Chapter 12. Injuries to the upper limb
Brachial plexus lesions
Brachial plexus lesions are serious and tragic. The most frequent victims are young men thrown from their motorcycles who may become unemployable as a result of their injuries.
Closed injuries
Closed injuries can occur in two ways:
1. By violent lateral flexion of the neck with depression of the shoulder or forced abduction of the arm.
2. At birth, although this is now rare in developed countries. This is associated with obstructed or difficult deliveries.
Open injuries
In the past, cavalrymen wielding sabres disabled the enemy by cutting the upper cords of the brachial plexus of opposing infantry. Today, open injuries still occur and are just as devastating but they are more often caused by falling objects such as glass or steel.
Patterns of brachial plexus lesion
• Supraclavicular lesions, which can be (1) preganglionic or (2) postganglionic.
• Infraclavicular lesions.
Supraclavicular lesions
Trauma
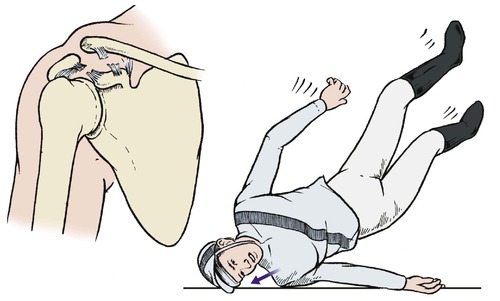
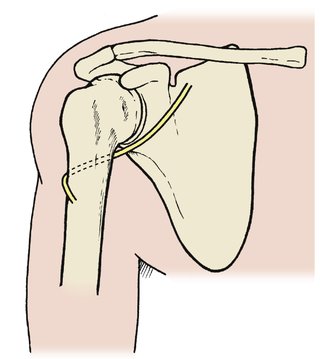
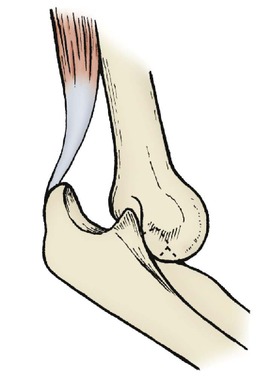
Blows to the shoulder and head cause violent lateral flexion of the cervical spine and depression of the shoulder. This tears the upper part of the brachial plexus. In the UK about 90% of these injuries occur in motorcyclists landing on the head and shoulder (Fig. 12.1).
 |
| Fig. 12.1
Traction injury of the brachial plexus. Violent abduction of the neck and shoulder can tear the upper cords of the brachial plexus.
|
Obstetric palsy
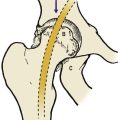
If the upper cords of the plexus are damaged at birth, the supinator, deltoid, wrist extensors and elbow flexors will be weak, causing a ‘waiter’s tip’ position of the arm (Fig. 12.2). This condition is known as Erb’s palsy, a term which is often applied to the same pattern of neurological deficit in the adult.
 |
| Fig. 12.2
The position of the hand in Erb’s palsy.
|
Infraclavicular lesions
Trauma
Injuries in which the arm is violently abducted can tear the lower part of the brachial plexus. The commonest mechanism is anterior dislocation of the shoulder, but the lesion can also be caused by a fall from a height in which the hand is caught so that the full weight is taken by the arm.
Birth trauma
The end result of damage to the lower cords of the brachial plexus at birth is a Klumpke’s palsy, which consists of a weakness of the finger flexors and intrinsics.
Assessment
The first step in management is to define the anatomy of the lesion. The roots, trunks or branches of the brachial plexus can be torn or the roots avulsed from the spinal cord. Each lesion has a different prognosis and the site of the lesion must be identified by a careful neurological examination.
The anatomy of the brachial plexus is so variable that trying to identify the exact site of the lesion using a map of the brachial plexus is most unreliable, but it does give a rough idea of the extent of the lesion (Fig. 12.3). In general terms, the more distal the lesion, the better the prognosis.
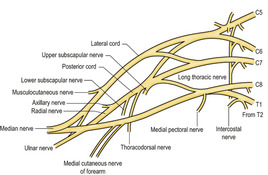 |
| Fig. 12.3
The brachial plexus. The anatomy is very variable.
|
It is important to decide whether the lesion lies between the spinal cord and the dorsal root ganglion (preganglionic) or distal to the ganglion (postganglionic). Preganglionic lesions never recover, postganglionic lesions sometimes do.
One way of determining the exact site of the lesion clinically is to assess muscle function. The first branches to leave the brachial plexus are the motor nerves to the rhomboids and levator scapulae. If the patient has power in these muscles and can elevate the scapula, the lesion must be distal to the origin of these nerves from the plexus and the prognosis will be better than for a patient who cannot elevate the scapula.
A useful approach is to look at the activity of the autonomic nervous system. If a Horner’s syndrome is present, the lesion must be close to the cord and the prognosis is poor (Fig. 12.4). Axonal reflexes involving the triple response or sweating can also be used. If axonal reflexes are present but the function of the dorsal root ganglion is absent, the lesion must be preganglionic and close to the cord.
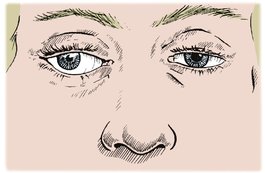 |
| Fig. 12.4
Horner’s syndrome, with drooping eyelid, small pupil, slight protrusion of the eyeball and no sweating of the surrounding skin.
|
Investigations are less useful than clinical examination. The most useful investigation is the EMG, which can identify accurately the roots involved. Radiculography will show if the roots are still attached to the spinal cord and may demonstrate traumatic meningocoeles along the roots, but reveals little else. CT scanning does not give much information about the peripheral nerves, although MRI may prove helpful.
Treatment
If the roots are torn out of the spinal cord, nothing can be done to restore continuity. If the lesions are distal to the ganglion or there is a clean cut across the nerve, microsurgical repair may be possible. Cable grafting of defects in the supraclavicular part of the plexus is practised but the results are unpredictable, and a few patients eventually request amputation to rid themselves of their heavy, useless arm (p. 86).
Artificial limbs are available but many patients find them an encumbrance and do not wear them.
Management of brachial plexus lesions
1. Identify the site of the lesion by careful neurological examination and EMG.
2. Decide if the lesion is preganglionic or postganglionic.
3. Preganglionic lesions (Horner’s syndrome, absent axonal reflex) cannot be repaired.
4. Postganglionic lesions have a better prognosis: the more distal, the better the outlook.
5. Surgical repair or grafting is sometimes possible for clean cuts and distal lesions.
Injuries to the clavicle
A fractured clavicle is one of the commonest of all fractures. Clavicular injuries include (Fig. 12.5):
 |
| Fig. 12.5
Sites of fracture of the clavicle.
|
1. Fracture of the midshaft of the clavicle.
2. Fracture of the outer end of the clavicle.
3. Acromioclavicular separation.
4. Sternoclavicular dislocation.
Fracture of the midshaft of the clavicle
The usual force that breaks a clavicle is a violent upwards and backwards thrust caused by landing on the outstretched hand or a direct blow to the point of the shoulder. This can happen after being thrown from a horse or going over the handlebars of a bicycle. The domestic cat does not have this problem because its clavicles are free at both ends (Fig. 12.6). Humans have clavicles firmly attached to the sternum medially and the acromion and coracoid laterally by ligaments that are stronger than the bone. The clavicle therefore fractures instead of moving to absorb the impact.
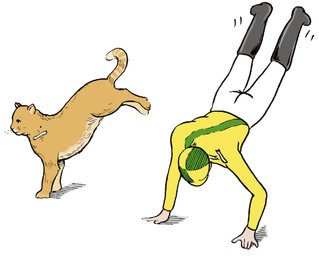 |
| Fig. 12.6
Falls on the outstretched arm. The cat does not fracture its clavicle because the sternum and humerus are not linked as in humans.
|
The cat’s clavicle is adapted for landing on the forelegs but the forearms of humans are adapted for carrying weights. The human clavicle acts as a strut to hold the shoulder and arm away from the body, like a cantilever (Fig. 12.7). This function is only possible if the bone is intact; when the clavicle is broken the weight of the arm makes the fragments overlap and go on to malunion (Fig. 12.8).
