Chapter 11. Injuries to the trunk
Rib fractures
The severity of rib fractures depends on their number and stability. Multiple fractures which interfere with breathing have serious complications, but isolated cracks can usually be treated as severe bruises.
Isolated fractures
Fractures of a single rib can follow a direct blow or, in elderly patients, a fit of violent coughing. At the moment of fracture the patient feels sudden pain in the chest followed by pain on deep inspiration. On examination, there is well localized tenderness at the fracture site and pain on ‘springing’ the ribs.
It is most unwise to reassure patients that their ribs are intact just because the radiographs do not show a fracture. Radiographs only show the fracture if the X-ray beam catches it at exactly the right angle, which is rare, and for practical purposes clinical signs are more reliable than radiographs in the first week after injury.
After 2 weeks, the fracture can be recognized more easily by the rarefaction of the bone ends and callus around the fracture.
Treatment
Isolated fractures seldom require active treatment and can be regarded as ‘a bad bruise’. Untreated, they are very painful for 10–14 days and moderately painful for a further 4 weeks. By 8 weeks from injury they should be pain-free, when the callus can be felt as a firm bony swelling at the fracture site.
Analgesics are essential in the first few days and an intercostal block with local anaesthetic is sometimes needed. Breathing is painful without analgesia, chest movement is limited, the underlying lung develops atelectasia, secondary infection can follow and the patients may die if they are infirm.
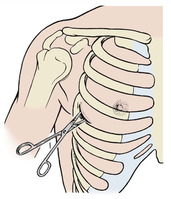
Strapping the chest. Once the standard treatment for all fractured ribs (Fig. 11.1), strapping relieves pain by restricting rib movement. Today, strapping is indicated only for robust, hard-working individuals who wish to get on with their job and pretend that the injury never happened.
 |
| Fig. 11.1
Strapping for broken ribs.
|
In dire emergencies, such as the battlefield, a pad bandaged over a flail segment reduces its excursion and minimizes the interference with inspiratory volume. A pad and bandage is also helpful if there is a penetrating wound of the pleura because it closes the opening into the pleural space.
Although valuable as an emergency measure, strapping is not good long-term treatment. Restricting thoracic movement and relying on diaphragmatic movement alone for breathing leads to lobar collapse, which predisposes to chest infection and creates further respiratory difficulties. Definitive treatment is therefore determined by the type of fracture and the stability of the chest.
Multiple fractures
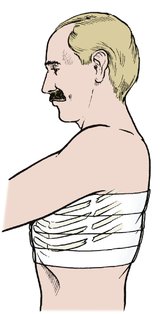
Flail chest. The main function of the ribs is to act as a moving cage to suck air into the lungs as it is elevated by the chest musculature. If this rigidity is lost and part of the chest wall is free to move independently of the rest of the thorax, it will be sucked inwards when the patient attempts to inhale and blown outwards on exhalation (Fig. 11.2). This is ‘paradoxical respiration’; it dramatically reduces tidal volume and can cause respiratory failure.
 |
| Fig. 11.2
A flail chest with paradoxical respiration. An unsupported segment of chest with ribs broken at each end moves inwards during inspiration and outwards during expiration.
|
Flail segments are commonly caused by a direct blow to the chest rather than by a crushing injury. A blow from a horse’s hoof produces a circular flail segment about 15 cm across, and a blow to the sternum from a steering wheel can fracture all ribs on both sides to produce a flail segment that includes the mediastinum.
Crushed chest. If a chest is crushed, there will be fractured ribs on both sides of the chest. Because it is difficult to fracture more than three ribs on one side of the chest and leave the other side intact, the presence of more than three fractures on one side of a crushed chest usually means that there are fractures on the other side as well, whatever the radiographs show.
A crushed chest does not usually have paradoxical movement but pain from the fractures interferes seriously with breathing and this can also cause respiratory failure.
Treatment
Treatment of multiple rib fractures depends upon their stability.
