CHAPTER 34 Injury of the Flexors of the Elbow: Biceps Tendon Injury
INTRODUCTION
Except for epicondylitis, injury to the muscles or tendons about the elbow, as an isolated event, is rather uncommon.3,13,16,30,70 Distal biceps tendon injury, usually avulsion from the radial tuberosity, is the most common tendinous injury in this region, and the incidence seems to be increasing. Calcific tendinitis has been observed in the biceps tendon, but it is very uncommon.58
DISTAL BICEPS TENDON INJURY
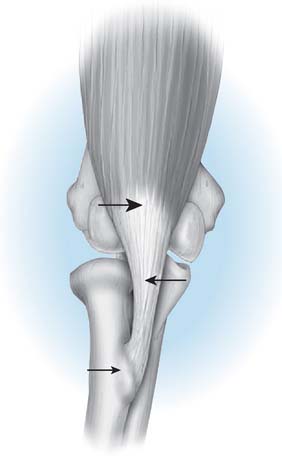
The biceps muscle-tendon complex may be injured at the musculotendinous junction by an incontinuity tear of the tendon and by a complete or partial tear or avulsion from the radial tuberosity (Fig. 34-1).
MUSCULOTENDINOUS JUNCTION
This is an uncommon injury and one rarely reported.68 The mechanism is similar for all biceps injuries—an eccentric load against a contracting biceps muscle. It may have a predilection for persons with encephalopathy, a condition present in many who experience triceps rupture.
AVULSION
By far, the most common injury is tendon avulsion, and complete avulsion is much more common than a partial injury. According to McReynolds,54 the first known diagnosis of a distal rupture was reported by Starks in 1843.
INCIDENCE
Avulsion of the biceps tendon at its distal insertion was reported in three of 100 patients with biceps tendon rupture who were studied by Gilcreest.25 The European literature suggests that distal avulsion injury accounts for approximately 3% to 10% of all biceps tendon ruptures.35 Only 24 cases were reported in a 43-year period after the original surgical descriptions by Johnson40 in 1897 and Acquaviva1 in 1898. Three hundred and fifty-five surgeons responded to a questionnaire Dobbie circulated in 1941, and only 51 cases were added.21 In addition, only three of this group had experience with as many as three cases. By 1956, the world literature contained 152 cases.27 At present, the injury is well known; either the incidence may be increasing or the lesion is recognized more often.*
More reports in the literature notwithstanding, we have encountered only two instances of involvement in a woman in the English literature.54 In addition, more than 80% of the reported cases have involved the right dominant upper extremity, usually in a well-developed man9,62 whose average age is about 50 years5,21,57 (range 2163 to 7021 years).
MECHANISM OF INJURY
In virtually every reported case,8,21,57 a single traumatic insult, often a force of 40 kg or more against resistance from an elbow in about 90 degrees of flexion, has been implicated. This mechanism, along with abuse of anabolic steroids, accounts for its surprisingly common occurrence in well-conditioned, healthy, but competitive weightlifters. Pre-existing degenerative changes in the tendon predispose to rupture.18,19 Acute pain in the antecubital fossa is noted immediately. Rarely, a patient complains of a second episode of acute pain several days later. Such a history suggests the possibility of an initial partial rupture or of secondary failure of the lacertus fibrosus.11,14 Occasionally, forearm pain has been reported, but it is considered rather uncommon.
ETIOLOGY
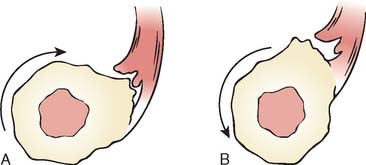
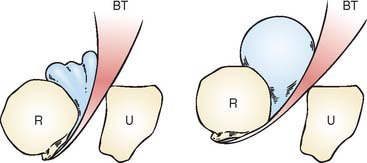
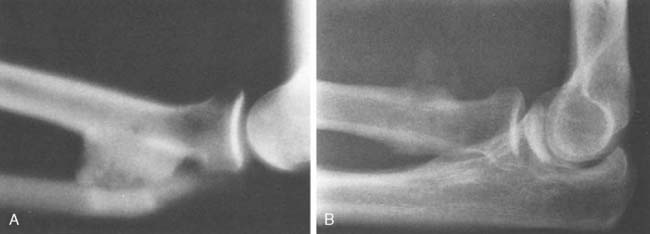
The cause of the injury has been discussed by several authors and is considered in detail by Davis and Yassine.18 The histologic pathology is that of a degenerative process, a finding consistent with the radiographic changes of spurring sometimes observed at the radial tuberosity (Fig. 34-2).21,37,62 During pronation and supination, inflammation and subsequent attenuation of the biceps tendon is initiated by irritation from the irregularity of the radial tuberosity (Fig. 34-3) or from chronic cubital bursitis (Fig. 34-4).42 Predisposition to this and other tendon injuries has been associated with anabolic steroid use,51 hyperparathyroidism,15,63 chronic acidosis,59 and systemic diseases such as lupus erythematosus.71 One study has also implicated a hypovascular zone of tendon near its attachment as a cause or contributing factor to the injury.66
More recent studies of the “footprint” and function of the biceps tendon insertion have revealed additional insight into the insertion pattern (Fig. 34-5). The portion oriented more distally is along the line of the short head tendon; the long head portion inserts further from the axis of rotation (see Fig. 34-5).22
PRESENTATION
Subjective Complaints
The common symptom of distal biceps tendon rupture is a sudden, sharp, tearing-type pain, followed by discomfort in the antecubital fossa or in the lower anterior aspect of the brachium. The intense pain usually subsides in several hours, but a dull ache persists for weeks. Immediately after the injury, activity is possible but difficult. If surgical repair is not performed, chronic pain with activity is common.38 Flexion weakness of about 15 percent inevitably develops but over time some flexion strength returns.46 Loss of supination strength has been reported as the source of variable dysfunction but has been measured as averaging 40 percent,57 and diminution of grip strength also has been recognized.2,46,57
Objective Complaints
Ecchymosis is variably present in the antecubital fossa,21,61 and occasionally over the proximal ulnar aspect of the elbow joint.8 Extensive bleeding is uncommon but is seen occasionally (Fig. 34-6). With elbow flexion, the muscle contracts proximally and a visible, palpable defect of the distal biceps muscle is obvious (Fig. 34-7). If the contour is relatively normal, the lacertus fibrosus may be intact or the lesion may be a partial tear. With time, stretch of the lacertus fibrosus14 may occur. Assessment of strength alteration is essential to substantiate the diagnosis. Local tenderness is present in the antecubital fossa. The defect may be palpable; if it is not and if symptoms are otherwise consistent with the diagnosis, a partial rupture may have occurred. With partial rupture, an intense peritendinosis or bursitis may develop and crepitus or grinding is noted with forearm rotation.11 Motion is not altered, except possibly as a result of pain at the extremes of flexion, extension, and supination. Flexion weakness usually is detectable by routine clinical examination. The loss of strength may be profound,21 especially on supination immediately after injury. Loss of grip strength is variable in degree but does occur with most injuries.