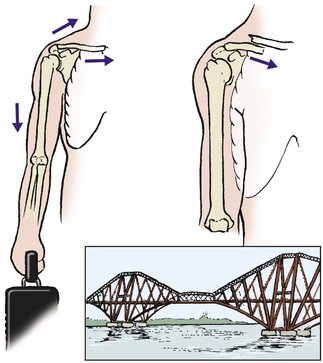 |
| Fig. 12.7
Cantilever action of the clavicle. When the clavicle is broken, the shoulder is not supported and moves downwards and medially.
|
 |
| Fig. 12.8
Malunion of the clavicle with overriding bone fragments.
|
In adults, a fractured clavicle takes about 6 weeks to become solid, although function returns after about 3 weeks. In children the fracture will be solid after only 2 or 3 weeks. If the fracture is comminuted, it will usually unite more quickly than a simple transverse fracture because there is more callus to ‘glue’ the bone ends together.
Complications
Complications are often seen after this injury (Fig. 12.9).
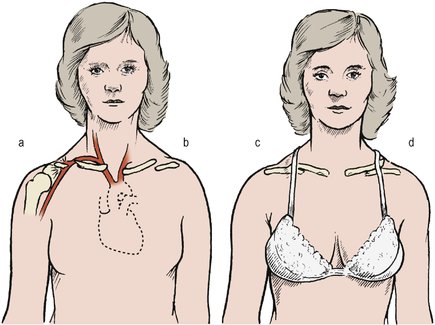 |
| Fig. 12.9
Complications of fractured clavicle: (a) damage to the great vessels; (b) non-union; (c) malunion; (d) a spike of bone.
|
Malunion. Because the fragments are displaced by the weight of the arm, malunion is unavoidable. Internal fixation with a contoured plate may give better anatomical results but the surgery has risks (neurovascular, skin etc.)
Damage to vessels. Splinters of bone can rupture the great vessels or the lung at the time of injury. It is said that Sir Robert Peel (the founder of the Metropolitan Police Force) died from this complication after being thrown by his horse.
Non-union is unusual and seldom causes symptoms. Internal fixation and grafting are required on the rare occasions when it does cause symptoms.
Deformity. Large spicules of bone around the fracture site can produce an unsightly appearance, as well as an unwelcome pressure area, and may need removing (Fig. 12.10).
 |
| Fig. 12.10
Malunion with an unsightly bony prominence at the site of fracture.
|
The callus at the fracture site also produces a visible lump that interferes with the shoulder straps of bras and backpacks. The lump is particularly alarming to the parents of children with a greenstick fracture of the clavicle. The clavicle looks normal immediately after injury and the swelling may be mistaken for a malignant tumour. In time, the swelling diminishes as the bone remodels and the surrounding bone enlarges.
Treatment
A sling to support the weight of the arm relieves pain at the fracture site, but the sling must not rub against the fracture. The sling can be removed after 10 days if pain permits. Greenstick fractures require very little support (Fig. 12.11).
 |
| Fig. 12.11
Greenstick fracture of the clavicle.
|
A firm support such as a figure-of-eight bandage to pull the shoulders backwards also helps to relieve pain but it must be readjusted every few days (Fig. 12.12). The function of a figure-of-eight bandage is to support the fracture and not to reduce it. Harnesses and braces that attempt to reduce the fracture by pulling the shoulder blades backwards are doomed to failure: the arm weighs several kilograms and anything that exerts such a force on the shoulder is bound to cause pressure sores in the soft axillary skin, even without the sweat that is inevitable under a bulky dressing.
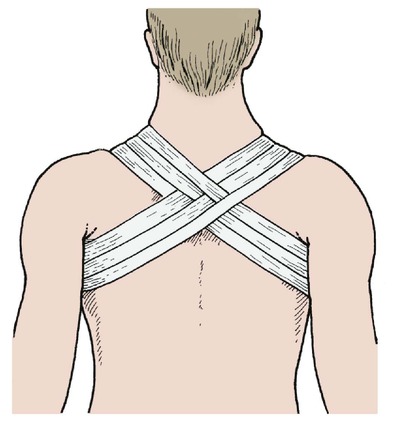 |
| Fig. 12.12
Figure-of-eight bandage for fractured clavicle.
|
Internal fixation is seldom required for fractures of the clavicle.
Fractures of the outer end of the clavicle
Fractures of the outer end of the clavicle lie lateral to the coracoclavicular ligament and the distal fragment remains attached to the acromion. Fractures may involve the acromioclavicular joint and may be displaced or undisplaced.
Thus, the fractures can be classified as displaced or undisplaced and articular or non-articular.
Treatment
Undisplaced non-articular fractures are treated conservatively with a sling, analgesics and early mobilization.
Complications
The fragment may fail to unite, causing a painful non-union. Excision of the un-united fragment may be needed if this occurs.
Acromioclavicular separation
The acromioclavicular joint is a plane joint between the end of the clavicle and the acromion. It contains a fibrocartilaginous disc and is easily disrupted by a fall onto the point of the shoulder (Fig. 12.13). The injury is sometimes called a ‘separated’ or ‘sprung’ shoulder and occurs in rugby football, riding accidents and ice hockey if the shoulder is struck against the boards around the rink. The lesion is usually a simple dislocation of the joint but a fragment of the clavicle sometimes remains attached to the acromion.
 |
| Fig. 12.13
Fracture of the acromioclavicular joint. Falling onto the point of the shoulder can rupture the coracoclavicular ligament.
|
Clinical examination will show tenderness of the acromioclavicular joint and a step at the joint, best seen when the arm is allowed to hang. The step can be eliminated by lifting the arm and the elbow while holding the clavicle down.
Grading and treatment
There are six grades of acromioclavicular separation. The grade determines the treatment:
1. Sprain with no displacement. Analgesics and symptomatic treatment only.
2. Subluxation. Treatment consists of analgesia and, if necessary, a sling to support the elbow.
3. Dislocation. Complete separation of the joint usually requires internal fixation.
4. Dislocation with perforation of the overlying deltotrapezius fascia. Open reduction with internal fixation and repair of the fascia may be needed.
5. Lesions described in (4) above with the addition of posterior dislocation. Open reduction and internal fixation is required for this serious injury.
6. Subcoracoid dislocation. Open reduction and internal fixation is required for this serious injury, which involves the scapula.
Sternoclavicular dislocation
The sternoclavicular joint lies medial to the stout costoclavicular ligament that acts as a pivot for the clavicle, which see-saws about this point. When the outer end of the clavicle is raised, the medial end moves downwards, and vice versa – confirm this by putting a finger on the medial end of the clavicle and moving the shoulder.
Treatment
If the injury is seen early, which is unusual, acute repair may be required. The decision to operate depends on the age and fitness of the patient and the severity of the injury. Left untreated, recurrent subluxation can occur. Soft tissue repair is difficult and the patient may prefer to accept the minor disability of recurrent subluxation instead.
Fractures of the scapula
Fractures of the acromion
The acromion can be broken by direct trauma or by violent abduction of the shoulder (Fig. 12.14). It is easy to confuse the normal apophysis of the acromion in the growing skeleton with a fracture, and many a normal acromioclavicular joint has been ‘treated’ in a sling for this reason.
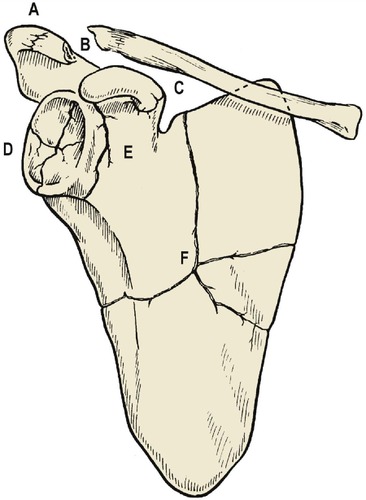 |
| Fig. 12.14
Sites of fracture of the scapula: ( A) acromion; ( B) fracture dislocation of the acromioclavicular joint; ( C) coracoid; ( D) glenoid; ( E) neck of scapula; ( F) blade of scapula.
|
Treatment
Acromioclavicular injuries with little separation and intact coracoclavicular ligaments require no treatment. Rest in a sling is sufficient unless there is gross displacement of the fragments, when internal fixation may be needed to stabilize the joint.