Stable fractures. Provided the rib cage is stable and there is no flail segment, inspiration is possible. Treatment is then similar to that of an isolated fracture, but more energetic. The pain is more severe, areas of tenderness are more numerous, inhibition of inspiration is more marked and breathing and movement are more painful. Stronger analgesics or intercostal nerve blocks may be required to make breathing comfortable.
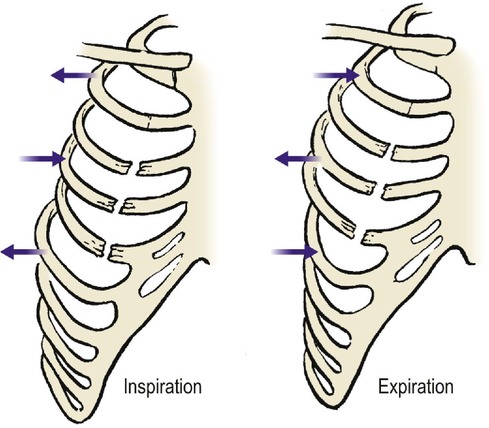
Unstable fractures. Unstable flail segments are best treated by positive pressure ventilation so that the ‘bellows’ function of the chest is disregarded and the chest inflated like a paper bag (Fig. 11.3). Strapping the flail segment is useful until the patient reaches hospital. Positive pressure ventilation can be instituted and, if necessary, maintained by tracheostomy for 2 or 3 weeks until the chest wall is stable.
 |
| Fig. 11.3
Positive pressure respiration. If there are multiple rib fractures, the chest may be inflated passively like a paper bag.
|
The decision to ventilate a patient is made in conjunction with the thoracic surgeons and anaesthetists and the patient is best managed in the intensive therapy unit.
Pathological fractures
The ribs are a common site for metastatic deposits and pathological fractures are common. Suspected rib fractures deserve radiological examination, even though they are often undetectable.
Injuries to the costal cartilages
The costal cartilages are softer and more flexible than ribs but can be fractured by direct violence. The clinical features are similar to those of an isolated rib fracture but the pain is less severe.
The joints between the costal cartilages of the false ribs can also be injured and dislocations of these joints produce pain and tenderness which can be very slow to resolve.
Treatment
Injection with hydrocortisone acetate is sometimes helpful.
Fractures in the elderly
In the elderly, the pain from rib fractures impairs respiratory function. Pain relief in these patients is particularly important and local infiltration of the fracture with local anaesthetic or an intercostal nerve block may be required.
Injuries involving the pleural cavity
There are three types of pneumothorax (Fig. 11.4):
1. Closed
2. Open
3. Tension.
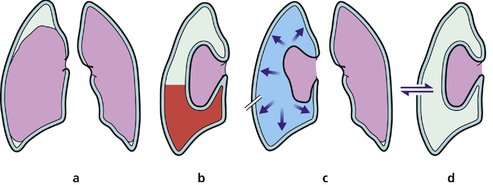 |
| Fig. 11.4
Types of pneumothorax: (a) simple pneumothorax; (b) haemopneumothorax; (c) tension pneumothorax; (d) open pneumothorax.
|
If lung and pleura are damaged, a pneumothorax, haemothorax or chylothorax may follow.
Closed pneumothorax
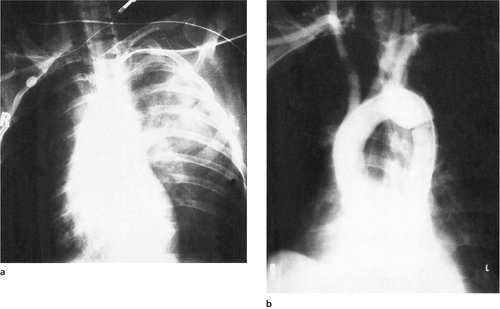
Most pneumothoraces consist of nothing more than a little air in the pleural cavity which will be absorbed in a few days (Fig. 11.5). Because the air in the pleural space floats upwards, a pneumothorax cannot be seen on an anteroposterior radiograph unless the patient is standing or sitting upright, when it is seen above the clavicle.
