8 Injury and Trauma
Etiology and Pathogenesis
The most common causes of injuries and resultant injury patterns are age specific. In infants (younger than 1 year of age), a high percentage of injuries are nonaccidental in nature, and it is important to maintain a high index of suspicion for possible inflicted injuries (see Chapter 12). Falls are the most common cause of injury in children from 1 to 14 years of age. Motor vehicle collisions and motor vehicle–pedestrian incidents are the most common causes of fatal injuries in children ages 1 to 18 years. Drowning (see Chapter 6) is the second most common cause of fatalities in younger children, and firearm-related deaths are the next most common cause in adolescents ages 15 to 18 years.
Evaluation and Management
Primary Survey (see Chapter 1)
Airway
Readers are directed to Chapter 1 for complete information about airway evaluation and management. However, it is important to reiterate here the need for inline stabilization of the cervical spine (c-spine) during this assessment and treatment, especially if intubation is attempted. The collar should be opened or removed before direct laryngoscopy because it can impede successful visualization of the larynx. An assistant should hold the patient in the midclavicular line with the ears firmly between the lower arms to eliminate movement of the c-spine during intubation.
Breathing
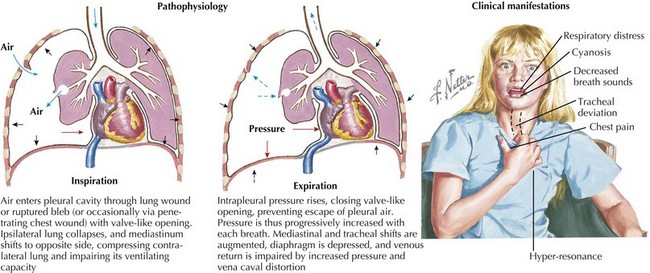
An absence of breath sounds, especially in conjunction with hypotension, should alert the clinician to possible tension pneumothorax. Tracheal deviation to the opposite side and hyperresonance of the chest to percussion may be less obvious in pediatric patients, and the more mobile mediastinum in this age group may produce vascular collapse in a more rapid fashion. Needle decompression can be immediately undertaken in such circumstances, with the introduction of a large-bore over-the-needle catheter (e.g., a 14-gauge intravenous [IV] catheter) into the second intercostal space in the midclavicular line. Needle decompression necessitates the subsequent placement of a chest tube. Massive hemothorax can present in a similar fashion, although the chest should be dull to percussion, and severe hypotension often predominates because of the significant blood loss (Figure 8-1).
Circulation
Complete details on hypoperfusion and shock may be found in Chapter 2. In patients who have sustained significant traumatic injuries, IV access should be secured as quickly as possible with two large-bore IV catheters placed in large peripheral veins. If peripheral access attempts are unsuccessful in a patient showing signs of shock, clinicians should proceed quickly to obtain interosseous (IO) access. IO lines should not be placed distal to any obvious fractures.
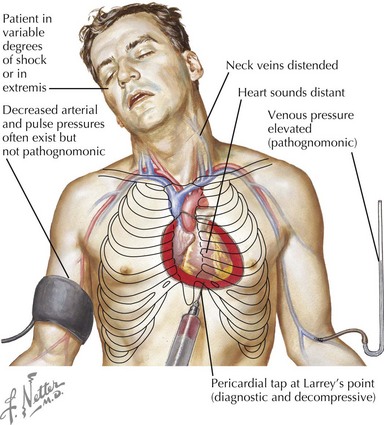
Cardiac tamponade is more common with penetrating chest wounds but can be caused by rupture of the myocardium with blunt traumatic force. As with tension pneumothorax, patients with cardiac tamponade present with tachycardia, hypotension, and distended jugular veins. However, with tamponade, there is no tracheal deviation. Pulsus paradoxus, which is exaggeration of the normal decrease in blood pressure with spontaneous inspiration, may be present in association with tamponade. Rapid bedside ultrasonography can help make the diagnosis, but if unavailable or if the patient is hemodynamically unstable, pericardiocentesis can be used to diagnose and treat tamponade (Figure 8-2).