The blade of the scapula
The blade of the scapula, like the wing of the ilium, functions mainly as an attachment for muscles. It can be fractured by direct trauma, causing pain, bruising and soft tissue swelling.
Treatment
Treatment is by support in a sling, analgesics and early mobilization. A good result is usual, but the shoulder girdle may be weaker than before because of muscle damage.
The glenoid
The glenoid can be fractured by a direct blow to the shoulder from the lateral side, comparable with the force which causes a fracture of the floor of the acetabulum.
Treatment
Unless there is gross displacement of the fragments, treatment is by early mobilization. Because the glenoid is not a weight-bearing joint, exact anatomical restitution of the joint surfaces is less important than early mobilization.
Dislocation of the shoulder
The shoulder is mechanically unstable. The head of the humerus is held against the glenoid by a cowl of muscles that pull the round head of the humerus up against the small flat glenoid, which faces downwards. The cowl of muscles is complete everywhere except below, in the axilla, where there is nothing to hold the humeral head against the glenoid. Bearing this intrinsic instability in mind, it is remarkable that dislocation is not more common.
There are five types of shoulder dislocation:
1. Anterior dislocation.
2. Posterior dislocation.
3. Luxatio erecta, or true inferior dislocation.
4. Fracture dislocations.
5. Multidirectional.
Anterior dislocation
Anterior dislocation is by far the commonest pattern and is the result of the head of humerus slipping off the front of the glenoid when the arm is abducted and externally rotated (Fig. 12.15). The shoulder can also dislocate during grand mal attacks or electroconvulsive therapy and may then pass unnoticed for some days.
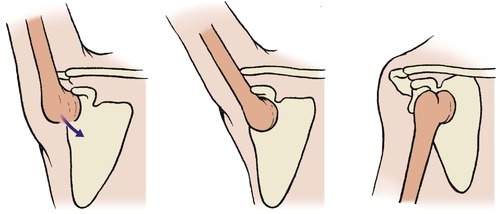 |
| Fig. 12.15
Mechanism of anterior dislocation of the humerus, beginning with abduction and extension.
|
Once off the glenoid, the head slips medially when the arm is lowered, producing the characteristic profile of a dislocated shoulder. Because the head of the humerus is not lying in its normal position, the shoulder has a flatter appearance than usual and the elbow points outwards. If the tip of the acromion and the lateral epicondyle can be joined by a straight line (Hamilton’s ruler test), the shoulder is dislocated (see Fig. 2.13).
This appearance, together with the observation that the patient is holding the injured arm in the other hand, makes it possible to diagnose a dislocated shoulder from the far end of the accident department. A similar flattened contour is also seen in patients with wasted deltoid muscles and in displaced fractures of the surgical neck, but in these patients the humeral head is still in its normal position and the ‘ruler test’ is negative.
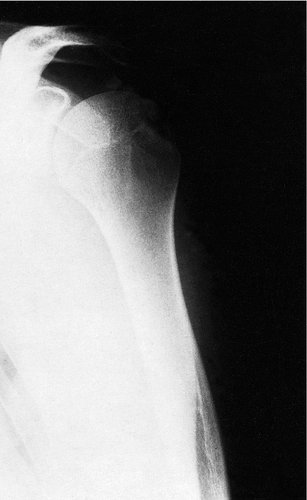
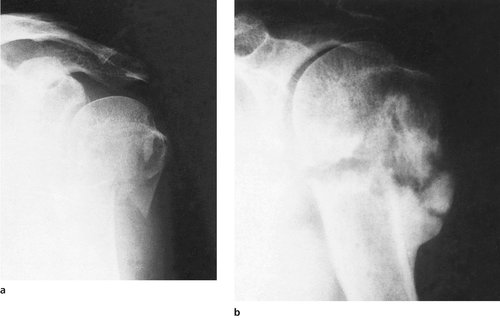
Radiographic examination of a dislocated shoulder is not easy (Fig. 12.16). It is difficult to position the patient accurately and the usual lateral film in abduction is impossible, but an axial view will reveal the dislocation. A lateral scapula view is excellent. Fractures of the humeral head should be looked for specifically, or they will be missed and a fracture dislocation will be treated as a simple dislocation, with potentially serious clinical and medicolegal consequences.
 |
| Fig. 12.16
Dislocation of the shoulder with separation of the greater tuberosity.
|
Complications
Complications of anterior dislocation of the shoulder
• Damage to the circumflex axillary nerve.
• Arterial damage.
• Irreducibility.
• Joint stiffness.
• Recurrent dislocation.
Neurological damage. Damage to the axillary nerve as it runs round the neck of the humerus (Fig. 12.17) causes partial or complete paralysis of the deltoid. When damage is suspected, the axillary nerve should be examined with an EMG 3 weeks after injury and again 3 weeks later. If there is no change between the two examinations, the nerve should be explored and, if necessary, repaired.
 |
| Fig. 12.17
To show the relationship of the circumflex humeral nerve to the deltoid and the surgical neck of the humerus.
|
Brachial plexus injuries also occur if there has been a violent abduction strain.
Arterial injury. The axillary artery can be damaged by traction at the time of injury or by pressure from the humeral head. The radial pulse should be checked and its presence recorded.
Irreducibility. The humeral head sometimes ‘buttonholes’ through the subscapularis, making reduction impossible. Open reduction is then necessary.
If the shoulder is not reduced within a few days of dislocation, reduction may then be impossible. This is a particular problem in elderly patients in whom the shoulder can be dislocated with trivial trauma. Open reduction is a difficult and uncertain operation and it may be better left dislocated in an elderly patient who places little demand on the shoulder.
Joint stiffness. Because the shoulder depends upon muscle and soft tissue for stability, adhesions or fibrosis in the rotator cuff can cause serious loss of movement. Physiotherapy is important to prevent this.
Recurrent dislocation. Once dislocated, the shoulder is liable to do so again and may require stabilization. Adequate treatment of the initial dislocation is therefore important.
Treatment
First, examine the shoulder radiologically, however obvious the diagnosis may be. Attempts to reduce the shoulder before radiographs are available are ill advised and may be dangerous if there is an associated fracture.
The humeral head must be reduced but, before attempting reduction, test the function of the axillary nerve, which runs around the surgical neck of the humerus. This nerve can be damaged either at the moment of dislocation or during reduction. Because the nerve is so vulnerable, it is important to test the function of the nerve and record it before reduction is attempted.
Motor function cannot be tested adequately but the area of sensory supply of the circumflex nerve, over the outer side of the deltoid, is easily tested. If there is any abnormality it should be clearly recorded and special care taken when the shoulder is reduced. If this is not done, any subsequent circumflex nerve dysfunction may be attributed to the reduction rather than the injury.
Manipulation under general anaesthetic (MUA). If there is no fracture of the humeral head, the shoulder can be reduced easily under general anaesthesia if required. No complicated manipulations are necessary; the arm can be pulled gently and the head pushed back over the lip of the glenoid.
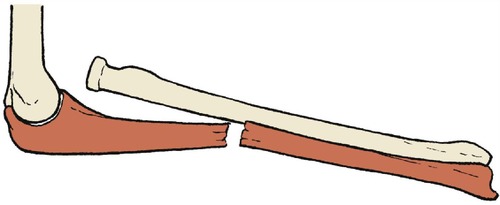
Hanging-arm technique. An alternative is to place the patient face down on a couch and allow the arm to hang freely without the patient holding on to the leg of the couch or supporting the arm in any way (Fig. 12.18). The weight of the arm will then achieve reduction but intravenous pethidine or valium may be needed to achieve adequate relaxation. This technique avoids general anaesthesia and the 4 h or so discomfort that is necessary if the patient has a full stomach and has to wait for general anaesthetic.
 |
| Fig. 12.18
Hanging-arm technique for reducing dislocation of the shoulder.
|
Hippocratic method. In days gone by, the shoulder had to be reduced without full muscle relaxation and, for many years, Hippocrates’ technique was used. The Hippocratic technique involved laying the patient on the floor, lifting and pulling the arm upwards and pushing the humeral head back into its correct position with the unbooted forefoot (Fig. 12.19).
 |
| Fig. 12.19
Hippocratic method of reducing a dislocated shoulder with the unbooted foot in the axilla.
|
Kocher’s method was less spectacular and consisted of a slow external rotation of the arm to relax the spasm of the subscapularis muscle (Fig. 12.20). When full external rotation had been achieved, the humeral head could be easily replaced. This method was considered to have been first described by Kocher in the 19th century until, in 1970, an Egyptian surgeon noted that some of the paintings on the pyramids depicted injuries occurring while they were being built, together with their treatment. One such illustration unmistakably demonstrated Kocher’s manoeuvre (Fig. 12.21). The unknown artist therefore preceded both Kocher and Hippocrates in his description of manipulative reduction. If only he had published his work in a reputable journal, he would have received the proper recognition for his discovery!