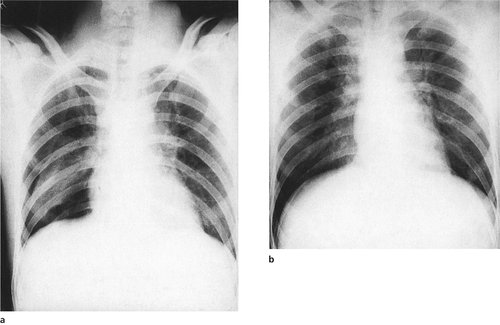 |
| Fig. 11.5
Simple pneumothorax: (a) marked collapse and (b) very slight collapse of the right lower lobe.
|
If the pneumothorax is small, the only evidence may be the absence of lung markings at the apex. If a standing or sitting radiograph is not possible, a lateral radiograph may show air lying against the lateral wall of the chest.
Treatment
A pneumothorax occupying more than 25% of the hemithorax causes respiratory embarrassment and draining may be needed, using a catheter attached to an underwater seal.
Open pneumothorax
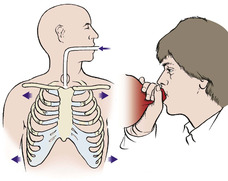
If the skin and parietal pleura are broken, the pleural space will communicate with the outside air, which will be sucked in and out of the chest on inspiration and expiration. Respiratory embarrassment follows unless the opening is closed. Infection is an additional risk but is unusual if the lung can be kept expanded and the pleural space obliterated.
Treatment
As first aid, a pad can be placed over the opening, or the patient simply laid with the wound downwards until a chest drain can be inserted. It is not necessary to close the wound unless it is large or contaminated.
Tension pneumothorax
If the opening into the pleura is oblique it can work like a flap valve and allow air into the pleural cavity on inspiration but will not let it out on expiration (Fig. 11.6). The pleural space will then be inflated under pressure, the lung will collapse and the mediastinum will shift to the opposite side. Unless treated promptly, the patient will die within minutes. This is a tension pneumothorax.
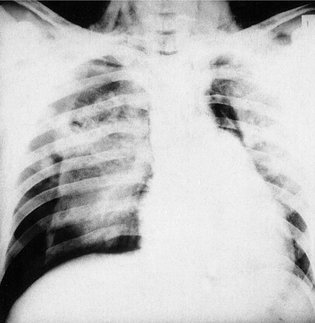 |
| Fig. 11.6
Bilateral pneumothorax with tension pneumothorax on the right side. Note the surgical emphysema in the neck.
|
If there is a rib fracture as well, the air will be forced out through the fracture site into the subcutaneous tissues to produce surgical emphysema, which can extend over the whole of the chest wall and into the neck (Fig. 11.7). A similar appearance is also seen after vigorous positive pressure ventilation of patients with fractured ribs.
 |
| Fig. 11.7
Massive surgical emphysema caused by rupture of a main bronchus.
|
Treatment
In patients with a tension pneumothorax the insertion of a chest drain is a life-saving procedure. A pneumothorax or chest drain pack is available in all accident departments and every doctor likely to be exposed to such a patient should know how to use it.
Emergency treatment of tension pneumothorax
1. Make a short skin incision in the fourth rib space (i.e. between the fourth and fifth ribs) in the midaxillary line on the side of the pneumothorax (Fig. 11.8).
 |
| Fig. 11.8
Site of drainage of a tension pneumothorax at the fourth intercostal space in the midaxillary line. Keep the scissors close to the upper border of the lower rib.
|
2. Dissect right down through the intercostal muscles and pleura with scissors. Open the scissors widely to release air. The hiss of air will be felt and heard and the patient will improve dramatically.
3. Pass a chest drain through the incision and into the pleural cavity. The situation is then under control.
4. Secure the drain to the patient and connect it to an underwater seal or valve.
To push a pair of sharp scissors into a patient’s chest may seem hazardous, but in a patient with a tension pneumothorax the vital structures are pushed well away from the point of entry. There is no time for a radiograph to confirm which side of the chest is involved but this is obvious clinically because the affected side contains so much air that it is tympanitic to percussion.