Imaging of the Distal Biceps Tendon
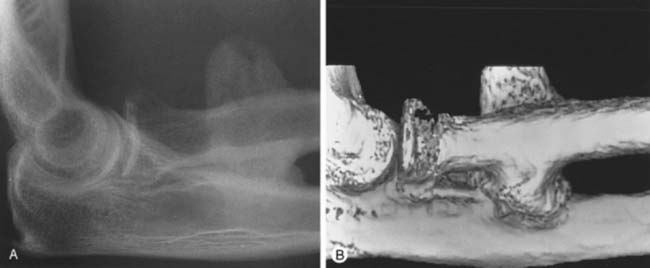
Plain x-ray study is usually normal; however, spurring of the bicipital tuberosity is sometimes seen as being suggestive of a chronic tendon enesiopathy. Magnetic resonance imaging is commonly used to make or to confirm the diagnosis,47 especially when the lacertus fibrosus is intact and the typical retraction deformity is not present or when trying to differentiate complete tears from partial tears. The treatment of complete tears without retraction or partial tears can benefit from precise delineation of the extent of the pathology. Guiffre and Moss26 have described the Flexion Abduction Supination (FABS) view. With the elbow flexed and forearm supinated, the radial tuberosity is directed medially and the distal biceps tendon is almost a direct line from the tuberosity to the muscle belly (Fig. 34-8), allowing a longitudinal view to include the muscle belly, tendon, and the difficult-to-assess bicipital tuberosity insertion (Fig. 34-9). Because the tendon is assessed longitudinally and is at full length and partially unravelled, the differentiation of partial from complete tears is made easier (Fig. 34-10). In addition, the elbow is near the center of the magnet and, thus, fat suppression is optimal, enhancing visualization of small amounts of fluid. Continuing technical advances allow visual reconstruction and enhancements (see Fig. 34-10B).
Surgical Findings
If the biceps tendon is explored early, local hemorrhage is present in the antecubital space but usually is not extensive. The tendon may have recoiled into the muscle or may lie loosely curled in the antecubital fossa. Invariably, the separation is clean and from the radial tuberosity,8,21,46,52,57,61 with a bulbous stump of degenerative tendon. This supports our histologic studies and the hypothesis that the underlying lesion is degeneration at the site of attachment.14,18 After several months, typically the tendon has retracted into the substance of the biceps muscle and cannot be retrieved to be reattached. However, this response as well as the status of the lacertus fibrosus is variable.
TREATMENT
Acute Disruption
Reliance on the older literature is unwise. Nonoperative management has been reported to provide satisfactoryresults37; however, the functional superiority of surgical treatment is obvious when the results of cases treated with and without surgical intervention are reviewed.57 The recent literature offers overwhelming documentation of the excellent results of early repair.2,6,50,60 Although tendon strains will heal, true partial rupture does not and chronic pain necessitates surgical repair.
Surgical Repair
Reattachment to the radius by any one of several techniques5,9,24,59,69 is clearly the treatment of choice. The difficulty of performing the anterior exposure needed to avoid radial nerve injury has inspired the development of a second incision that is placed over the dorsal aspect of the forearm.12 Curiously, this technique appears first to have been employed in 1937 by Plummer to reattach the biceps tendon to the proximal ulna.21 It is paramount to understand that the two-incision Boyd-Anderson technique originally described has been modified at the Mayo Clinic to reduce the likelihood of the development of ectopic bone between the radius and ulna. This point is explained later.