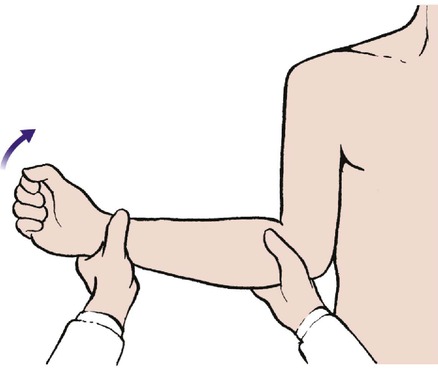 |
| Fig. 12.20
Kocher’s technique for reducing a dislocated shoulder.
|
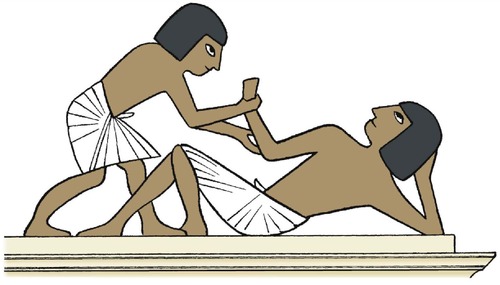 |
| Fig. 12.21
Original illustration of Kocher’s method in an Egyptian wall painting.
|
Aftercare. Whichever technique is used, the arm should be brought across the body and bandaged in that position for 3 weeks, when the shoulder can be mobilized. Treating without immobilization runs the risk of recurrent dislocation (p. 365).
Posterior dislocation
Posterior dislocations are much less common than anterior dislocations and are often caused by a direct blow to the shoulder in internal rotation or after an epileptic seizure. Posterior dislocation can become recurrent, particularly if the patient has generalized ligamentous laxity. Some patients can dislocate the shoulder posteriorly at will as a ‘party trick’.
Posterior dislocations often escape diagnosis and the lesion may be missed on the radiographs but the characteristic ‘light bulb’ appearance (Fig. 12.22), caused by internal rotation of the humerus, should suggest the diagnosis.
 |
| Fig. 12.22
Posterior dislocation of the humeral head with the ‘light bulb’ sign.
|
Treatment
Reduction is easily done by pulling the arm gently forwards and externally rotating it, but the reduction is often unstable. Aftercare is the same as for anterior dislocation.
Luxatio erecta
In exceptional circumstances, the humeral head becomes jammed below the glenoid with the arm pointing directly upwards, presenting a spectacular appearance sometimes mistaken for hysteria. This is a true inferior dislocation, in contrast to anterior dislocation in which the head only slips downwards after it has dislocated anteriorly.
The humeral head lies against the vessels and can cause ischaemia, and the rotator cuff is always damaged.
Treatment
Reduction can be difficult but once achieved immobilization is not required.
Fracture dislocations
Most fractures associated with dislocations of the shoulder involve the humeral head and are dealt with on page 197. The greater tuberosity may also be separated.
Rupture of the supraspinatus tendon
The supraspinatus tendon can be ruptured without a fracture. This injury is comparatively common in older patients with degenerate tendons and is usually seen in the orthopaedic clinic rather than an accident department, but sudden ruptures of the supraspinatus can also occur in young people after a violent injury.
Clinically, there is both bruising and tenderness around the supraspinatus muscle and weakness of abduction.
Treatment
Surgical repair is advisable in acute tears in young or active patients. Rehabilitation is prolonged.
Fractures of the upper end of the humerus
Avulsion of the greater tuberosity
The greater tuberosity, to which the supraspinatus tendon is attached, can be avulsed in a fall onto the shoulder in older patients. The fragment will usually unite in a good position but sometimes the supraspinatus tendon pulls it away from the bone. The fragment may then become wedged in the space between the acromion and the humeral head, obstructing shoulder movement (Fig. 12.23).
 |
| Fig. 12.23
Fragment of greater tuberosity with attached supraspinatus tendon caught in the joint between the humeral head and the acromion.
|
Treatment
Treatment is by support to the shoulder until the pain has settled, followed by physiotherapy 3–4 weeks later when the fragment has reattached. If the fragment is jammed in the joint, operation is needed to reduce and fix it.
Fractures of the surgical neck of the humerus
Fractures of the surgical neck occur in adults from a fall on the outstretched arm. The fractures can be displaced or impacted, stable or unstable, and are classified according to the site and number of the fragments.
Impacted fractures are more common and are visible as a line of dense bone on the radiograph (Fig. 12.24). Displaced fractures are less common but potentially more serious because the sharp bone ends can damage vessels or nerves. They may also go on to non-union and avascular collapse of the humeral head.
 |
| Fig. 12.24
Fracture of the humeral head with impacted fracture of the neck.
|
Treatment
Support to the limb in a sling or collar and cuff for 4–6 weeks, depending on the stability of the fracture, is often all that is required in undisplaced fractures. Mobilization can then be commenced and rehabilitation begun when pain allows.
Extensive bleeding and bruising around the fracture is usual but not of serious significance, though it may track down to the elbow and produce a spectacular discoloration. This should not delay mobilization.
Impacted fractures can be mobilized after 2 weeks, but the fragments can become disimpacted unless some protection is given until then.
Undisplaced or minimally displaced fractures almost always unite because the fracture is surrounded by muscle, and remodelling is good at the shoulder (Fig. 12.25). Fractures that are displaced or severely angulated may need operative intervention. In the young patient the fracture should be reduced and fixed with internal fixation. In the elderly it may be more judicious to proceed to a hemiarthroplasty, especially in four-part fractures (see Fig. 12.26).
 |
| Fig. 12.25
(a) Displaced fracture of the neck of the humerus; (b) the fracture remodelled well to give good function.
|
Proximal epiphyseal separation
Separation of the upper humeral epiphysis is a common injury in children and is one of the injuries seen in non-accidental injury.
Treatment
Treatment is by rest in a sling. In children under the age of 12 any deformity will correct by remodelling and manipulation is hardly ever required.
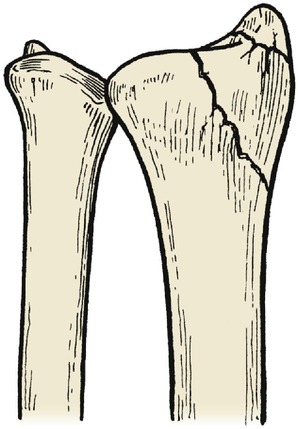
Fracture dislocations of the shoulder
Fractures of the humeral head with several fragments are usually accompanied by a dislocation (Fig. 12.26). Fracture dislocations of the humeral head present several problems:
1. The fragment may obstruct reduction and make open reduction necessary.
2. The reduction will be very unstable.
3. Soft tissue damage and haemorrhage into and around the shoulder lead to joint stiffness.
4. Avascular necrosis of the humeral head can follow fractures through the anatomical neck.
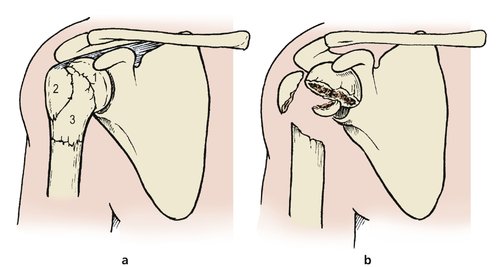 |
| Fig. 12.26
(a) Fracture sites at the humeral head: (1) fracture through the anatomical neck of the humerus; (2) fracture of the greater tuberosity; (3) fracture through the surgical neck of the humerus. (b) Four-part fracture of the humeral head.
|
Treatment
Closed reduction is difficult. Open reduction may be needed in younger patients but in older patients it is preferable to accept some loss of function and institute early movement.
