frequency of injury, mechanism of injury, and epidemiology of ankle sprains. Am J Sports Med. 1977;5:241-242.
2. Freeman M, Dean M, Hanham I. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47:678-685.
3. Burks RT, Morgans J. Anatomy of the lateral ankle ligaments. Am J Sports Med. 1994;22:72-77.
4. Clanton TO. Athletic injuries to the soft tissues of the foot and ankle. In: Coughlin MJ, Mann RA, editors. Surgery of the Foot and Ankle. ed 7. St Louis, MO: Mosby; 1999:1090-1209.
5. Scranton PEJr, McDermott JE, Rogers JV. The relationship between chronic ankle instability and variations in mortise anatomy and impingement spurs. Foot Ankle Int. 2000;21:657-664.
6. Van Bergeyk AB, et al. CT analysis of hindfoot alignment in chronic lateral ankle instability. Foot Ankle Int. 2002;23:37-42.
7. Ajis A, Younger A, Maffuli N. Anatomic repair for chronic lateral ankle instability. Foot Ankle Clin. 2006;11:539-545.
8. Rasmussen O. Stability of the ankle joint. analysis of the function and traumatology of the ankle ligaments, Acta Orthop Scand Suppl. 2111985 1-75.
9. Kjaersgaard-Andersen P, Wethelund J, Helmig P, et al. Effect of the calcaneofibular ligament on hindfoot rotation in amputation specimens. Acta Orthop Scand. 1987;58:135-138.
10. Lassiter TEJr, Malone TR, Garret WEJr. Injury to the lateral ligaments of the ankle. Orthop Clin North Am. 1989;20:629-640.
11. Tochigi Y, Amendola A, Rudert MJ, et al. The role of the interosseous talocalcaneal ligament in subtalar joint stability. Foot Ankle Int. 2004;25:588-596.
12. Clarke HD, Kitaoka HB, Ehman RL. Peroneal tendon injuries. Foot Ankle Int. 1988;19:280-288.
13. Hatch GF, Labib SA, Hutton W. Role of the peroneal tendons and superior peroneal retinaculum as static stabilizers of the ankle. J Surg Orthop Adv. 2007;16:187-191.
14. Freeman M. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47:669-676.
15. Watson AD. Ankle instability and impingement. Foot Ankle Clin. 2007;12:177-195.
16. Maffulli N, Ferran NA. Management of acute and chronic ankle instability. J Am Acad Orthop Surg. 2008;16:608-615.
17. Coughlin MJ, Mann RA, Saltzman CL. Surgery of the Foot and Ankle. Philadelphia, PA: Mosby Elsevier; 2007. 1467-1468
18. Ross SE, Guskiewicz KM. Examination of static and dynamic postural stability in individuals with functionally stable and unstable ankles. Clin J Sport Med. 2004;14:332-338.
19. Renstrom AFH, Lynch SA. Acute ligament injuries of the ankle. Foot Ankle Clin. 1999;4:697-711.
20. Thermann H, Zwipp H, Tscherne H. Treatment algorithm of chronic ankle and subtalar instability. Foot Ankle Int. 1997;18:163-169.
21. Saltzman CL, El-Khoury GY. The hindfoot alignment view. Foot Ankle Int. 1995;16:572-576.
22. Scranton PE. Sprains and soft-tissue injuries. In: Pfeffer GB, editor. Chronic Ankle Pain in the Athlete. ed 1. Rosemont, IL: American Academy of Orthopedic Surgeons; 2000:3-20. Monograph series
23. Griffith JF, Brockwell J. Diagnosis and imaging of ankle instability. Foot Ankle Clin. 2006;11:475-496.
24. Maiotti M, Massoni C, Tarantino U. The use of arthroscopic thermal shrinkage to treat chronic lateral ankle instability in young athletes. Arthroscopy. 2005;21:751-757.
25. Ferkel RD, Chams RN. Chronic lateral instability. arthroscopic findings and long term results, Foot Ankle Int. 282007 24-31.
26. Kaikkonen A, Kannus P, Jarvinen M. Surgery versus functional treatment in ankle ligament tears. Clin Orthop Relat Res. 1996;326:194-202.
27. Brostrom L. Sprained ankles. VI. Surgical treatment of “chronic” ligament ruptures. Acta Chir Scand. 1966;132:551-565.
28. Gould N, Seligson D, Gassman J. Early and late repair of lateral ligament of the ankle. Foot Ankle. 1980;1:84-89.
29. Hamilton WG, Thompson FM, Snow SW. Modified Brostrom procedure for lateral ankle instability. Foot Ankle. 1993;14:1-7.
30. Krips R, Van Dijk CN, Halasi PT, et al. Long-term outcome of anatomical reconstruction versus tenodesis for the treatment of chronic anterolateral instability of the ankle joint. a multi-center study, Foot Ankle Int. 222001 415-442.
31. Komenda G, Ferkel R. Arthroscopic findings associated with the unstable ankle. Foot Ankle Int. 1999;20:708.
32. Hintermann B, Boss A, Schäfer D. Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med. 2002;30:402-409.