Chapter 16 Instability
The term ‘instability’ has crept into the literature on low back pain as a diagnostic entity. The implication is that the patient has something wrong biomechanically in their back, and that this is somehow the cause of their pain. Furthermore, since the cause of pain is biomechanical in nature, its treatment should be mechanical. The notion of lumbar instability, however, has become very controversial, as is evident in several reviews1,2 and symposia.3–5 Physicians have abused the term and have applied it clinically without discipline and without due regard to available biomechanical definitions and diagnostic techniques.
Biomechanics
Instability has been defined as a condition of a system in which the application of a small load causes an inordinately large, perhaps catastrophic, displacement.6 This definition conveys the more colloquial sense of something that is about to fall apart or could easily fall apart. Bioengineers have insisted that instability is a mechanical entity and should be treated as such,7 but how biomechanists have portrayed the definition graphically in mathematical terms has evolved over recent years, as more and more embellishments and alternatives have been added.
Stiffness
An early definition simply maintained that instability was loss of stiffness.7 A later elaboration introduced a clinical dimension, to the effect that instability is a
loss of spinal motion segment stiffness such that force application to the structure produces a greater displacement(s) than would be seen in a normal structure, resulting in a painful condition, the potential for progressive deformity, and that places neurologic structures at risk.8
Other engineers have disagreed, insisting that any definition of instability should include the sense of sudden, unpredictable behaviour; that a small load causes a large, perhaps catastrophic, displacement.6 They argue that loss of stiffness may simply describe loose or hypermobile segments that are not at risk of catastrophic collapse.
Neutral zone
a significant decrease in the capacity of the stabilising system of the spine to maintain the intervertebral neutral zones within the physiological limits so that there is no neurological dysfunction, no major deformity, and no incapacitating pain.9
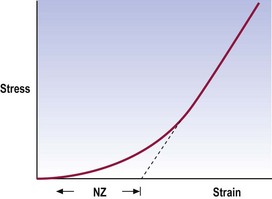
The neutral zone is that part of the range of physiological intervertebral motion, measured from the neutral position, within which the spinal motion is produced with a minimal internal resistance.9 In essence, although not exactly the same mathematically, it is similar to the length of the toe phase of the stress–strain curve that describes the behaviour of the segment (Fig. 16.1).
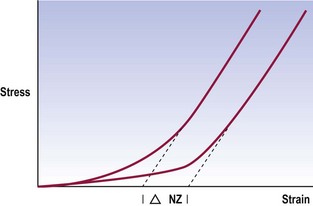
This definition describes joints that are loose but early in range. Their ultimate strength may be normal but early in range they exhibit excessive displacement (Fig. 16.2). This definition captures the sense of excessive displacement; it captures the sense of excessive displacement under minor load but it defies the engineering sense of impending catastrophic failure. However, it does so deliberately and not totally without regard to catastrophe.
Instability factor
Flexion–extension of the lumbar spine is not a singular movement; it involves a combination of rotation and translation (see Ch. 8). Notwithstanding the range of motion, the quality of motion may be defined in terms of the ratio between the amplitude of translation and the amplitude of rotation. For each phase of movement there should be a certain amount of translation accompanied by an appropriate degree of rotation. If this ratio is disturbed, the motion becomes abnormal and the sense of instability may arise. In this regard, the instability would be defined as an inordinate amount of translation for the degree of rotation undergone, or vice versa.
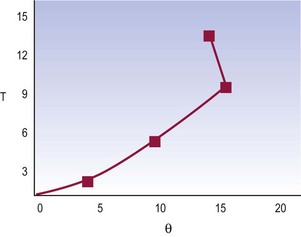
Normal lumbar segments exhibit an essentially uniform ratio of translation to rotation during flexion–extension.10 The overall pattern of movement looks smooth; translation progresses regularly, as does rotation (Fig. 16.3). The ratio between translation and rotation at any phase of movement is the same as the ratio between total translation and total rotation.
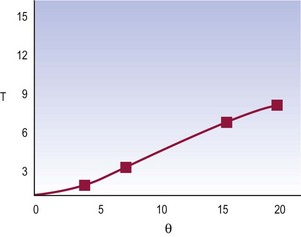
Figure 16.3 A normal movement pattern of a lumbar segment in terms of the ratio between translation and rotation.
(Based on Weiler et al. 1990.10)
It may be defined that instability occurs when, at any time in the movement, there is an aberration to this ratio. The segment suddenly exhibits an inordinate translation for the degree of rotation undergone, or may translate without any rotation (Fig. 16.4).
