CHAPTER 26 Inlay Posterior Cruciate Ligament Reconstruction
Treatment of posterior cruciate ligament (PCL) injuries has faced debate and continues to evolve. Debate is caused by the sparse number of PCL injuries available for surgical standardization of technique and the relative heterogeneity of these injuries. Posterior cruciate ligament tears are often not diagnosed because they are often asymptomatic. However, studies have shown that PCL injuries are more common than previously thought and can comprise up to 3% of knee injuries in the general population and 37% of trauma patients with an acute hemarthrosis.1,2 As the detection of such injuries improves, there will be a corresponding rise in the number of basic science and clinical studies investigating these injuries. The result will be improved understanding of the proper techniques for treatment and standardization of operative procedures. However, one issue that may continue to be subjective and thus more controversial is the indication for surgical intervention.
ANATOMY
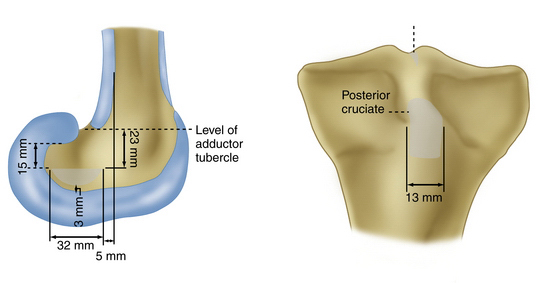
Knee stability requires the intact integrity of four ligaments—the anterior cruciate ligament (ACL), PCL, medial collateral ligament (MCL), and lateral collateral ligament (LCL). The PCL is the primary structure that confers static stabilization against posterior translation of the tibia with respect to the femur. The PCL averages 38 mm in length and 13 mm in width and is believed to be the stronger of the two cruciate liagments.3 Selective division of the PCL has shown that it is most important in flexion, although it acts as a check during hyperextension when the anterior cruciate ligament has been compromised.4 The PCL originates from the posterolateral aspect of the medial femoral condyle in the intercondylar notch and inserts on the posterior aspect of the tibial plateau (Fig. 26-1).5,6 The PCL is more vertically than obliquely oriented and the midpoint of its femoral attachment is 1 cm posterior to the articular cartilage.7 The insertion of the ligament is within a central depression about 1.0 to 1.5 cm distal to the articular surface of the posterior tibia in an area known as the PCL facet, or fovea.8 This posterior insertion is a major factor in anatomic reconstructive techniques because of its proximity to the popliteal vessels that may be injured during posterior approaches to the knee.
The posterior cruciate ligament has two major bands, also known as bundles. These bundles are named for their specific insertion on the femur (anterior or posterior) and tibia (lateral or medial).9 The anterolateral band is tight in flexion and loose in extension, and the posteromedial band is loose in flexion and tight in extension. The posteromedial band is half the size of the anterolateral band in cross section. The anterolateral band is reconstructed during single-bundle reconstruction. The PCL is also composed of meniscofemoral ligaments, the ligament of Humphry, which is located anteriorly, and the ligament of Wrisberg, located on the posterior aspect. These ligaments travel from the posterior horn of the lateral meniscus to the posteromedial femoral condyle.10
PATIENT EVALUATION
History and Physical Examination
Most patients with posterior cruciate ligament injuries do not report a pop or any feeling of subjective instability, which is distinctly different from anterior cruciate ligament injuries. Instead, most patients will complain of knee pain, swelling, or a “ funny feeling “ in the knee. The physician should inquire about to the chronicity of symptoms to classify the injury as acute or chronic. One of the most common mechanisms of PCL injury is the dashboard injury. This term is used to describe the phenomenon of the anterior tibia sustaining a posteriorly directed force from the dashboard with the knee in 90 degrees of flexion. In the case of an athlete, the history usually includes a direct blow to the anterior tibia or a fall on a flexed knee with the foot in plantar flexion. This is in contrast to a fall on a dorsiflexed foot, which causes patellofemoral injury. Isolated partial tears in athletes are often secondary to hyperflexion injuries, which can occur, for example, during a football tackle.10,11
On physical examination, several considerations must be made. Such considerations include the possibility of multiple ligament injuries, most notably the effect of a concurrent posterolateral corner (PLC) or ACL injury. When examining a knee with a PCL injury, it is often missed that the tibia is starting in a subluxed position and further posterior stress does not lead to additional translation. An anterior drawer does result in anterior translation and the diagnosis of an ACL tear can be erroneously made. Despite this, the most accurate clinical test of PCL integrity is the posterior drawer test. This is performed by placing the patient supine and placing a posteriorly directed force to the anterior tibia (Fig. 26-2) with the knee flexed at 90 degrees. The examiner palpates the medial joint line before applying force to determine the location of the tibia in relation to the medial femoral condyle.