Severe fracture dislocations may need prosthetic replacement of the humeral head.
Humeral shaft
Fractures of the humerus can be spiral, transverse, segmented or pathological.
Spiral fractures
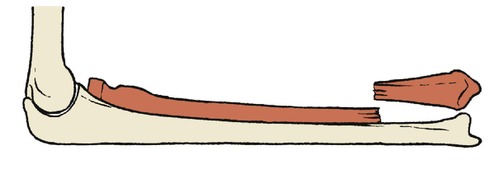
Twisting injuries of an arm produce a spiral fracture of the humerus (Fig. 12.27).
 |
| Fig. 12.27
Spiral fracture of the shaft of the humerus.
|
Transverse fractures
Transverse fractures of the humerus are caused by direct trauma or a fall onto the arm.
Pathological fractures
The humerus is a common site for metastases and pathological fractures are often seen.
Complications (Fig. 12.28)
Neurovascular damage
The fragments are shaped like spikes and can damage the radial nerve or the vessels, as well as muscle, as they wind around the bone.
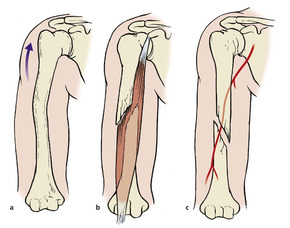 |
| Fig. 12.28
Complications of fractures of the shaft of the humerus. (a) Malunion caused by abduction of the proximal fragment. (b) Soft tissue interposition. The biceps is lying between the muscle fragments. (c) Neural damage. The radial nerve has become caught between the bone fragments.
|
Brachioradialis is a useful guide to neurological function. If there is a neurological deficit involving brachioradialis and no clinical or electrical sign of recovery after 6 weeks, the radial nerve should be explored. In the longer term, flexor tendons may need to be transferred to restore extensor function.
Malunion
Malunion may occur because the deltoid can abduct the upper fragment without opposition from other muscles or the weight of the arm.
Non-union
Soft tissue, including the radial nerve and triceps, can be caught between the bone ends and lead to non-union.
Treatment
Soft tissue usually holds the fragments in good position and conservative treatment is generally successful (Fig. 12.29). Either a U-slab or a hanging cast will protect the humeral shaft from additional trauma and, provided that it is supported by a collar and cuff and not a sling, the weight of the cast applies traction to the fracture site.
 |
| Fig. 12.29
Union of the spiral fracture shown in Figure 12.27, achieved with a hanging cast.
|
Some degree of malalignment is acceptable in the upper limb because it does not bear weight and because of the excellent range of glenohumeral motion. If the position is unacceptable, internal fixation with an intramedullary nail or plate is simple and straightforward.
If the fracture is in the distal humerus, brachialis may be pulled into the fracture line. Unless this problem is recognized and treated by open reduction, with or without internal fixation, the fracture will not unite.
For pathological fractures, internal fixation is effective and allows early mobilization and restoration of function.
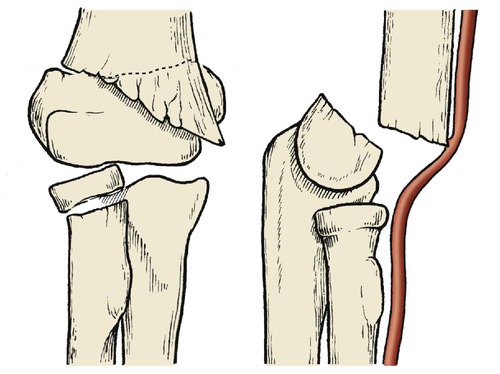
Fractures at the elbow (Fig. 12.30)
Supracondylar fracture of the humerus
Supracondylar fractures of the humerus occur in children who fall on the outstretched arm (Fig. 12.31). Treatment is difficult and the fracture is notorious for its complications.
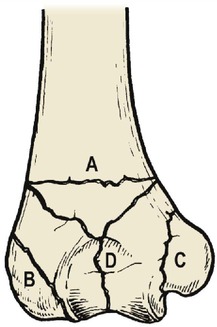 |
| Fig. 12.30
Fracture lines at the elbow: ( A) supracondylar fracture; ( B) lateral epicondyle; ( C) medial epicondyle; ( D) Y-shaped fracture.
|
 |
| Fig. 12.31
(a) Supracondylar fracture of the humerus. (b) The same fracture 5 months later showing union and early remodelling.
|
Complications
Complications of supracondylar fractures of the humerus in children
1. Vascular damage.
2. Compartment syndrome.
3. Volkmann’s ischaemic contracture.
4. Median nerve damage.
5. Malunion.
6. Myositis ossificans.
Vascular problems. At the moment of greatest displacement the distal fragment and the forearm are pushed backwards, pulling the brachial artery and median nerve violently against the sharp lower end of the upper fragment (Fig. 12.32). The circulation must therefore be checked carefully and recorded, with special attention to the five ‘P’s:
1. Pulselessness.
2. Pallor.
3. Pain.
4. Paraesthesiae.
5. Paralysis.
 |
| Fig. 12.32
Displacement in a supracondylar fracture of the humerus showing how the brachial artery can be damaged.
|
The skin will be cool if the circulation is interrupted and there will be loss of passive finger extension because of oedema in the flexor compartment. If these signs are present before or after reduction, the following steps should be taken:
1. The splint and dressings should be removed, down to skin.
2. The elbow should be extended slightly, even if this loses the reduction.
3. If the circulation still does not improve, the brachial artery must be explored at the elbow. If the artery is in spasm, it can be painted with papaverine to relax the smooth muscle of the arterial wall. If this is ineffective, as it almost always is, the artery must be opened, intimal tears corrected, and a vein patch applied if necessary.
Compartment syndrome. The median nerve and radial artery can both be compressed by swelling within the anterior compartment of the forearm. If there are paraesthesiae in the median distribution with loss of finger extension, a fasciotomy is probably needed.
Note: Compartment syndromes can occur even if the radial pulse is present!
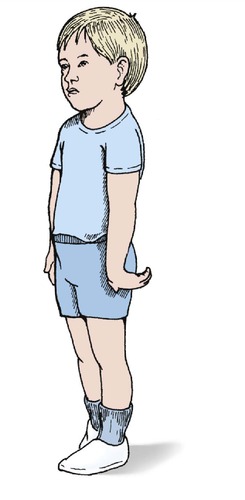
Volkmann’s ischaemic contracture is the end result of muscle necrosis caused by occlusion of the microcirculation from any cause. Untreated vascular insufficiency following a supracondylar fracture, perhaps aggravated by a compartment syndrome, is one cause. Masses of fibrous tissue replace patches of necrotic muscle in the flexor compartment and these contract, pulling the fingers into flexion and the wrist into flexion and pronation (Fig. 12.33). The result is disabling.
 |
| Fig. 12.33
The position of the hand in Volkmann’s ischaemic contracture.
|
Median nerve damage. The median nerve, like the brachial artery, is vulnerable at the fracture site. Because the nerve is tough it is seldom divided and function usually recovers. The anterior interosseous branch to the deep muscles is more likely to be affected than the superficial branch, which continues as the median nerve into the hand.
Malunion. Unless a good position is achieved, an unsightly malunion is likely, with the medial epicondyle pushed backwards and medially. The result is, at best, a slight loss of carrying angle, and at worst a ‘gunstock’ deformity (see Fig. 2.16). Corrective osteotomy may be required when growth is complete.
Myositis ossificans can follow any fracture in the region of the elbow, including a supracondylar fracture.
Treatment
Undisplaced fractures can be treated in a backslab with the elbow flexed for 3 weeks. Unstable fractures are more difficult. The fractured surfaces are small and do not ‘fit’ together neatly. The distal fragment has many powerful muscle groups attached to it, which can displace the fragments after reduction.