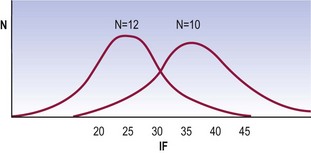
where (ΔT)i is the range of translation for each phase of motion (i) and (Δθ)i is the range of rotation for each phase.10 In normal spines, the instability factor has a mean value of 25 (mm radian−1) and a standard deviation of 8.7. Values beyond the upper two SD range nominally qualify for instability.
Anatomy
In principle, a spectrum of possibilities arises (Fig. 16.5). Instability may be related to the extent of injury to a segment and the factors that remain trying to stabilise it. At one extreme lies complete dislocation, where no factors maintain the integrity of the segment. At the opposite extreme lies an intact segment that is absolutely stable. Between lies a hierarchy of possibilities.
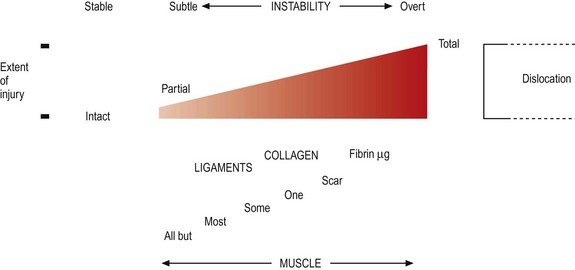
Figure 16.5 The relationship between instability, extent of injury and the factors maintaining stability.
For any degree of stability, the segment requires its stabilising elements: its facets and ligaments (see Chs 3 and 4). The fewer of these that are intact, the more liable the segment is to catastrophic failure; the more that are intact, the more stable the segment becomes.
Numerous studies have been conducted that demonstrate how progressively removing each of the restraining elements progressively disables a lumbar motion segment. Transecting the posterior longitudinal ligament and posterior anulus fibrosus produces hypermobility, even when other elements remain intact.11 Progressively transecting the supraspinous and interspinous ligaments, ligamentum flavum, joint capsules, facets, the posterior longitudinal ligament and the posterior anulus fibrosus leads to progressively greater displacements when a segment is loaded in flexion, with the greatest increase in displacement occurring after transection of the posterior disc.12 Short of transecting the disc, the zygapophysial joints appear to be the major stabilising elements in flexion.13,14
Superimposed on the facets and ligaments are muscles. These contribute to stability in two ways. The lesser mechanism is to pull directly against threatened displacements. In this regard, however, the back muscles are not well oriented to resist anterior or posterior shear or torsion; they run longitudinally and can only resist sagittal rotation (see Ch. 9). However, whenever the muscles act they exert compressive loads on the lumbar spine. This achieves a stabilising effect. By compressing joints, the muscles make it harder for the joints to move, and a variety of studies have now documented the stabilising effect of muscles on the lumbar spine.15,16 Specifically, muscle contraction decreases the range of motion and decreases the neutral zone of lumbar spinal segments, with the multifidus contributing the strongest influence.16
• Overt failure or impending failure is readily recognised radiographically in conditions such as fracture-dislocation when a vertebra exhibits malposition or an excessive motion apparent to the unaided eye. In such circumstances, instability is beyond doubt because the evident motion could not possibly have occurred unless the restraining elements were totally disrupted. However, the challenge obtains to determine the threshold for instability when the abnormal motion is not readily apparent.
• For instability within range, the challenge is to demonstrate its presence and to be certain that the abnormal motion is responsible for the patient’s symptoms.
Hypothetical models
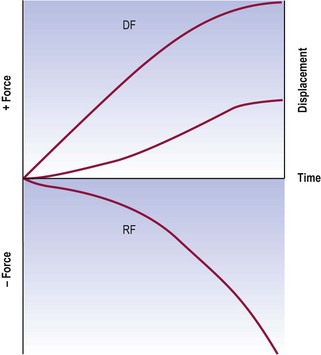
The concepts offered by biomechanists can be collated and summarised graphically using a unifying device: a force and displacement graph (Fig. 16.6). For any lumbar movement there will be a force that induces displacement. Acting against this force will be restraining forces that stem from the facets, ligaments and muscles of the segment. These restraining forces act to prevent uncontrolled acceleration of the segment, under gravity for example. Given an appropriate combination of displacing forces and restraining forces, motion occurs; displacement progresses with time, and a velocity of motion emerges. The graph (see Fig. 16.6) shows the two opposing sets of forces and the change of displacement. The slope of this latter curve will be the velocity of movement. Under normal conditions, as displacing forces build up, the segment accelerates. As long as displacing forces exceed the restraining forces, movement continues. Towards the end of range, restraining forces exceed the displacing forces and movement decelerates, eventually stopping at end of range.