Because of concern over the development of ectopic bone associated with the two-incision technique, and with the advent of suture anchors, the anterior exposure using these anchors is gaining popularity. If the procedure is performed promptly, the tract of the biceps tendon is still present and is easily identified. Later (more than 2 weeks after injury), the tract may be obliterated, making the exposure more difficult36 and complications more frequent.44
SURGICAL TECHNIQUE
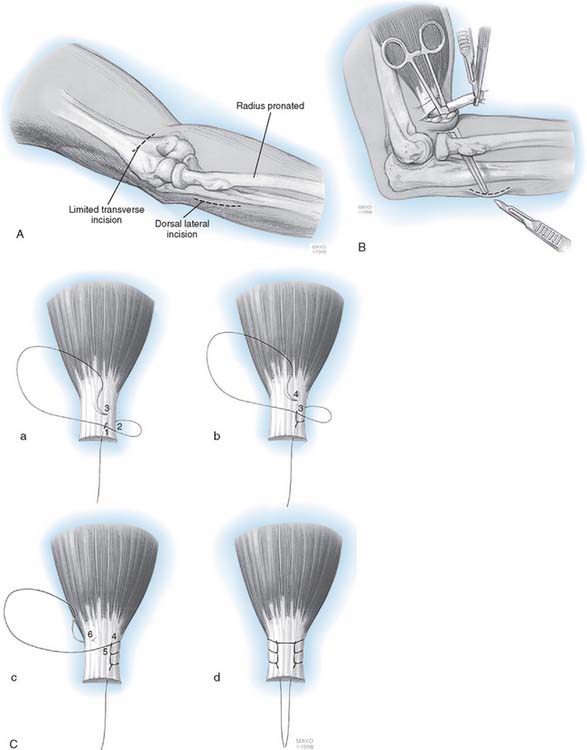
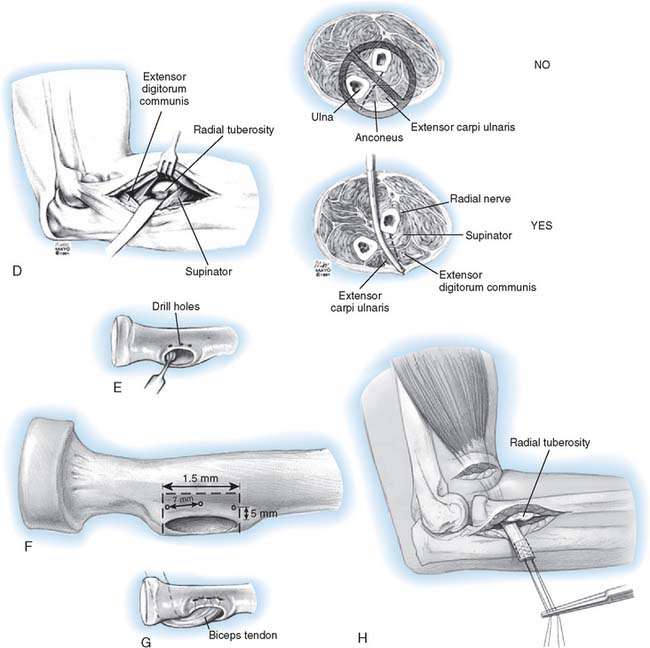
Two-Incision Technique (Mayo)
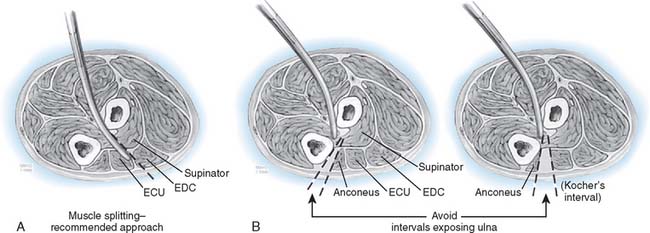
This technique has been described in detail elsewhere.56 With the patient in the supine position, a tourniquet is applied to the arm and the extremity is prepared, draped, and placed on an elbow table. A limited 3-cm transverse incision is made in the cubital crease (Fig. 34-11). The brachium is grasped and milked distally to deliver the biceps tendon. In the majority of cases, the tendon is readily retrieved with this maneuver. The tendon is inspected and invariably is found to be cleanly avulsed from the radial tuberosity. The distal 5 to 7 mm of degenerative tendon is resected, and two No. 5 nonabsorbable Bunnell or whipstitch (Krackow) sutures are placed in the torn tendon for a distance of at least 3 cm (see Fig. 34-11). The tuberosity is palpated with the indexfingers, and a blunt, curved hemostat is carefully inserted into the space previously occupied by the biceps tendon. The instrument slips past the tuberosity and is advanced below so its tip may be palpated on the dorsal aspect of the proximal forearm (see Fig. 34-11). A second incision is made over the instrument. The tuberosity is exposed by a muscle-splitting incision, with the forearm maximally pronated.
Note: The ulna is never exposed.24 A high-speed burr is used to evacuate a defect 1.5 cm wide and 1 cm deep in the radial tuberosity (see Fig. 34-11). Three holes are then placed 7 to 8 mm apart and at least 5 mm from the edge of the excavation. The tendon is delivered through the second incision, and No. 5 sutures are brought through the holes in the tuberosity. The tendon is carefully introduced into the excavation formed in the tuberosity, and with the forearm in the neutral position, the sutures are pulled tight and secured. The wounds are closed in layers, and a suction drain is inserted in the depths of the wound, both anteriorly and posteriorly. The elbow is placed in 90 degrees of flexion with the forearm placed in 45 degrees of supination. A compressive dressing is applied.
Single-Incision Technique
In the acute presentation the residual tendon sheath is usually composed of inflammatory bursa filled with haemoserous fluid.4 This is easily followed down onto the bicipital tuberosity by fully supinating the forearm to orientate the tuberosity volarwise. In the chronic case, the sheath may be scarred and obliterated.36,44 If this is the case, then the anterior aspect of the brachialis muscle is followed distally, between the common flexor and common extensor muscles.