Documentation of the examination should include the amount of translation and the presence of an end point. Traditional teaching described tibial translation in numeric terms. PCL injury was described as grade I for 0 to 5 mm of tibial translation, grade II for 5 to 10 mm of translation, and grade III for more than 10 mm of translation. However, many have suggested classifying PCL injuries based on the medial tibial plateau–medial femoral condyle position.12 The tibial plateau is usually 1 cm anterior to the femoral condyle. In the positional classification system, grade I injuries have some preservation of the anterior position of the tibia in relation to the femur, grade II injuries occur when the tibia is flush with the medial femoral condyle, and grade III injuries are manifested by displacement of the anterior tibia posterior to the medial femoral condyle. The ligament of Wrisberg and the ligament of Humphry are a part of the posterior cruciate ligament. These ligaments can confer stability with internal rotation and lead to a decrease in posterior laxity in this position.13
Other tests for PCL integrity include the posterior sag test (Godfrey test), quadriceps active test, and reverse pivot shift test.14 The posterior sag test involves flexing the hip to 45 degrees and the knee to 90 degrees and noting the posterior pull of gravity creating a sag or dimple at the joint line, indicating the posterior location of the tibia on the femur. The quadriceps active test involves watching for a reduction of this displacement by asking the patient to contract the quadriceps muscle. If the patient does not understand this request, one can ask the patient to try to extend the knee or kick the leg out while the examiner holds the foot down. The reverse pivot shift test is similar to the pivot shift evaluation performed with ACL injury.15 The position of the hands on the knee is the same as for the pivot shift examination (valgus force on an externally rotated foot) with an axial load. However, instead of starting in extension, the examiner starts in 90 degrees of flexion and brings the leg into complete extension; a palpable reduction of the tibial plateau is observed between 20 and 30 degrees of flexion. The external rotation recurvatum and posterolateral drawer tests can also serves as adjuncts to these tests, but are rarely used in isolation because of their high false-positive rate.16,17
Diagnostic Imaging
The initial evaluation of a patient with knee complaints should include plain radiography. Subtle posterior subluxation of the tibia on the femur and avulsion fractures of the tibia can be seen on plain radiographs. In trauma patients, plain radiographs are important to evaluate for osseous injury, dislocation, and other associated injuries. Stress posterior drawer radiographs and comparisons to the contralateral side are important for increasing the sensitivity when attempting to detect PCL injuries and are also helpful for measuring PCL reconstruction results. Stress radiographs are taken with the knee in 90 degrees of flexion. A side to side difference measured from the medial femoral condyle to the posterior plateau of the tibia of more than 8 mm is considered indicative of a PCL tear (Fig. 26-3).17–19 Anteroposterior (AP) films, standing AP films with the patient in 45 degrees of flexion, and a sunrise view can be helpful to detect arthritis in patients with chronic PCL injuries. Moreover, plain radiographs may be necessary in patients with claustrophobia or metallic implants that prevent the use of magnetic resonance imaging (MRI).8,10
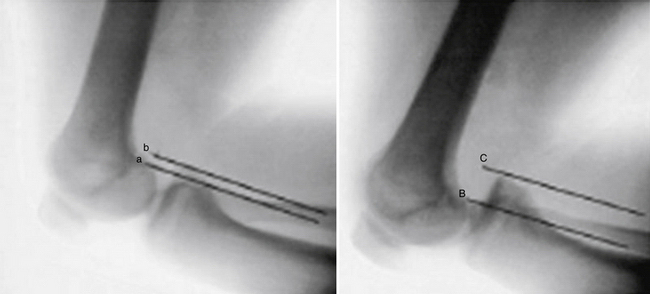
FIGURE 26-3 Stress radiographs showing normal knee (left), PCL-deficient knee (right). Translation is measured from the posterior medial femoral condyle to the posterior tibial plateau. a,; b,; B,; C,.