Reduction is achieved by a gentle longitudinal pull with the forearm in the midprone position. Once reduced, the elbow is flexed beyond a right angle, a plaster backslab applied and the arm supported in a collar and cuff. This position can usually be maintained but if flexing the elbow beyond 90° interferes with the blood supply it must be extended until the pulse returns. If this loses reduction, the arm should be suspended and Dunlop traction (Fig. 12.34) applied.
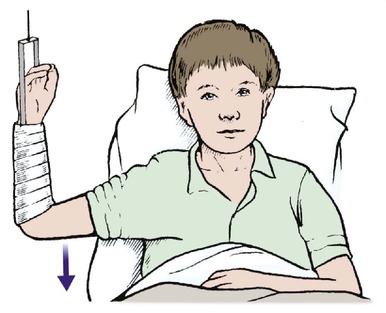 |
| Fig. 12.34
Dunlop traction for supracondylar fracture of the humerus.
|
Percutaneous ‘K’ wiring or open fixation with wires may be needed, not only to reduce difficult fragments but also to hold them in the reduced position. These wires can be removed after 3–4 weeks.
Medial epicondyle
In children, the medial epicondyle and its growth plate can be pulled off the humerus by valgus forces. The fracture is made more treacherous because it happens before the epicondyle has ossified; unless the radiographs of the two elbows are compared carefully, the lesion may be missed. The fragment can also be pulled into the joint space, where it interferes with joint movement.
Untreated, the fragment usually joins with fibrous tissue, but function may be good.
Complications (Fig. 12.35)
Ulnar nerve palsy. The valgus strain that causes the fracture can also stretch the ulnar nerve.
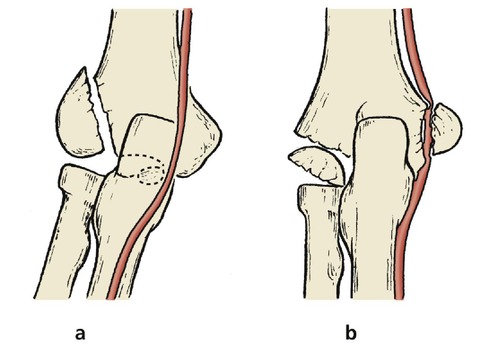 |
| Fig. 12.35
Fracture of the epicondyle: (a) the capitellum may be completely displaced; (b) complications include a fragment of medial epicondyle caught in the medial joint space, non-union of the capitellum and tardy ulnar palsy.
|
Growth arrest. If the growth of the epicondyle is impaired or the fracture is not reduced, a varus deformity at the elbow (cubitus varum) follows.
Treatment
The fragment should be accurately reduced, openly if necessary, and secured with a Kirschner wire for extra stability. The wire must be removed later.
Lateral condyle
Avulsion of the lateral condyle is commonest between the ages of 3 and 5. If the fragment is small and involves just the capitellum, it may turn through 180° and make closed reduction impossible.
Complications
If the fragment does not unite, or there is growth arrest from damage to the epiphyseal plate or malunion, a valgus deformity of the lower end of the humerus follows. This stretches the ulnar nerve and causes a tardy ulnar palsy (p. 387). Non-union can occur, even if the fragment is undisplaced, and the injury must always be taken seriously.
Treatment
The fragment should be accurately reduced, by manipulation if possible, but open reduction may be necessary to replace the fragment and hold it with a Kirschner wire.
Pulled elbow
If children under 4 years of age are lifted by their hands the radial head can slip partly out of the annular ligament. The child will experience pain, will not use the arm, and the radiographs will be normal.
Treatment
The subluxation can be reduced by longitudinal pressure of the radius against the humerus with the elbow flexed. The forearm can then be alternately pronated and supinated and the radial head will pop back into position with dramatic relief of pain.
Fractures into the elbow joint
The lower end of the adult humerus can be fractured by direct trauma to produce a comminuted fracture that enters the elbow joint.
Complications
Like any fracture involving a joint, this injury is followed by loss of joint movement and late osteoarthritis.
Treatment
Exact anatomical restitution is not required unless there is gross displacement of the fragments. Conservative management with early mobilization may produce a better result than open reduction and internal fixation.
If there is gross displacement of the fragments with complete disintegration of the elbow it may be necessary to reassemble the bones and fix them internally (Fig. 12.36). The operation is difficult and the results are not always good.
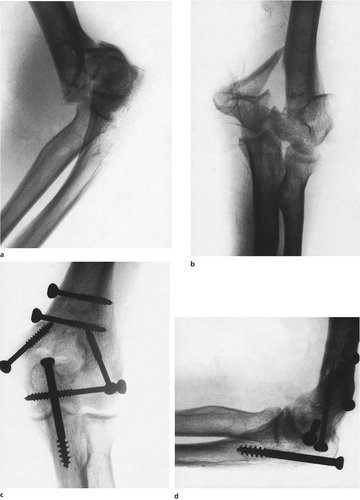 |
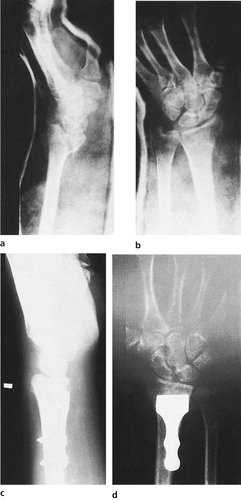
| Fig. 12.36
Comminuted fracture of the lower end of the humerus: (a), (b) position of the fragments; (c), (d) position after internal fixation.
|
Dislocations of the elbow
Although the elbow is a mechanically stable joint, it can be dislocated by a fall on the outstretched arm in almost full extension (Fig. 12.37). The lower end of the humerus will then slide forward over the coronoid process, which may be fractured (Fig. 12.38).
 |
| Fig. 12.37
Anterior dislocation of the elbow.
|
 |
| Fig. 12.38
(a), (b) Anterior dislocation of the elbow.
|
Complications
Joint stiffness. Full restoration of movement is unusual and a permanent loss of 15–20° of extension is almost inevitable.
The fragment can be removed and some movement restored, but the operation is technically difficult and the bone can reappear.
Recurrent dislocation can occur but is very rare.
Treatment
The dislocation can be reduced by a longitudinal pull in slight flexion and the reduction is usually stable. The arm should be rested in a collar and cuff for 2 weeks and mobilized gently.
Olecranon
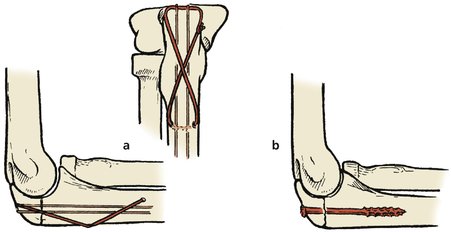
The olecranon is easily fractured in direct falls onto the point of the elbow because the lower end of the humerus acts like a chisel and splits the olecranon at its narrowest point (Fig. 12.39). Avulsion injuries due to the pull of the triceps muscle are also common.
 |
| Fig. 12.39
(a) Displaced fracture of the olecranon; (b) the position after tension band wiring.
|
Treatment
Unless the fragments are undisplaced, which is unusual, internal fixation is needed, using either a screw or tension band wiring (Fig. 12.40). Rigid splintage is unnecessary if the fixation is secure.
 |
| Fig. 12.40
Methods of fixation of fractures of the olecranon: (a) tension band wiring; (b) screwing.
|
Comminuted fractures in which the fragments cannot be reassembled and fixed can be treated by excision of the olecranon, especially in the elderly.
Injuries to the radius and ulna
Fractures of the radial head and neck
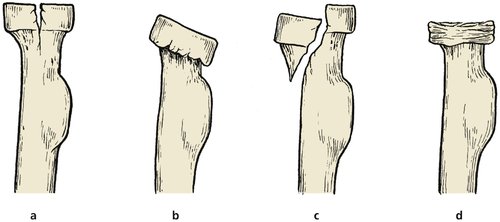
The radial head is easily fractured by a fall onto the outstretched arm and three main types of fracture are seen (Fig. 12.41).
 |
| Fig. 12.41
Types of fracture of the radial head: (a) vertical split; (b) tilt; (c) shear fracture; (d) crush.
|
Treatment
Treatment varies according to the type of fracture.