Disability
After the patient’s hemodynamic status has been stabilized, the neurologic status is evaluated. The symmetry, size, and briskness of pupillary response should be documented along with the level of responsiveness. Numerical scales, such as the Glasgow Coma Scale (GCS, see Figure 1-8), are used to generate structured assessments of the level of responsiveness. This allows for comparisons in mental status evaluations over time, comparisons of assessments performed by different clinicians, and improved communication among providers. The GCS has been adapted for use in preverbal patients as well. A more straightforward, although somewhat less nuanced, system for rapid neurologic evaluation is the AVPU (awake, verbal, pain, unresponsive) system. Abnormalities in the pupillary response or level of consciousness should increase concern for intracranial injuries and alert the team to prepare for possible interventions such as intubation for airway protection or to improve ventilation, mannitol, or hypertonic saline administration for increased intracranial pressure (ICP) or emergent neurosurgical intervention.
Secondary Survey
Head
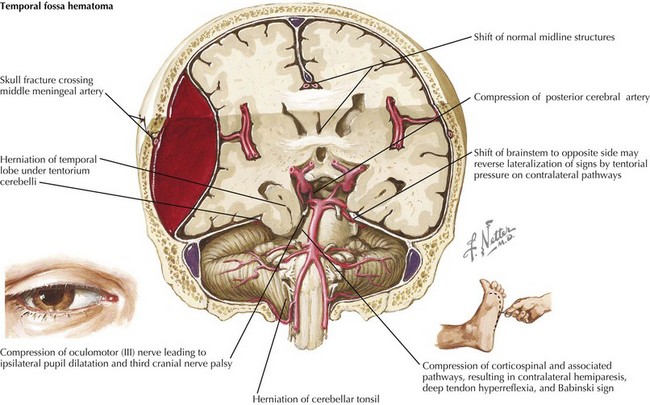
The initial evaluation of the head involves inspection for evidence of injury to the skull, as well as assessment of level of consciousness and neurologic status, which may indicate underlying brain injuries. Locations of all hematomas, lacerations, abrasions, depressions, and areas of tenderness should be documented. Because the middle meningeal artery runs through the temporal bone, hematomas or other signs of injury in the temporal region raise concerns for the possibility of an underlying epidural hematoma as a result of tearing of this artery. Epidural hematomas (Figure 8-3) are often described as presenting with a lucid interval followed by a rapid deterioration in mental status when the volume of blood filling the epidural space reaches the threshold to cause significant mass effect. On computed tomography (CT), epidural hematomas are seen as a convex fluid collection between the skull and brain. Significant epidural hematomas represent a neurosurgical emergency because evacuation of the growing hematoma before herniation can be lifesaving.
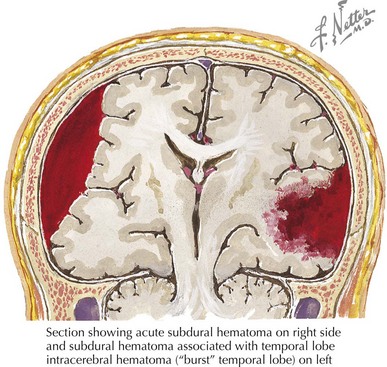
Subdural hematomas are a second, more common intracranial hemorrhage. They may be seen without significant external signs of trauma. Subdural hematomas (Figure 8-4) are usually caused by tearing of small bridging veins from the surface of the cortex to the inner layer of the dura mater. These injuries are often caused by high-force, rapid flexion and extension of the head. CT will show concave fluid collections between the skull and brain. Although subdural hematomas are less likely to lead to the rapid onset of significant symptoms than are epidural hematomas, they are more often associated with significant underlying brain damage because of the mechanism of injury. In infants and toddlers, it is important to remember that subdural hematomas can be associated with nonaccidental injury from shaking the child or as part of the shake and impact syndrome (see Chapter 12).