(From Margheritini F, Mancini L, Mauro CS, Mariani PP. Stress radiography for quantifying posterior cruciate ligament deficiency. Arthroscopy. 2003;19:706-711.)
MRI is the advanced imaging modality of choice for suspected PCL and soft tissue injuries of the knee. MRI has a sensitivity from 96% to 100% in diagnosing PCL tears. It has the added effect of being able to detect associated injuries, such as posterolateral corner injuries.9,20 There has been evidence to suggest that PCL injuries can heal and look relatively normal on MRI scans.21 MRI has also been helpful in establishing the fact that PCL injures have a decreased likelihood of meniscal tears and bone bruise patterns as compared with ACL injuries.2
Other advanced techniques such as radionuclide bone scans can be helpful in patients with chronic PCL tears. Because these patients are at increased risk of patellofemoral and medial compartment arthritis, bone scans can be helpful for the detection of early arthritis. If the history and physical examination do not directly indicate PCL reconstruction, but the bone scan demonstrates increased uptake in susceptible knee compartments, the patient may be a more suitable candidate for surgery.20,22
TREATMENT
Conservative Management
Conservative treatment is mostly reserved for patients with advanced degenerative changes of the knee and those with isolated grade I and symptomatic grade II PCL injures.11 Numerous studies have shown that up to 80% of isolated PCL injuries have good to excellent results when treated conservatively.23,24 Quadriceps strengthening and motion are the cornerstones of conservative treatment. Quadriceps strengthening helps in keeping the tibia reduced under the femur and decreases the tension on the injured PCL. Strengthening exercises include quadriceps sets, straight leg raises, and partial weight bearing in extension. These patients usually recover strength fairly quickly and are able to return to activity in 4 weeks.9 Bracing is generally ineffective in controlling PCL laxity. Because grade III injuries are often associated with other injuries, especially posterolateral corner injuries, they are largely treated surgically. If conservative treatment is elected for grade III injuries, the knee is splinted in full extension for 2 to 4 weeks.9 Children with PCL injuries often undergo similar treatment with cast immobilization in extension; however, these injuries are infrequent in this patient population.8 Failed conservative treatment usually manifests as continued knee pain rather than instability, because persistent tibial subluxation causes increased stress on the patellofemoral and medial compartments of the knee.25
Arthroscopic Technique
Operative treatment of PCL injuries are usually found in situations that include displaced avulsion injuries of the PCL, combined ligamentous injuries, and symptomatic grade II or III injuries that fail rehabilitation and in active patients unwilling to alter their lifestyle in compliance with conservative management.6 Preoperative planning includes the presence or absence of repairable meniscus tears or chondral lesions and affected limb alignment.26 In the presence of the former, operative intervention should include treatment of the associated injuries to prevent future arthrosis. In the latter case, an osteotomy may be needed to prevent failure of the reconstruction.27 Once operative treatment has been decided on, the manner in which surgery is performed is determined by the site of injury. Primary repair is indicated for fractures from the origin or insertion site; however, repair of midsubstance tears has been shown to result in poorer outcomes and is generally not recommended.12 Reconstructive methods are divided into two categories, transtibial reconstruction and tibial inlay reconstruction. Tibial inlay reconstruction has the advantage of avoiding the “killer turn,” postoperative laxity, and late graft failure seen in transtibial techniques.12
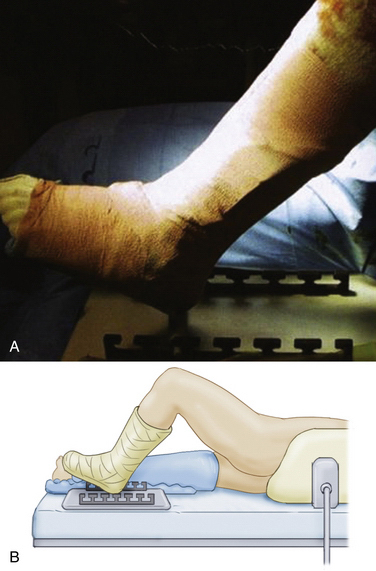
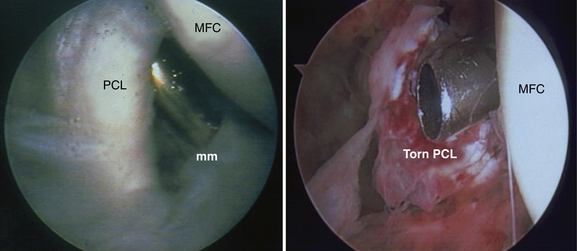