If the tear is acute, then the tendon stump may be milked into the surgical field, as described earlier. If the tear is a few weeks old, formal dissection may be required because the tendon often recoils and lies in a phlegmonous stump, possibly even tethered to the median or the lateral antebrachial cutaneous nerve. The distal 5 to 7 mm of degenerative tendon is resected. Generally, the lacertus fibrosis is left intact to maintain its function to the transfer flexion forces to the ulna. If there is a marked retraction of the biceps tendon and a tight repair is required, then release and reapposition should be considered as a potential median nerve entrapment has been postulated.4
Tendon Fixation
A number of different means of tendon fixation to the bicipital tuberosity have been described either using various suture anchors7 or an endobutton.4
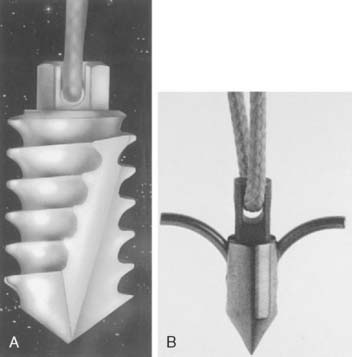
Suture Anchor
The precise technique depends on three variables: exposure, type of anchor used, and method of reattachment. Usually a limited anterior approach is employed. The use of both the screw and the barb designs has been described (Fig. 34-12). Typically, two or three suture anchors are used, most often placed directly into the tuberosity, which has been dèbrided but not decorticated. One technique places a hole the diameter of the tendon stump in the bicipital tuberosity, and the anchors are placed proximal and distal on either side of the biceps tuberosity. The tendon suture is placed approximately 1 cm distal to the end of the tendon stump and the suture tensioned on the anchors, thus allowing apposition of the tendon stump into the radius.53 Greenberg and associates29 compared fixation strength with the endobutton and traditional techniques. A mean pullout strength of 253 N for the Mitek G4 Superanchor (barb design), 177 N for a conventional bone grid, and 584 N for the titanium endobutton. The button was three times stronger than the bone bridge (P > .0001) and two times stronger than the Mitek anchor (P > .0007). Note that 19-gauge wire was used to exclude suture properties. Other studies,67 however, have not demonstrated any real differences between barbed anchors and endobutton with No. 2 reinforced polyester suture (Fiberwire; Arthrex Corp., Naples, FL) and cyclic loading. The endobutton did reveal a nonsignificant 16% greater ultimate tensile load to failure than did the suture anchor group (274.77 N versus 230.06 N).
Endobutton Technique
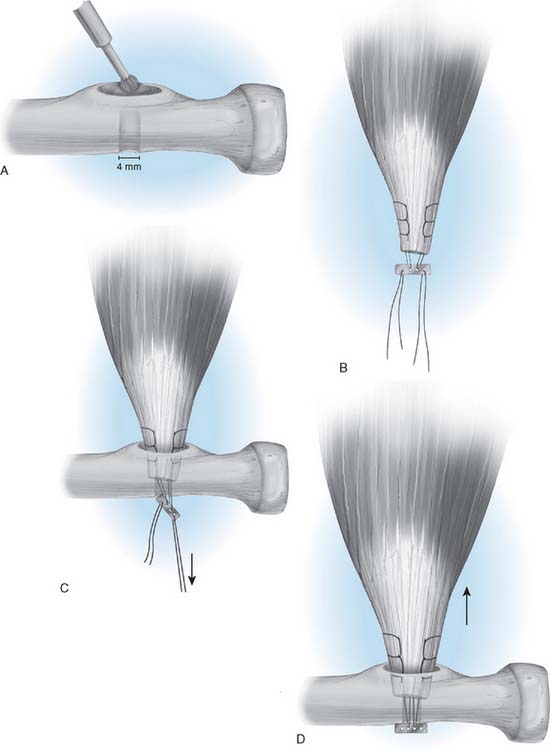
The endobutton (Acufex; Smith & Nephew, Inc., Andover, MA) technique was first described by Bain and colleagues4 for both primary repair and late reconstruction with a semitendinosis tendon. The advantage of this technique is that the biceps tendon fixation construct is prepared outside the wound (Fig. 34-13A) rather than down a deep tunnel, and the construct is the strongest available to date.29
The cortical window is achieved by drilling a 2-mm guidewire into the bicipital tuberosity and just penetrating the far cortex of the radius (all drilling is undertaken with a tissue guard to protect the soft tissues). Using a 6-mm drill, only the radial tuberosity cortex is drilled (not the far cortex). The drill is then lifted on the guidewire, tilted proximally and drilled, lifted and tilted distally and drilled, resulting in an elliptical cortical window. Using the same guidewire, the far cortex of the radius is drilled with 4.5-mm drill to allow passage of the endobutton through the far cortex (see Fig. 34-13B).
The degenerated tendon is dèbrided to healthy tissue and using a nonabsorbable suture (No. 5 ethibond [Ethican Inc., Sommerville, MA] or No. 2 Fiberwire [Arthrex Corp., Naples, FL]), a Bunnell or “whip” stitch is placed in both the medial and lateral margins of the tendon (see Fig. 34-13A). A gap of 2 mm is left between the tendon end and endobutton to allow it to be passed through the dorsal cortex of the radius and to flip in place. Two strong sutures, which can be differentiated from each other, are placed in the leading and trailing holes of the endobutton. These sutures are threaded onto a long-eyed needle. The forearm is maximally supinated and the elbow held flexed to bring the forearm to the tendon in a straight line. The needle is passed through the bicipital cortical window, through the dorsal cortex and out through the extensor compartment and skin. The needle is directed in an ulna direction (but should not touch the ulna) to avoid injury to the posterior interosseous nerve. The leading suture is tractioned to deliver the endobutton through the radius and then the trailing suture is tensioned to flip the endobutton and lock it on the dorsal surface of the radius (see Fig. 34-13C). Intraoperative confirmation of a locked button should be done in all cases (usually with fluoroscopy), because it can appear locked when it is only partially passed through the volar cortical window (see Fig. 34-13D).