Haemothorax
Bleeding into the pleural cavity will produce a more gradual deterioration than a pneumothorax. The pulse rate rises, blood pressure falls and the chest is dull to percussion; the diagnosis can be confirmed radiologically.
Treatment
Treatment is by drainage as described, or if the bleeding cannot be controlled then a thoracotomy may be required to stop the bleed.
Chylothorax
Damage to the thoracic duct can cause chyle (lymph) to run into the pleural cavity, producing a chylothorax, which causes a steady deterioration.
Treatment
Treatment is difficult and may require the attention of the thoracic surgeons to close a thoracic duct leak, but many heal spontaneously with tube drainage and parenteral nutrition. Healing may take several weeks and the patient must take nothing by mouth during this time.
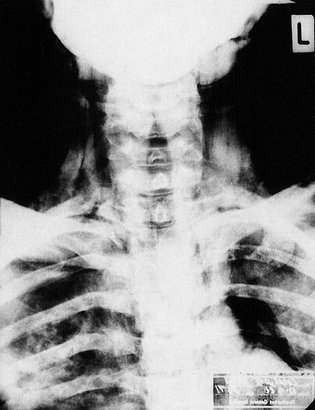
Injuries to the mediastinum
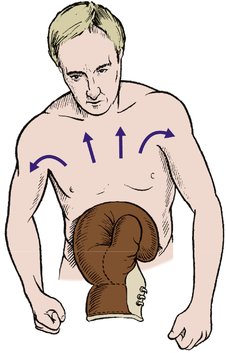
The steering column of every car is aimed liked a spear at the heart of the driver and injuries to the mediastinum are a common cause of death. Despite collapsible steering columns, steering wheels contoured to fit the thorax (Fig. 11.9) and adequate seat-belts worn correctly, rapid deceleration from a head-on collision can still force the steering wheel back against the chest. The result may be a fracture of the sternum and the ribs attached to it, or rupture of the heart, aorta, a main bronchus and occasionally the oesophagus. More recently, cars fitted with ‘air bags’ have become more popular. When inflated these reduce the risk of direct damage to the anterior chest as well as the head and neck.
 |
| Fig. 11.9
Effect of not wearing a seat-belt. The head strikes the windscreen, the neck is hyperextended and the steering column is driven into the precordium.
|
Aortic and cardiac rupture
Rupture of the heart is usually so rapidly fatal that it need concern neither the casualty officer nor the orthopaedic surgeon. A laceration or rupture of the aortic arch may leak into the mediastinum over a period of days or suddenly increase and cause exsanguination. The usual site of aortic rupture lies just distal to the left subclavian artery at the junction where the fixed and mobile parts of the aorta meet (Fig. 11.10).
 |
| Fig. 11.10
(a) Widened mediastinum. (b) Complete transection of the aorta demonstrated by aortography. The blood is contained by the adventitia only.
|
To diagnose this serious injury, the width of the mediastinum should be noted on a radiograph (taken at 1.8 m) of every patient who has suffered a blow to the chest, particularly drivers.
Not all injuries to the heart are so serious. Cardiac contusion may cause arrhythmias, and valves can be ruptured, causing murmurs which can be heard.
Treatment
If there is any widening of the mediastinal shadow it must be assumed that this is due to haemorrhage into the mediastinum and the opinion of a thoracic surgeon obtained as a matter of urgency. A CT scan or arch arteriogram may be needed to demonstrate the lesion.
Fracture of the sternum
Fracture of the sternum can be caused either by direct trauma, which requires extreme force and is usually associated with other injuries, or by violent flexion of the thoracic spine accompanied by a wedge fracture of the thoracic spine.