The patient is placed in the lateral decubitus position with the operative leg up and the contralateral leg, or well leg, padded in its entirety using a bed roll technique. The operative leg is placed in an ankle-foot orthosis-type leg holder (Fig. 26-4). A well-padded tourniquet is placed as far proximal as possible on the operative thigh and all extremities are padded, with particular attention paid to the axilla (axillary roll), the peroneal nerve of the contralateral leg, and the ulnar nerves. The leg is examined under anesthesia to assess for associated ligamentous laxity before prepping and draping the operative extremity. The leg is positioned for graft harvest and arthroscopy by rotating the hip and placing the foot eccentrically in the foot holder (Fig. 26-5). Standard arthroscopic portals are used for this procedure. The inferior lateral portal is the primary viewing portal and the inferior medial portal is the primary instrumentation portal. A diagnostic arthroscopy confirms the absence of the PCL from the lateral aspect of the medial femoral condyle and can determine the presence of associated injuries. Arthroscopic indicators of PCL injury include hemorrhage, decreased tension, and pseudolaxity of the ACL (Fig. 26-6). Once the PCL tear is confirmed, the surgeon proceeds with graft harvest.

FIGURE 26-4 Operative extremity in well-padded leg holder wrapped in Coban.
(From Miller MD, Harner CD, Koshiwaguchi S. Acute posterior cruciate ligament injuries. In: Fu FH, Vince KG, Harner CD, eds. Knee Surgery. Baltimore: Williams & Wilkins; 1991:749-767.)
Graft harvest begins by making a central anterior knee incision just medial to the midline from the middle of the patella down to approximately 2 cm distal to the tibial tubercle. This incision is carried down through the subcutaneous tissue until the peritenon layer is identified around the patellar tendon. The peritenon layer is incised along the entire length of the patellar tendon and saved for later closure. Once the medial and lateral borders of the patella tendon have been established from the midpatella proximally to the tibial tubercle distally, a sharp blade is used to take the central third of the patella tendon. A sagittal saw is used to take the bone plugs, measuring approximately 25 mm in length from both the tibia and patella. The sagittal saw is angled to protect the articular cartilage and prevent fracture. During graft preparation, a flat surface is made on the tibial side of the harvested graft so that it can be laid onto the tibia. This bone block must also be prepared to accept a 4.5-mm bicortical screw by drilling and tapping. The patellar portion of the graft is contoured in a cylindric fashion and the tip sculpted in a bullet shape to facilitate graft passage. The graft should be at least 18 mm long and perpendicular sutures passed into the ends to avoid suture cut-out during graft fixation (Fig. 26-7).
Preparation for acceptance of the graft can occur simultaneously as the graft itself is being prepared. The arthroscopic shaver is used to débride the lateral aspect of the medial femoral condyle (medial wall), the injured PCL, and the soft tissue in the notch. There must be a clear arthroscopic view from the anterior notch to the posterior capsule for successful graft passage. Once the soft tissue has been cleared, a commercially available PCL guide is placed approximately 6 to 8 mm from the articular surface on the anteromedial portion of the intercondylar notch at the 11 or 1 o’clock position. The guide is used to determine the incision that is made on the medial portion of the knee at the medial femoral condyle along Langer’s lines. This incision is approximately 2 cm in length and is carried down through the subcutaneous tissue until of the inferior border of the vastus medialis oblique is identified. A subvastus approach is used with electrocautery to encounter the bone of the medial condyle, with protection of the musculature at all times. Once contact is made with bone, the guide wire is placed using a drill and the correct position inside the intercondylar notch is confirmed (Fig. 26-8). The guide pin is then overdrilled with a drill bit sized appropriately for the graft. The posterior aspect of the tunnel is rasped to reduce graft abrasion. An 18-gauge guide wire or commercially available graft passer is then introduced into the femoral tunnel and the posterior aspect of the knee joint to facilitate future graft passage from the posterior incision that will be made.