RESULTS
Two-Incision Technique
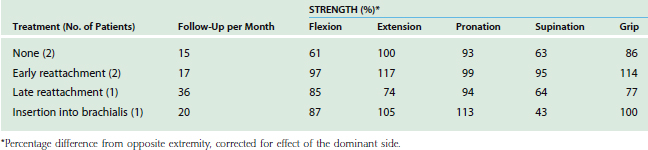
Today, few surgeons attach the acutely ruptured tendon to the brachialis, but in the past, this maneuver has been said to produce full function of the forearm,13,45 including adequate supination.10,62 Restoration of normal or nearly normal supination strength without anatomic reinsertion of the biceps tendon is incomprehensible. The result may be surprisingly good, but it is not normal and cannot restore supination strength. We have conducted isometric strength assessment tests on seven patients at least 15 months after the two-incision technique.57 Restoration of strength approached normal in flexion and supination (Table 34-1). Nontreated distal biceps rupture results in loss of about 20% flexion and 40% supination strength.57,65
The objective measurements of restoration of normal strength have been reaffirmed with the use of Cybex testing for strength but also endurance.2 Interestingly, these investigators found restoration of normal strength only if the dominant extremity was involved, and a residual 20% to 30% weakness if the nondominant side was involved. Although this observation of different results by the dominant extremity has also been made by others,48 this certainly has not been our experience with isometric testing.
Suture Anchors
Barbed suture anchors for distal biceps repair were first reported in 1993.7 In one study, using a single limited incision and two barbed suture anchors, 53 patients were evaluated at a mean follow-up of 38.1 months. Using the Andrews-Carson scores, there were 46 excellent and seven good results. Two patients developed ectopic ossification associated with mild loss of forearm rotation and mild arm pain. One patient developed a temporary radial nerve palsy, which resolved completely within 8 weeks.39
Endobutton Technique
Bain and coworkers4 first reported on 12 patients with endobutton repair. Motion averaged 5 to 146 degrees and 81 degrees supination and 80 degrees pronation. All returned to previous activities and had a grade 5 strength. There was no synostosis, reruptures, or neurologic complications. A subsequent study of 14 patients who had tendons repaired with the endobutton technique revealed recovery of 97% of flexion strength and 82% of supination strength. Patients were able to participate in an aggressive postoperative rehabilitation program and were able to regain strength and function rapidly, with satisfactory return to preinjury activities and occupations.29
COMPLICATIONS
As a result of consistent reports of ectopic ossification and neurologic injury associated with distal biceps repair, interest has centered on the surgical exposure and means of fixation as potential factors influencing complications. Only one report in the English literature from the Mayo Clinic specifically deals with the complications of surgical treatment for distal biceps tendon rupture.44 This experience reported 74 tendon repairs using the Mayo modified Boyd-Anderson approach stratified by acute (<10 days), subacute (10-21 days) and chronic (>21 days) repairs. The association between the incidence of complications and the delay to surgery was highly significant. Repairs performed less than 10 days from injury incurred complications in 24% of patients, 10 to 21 days in 38% of patients and greater than 21 days in 41% of patients. This probably represents the greater dissection that is required to identify and reattach the tendon. Eighty-six percent of patients who had a repair at less than 10 days and only 53% in the 10-to-21-day group had a patent tunnel at surgery. Most complications were mild including sensory paresthesias (5), temporary posterior interosseous nerve palsy (1), and persistent pain (6). Heterotopic ossification was observed in four but there were no synostosis.
Transient sensory paresthesias especially of the lateral antebrachial cutaneous nerve, are relatively common. This nerve is at risk proximally as it passes from behind the lateral border of the biceps tendon. Distally, it passes deep to the median cephalic vein, where it may be inadvertently divided or ligated with the vein. In very tight repairs, there may be entrapment of the lateral antebrachial nerve as it passes from behind the tendon. If symptoms occur, then a slower restoration of extension may be indicated. Similarly, the median nerve may be trapped if the tendon is advanced excessively while leaving the lacertus fibrosus intact.4 If this is the case, then consideration to release the lacertus may be indicated.
Transient radial or posterior interosseous nerve palsy with reattachment to the tuberosity has been,21,55 and continues to be, noted occasionally.50,60 The lesions have still been seen with both single and double incision exposures. The mechanism of injury is thought to be due to retraction, possibly with the use of bone levers over the lateral border of the radial neck where the nerve lies on the bone and where it can be compressed or stretched by retractors. Long retractors may minimize this risk. Nonanatomic routing of the tendon in relation to the median, radial, and lateral antebrachial cutaneous nerve can result in persistent postoperative palsies.43 Most palsies are temporary.39,44
Reattachment of the tendon through an anterior approach with a pullout suture has received support50,60 but potentially has skin and wound problems. In two recent series of 24 cases in all, this approach produced excellent restoration of function but also one musculocutaneous nerve injury and two temporary radial nerve palsies, complications that are clearly associated with an anterior surgical approach for this condition.
The possibility of ectopic bone formation is well known. The formation of ectopic bone has been reported with both single- and double-incision (Fig. 34-14) exposures, and may be associated with pain but generally does not cause a significant restriction of rotation, as noted earlier. Bridging synostosis is most commonly associated with the Boyd-Anderson two-incision technique. The development of proximal radioulnar synostosis is thought to be associated with exposing the periosteum of the lateral ulna, and in our opinion, it can be avoided, or at least minimized, with a muscle-splitting incision (Fig. 34-15).24 The role of nonsteroidal anti-inflammatory drugs to prevent ectopic ossification has not been established one way or the other.
If an osseous bridge does develop, successful resection can be undertaken about 8 to 9 months after the initial surgery (Fig. 34-16).23 In some cases, extensive involvement of the interosseous space compromises the site of attachment (Fig. 34-17). Removing the osseous bar may thus result in detachment of the biceps tendon, which then must be reattached into the tuberosity (Fig. 34-18). A good result may be anticipated, but rehabilitation must begin anew. If a bridge is excised, irradiation (700 cGy) may be administered, but in my practice, there has been little tendency for recurrence of the ectopic bone. If the surface area of resection is large and recurrence is a concern, a vascularized interposition adipofascial interposition graft may be a useful adjunct to prevent recurrence.41 Recurrence of the avulsion is rarely reported and usually is associated with patient (inappropriate early or abnormal use) or surgeon factors (poor positioning of bone bridges). One of us (BFM) has had one such case in a paralytic man who uses his arms for transfer and local motion sustained a recurrent avulsion less than 1 month after repair. A revision was successfully performed.