Both epidural hematomas and subdural hematomas can become large enough to lead to significant increases in ICP (see Chapter 10). When ICP increases, herniation of brain tissue across the tentorium or downward through the foramen magnum may occur. Bradycardia, hypertension, and irregular respirations (Cushing’s triad) indicate impeding herniation. Transtentorial herniation is heralded by a decreased level of consciousness and asymmetric pupillary responses. Rapid therapy, including brief periods of hyperventilation and IV administration of 0.25 to 1.0 g/kg of mannitol or 5 mL/kg of 3% sodium chloride solution may temporize the situation until more definitive therapy, such as surgical evacuation of a hematoma or drainage of cerebrospinal fluid (CSF) through an intraventricular catheter, can occur.
Most children who sustain head injuries have seemingly mild injuries and look well on initial presentation. In these children, the relatively low risk of underlying significant intracranial injuries must be weighed against the radiation involved in imaging the brain and the possible risk of malignancies in the future associated with this imaging. A decision rule based on a large, multicenter, prospective study has identified historical and physical findings associated with intracranial injuries on CT scans in children (Box 8-1). CT scans are rarely indicated in the absence of any of these findings in children.
Box 8-1
Factors Associated with Positive Findings on Computed Tomography Scans in Children with Seemingly Mild Head Injuries
Children younger than 2 years old
Adapted from Kuppermann N, Holmes JF, Dayan PS, et al: Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet 374:1160-1170, 2009.
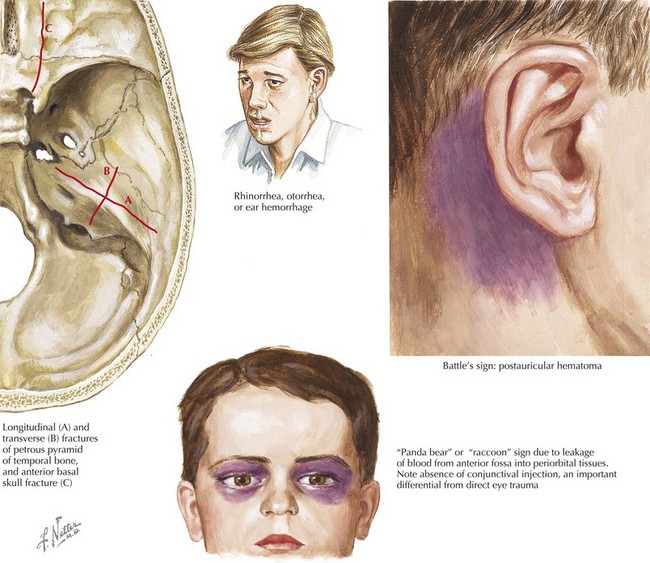
Basilar skull fractures require special evaluation and treatment because they raise concern for other injuries associated with the significant forces needed to produce them, as well as their unique location, which may lead to significant complications, including late intracranial hemorrhages, carotid artery dissections, and intracranial infections. Basilar skull fractures should be suspected when any of the following are present: “raccoon eyes” caused by periorbital ecchymoses; Battle sign or postauricular ecchymoses; hemotympanum; clear rhinorrhea or clear otorrhea caused by CSF leakage from the nose or ear, respectively; or cranial nerve VII or VIII dysfunction (Figure 8-5). Neurosurgical input should be obtained early in management.
Neck and Spine
Any child who has sustained a severe head injury should be assumed to have a c-spine injury and remain in spinal immobilization until there is clear clinical or radiologic evidence that there is no spinal injury. Plain radiographs and CT scans may aid in this evaluation, but in patients with a decreased level of consciousness, magnetic resonance imaging may be required. As long as immobilization is maintained, this can be delayed until the child has been stabilized and other major traumatic injuries have been addressed. In awake patients, clinical signs of spine injuries include posterior midline tenderness and limitation of motion. Even in patients with a normal level of consciousness, clinical clearance of the c-spine is especially difficult in patients who are preverbal and young children who are uncooperative because of fear, anxiety, or pain associated with other injuries. It is important to remember that children are at risk of spinal cord injury without radiologic abnormalities (SCIWORA) because of the relative ligamentous laxity found in their c-spines. Therefore, normal radiographs may not completely rule out injury to the spinal cord itself, and MRI may be necessary for complete diagnosis. Detailed discussion of spinal injuries can be found in Chapter 24.