If a segment suffers a loss of stiffness, the restraining forces that resist forward flexion are reduced, but the gravitational forces that produce forward bending are unaltered and displacing forces remain the same (Fig. 16.7). As a result, the acceleration and eventual velocity of the resultant movement must, prima facie, be greater. Instability ensues if the balance between the displacing and restraining forces is insufficient to prevent inordinate displacement or the threat of failure of the segment. Such instability obtains both throughout range and at terminal range.
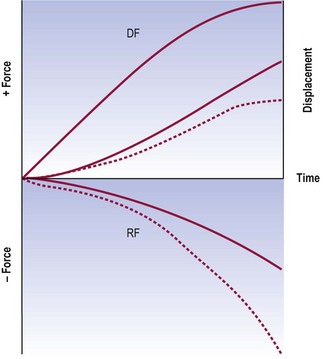
Figure 16.7 A force and displacement diagram of a motion segment with decreased stiffness. Throughout the range, the restraining forces (RF) are considerably less than the displacing forces (DF) and the segment develops a higher than normal velocity towards end of range. For comparison, the normal curves for restraining forces and displacement (see Fig. 16.6) are shown as dotted lines.
If a segment suffers a loss of restraints that operate early in range but no loss of terminal restraints, the restraining forces will exhibit an increased neutral zone, but the displacing forces are unchanged (Fig. 16.8). As a result, the motion segment exhibits an essentially normal early velocity but as the difference between displacing and restraining forces increases, it accelerates and eventually exhibits a higher than normal velocity. The sense of instability arises because the terminal velocity is excessive and unexpected. Instead of the accustomed pattern of motion, there is an unfamiliar acceleration, which is alarming because it predicts (albeit inappropriately) that, at this rate of displacement, the segment threatens to fall apart.
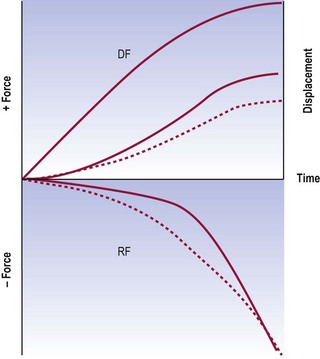
Figure 16.8 A force and displacement diagram of a motion segment with an increased neutral zone. The displacing forces (DF) and restraining forces (RF) are imbalanced early in range, and the segment accelerates towards end of range and develops a higher than normal terminal velocity. For comparison, the normal curves for restraining forces and displacement (see Fig. 16.6) are shown as dotted lines.
If a segment suffers a loss of restraints that operate in mid-range or late in range, initial movements may be normal but the loss of restraints results in an acceleration late in range (Fig. 16.9). This acceleration is alarming because it feels as if the segment is about to shoot out of control.
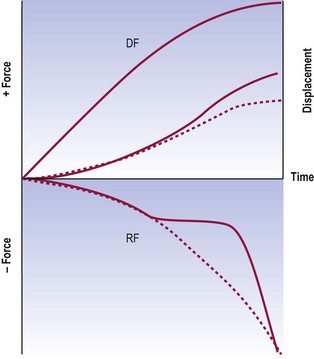
Figure 16.9 A force and displacement diagram of a motion segment exhibiting instability in mid-range. Early in range the balance between displacing forces (DF) and restraining forces (RF) is normal, and a normal velocity of movement occurs. When suddenly a restraining component fails to engage, the movement accelerates, reaching a higher than normal terminal velocity. For comparison, the normal curves for restraining forces and displacement (see Fig. 16.6) are shown as dotted lines.
Clinical instability
One use is explicitly clinical and temporal; it bears no relationship to biomechanics. It maintains that clinical instability is a condition in which the clinical status of a patient with back problems steps, with the least provocation, from the mildly symptomatic to the severe episode.17 Philosophically and semantically this does amount to instability in the sense that a trivial force causes a major displacement, but the displacement is not of a mechanical entity; it is a displacement of the patient’s symptoms or of their clinical course. This use of the term is akin to speaking of an individual’s mood or emotions being ‘unstable’. This use of the term should not be confused or equated with the biomechanical use. More seriously, because it lacks any relationship to biomechanics, a diagnosis of clinical instability does not suggest, let alone indicate, mechanical therapy. There is a risk that, because ‘clinical instability’ and ‘biomechanical instability’ sound alike, they are equivalent. They are not.
The diagnosis of instability still hinges on biomechanical tests.