AUGMENTATION PROCEDURES
Sometimes, after careful discussion with the patient, improved supination strength is found to be required. Chronic pain, due to tethering of neurovascular structures or cramping of a chronically retracted biceps muscles, is an indication for intervention. In chronic tears, a graft is usually necessary to restore muscle tendon length. Autologous grafts described include hamstring tendon (semitendinosus),34 fascia lata,37 palmaris longus,64 flexor carpi radialis,49 and Achilles tendon allograft.65
Hallam and Bain31 reported the results of anatomic repair for chronic distal biceps tendon ruptures by use of a semitendinosus autograft with the endobutton. All nine patients were satisfied with their outcome and were able to return to their jobs. The mean pain score was 0.5, and the postoperative flexion arc was from3 degrees to 147 degrees, with supination to 75 degrees and pronation to 62 degrees. The mean Mayo Clinic Elbow score was 96.3 (range, 85 to 100). Wiley72 reported results with delayed semitendinosus reconstruction compared with nonoperative management. Superior results were documented in the delayed reconstruction group. The autograft reconstruction group was employed with a two-incision technique, and flexion and supination strength were restored to the normal range. The nonoperative group lacked 20% of normal strength. Endurance in both groups was within the normal range. No radial nerve injuries or heterotopic ossification occurred, and all reconstructions remain intact.
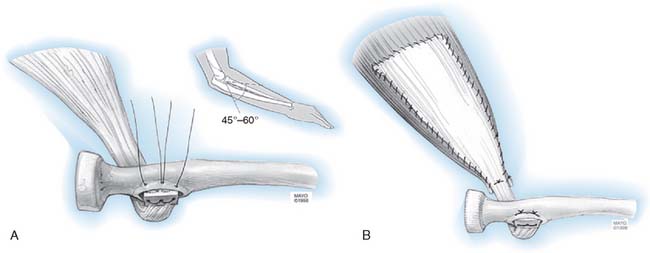
At the Mayo Clinic, we favor an autologous Achilles tendon graft (Fig. 34-19). This is a very satisfying tissue and one ideally suited to this reconstruction. The fleck of calcaneus bone may be trimmed and embedded into the excavated radial tuberosity. Then, with the elbow flexed to 45 to 60 degrees, the Achilles fascia is draped over the biceps muscle and the bone tendon stump is sewn into the muscle. This offers a very gratifying reconstruction that allows more aggressive rehabilitation.
PARTIAL (INCOMPLETE) DISTAL BICEPS RUPTURE
In a study conducted by Karanjia and Stiles,42 one of the two patients with cubital bursitis was found at surgery to have distal biceps tendon degeneration in association with the bursitis. I (BFM) have observed this finding in one female patient in whom the initial exploration through Henry’s approach revealed extensive “bursitis.” Only after careful inspection of the biceps tendon was it noted that a 50% disruption had occurred.11 My experience suggests that a partial rupture of the biceps tendon occurs first and that the second episode of pain indicates complete rupture. Later, secondary stretch or rupture of the lacertus fibrosus may occur (Fig. 34-20). Rarely, the cubital bursitis can enlarge to produce an insidious compressive neuropathy of the posterior interosseous nerve.
TREATMENT
The treatment of the partial tendon rupture may best be understood by considering the pathology of a degenerative tendon. Reimplantation of the remaining portion of the tendon to the radial tuberosity does not reliably relieve pain.16 Complete removal of the remaining fibers (which effectively creates a complete tear), trimming of the distal tendon, and then reattachment as for an acute injury is the treatment of choice.
CALCIFIC TENDINITIS
Acute calcific tendinitis does occur in the distal biceps tendon but very rarely.58 Calcification has also been observed in more chronic presentations associated with overuse activities.10 There appears to be no relationship between the acute process and subsequent degeneration and rupture. It is possible for the process to resolve spontaneously and completely. Cortisone injections must be considered very cautiously owing to the proximity of the radial nerve. Supportive treatment includes rest and anti-inflammatory medications.
RUPTURE OF THE BRACHIALIS MUSCLE
A single case report describes rupture of the brachialis muscle at the musculotendinous junction after direct trauma to the muscle.32 Diagnosis was made by demonstrating a palpable defect at the musculotendinous junction. Treatment by direct suture was reported to be successful.32 Coonrad and coworkers17 also reported snapping of a brachialis tendon that caused pain and median nerve irritation after a hyperextension injury. Release of the abnormal bone relieved the symptoms.
1 Acquaviva J. Rupture du tendon inférieur du biceps brachial droit a son insertion sur la tuberosité bicipitale: Tenosuture success operatoire. Marseilles Med. 1898;35:570.
2 Agins H.J., Chess J.L., Hoekstra D.V., Teitge R.A. Rupture of the distal insertion of the biceps brachii tendon. Clin. Orthop. Relat. Res. 1988;234:34.
3 Anzel S.H., Covey K.W., Weiner A.D., Lipscomb P.R. Disruption of muscles and tendons: An analysis of 1,014 cases. Surgery. 1959;45:406.
4 Bain G.I., Prem H., Heptinstall R.J., Verhellen R., Paix D. Repair of distal biceps tendon rupture: A new technique using the Endobutton. J. Shoulder Elbow Surg. 2000;9:120.
5 Baker B.E. Operative vs. nonoperative treatments of disruption of the distal tendon of biceps. Orthop. Rev. 1982;11:71.
6 Baker B.E., Bierwagen D. Rupture of the distal tendon of the biceps brachii. J. Bone Joint Surg. 1985;67A:414.
7 Barnes S.J., Coleman S.G., Gilpin D. Repair of avulsed insertion of biceps: A new technique in. 4 cases. J. Bone Joint Surg.. 1993;75B:938.