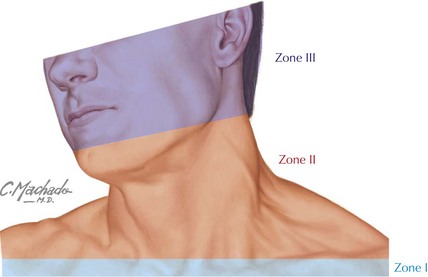
Evaluation of the neck should also involve inspection for signs of penetrating injury. The neck is often divided into three zones (Figure 8-6) according to the collection of structures at risk of injury, with zone I covering the area between the thoracic inlet and the cricoid cartilage, zone II covering the cricoid cartilage to the angle of the mandible, and zone III above the angle of the mandible. Injuries to zones I and II may be associated with pneumothorax or hemothorax. Injuries in zone II are the easiest to explore surgically but also the most likely to involve major vascular structures and therefore are often brought directly to the operating room for exploration if they extend through the platysma. If clinically stable, zone I and III injuries are often evaluated with diagnostic imaging to determine appropriate management before surgical exploration.
Abdomen
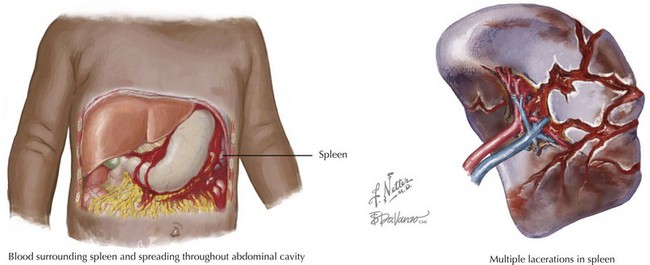
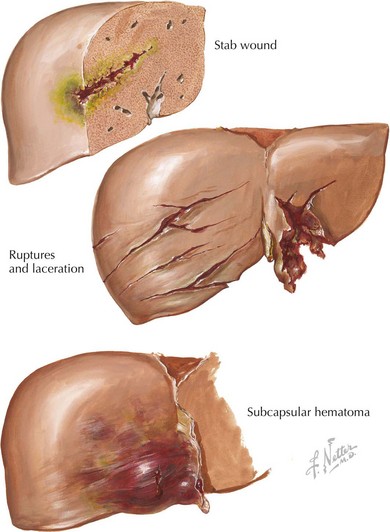
The spleen is the most commonly injured abdominal organ (Figure 8-7). Patients with splenic lacerations may present with left upper quadrant pain that radiates to the left shoulder with or without signs of peritoneal irritation. The liver is also commonly injured in children sustaining trauma (Figure 8-8). Liver lacerations may present with right upper quadrant tenderness that may radiate to the right shoulder after blunt trauma. Hemodynamically stable children with spleen or liver lacerations can be conservatively managed with bed rest and close monitoring of vital signs and hematocrit levels. Children with unstable vital signs that do not improve with aggressive volume resuscitation may require operative intervention or embolization of bleeding vessels by an interventional radiologist experienced in the treatment of children with significant injuries. Children who have sustained significant splenic injuries, especially those who undergo splenectomy, are at increased risk of overwhelming sepsis with encapsulated bacteria (e.g., Streptococcus pneumoniae). Pneumococcal vaccination and consideration of long-term antibiotic prophylaxis (e.g., daily oral penicillin) should be considered based on the child’s age and clinical situation.