Undisplaced fractures and those with little displacement need blood aspirating from the joint, a soft supporting bandage and early mobilization.
Displaced fractures through the radial neck with more than 30° of angulation cause a painful restriction of pronation and supination if left untreated. The displacement should be corrected, by open reduction if necessary.
Comminuted fractures. Grossly displaced or comminuted fractures of the radial head are best treated by radial head excision and early mobilization. Prosthetic replacement of the radial head has been tried but excision is usually preferred.
Dislocation of the radial head with fracture of the ulna (Monteggia fracture)
Dislocation of the radial head accompanied by a fracture of the ulna is called a Monteggia fracture. It is a trap to catch the unwary (Fig. 12.42). Unless both components of the injury are recognized, which is not always easy, one of them will go untreated and a bad result will follow. Before treating a dislocated radial head or fractured ulna, always check that it is not one half of a Monteggia fracture.
 |
| Fig. 12.42
Monteggia fracture.
|
If the ulnar fracture is very high, near the elbow joint, it may be mistaken for a fractured olecranon (Fig. 12.43). The consequences of this error can be very serious indeed.
 |
| Fig. 12.43
(a), (b) A high Monteggia fracture which was treated like a fractured olecranon with a tension band wire. The position is poor: a plate would have been better.
|
Treatment
The ulnar fracture is so unstable that it must be internally fixed. Conservative treatment may succeed in children but the position must be checked frequently to be certain that the fragments have not slipped.
Fracture of the radius and ulna
The radius and ulna are easily broken by a twisting injury. The fracture line separates the pronators from the supinators. Both muscle groups act unopposed and produce a nasty rotational deformity that is easily missed on a two-dimensional radiograph, which shows only the angulation and length of the bones but not their rotational relationship. If rotation is present, the radiographs will show a lateral view of the elbow and an anteroposterior view of the forearm on the same film and this sign should be looked for specifically (Fig. 12.44).
 |
| Fig. 12.44
Fracture of the radius and ulna to show displacement. This is a greenstick fracture and some bony continuity remains.
|
Complications
Complications are common after fractures of the radius and ulna.
Malunion. Unless the rotational deformity is corrected, a malunion will follow and the patient will be unable to supinate the forearm, which makes it difficult to wash the face or collect change when shopping.
Compartment syndromes and vascular damage are common.
Non-union is common, particularly if rotation has not been controlled.
Cross-union. Some fractures unite with cross-union between the two bones, which makes pronation and supination impossible.
Treatment
These fractures are so unstable that conservative treatment is seldom successful in adults, and internal fixation may even be required in children to achieve stability.
Conservative. A well applied cast can sometimes correct and hold the rotational deformity by bringing the distal fragment round to meet the proximal, which is held in unopposed supination. The cast must include both the upper arm and the hand, which is held in supination, but in this position the longitudinal position may slip and open reduction is then required.
Operative. Open reduction and internal fixation is the treatment of choice for most of these fractures (Fig. 12.45) but external fixation is needed if the wounds are contaminated. Plates and screws or intramedullary nails are generally used.
 |
| Fig. 12.45
Plating of a fracture of the radius and ulna.
|
Isolated fracture of the ulna
The subcutaneous margin of the ulna is vulnerable to direct trauma and easily cracked by a direct blow when protecting the face from an impact or from missiles such as cricket balls.
Treatment
Treatment varies according to the amount of displacement.
Undisplaced fractures. Although these fractures look deceptively straightforward on the radiograph, they should be treated with great suspicion and immobilized in a full arm cast with the elbow flexed. If this is not done the fracture will be exposed to rotational stresses and non-union can follow.
Displaced fractures. The rotational element makes displaced fractures almost impossible to immobilize and they are best treated by internal fixation with a plate.
Isolated fracture of the radius
The radius can be fractured by direct trauma. Because the radiohumeral joint reduces rotational strains on the fracture, non-union is less common than in isolated fractures of the ulna.
Treatment
Treatment varies according to the amount of displacement.
Undisplaced fractures. Although these fractures look deceptively straightforward on the radiograph, like isolated fractures of the ulna, they should be treated with great suspicion and immobilized in a full arm cast with the elbow flexed.
Displaced fractures. The rotational element makes displaced fractures difficult to immobilize and they are best treated by internal fixation.
Fractured radius with dislocation of the distal radioulnar joint (Galeazzi fracture)
A fall on the outstretched hand can cause an isolated fracture of the radius with subluxation of the inferior radioulnar joint (Fig. 12.46). This is a Galeazzi fracture and is quite different from a Colles’ fracture (p. 213).
 |
| Fig. 12.46
Galeazzi fracture.
|
In many ways, the Galeazzi and Monteggia fractures are mirror images. The Monteggia involves dislocation of the superior radioulnar joint and fracture of the ulna, the Galeazzi a fracture of the radius and dislocation of the inferior radioulnar joint. Both slip after an initial good result, both are mistaken for other fractures, and both may need internal fixation. Beware of both!
The reason for the similarity is simple: if one forearm bone shortens, the other can only support it if it is stable, and in both fractures the ‘intact’ bone is dislocated at one end.
Complications
Malunion is common. Because the distal fragment has no longitudinal stability, the fracture is unstable and is notorious for slipping in plaster after an initial good position.
Treatment
The fracture is best treated by internal fixation of the radius (Fig. 12.47). It must not be treated in a short forearm cast as if it were a Colles’ fracture, for which it may be mistaken.
 |
| Fig. 12.47
A Galeazzi fracture: (a) before internal fixation; (b) after fixation with a plate and screws.
|
Monteggia versus Galeazzi
• Monteggia – fractured ulna, dislocated proximal radioulnar joint.
• Galeazzi – fractured radius, dislocated distal radioulnar joint.
• Beware of both!
Crush injuries of the forearm
The forearm is frequently crushed between heavy objects or rollers. Even if no bone is broken, these injuries are serious because of soft tissue swelling inside the closed fascial compartments of the forearm.
Treatment
The arm must be elevated, the circulation watched carefully and any loss of extension of the wrist and fingers treated seriously. If in any doubt, a wide fasciotomy of the fascial compartment of the forearm is needed to prevent the complications of a compartment syndrome.
Fractures at the lower end of the radius
Colles’ fracture
The Colles’ fracture, described by Abraham Colles (1773–1843), who was Professor of Surgery in Dublin, is probably the commonest fracture seen in fracture clinics and general practice (Fig. 12.48).
 |
| Fig. 12.48
(a), (b) Colles’ fracture.
|
The fracture that Colles described:
1. Was within 1 inch (2.5 cm) of the wrist joint.
2. Had dorsal angulation of the distal fragment.
3. Had dorsal displacement of the fragment.
4. Was associated with a fracture of the ulnar styloid.
Colles’ fracture is most often caused by a fall on the outstretched arm in patients over 50, usually women.
Deformity. The obvious deformity of a Colles’ fracture is the classical ‘dinner fork’ of backward angulation but the deformity has five separate elements (Fig. 12.49):
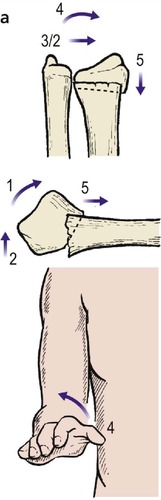 |
 |
| Fig. 12.49
(a) Displacement of the fragments in a Colles’ fracture. (b) The ‘dinner fork’ deformity of Colles’ fracture.
|
1. Backward angulation.
2. Backward displacement.
3. Radial deviation.
4. Supination.
5. Proximal impaction.
In gross deformities the distal radioulnar joint may be dislocated.
Complications
Complications are regrettably frequent after such a common and apparently straightforward injury. Most complications occur not from neglect, but simply because there is no treatment that is truly effective.
Complications of Colles’ fracture
• Sudeck’s atrophy.
• Median nerve injury.
• Rupture of extensor pollicis longus.
• Malunion.
Sudeck’s atrophy. The hand becomes stiff, blue and cold in this variety of reflex sympathetic dystrophy, caused by a disturbance of the sensory and the autonomic supply of bone and blood vessels. The condition is particularly common if the patient is allowed to rest the hand without moving the fingers and can be prevented by ensuring that the patient keeps the fingers moving. Sometimes the condition involves the shoulder as well and is then called the ‘shoulder–hand syndrome’.