Diagnosis
Criteria
Various authorities have issued guidelines for the legitimate use of the term instability.8,18 The major categories are shown in Table 16.1. Categories I, II and III are beyond controversy. Each involves a condition that threatens the integrity of the spine and which can be objectively diagnosed by medical imaging, perhaps supplemented by biopsy.
| Category | Causes |
|---|---|
| I | Fractures and fracture-dislocations |
| II | Infections of the anterior elements |
| III | Neoplasms |
| IV | Spondylolisthesis |
| V | Degenerative |
Spondylolisthesis rarely progresses in adults19 or teenagers,20 and therefore it appears inherently stable, despite its threatening appearance. Indeed, biplanar radiography studies of moving patients have shown that, if anything, grade 1 and grade 2 spondylolisthesis are associated with reduced range of motion rather than instability.21 However, some patients with spondylolisthesis may exhibit forward slipping upon standing from a lying position,22 but it is not clear whether the extent of slip in such cases is abnormal. Studies, using implanted tantalum balls in order to establish landmarks accurately, have found no evidence of instability.23 In some patients, movement abnormalities may be revealed using special radiographic techniques, which include having the patient stand loaded with a 20 kg pack and hanging by their hands from an overhead bar.24,25 These extreme measures, however, have been criticised as unrealistic and cumbersome.6
It is with respect to degenerative instability that the greatest difficulties arise. A classification system of this category of lumbar instability has been proposed (Box 16.1).8,18 The secondary instabilities are easy to accept and understand. They involve surgical destruction of one or more of the restraining elements of the spine, and are thereby readily diagnosed on the basis of prior surgery and subsequent excessive or abnormal motion. It is the primary instabilities that pose the greatest difficulties.
Rotational instability has been described as a hypothetical entity.26 Based on clinical intuition, certain qualitative radiographic signs have been described17 but their normal limits have not been defined, nor has their reliability or validity been determined. Consequently, rotational instability remains only a hypothetical entity.
Translational instability is perhaps the most classic of all putative instabilities. It is characterised by excessive anterior translation of a vertebra during flexion of the lumbar spine. However, anterior translation is a normal component of flexion (see Ch. 8). The difficulty that arises is setting an upper limit of normal translation. Posner et al.12 prescribed a limit of 2.3 mm or 8% of the length of the vertebral endplate for the L1–L4 vertebrae, and 1.6 mm or 6% for the L5 vertebra. Boden and Wiesel27 however, demonstrated that many asymptomatic individuals exhibited static slips of such magnitude, and emphasised that, in the first instance, any slip should be dynamic before instability could be considered. A dynamic slip is one that is evident in full flexion but not in extension, or vice versa. Furthermore, even dynamic slips of up to 3 mm can occur in asymptomatic individuals; only 5% of an asymptomatic population exhibited slips greater than 3 mm. Accordingly, Boden and Wiesel27 have advocated that 3 mm should be the threshold limit for diagnosing anterior translational instability. Hayes et al.,28 however, found that 4 mm of translation occurred in 20% of their asymptomatic patients. Accordingly, 4 mm might be a better threshold limit.
Belief in retrolisthetic instability dates to the work of Knutsson.29 He maintained that degenerative discs exhibited instability in the form of abnormal motions, notably retrolisthesis upon extension of the lumbar spine. This contention, however, was subsequently disproved when it was shown that similar appearances occurred in asymptomatic individuals.28,30 As a result, there are no operational criteria for instability due to retrolisthesis, other than the guidelines of Boden and Wiesel27 or Hayes et al.,28 which state that up to 3 mm or 4 mm of translation can be normal.
Although positive correlations are lacking between disc degeneration and retrolisthetic rotational and translational instability, there are associations between disc degeneration and a raised instability factor.10 Patients with disc degeneration exhibit a greater mean value of instability factor that is statistically significant (Fig. 16.10). However, because the technique for determining the instability factor is very demanding and time consuming, this method of studying instability has not been pursued further, to date.
Clinical diagnosis
Various clinical criteria have been proclaimed as indicative or diagnostic of lumbar instability.17,31,32 At best, these constitute fancy. To be valid, clinical signs have to be validated against a criterion standard. The only available criterion standard for instability is offered by radiographic signs, but the radiographic signs of instability are themselves beset with difficulties. Consequently, no studies have yet validated any of the proclaimed clinical signs of instability.
1 Nachemson AL. Instability of the lumbar spine: pathology, treatment, and clinical evaluation. Neurosurg Clin North Am. 1991;2:785-790.