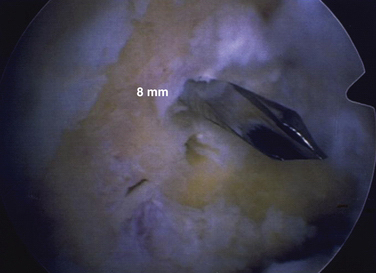
FIGURE 26-8 Placement of femoral guide pin 8 mm from the articular surface of the medial femoral condyle.
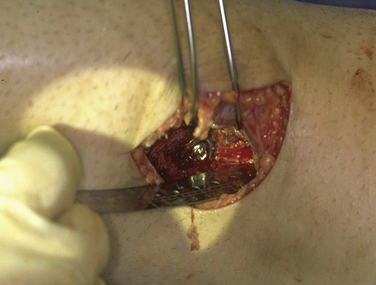
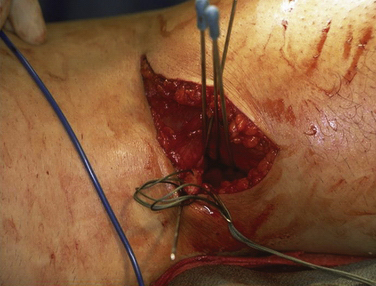
After preparing the femoral tunnel, arthroscopic instruments are removed and the leg is rotated with the hip and knee extended, allowing the patient to be fully in the lateral decubitus position (Fig. 26-9). An incision is marked for a modified posterior approach to the knee. A horizontal incision is made in the crease of the popliteal fossa. The interval between the medial head of the gastrocnemius and the semimembranosus is developed. Lateral retraction of the gastrocnemius using Steinmann pins bent laterally provides access to the posterior capsule of the knee and simultaneously protects the neurovascular structures of the popliteal fossa (Fig. 26-10). This allows for excellent visualization and exposure of the sulcus between the medial and lateral tibial plateaus posteriorly. Electrocautery can then be used to clear the soft tissue from the sulcus and to expose as laterally as possible through the window. With the use of an osteotome, burr, and tamp, a unicortical window is made at the site of the tibial insertion of the PCL to match the size of the tibial side of the graft prepared earlier. A posterior arthrotomy can then be performed sharply and carried proximally enough to ensure passage of the bone block. The arthrotomy will allow for visualization of the guide wire placed posteriorly in previous steps and a clamp is used to grasp the looped wire for passage through the posterior arthrotomy. On the preparation table, one or two guide pins are placed through the bone block of the tibia to allow for provisional fixation and assess screw length for definitive fixation. The graft, with the provisional pins, are brought to the surgical field and placed in the trough that is created. The two pins are inserted through the anterior tibial cortex and adjusted for proper length. Once the correct length has been determined, the screw sizes are measured and a cannulated drill bit is used to overdrill the guide pins; 4.5-mm cortical screws and a flat washer of appropriate length are then placed to lag the tibial bone block to the tibia (Fig. 26-11).
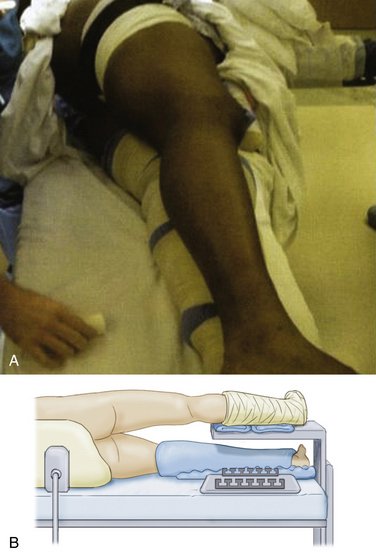
FIGURE 26-9 A, B, Lateral decubitus position in preparation for posterior approach to the knee.