Treatment is difficult and requires much patience, physiotherapy and reassurance. Because of this fearful complication, it is vitally important to ensure that the patients really do keep their fingers and shoulder moving after a Colles’ fracture.
Median nerve damage. The median nerve runs right across the site of a Colles’ fracture and may be compressed by the bruising and bleeding around it. Median nerve symptoms usually settle by the time the fracture is united but decompression is sometimes required.
Rupture of the extensor pollicis longus tendon. The extensor pollicis longus tendon runs across the fracture site at the dorsum of the wrist and may be worn through by movement across the sharp edge of the broken bone, producing an ‘attrition rupture’.
The problem is also seen in fractures with very slight displacement and may be due to ischaemia rather than attrition. If a patient reports that the thumb has dropped following a Colles’ fracture, the tendon has ruptured and must be repaired.
Malunion. Because the fracture is unstable and the bone is crushed, malunion is common (Fig. 12.50). The disability from a malunion is unpredictable and many patients manage well despite a marked and unsightly deformity.
 |
| Fig. 12.50
Typical malunion of a Colles’ fracture, with shortening of the radius, backward angulation and radial rotation of the radial fragment and non-union of the ulnar fragment.
|
Treatment
Left untreated, the fracture will unite with backward angulation, a loss of supination, weakness of grip and loss of ulnar deviation. The functional result is often surprisingly good.
Displaced fractures. The fracture can be manipulated into good position by pulling the hand distally to disimpact the fracture, flexing the wrist and pulling the hand round into ulnar deviation. Reducing the fracture in this way is easy but holding the position is not. Because the fragment is impacted, the bone on the dorsum of the radius is crushed and a hole is left in the dorsum of the radius when the fracture is reduced. This leaves the distal fragment unsupported dorsally and the deformity recurs as the swelling subsides.
Once reduced, a plaster is applied from the elbow to the metacarpophalangeal joints, which lie in the line of the proximal skin crease in the palm and not at the base of the fingers. The fingers and the thumb must be left free so that they can move freely.
The fracture should be inspected the next day to be sure that there is no undue swelling and that the patient is moving the fingers, arm and shoulder.
The patient is then seen between 7 and 10 days later and a radiograph taken to check the position. If the fragments have slipped, a further manipulation may be required. If the patient is not using the hand and shoulder at this stage, physiotherapy should be instituted at once.
The cast is retained for a total of 4 weeks, by which time there should be full movement in the fingers, thumb, elbow and shoulder. Physiotherapy or occupational therapy may be needed if the patient is reluctant to use the hand.
Impacted fractures in good position. A fracture will sometimes impact in acceptable position with little backward angulation. Such fractures need not be manipulated, but it is wise to apply a cast for 2 weeks to prevent accidental displacement.
Operations for malunion
Operation is sometimes needed to restore supination, or to relieve pain. Three procedures are available:
1. Baldwin’s procedure, in which a 2 cm long segment of ulna is excised with its periosteum, leaving the distal 2 cm of the ulna intact. This allows the head of the ulna to move proximally and improves supination as well as the appearance of the wrist.
2. Excision of the lower end of the ulna improves the appearance but disturbs the stability of the wrist.
3. Corrective osteotomy is a more extensive procedure, sometimes needed if backward angulation of the radius is the main problem.
Colles’ fracture in children
Do not make the diagnosis of a Colles’ fracture in a child; it does not occur. If a ‘dinner fork’ deformity is present, the likely diagnosis is a fracture separation of the radial epiphysis or a greenstick fracture of the radius at its distal end (p. 219) (Fig. 12.52).
 |
| Fig. 12.52
(a), (b) Fracture of the lower end of the radius in a child.
|
Fractures of the radial styloid
The radial styloid can fracture in falls on the outstretched arm and this is commoner in the firm bone of young adults than the soft bone of the elderly (Fig. 12.51). The fracture usually heals well without lasting disability. The size of the fragment and the degree of displacement vary.
 |
| Fig. 12.51
Fractures of the radial styloid.
|
Treatment
The majority of these fractures need no reduction and a cast for 4 weeks is enough. Large displaced fragments must be reduced and internally fixed if manipulation is unsuccessful.
Fractures of the lower end of the radius and ulna
Transverse fractures across one or both bones of the forearm, with backward angulation, are seen after falls on the outstretched arm in young patients (Fig. 12.53).
 |
| Fig. 12.53
(a), (b) Impacted fracture of the lower end of the radius with minimal displacement.
|
Treatment
Manipulative reduction is usually easy and a cast for 4 weeks is sufficient. If the fracture is impacted with minimal displacement, 2 weeks immobilization is sufficient, provided that the patient is careful to avoid stressing the fracture for a further 4 weeks.
Smith’s fracture and Barton’s fracture
Colles’ successor in the post of Professor of Surgery at Dublin was R.W. Smith, who is said to have performed the post-mortem examination on his predecessor. Smith also described the fracture of the lower end of the radius now known as a Smith’s, or reverse Colles’ fracture (Fig. 12.54a), which occurs if the victim lands with the wrist in flexion. Smith’s fracture is very unstable and will cause a disabling flexion deformity at the wrist if not treated correctly.
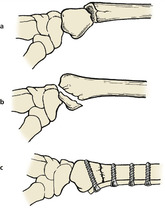 |
| Fig. 12.54
(a) Smith’s fracture; (b) Barton’s fracture, which enters the joint; (c) internal fixation of Smith’s fracture.
|
In some patients, the fracture line enters the joint so that the anterior lip of the radius is displaced proximally with the hand (Fig. 12.54b). This is not a Smith’s fracture but a Barton’s fracture, first described by John Rhea Barton of Philadelphia, a founding father of American orthopaedic surgery.
Treatment
Both these fractures must be distinguished carefully from a Colles’ fracture and treated in a forearm cast with the hand supinated and the wrist in full extension. If a good position cannot be achieved and maintained, the fracture must be reduced openly and secured with a small buttress plate attached to the volar aspect of the radius (Fig. 12.55).
 |
| Fig. 12.55
Internal fixation of Barton’s fracture: (a), (b) position before operation. The hand is in full extension but the position cannot be controlled; (c), (d) the position is satisfactory after insertion of an Ellis plate.
|
If this is not done, a disabling malunion and flexion deformity follows and arthrodesis may be needed.
Fractures in children
Epiphyseal separations
Fracture separations of the epiphyses occur only in children and must be reduced carefully if serious deformities are to be avoided (Fig. 12.56).
 |
| Fig. 12.56
Anteroposterior and lateral view of a type 2 Harris and Salter fracture separation of the lower radial epiphysis with a fracture of the ulnar styloid.
|
The injuries occur at the wrist, elbow and shoulder. Any injury can cause a fracture separation but they can be caused by a child being swung or thrown by the arms. If a child has more than one such fracture, the possibility of non-accidental injury should be considered.
Complications
Epiphyseal arrest is the principal complication of epiphyseal injuries but aseptic necrosis of the epiphysis is also seen.
Treatment
Accurate reduction and great gentleness are required. Closed reduction is usually successful but, if the epiphysis is fractured as well as dislocated, open reduction may be needed.
Greenstick fractures
Greenstick fractures occur only in childhood and are a mixed blessing. Although bony continuity is maintained and a good result can be expected, the fracture cannot be manipulated into perfect position because the bone springs back slightly. The similarity to a ‘green stick’ is close (p. 99).
Complications
The appearance of a greenstick fracture after removal from the cast can be alarming to the parents. The arm is not entirely straight and the parents need firm reassurance that this is normal and that the limb will remodel. Angular deformities of up to 30° in the plane of the nearest joint usually remodel perfectly but rotational deformities do not.
Treatment
If both cortices are buckled but intact, a light protective plaster for 2–3 weeks is all that is needed. These fractures cannot be manipulated into perfect position and some imperfection must be accepted.
It is impossible to overcorrect a greenstick fracture, even with three-point pressure. Provided the child does not fall again before the fracture is solid, an excellent result will be achieved whatever is done.
If one cortex is broken, a deformity can develop and correction may be needed. The cast should be retained for 3 weeks.