8 Bauman B.S. Triceps tendon rupture. J. Bone Joint Surg. 1962;44A:741.
9 Bauman G.I. Rupture of the biceps tendon. J. Bone Joint Surg. 1934;16:966.
10 Bell M.M. Elbow pain in a cyclist. Physician Sports Med. 1997;25:83.
11 Bourne M.H., Morrey B.F. Partial rupture of the distal biceps tendon. Clin. Orthop. Relat. Res. 1981;291:143.
12 Boyd H.B., Anderson M.D. A method for reinsertion of the distal biceps brachii tendon. J. Bone Joint Surg. 1961;43A:1041.
13 Brickner W.M., Milch H. Ruptures of muscles and tendons. Int. Clin. 1928;2:94.
14 Chevallier C.H. Sur un cas de desinsertion du tendon bicipital inferieur. Mem. Acad. Chir. 1953;79:137.
15 Cirincione R.J., Baker B.E. Tendon ruptures with secondary hyperparathyroidism: A case report. J. Bone Joint Surg. 1975;57A:852.
16 Conwell H.E., Alldredge R.H. Ruptures and tears of muscles and tendons. Am. J. Surg. 1937;35:22.
17 Coonrad R.W., Spinner R.J. Snapping brachialis tendon associated with median neuropathy. A case report. J. Bone Joint Surg. 1995;7:1891.
18 Davis W.M., Yassine Z. An etiologic factor in the tear of the distal tendon of the biceps brachii. J. Bone Joint Surg. 1956;38A:1368.
19 Debeyre J. Desinsertion du tendon inferieur du biceps brachial. Mem. Acad. Chir. 1948;74:339.
20 Delarue J., Denoix P. L’alteration degenerative des tendons: Cause de rupture-amorce de tumeurs. Presse Med. 1946;54:869.
21 Dobbie R.P. Avulsion of the lower biceps brachii tendon: Analysis of fifty one previously reported cases. Am. J. Surg. 1941;51:661.
22 Eames M.H., Bain G.I., Fogg Q.A., van Riet R.P. Distal biceps tendon anatomy: A cadaveric study. J. Bone Joint Surg. 2007;89A:1044.
23 Failla J.M., Amadio P.C., Morrey B.F. Posttraumatic proximal radioulnar synostosis: Results of surgical treatment. J. Bone Joint Surg. 1989;71A:1208.
24 Failla J.M., Amadio P.C., Morrey B.F., Beckenbaugh R.D. Proximal radioulnar synostosis after repair of distal biceps brachii rupture by the two incision technique: Report of four cases. Clin. Orthop. Relat. Res. 1990;253:133.
25 Gilcreest E.L. Rupture of muscles and tendons. J. A. M. A. 1925;84:1819.
26 Giuffre B.M., Moss M.J. Optimal position for MRI of the distal biceps brachii tendon: flexed abducted supinated view. Am. J. Radiol. 2004;182:994.
27 Giugaro A., Proscia N. Le rotture del tendine distale e del tendine del capo breve del bicipite brachiale. Min. Orthop. 1957;8:57.
28 Granato F., Marcacci G. Su tre casi di lacerazione traumatic della inserzione distale del bicipite brachiale. Clin. Orthop. Relat. Res. 1957;9:245.
29 Greenberg J.A., Fernandez J.J., Wang T., Turner C. EndoButton-assisted repair of distal biceps tendon ruptures. J. Shoulder Elbow Surg. 2003;12:484.
30 Haldeman K.O., Soto Hall R. Injuries to muscles and tendons. J. A. M. A. 1935;104:2319.
31 Hallam P., Bain G.I. Repair of chronic distal biceps tendon ruptures using autologous hamstring graft and the endobutton. J. Shoulder Elbow Surg. 2004;13:648.
32 Hamilton A.T. Subcutaneous rupture of the brachioradialis muscle. Surgery. 1948;23:806.
33 Hang D.W., Bach B.R.Jr., Bojchuk J. Repair of chronic distal biceps brachii tendon rupture using free autogenous semitendinosus tendon. Clin. Orthop. Relat. Res. 1996;323:188.
34 Hang L., Josefsson G. Rupture of the distal biceps tendon. Acta Orthop. Scand. 1977;48:280.
35 Hempel K., Schwenke K. Uber Abrisse der distalen Bizepssehne. Arch. Orthop. Unfallchir. 1974;79:313.
36 Hook F.R., Mazet R.Jr. Avulsion of the biceps tendon from its radial insertion. U.S. Nav. Med. Bull. 1942;40:409.
37 Hovelius L., Josefsson G. Rupture of the distal biceps tendon. Acta Orthop. Scand. 1977;48:280.
38 Jaslow I.A., May V.R. Avulsion of the distal tendon of the biceps brachii muscle. Guthrie Clin. Bull. 1946;15:124.
39 John, C. K., Field, L. D., Weiss, K. S., Savoie, F. H., and Roanoke, B. C.: Single incision repair of acute distal biceps ruptures by use of suture anchors. J. Shoulder Elbow Surg. (in press).
40 Johnson A.B. Avulsion of biceps tendon from the radius. N. Y. Med. J. 1897;66:261.
41 Jones M.E., Rider M.A., Hughes J., Tonkin M.A. The use of a proximally based posterior interosseous adipofascial flap to prevent recurrent of synostosis of the elbow joint and forearm. J. Hand Surg. Eur. 2007;32:143.
42 Karanjia N.D., Stiles P.J. Cubital bursitis. J. Bone Joint Surg. 1988;70B:832.
43 Katzman B.M., Caligiuri D.A., Klein D.M., Gorup J.M. Delayed onset of posterior interosseous nerve palsy after distal biceps tendon repair. J. Shoulder Elbow Surg. 1997;6:393.