(From Miller MD, Harner CD, Koshiwaguchi S. Acute posterior cruciate ligament injuries. In: Fu FH, Vince KG, Harner CD, eds. Knee Surgery. Baltimore: Williams & Wilkins; 1991:749-767.)
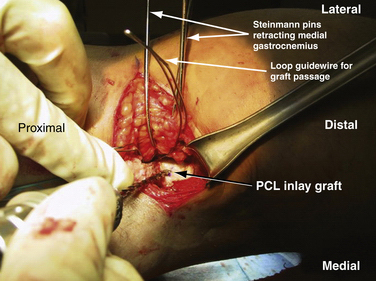
FIGURE 26-10 Steinmann pins retracting medial gastrocnemius. A looped guide wire is used for graft passage.
(From Miller MD, Cole BJ. PCL tibial inlay and posterolateral corner reconstruction. In: Gill SS, Cohen SB, Miller MD, eds. Philadelphia: WB Saunders; 2004:.)
The patellar end of the tendon graft is then pulled through the posterior arthrotomy into the joint and up into the femoral tunnel using the prepositioned looped guide wire (Fig. 26-12). This maneuver can be done in two steps, if needed. First, the graft is passed into the notch by passing the sutures from the bony end of the graft through the anteromedial portal. Second, another loop is passed from the femoral tunnel out of the same portal and is used to the pull the bone plug into the femoral tunnel. Once the bone block on the patellar side is in the femoral tunnel, the location of the bone plug tendon junction is evaluated. The junction should be at the articular margin of the femoral tunnel. Once the position of the bone plug in the femoral tunnel is complete, a maximum amount of tension is applied (knee angle) to the sutures on the femoral side and an anterior drawer force is applied while a 9- × 20-mm metal interference screw is fully seated into the femoral tunnel. Once the interference screw is placed, a posterior drawer test confirms that PCL stability has been restored.
The bone graft, which is saved during graft preparation and femoral tunnel drilling, is packed into the patella and the tibial tubercle if enough remains. Wounds are closed in layered fashion, with care taken to irrigate all wounds copiously, especially the posterior arthrotomy. Radiographs should be taken before the patient exits the operating room to ensure that the graft and hardware placement are appropriate (Fig. 26-13). The knee is braced in extension after the dressing is placed. Bracing should support the posterior tibia to prevent posterior translation.
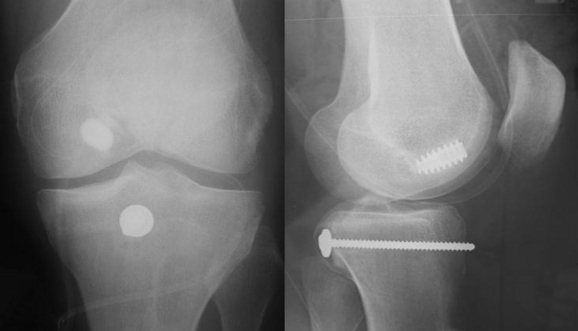
FIGURE 26-13 Postoperative AP (left) and lateral (right) views of tibial inlay fixation.
(From Miller MD, Harner CD, Koshiwaguchi S. Acute posterior cruciate ligament injuries. In: Fu FH, Vince KG, Harner CD, eds. Knee Surgery. Baltimore: Williams & Wilkins; 1991:749-767.)
PEARLS& PITFALLS
PEARLS
PITFALLS
Postoperative Rehabilitation
The patient may begin jogging on a treadmill at 3 months postoperatively, with lateral movements, stepping, shuffling, and hopping supervised by a physical therapist or athletic training. At 14 to 16 weeks, sport-specific activities and plyometrics are initiated under supervision. Plyometrics focused on low-intensity vertical and lateral hopping begins with both feet, with transition to one foot as soon as possible. The volume for plyometric exercises is adjusted based on the intensity of the exercise and is focused on strengthening, not conditioning. Beginning at 4 months, progression of therapy proceeds with running and sport-specific drills. Strength and power development are emphasized and isokinetic tests for quadriceps strength differences and unilateral hamstring-to-quadriceps strength ratio are performed. The goal for quadriceps strength differences and unilateral hamstring-to-quadriceps strength ratio is less than 15 % and 65 % or better, respectively. The patient is tested monthly until isokinetic tests are passed and then functional testing begins if the person is to return to advanced recreational activities or sports.