Fractures of the sternum are not serious in themselves and usually unite soundly, but their presence should alert the doctor to the possibility of a more serious injury. A flail segment including the mediastinum may be difficult to control, even by positive pressure respiration (see Fig. 11.3).
Treatment
If the fractured sternum is not properly aligned it may need reduction and wiring.
Injuries to viscera
Lung
Like other tissues, damaged lung becomes inflamed and engorged. Damaged lung does not function as well as healthy tissue and extensive lung contusion leads to respiratory failure. This, together with poor thoracic movement, pain, flail segments and pneumothorax, may precipitate respiratory failure even when the initial resuscitation has been successful.
The result, sometimes known as ‘shock lung’, is due to a combination of factors:
2. Over-transfusion, especially with saline or dextrose.
3. Poor chest movement.
4. Adult respiratory distress syndrome (ARDS).
The initial trauma causes platelet aggregation and activation of the neutrophils. The platelet aggregates occlude small vessels, leading to shunting and the release of hormones, which in turn cause bronchospasm and pulmonary hypertension. Superoxide radicals are also released by neutrophils and these act on the alveolar epithelium to increase pulmonary permeability.
Treatment
Adequate oxygenation, diuretics and positive pressure ventilation are required. Do not over-transfuse with crystalloid solutions.
Bronchus
Rapid deceleration can tear a bronchus, causing a massive leak into the pleural space.
Treatment
The lesion must be repaired as soon as possible by a thoracic surgeon.
Heart
Rupture of the heart is usually fatal but stab wounds are less serious. Because the heart contracts during systole, the wound is sealed at the moment of greatest pressure and blood loss is reduced. A haemopericardium follows but only causes cardiac tamponade if the pericardium is intact (Fig. 11.11). If the pericardium is ruptured or cut, as it would be with a stab wound, the cardiac tamponade decompresses itself and exsanguination is the main danger.
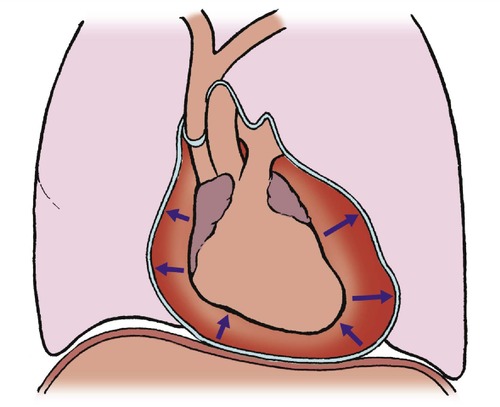 |
| Fig. 11.11
Cardiac tamponade.
|
Treatment
Thoracotomy and repair of the injury, with pericardial drainage.
Traumatic asphyxia and compression injuries
Rapid compression of the trunk squeezes the fluid contents, both liquid and gas, within the chest and abdomen and causes a violent surge of pressure in the peripheral vessels of the face, arms and legs. This can cause petechial haemorrhages at the periphery, ruptured bowel, and rupture of the diaphragm with bowel lying in the pleural cavity (Fig. 11.12). The petechial haemorrhages on the face, neck and arms are similar to those seen after strangulation and the condition is called traumatic asphyxia.
 |
| Fig. 11.12
Severe pressure on the abdomen may cause petechial haemorrhages in the face and hands.
|
Treatment
No specific treatment is required apart from adequate oxygenation and repair of the intrathoracic and intra-abdominal injuries.
Beware of abdominal trauma!
Small wounds or bruises may be the only sign of:
• Ruptured spleen.
• Ruptured liver.
• Ruptured gut.
Ruptured spleen
The spleen is a very vascular structure and remarkable for its trouble-free performance. The main affliction of the spleen is rupture; this can be followed by bleeding into the peritoneal cavity, which can be life-threatening and need surgery for its control. The injury that damages the spleen need not be violent: a blow to the left hypochondrium on the edge of a desk is quite sufficient, although more vigorous blunt trauma is usually involved.