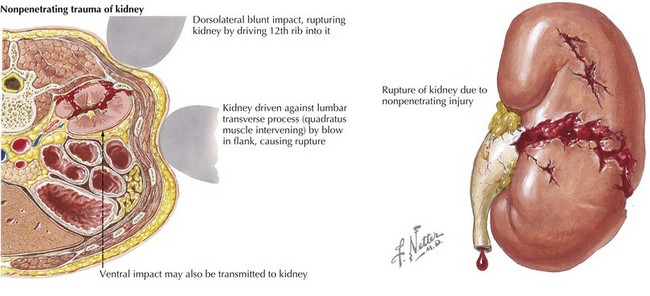
Although the kidneys are more protected than other abdominal organs, renal injury should be suspected in children with injury to the flank or back, significant back pain, or gross hematuria (Figure 8-9). Urinalysis can be used as screening for more subtle injury, and CT or renal ultrasonography can be used to confirm and detail injuries.
Extremities and Neurologic Status
The final steps in the secondary survey include a rapid but complete evaluation of the extremities and evaluation for focal neurologic deficits. This is usually accomplished by palpation of the full extent of each extremity noting tenderness, lacerations, and deformity. Tenderness to palpation or observed deformity should prompt radiologic evaluation. Further discussion of common pediatric fractures can be found in Chapter 22. Neurologic evaluation is often accomplished in conjunction with the extremity evaluation, briefly testing strength and sensation of each extremity, with cooperation acting as a quick evaluation of mental status. Focal deficits raise concern for intracranial or spinal cord injury depending on the location and extent. Appropriate imaging of the head and spine should follow from the clinical examination, as appropriate.
AAP Joint Statement. Management of pediatric trauma. Pediatrics. 2008;121:849-854.
Abujamra L, Joseph MM. Penetrating neck injuries in children: a retrospective review. Pediatr Emerg Care. 2003;19(5):308-313.
American College of Surgeons Committee on Trauma. Advanced Trauma Life Support for Doctors (ATLS) Student Course Manual, ed 7. Chicago: ACS; 2004.
Avarello JT, Cantor RM. Pediatric major trauma: an approach to evaluation and management. Emerg Med Clin of North Am. 2007;25:803-836.
DeRoss AL, Vane DW. Early evaluation and resuscitation of the pediatric trauma patient. Semin Pediatr Surg. 2004;13(2):74-79.
Durbin DR, American Academy of PediatricsCommittee on InjuryViolencePoison Prevention. Policy Statement—Child Passenger Safety. Pediatrics. 2011;127:788-793.
Gaines BA, Ford HR. Abdominal and pelvic trauma in children. Crit Care Med. 2002;30(suppl):S416-S423.
Garcia VF, Brown RL. Pediatric trauma beyond the brain. Crit Care Clin. 2003;19:551-561.
Kirkwood MW, Yeates KO, Wilson PE. Pediatric sport-related concussion: a review of the clinical management of an oft-neglected population. Pediatrics. 2006;117:1359-1371.
Kleinerman RA. Cancer risks following diagnostic and therapeutic radiation exposure in children. Pediatr Radiol. 2006;36(suppl 2):121S-125S.
Kuppermann N, Holmes JF, Dayan PS, et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 2009;374:1160-1170.
Mami AG, Nance ML. Management of mild head injury in the pediatric patient. Adv Pediatr. 2008;55:385-394.
Meehan WPIII, Bachur RG. Sport-related concussion. Pediatrics. 2009;123:114-123.
McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport: the 3rd International Conference on Concussion in Sport, Zurich, Nov 2008. Br J Sports Med. 2009;43:76-84.
O’Connell KJ, Farah MM, Spandorfer P, Zorc JJ. Family presence during pediatric trauma team activation: an assessment of a structured program. Pediatrics. 2007;120(3):e565-e574.
Wegner S, Colletti JE, Wie DV. Pediatric blunt abdominal trauma. Pediatr Clin North Am. 2006;53:243-256.