Complications
The most common complication following PCL reconstruction is the return of objective posterior laxity on physical examination.12,28 Also, acute PCL reconstruction in the setting of multiligamentous knee reconstruction or repair can result in arthrofibrosis and extensive scarring. Other complications include anterior knee pain, infection, heterotopic ossification, and painful hardware.29 Recent studies have shown that the use of bioabsorbable screws can decrease the effects of painful hardware and eliminate future hardware removal.30 There have also been reports of avascular necrosis of the medial femoral condyle. Therefore, tunnel placement should be proximal to the articular margin.
CONCLUSIONS
There continues to be an evolution of knowledge regarding posterior cruciate ligament injuries and their treatment. A thorough understanding of the anatomy of the PCL is critical to understanding its function when planning for proper treatment. It is well known that the PCL consists of an anterolateral bundle and a posteromedial bundle and interest has increased regarding double-bundle PCL reconstruction and all-arthroscopic inlay techniques.31 However, double-bundle PCL reconstruction has been shown to be comparable to single-bundle PCL reconstruction in providing posterior stability for knees with an intact posterolateral corner.32 The history and physical examination allow the surgeon to assess the most appropriate diagnostic tests and provide information on chronicity and severity of injury. When diagnostic tests confirm PCL disruption, the degree of laxity and associated injuries will aid in the decision to undergo surgery. Once the decision to proceed with intervention is made, preoperative planning is important to ensure a successful operation and postoperative rehabilitation. The tibial inlay technique described attempts to re-create the anatomy of the PCL and restore its biomechanical function while decreasing the intraoperative complications observed in alternative techniques. Whether conservative or surgical treatment is chosen, the key to a functional recovery after PCL injury is strong quadriceps musculature and a competent extensor mechanism. Information regarding PCL injuries continues to evolve and, as studies focusing on the multitude of factors that affect outcome improve, more standardized treatment algorithms will arise.
1. Fanelli GC, Edson CJ. Posterior cruciate ligament injuries in trauma patients: part II. Arthroscopy. 1995;11:526-529.
2. Shelbourne KD, Davis TJ, Patel DV. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries. A prospective study. Am J Sports Med. 1999;27:276-283.
3. Covey CD, Sapega AA. Injuries of the posterior cruciate ligament. J Bone Joint Surg Am. 1993;75:1376-1386.
4. Noyes FR, Stowers SF, Grood ES, et al. Posterior subluxations of the medial and lateral tibiofemoral compartments. An in vitro ligament sectioning study in cadaveric knees. Am J Sports Med. 1993;21:407-414.
5. •••. The posterior cruciate ligament. In: DeLee JC, Drez D, Miller MD, editors. DeLee & Drez’s Orthopaedic Sports Medicine: Principles and Practice. 2nd ed. Philadelphia: WB Saunders; 1994:1374-1400.
6. Miller MD, Harner CD, Koshiwaguchi S. Acute posterior cruciate ligament injuries. In: Fu FH, Vince KG, Harner CD, editors. Knee Surgery. Baltimore: Williams & Wilkins; 1991:749-767.
7. Miller RH, Azar FM. Knee injuries. In: Canale ST, Beaty JH, editors. Campbell’s Operative Orthopaedics. Philadelphia: Elsevier, 2008.
8. Cosgarea AJ, Jay PR. Posterior cruciate ligament injuries: evaluation and management. J Am Acad Orthop Surg. 2001;9:297-307.
9. Harner CD, Hoher J. Evaluation and treatment of posterior cruciate ligament injuries. Am J Sports Med. 1998;26:471-482.
10. Skinner HB. Current diagnosis and treatment in orthopedics. In: Knee Injuries. New York: Lange Medical Books/McGraw-Hill; 2003.
11. Miller MD, Cole BJ. PCL tibial inlay and posterolateral corner reconstruction. Gill SS, Cohen SB, Miller MD, eds. Philadelphia: WB Saunders; 2004.
12. Miller MD, Bergfeld JA, Fowler PJ, et al. The posterior cruciate ligament injured knee: principles of evaluation and treatment. Instr Course Lect. 1999;48:199-207.