Because the spleen has no sensory fibres, the patient does not experience pain but shows the signs of blood loss with a rapid pulse, falling blood pressure and pallor. The abdomen may be normal apart from diminished bowel sounds and there may be no other abnormality on clinical examination, but unless treated promptly the patient is likely to die from haemorrhage.
Some ruptured spleens behave in an even more treacherous manner. If the capsule remains intact it will limit the extent of the haemorrhage, but in some patients the capsule may rupture 24 h after injury. Detecting small amounts of intraperitoneal blood is therefore important, and abdominal paracentesis, with a few hundred millilitres of warmed saline run into the peritoneal space, drained out and inspected for blood, may be needed to make the diagnosis.
MRI is helpful but difficult to arrange as an emergency procedure on an ill patient. Laparoscopy is also helpful.
Treatment
Urgent laparatomy and splenectomy are life-saving measures. The abdominal surgeons should be asked to see any patient in whom a ruptured spleen is suspected.
Ruptured liver
Rupture of the liver, which is larger than the spleen and just as vascular, can also cause intraperitoneal haemorrhage. The commonest causes are rapid deceleration injuries and blunt trauma, usually sustained in road traffic accidents and accompanied by chest injuries. The liver cannot be removed but bleeding must be controlled, which is difficult because the liver is so soft and friable.
Treatment
Laparatomy is required to control bleeding by suturing individual vessels, packing, or selective ligation of the hepatic vessels. Dead and doubtful tissue must be excised to avoid sepsis.
Ruptured gut
Although the bowel and stomach can be ruptured by direct trauma, great force is required. Radiographs will often demonstrate gas in the peritoneal cavity on a sitting or standing film because the gas rises. The presence of gas under the diaphragm in an injured patient always indicates rupture of the stomach or bowel.
Treatment
Laparatomy and repair or resection of the affected bowel.
Stab wounds
Any stab wounds between the nipple line and the pubis can cause serious intra-abdominal damage. The length of the wound is no guide to the length of the blade and quite serious lesions, even perforation of the aorta, can be caused by a very narrow blade or glass sliver.
Treatment
Most wounds need formal exploration, including laparotomy, but careful exploration sometimes shows that the wound has not entered the peritoneum.
Retroperitoneal haematoma
The retroperitoneal space is large and includes the aorta, vena cava, kidney, psoas muscles and parts of the autonomic nervous system (Fig. 11.13). Haemorrhage into the space can follow damage to any of these structures, and is seen after fractures of the lumbar vertebrae or avulsion of the transverse processes.
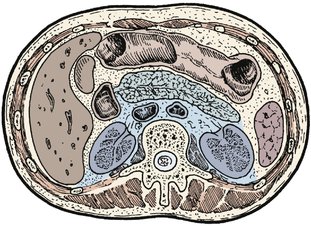 |
| Fig. 11.13
The retroperitoneal space.
|
A retroperitoneal haematoma not only causes a painful restriction of lumbar movement but also interferes with the autonomic nervous system and may cause paralytic ileus.
Treatment
No specific treatment is required but the patient must not eat or drink until bowel function has returned.
Kidneys
Trauma to the lumbar region may cause renal injury, followed by an accumulation of urine and blood in the retroperitoneal space. Damage to the upper urinary tract should be suspected if there is haematuria and the opinion of a urologist obtained. An excretion urogram will usually be required.
Treatment
Treatment is best in the hands of urologists and depends on the site and extent of the lesion. Suture, partial nephrectomy or total nephrectomy may be needed.
Pelvic injuries
Like fractures of the ribs, fractures of the pelvis are of varying severity. Patients can bleed to death from pelvic fractures if the iliac vessels are torn, and some fractures destroy the hip joint while others are little more serious than a bad bruise.
Pelvic fractures have a well-deserved reputation for being missed. The pelvis is easily fractured in crushing injuries and a serious fracture with an unstable pelvis should always be suspected after any compression injury. A pelvic X-ray is mandatory in the assessment of the acutely injured patient who has signs of cardiovascular instability.