44 Kelly E.W., Morrey B.F., O’Driscoll S.H. Complications of repair of the distal biceps tendon with modified two-incision technique. J. Bone Joint Surg. 2000;82A:1575.
45 Kron S.D., Satinsky V.P. Avulsion of the distal biceps brachii tendon. Am. J. Surg. 1954;88:657.
46 Lee H.G. Traumatic avulsion of tendon of insertion of biceps brachii. Am. J. Surg. 1951;82:290.
47 Le Huec J.C., Moinard M., Liquois F., Zipolia B., Chauveaux D., Le Rebeller A. Distal rupture of the tendon of biceps brachii: Evaluation by MRI and the results of repair. J. Bone Joint Surg. 1996;78B:767.
48 Leighton M.M., Bush-Joseph C.A., Bach B.R.Jr. Distal biceps brachii repair: Results of dominant and nondominant extremities. Clin. Orthop. Relat. Res. 1995;317:114.
49 Levy H.J., Mashoof A.A., Morgan D. Repair of chronic ruptures of the distal biceps tendon using flexor carpi radialis tendon graft. Am. J Sports Med. 2000;28:538.
50 Louis D.S., Hankin F.M., Eckenrode J.F., Smith P.A., Wojtys E.M. Distal biceps brachii tendon avulsion: A simplified method of operative repair. Am. J. Sports Med. 1986;14:234.
51 Louis D.S., Peck D. Triceps avulsion fracture in a weightlifter. Orthopedics. 1992;15:207.
52 Maydl K. Uber subcutane Muskel und Sehnenzerreissungen, sowie Rissfracturen mir Berucksichtigung der Analogen, durch directe gewalt Enstandenen und offenen Verletzungen. Deut. Zschr. Chir. 1883;17(306):35. 1882;18
53 McKee M.D., Hirji R., Schemitsch E.H., Wild L.M., Waddell J.P. Patient-oriented functional outcome after repair of distal biceps tendon ruptures using a single-incision technique. J. Shoulder Elbow Surg. 2005;14:302.
54 McReynolds I.S. Avulsion of the insertion of the biceps brachii tendon and its surgical treatment. J. Bone Joint Surg. 1963;45A:1780-1781.
55 Meherin J.H., Kilgore B.S.Jr. The treatment of rupture of the distal biceps brachii tendon. Am. J. Surg. 1960;99:636.
56 Morrey B.F. Distal biceps tendon injury. In Morrey B.F., editor: The Elbow: Master Techniques in Orthopaedic Surgery, 3rd ed., Philadelphia: Lippincott Williams & Wilkins, 2007.
57 Morrey B.F., Askew L.J., An K.H., Dobyns J.H. Rupture of the distal biceps tendon: Biomechanical assessment of different treatment options. J. Bone Joint Surg. 1985;67A:418.
58 Murase T., Tsuyuguchi Y., Hidaka N. Calcific tendinitis at the biceps insertion causing rotatory limitation of the forearm: A case report. J. Hand Surg. 1994;19:266.
59 Murphy K.J., McPhee I. Tears of major tendons in chronic acidosis with elastosis. J. Bone Joint Surg. 1965;47A:1253.
60 Norman W.H. Repair of avulsion of insertion of biceps brachii tendon. Clin. Orthop. Relat. Res. 1985;193:189.
61 Platt H. Observations of some tendon ruptures. Br. Med. J. 1931;1:611.
62 Postacchini F., Puddu G. Subcutaneous rupture of the distal biceps brachii tendon. J. Sports Med. 1975;15:81.
63 Preston F.S., Adicoff A. Hyperparathyroidism with avulsion at three major tendons. N. Engl. J. Med. 1961;266:968.
64 Rantanen J., Orava S. Rupture of the distal biceps tendon. A report of 19 patients treated with anatomic reinsertion, and a metaanalysis of 147 cases found in the literature. Am. J. Sports Med. 1999;27:128.
65 Sanchez-Sotelo J., Morrey B.F., Adams R.A. Reconstruction of chronic ruptures of the distal biceps tendon with use of an Achilles tendon allograft. J. Bone Joint Surg. 2002;84:999.
66 Seiler J.G.3rd, Parker L.M., Chamberland P.D., Sherbourne G.M., Carpenter W.A. The distal biceps tendon. Two potential mechanisms involved in its rupture: Arterial supply and mechanical impingement. J. Shoulder Elbow Surg. 1995;4:149.
67 Spang J.T., Weinhold P.S., Karas S.G. A biomechanical comparison of EndoButton versus suture anchor repair of distal biceps tendon injuries. J. Shoulder Elbow Surg. 2006;15:509.
68 Steindler D. Traumatic Deformities of the Upper Extremities. Springfield, IL: Charles C Thomas, 1946.
69 Straugh R.J., Michelson H., Rosenwasser M.P. Repair of rupture of the distal tendon of the biceps brachii. Review of the literature and report of three cases treated with a single anterior incision and suture anchors. Am. J. Orthop. 1997;26:151.
70 Waugh R.L., Hathcock T.A., Elliott J.L. Ruptures of muscle and tendons. Surgery. 1949;25:370.
71 Wener J.A., Schein A.J. Simultaneous bilateral rupture of the patella tendon and quadriceps expansions in systemic lupus erythematosus: a case report. J. Bone Joint Surg. 1974;56A:823.
72 Wiley W.B., Noble J.S., Dunlaney T.D., Bell R.H., Noble D.D. Late reconstruction of chronic distal biceps tendon ruptures with a semitendinosus autograft technique. J. Shoulder Elbow Surg. 2006;15:440.
73 Witvoet J., Robin B., Charbrol J. A propos d’une desinsertion de l’extremite inférieur du biceps brachial. Presse Med. 1966;74:389.