13. Clancy WGJr, Shelbourne KD, Zoellner GB, et al. Treatment of knee joint instability secondary to rupture of the posterior cruciate ligament. Report of a new procedure. J Bone Joint Surg Am. 1983;65:310-322.
14. Daniel DM, Stone ML, Barnett P, Sachs R. Use of the quadriceps active test to diagnose posterior cruciate-ligament disruption and measure posterior laxity of the knee. J Bone Joint Surg Am. 1988;70:386-391.
15. Jakob R, Warne, J. Lateral and posterolateral rotatory instability of the knee. In: Jakob RP, Staubli H, editors. The Knee and the Cruciate Ligaments: Anatomy, Biomechanics, Clinical Aspects, Reconstruction, Complications, and Rehabilitation. New York: Springer; 1992:463-494.
16. Cooper DE. Tests for posterolateral instability of the knee in normal subjects. Results of examination under anesthesia. J Bone Joint Surg Am. 1991;73:30-36.
17. Hughston JC, Norwood LAJr. The posterolateral drawer test and external rotational recurvatum test for posterolateral rotatory instability of the knee. Clin Orthop Relat Res. 1980;(147):82-87.
18. Hewett TE, Noyes FR, Lee MD. Diagnosis of complete and partial posterior cruciate ligament ruptures. Stress radiography compared with KT-1000 arthrometer and posterior drawer testing. Am J Sports Med. 1997;25:648-655.
19. Margheritini F, Mancini L, Mauro CS, Mariani PP. Stress radiography for quantifying posterior cruciate ligament deficiency. Arthroscopy. 2003;19:706-711.
20. Fanelli GC, Giannotti BF, Edson CJ. Arthroscopically assisted combined posterior cruciate ligament/posterior lateral complex reconstruction. Arthroscopy. 1996;12:521-530.
21. Shelbourne KD, Jennings RW, Vahey TN. Magnetic resonance imaging of posterior cruciate ligament injuries: assessment of healing. Am J Knee Surg. 1999;12:209-213.
22. Petrie RS, Harner CD. Evaluation and management of the posterior cruciate injured knee. Oper Tech Sports Med. 1999;7:93-103.
23. Tietjens BR. Posterior cruciate ligament injuries. J Bone Joint Surg Br. 1985;67:674.
24. Parolie JM, Bergfeld JA. Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am J Sports Med. 1986;14:35-38.
25. Torg JS, Barton TM, Pavlov H, Stine R. Natural history of the posterior cruciate ligament-deficient knee. Clin Orthop Relat Res. 1989;(246):208-216.
26. Shino K, Horibe S, Nakata K, et al. Conservative treatment of isolated injuries to the posterior cruciate ligament in athletes. J Bone Joint Surg Br. 1995;77:895-900.
27. Noyes FR, Roberts CS. High tibial osteotomy in knees with associated chronic ligament deficiencies. In: Jackson DW, editor. Reconstructive Knee Surgery. New York: Raven Press; 1995:185-210.
28. Miller MD, Olszewski AD. Posterior cruciate ligament injuries. New treatment options. Am J Knee Surg. 1995;8:145-154.
29. Jung YB, Lee YS, Jung HJ. Heterotopic bone formation after posterior cruciate ligament reconstruction using inlay method and posterolateral corner sling with tibia tunnel: report of one case. Knee Surg Sports Traumatol Arthrosc. 2007;15:729-732.
30. Gupta A, Lattermann C, Busam M, et al. Biomechanical evaluation of bioabsorbable versus metallic screws for posterior cruciate ligament inlay graft fixation: a comparative study. Am J Sports Med. 2009;37:748-753.
31. Campbell RB, Jordan SS, Sekiya JK. Arthroscopic tibial inlay for posterior cruciate ligament reconstruction. Arthroscopy. 2007;23:1356.
32. Whiddon DR, Zehms CT, Miller MD, et al. Double compared with single-bundle open inlay posterior cruciate ligament reconstruction in a cadaver model. J Bone Joint Surg Am. 2008;90:1820-1829.



 -inch pins that are drilled from posterior to anterior and bent over as retractors.
-inch pins that are drilled from posterior to anterior and bent over as retractors.