2 Pope MH, Frymoyer JW, Krag MH. Diagnosing instability. Clin Orthop. 1992;279:60-67.
3 Kirkaldy-Willis WH. Presidential symposium on instability of the lumbar spine: introduction. Spine. 1985;10:254.
4 Nachemson A. Lumbar spine instability: a critical update and symposium summary. Spine. 1985;10:290-291.
5 Wiesel S. Editor’s corner. Semin Spine Surg. 1991;3:91.
6 Ashton-Miller JA, Schultz AB. Spine instability and segmental hypermobility biomechanics: a call for the definition and standard use of terms. Semin Spine Surg. 1991;3:136-148.
7 Pope MH, Panjabi M. Biomechanical definitions of spinal instability. Spine. 1985;10:255-256.
8 Frymoyer JW, Pope MH. Segmental instability. Semin Spine Surg. 1991;3:109-118.
9 Panjabi MM. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord. 1992;5:390-397.
10 Weiler PJ, King GJ, Gertzbein SD. Analysis of sagittal plane instability of the lumbar spine in vivo. Spine. 1990;15:1300-1306.
11 Akkerveeken PF, O’Brien JP, Parl WM. Experimentally induced hypermobility in the lumbar spine: a pathologic and radiologic study of the posterior ligament and annulus fibrosus. Spine. 1979;4:236-241.
12 Posner I, White AA, Edwards WT, et al. A biomechanical analysis of the clinical stability of the lumbar and lumbosacral spine. Spine. 1982:374-389.
13 Abumi K, Panjabi MM, Kramer KM, et al. Biomechanical evaluation of lumbar spinal stability after graded facetectomies. Spine. 1990;15:1142-1147.
14 Pintar FA, Cusick JF, Yoganandan N, et al. The biomechanics of lumbar facetectomy under compression–flexion. Spine. 1992;17:804-810.
15 Panjabi M, Abumi K, Duranceau J, et al. Spinal stability and intersegmental muscle forces: a biomechanical model. Spine. 1989;14:194-200.
16 Wilke HJ, Wolf S, Claes LE, et al. Stability increase of the lumbar spine with different muscle groups: a biomechanical in vitro study. Spine. 1995;20:192-198.
17 Kirkaldy-Willis WH, Farfan HF. Instability of the lumbar spine. Clin Orthop. 1982;165:110-123.
18 Hazlett JW, Kinnard P. Lumbar apophyseal process excision and spinal instability. Spine. 1982;7:171-176.
19 Fredrickson BE, Baker D, McHolick WJ, et al. The natural history of spondylosis and spondylolisthesis. J Bone Joint Surg. 1984;66A:699-707.
20 Danielson BI, Frennered AK, Irstam LKH. Radiologic progression of isthmic lumbar spondylolisthesis in young patients. Spine. 1991;16:422-425.
21 Pearcy M, Shepherd J. Is there instability in spondylolisthesis? Spine. 1985;10:175-177.
22 Lowe RW, Hayes TD, Kaye J, et al. Standing roentgenograms in spondylolisthesis. Clin Orthop. 1976;117:80-84.
23 Axelsson P, Johnsson R, Stromqvist B. Is there increased intervertebral mobility in isthmic adult spondylolisthesis? A matched comparative study using roentgen stereophotogrammetry. Spine. 2000;25:1701-1703.
24 Friberg O. Lumbar instability: a dynamic approach by traction–compression radiography. Spine. 1987;12:119-129.
25 Kalebo P, Kadziolka R, Sward L. Compression–traction radiography of lumbar segmental instability. Spine. 1990;15:351-355.
26 Farfan HF, Gracovetsky S. The nature of instability. Spine. 1984;9:714-719.
27 Boden SD, Wiesel SW. Lumbosacral segmental motion in normal individuals. Have we been measuring instability properly? Spine. 1990;15:571-576.
28 Hayes MA, Howard TC, Gruel CR, et al. Roentgenographic evaluation of lumbar spine flexion–extension in asymptomatic individuals. Spine. 1989;14:327-331.
29 Knutsson F. The instability associated with disk degeneration in the lumbar spine. Acta Radiol. 1944;25:593-609.
30 La Rocca H, MacNab I. Value of pre-employment radiographic assessment of the lumbar spine. Ind Med Surg. 1970;39:31-36.
31 Grieve GP. Lumbar instability. In: Grieve G, editor. Modern Manual Therapy of the Vertebral Column. Edinburgh: Churchill Livingstone; 1986:416-441.
32 Paris SV. Physical signs of instability. Spine. 1985;10:277-279.