In general, fractures can be divided into:
1. Avulsion.
2. Single bone.
3. Complex.
4. Acetabulum.
Avulsion
Avulsion fractures of the origin of the adductors, rectus femoris and sartorius muscles are seen in young fit athletes.
Treatment
The treatment is based on the severity of the injury and the degree of displacement. At times, large fragments will need to be reduced and held with internal fixation, i.e. a screw.
Single bone
These injuries are common in elderly patients with porotic bone or where there has been a well localized area of trauma. Fractures include pubic rami (Fig. 11.14 and Fig. 11.15) and the wing of the ilium. Pubic rami fractures often occur in pairs and can be trivial in nature. Occasionally, however, there can be associated injury to bladder or urethra.
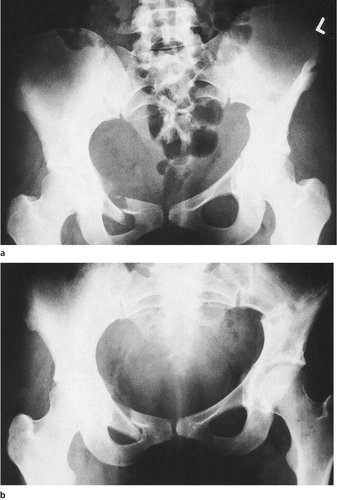 |
| Fig. 11.14
(a) Fracture of the right pubic rami and a fracture of the left ilium combined with a fracture extending into the left acetabulum, immediately after injury. (b) The same fracture 12 weeks later. Note the remodelling of the pubic rami.
|
 |
| Fig. 11.15
Fracture of the upper and lower pubic rami on the right side.
|
Treatment
Early mobilization in uncomplicated injuries is recommended. Patients will be in severe pain for the first few days but should be mobile in about a week.
Wing of the ilium
The main function of the wing of the ilium is to provide a firm foundation for muscle attachment and the protection of the pelvic contents. A fracture is caused by a direct blow or a crush injury.
Complex
The pelvis can be considered to be a ring structure. It is uncommon to be able to break the true ring in a single place, and fractures can therefore be multiple. There are three main fracture patterns, depending on the mechanism of the injury. These are:
1. Anterior/posterior compression (open book).
2. Side compression.
3. Vertical compression.
Anterior/posterior compression
Anterior/posterior compressions can involve not only the pubic diastasis but also fractures of the pubic rami and/or sacroiliac joints, ilium or sacral body. This injury can cause catastrophic blood loss from tearing of the iliac vessels.
Treatment. Minor injuries can be treated with bed rest and gradual mobilization. More major injuries may need the reduction of the fracture – i.e. ‘closing the book’. This can be accomplished by a pelvic sling, or internal or external fixator. In those cases with significant blood loss, early rapid application of an external fixation (Fig. 11.16) can be life-saving. This may be necessary in the emergency room.
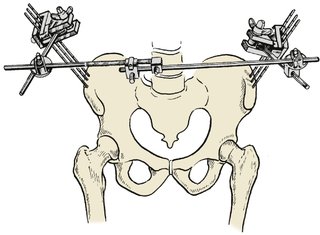 |
| Fig. 11.16
External fixation of a pelvic fracture.
|
External compression
These are caused by a blow to the side of the pelvis or greater trochanter. The side of the injury is rotated inwards, resulting in fractures of the pubis or ilium, disruption of the sacroiliac joint or fracture of the sacrum.
Treatment. Minor injuries can be left and patients treated conservatively with bed rest until the pain has settled. They can be mobilized with the aid of crutches until the fracture has consolidated (> 6 weeks). More major injuries may require open reduction and internal fixation of the fracture fragments.
Vertical compression
These are often associated with a fall from a height. There is disruption not only of the anterior part of the ring but also of the sacrum, sacroiliac joint or ilium. Neurological damage can occur due to the shearing injury and damage to the sacral plexus.
Treatment. Reduction of the hemipelvis is necessary in order to stabilize the pelvis. This can be achieved by traction, or external or internal fixation.
Acetabulum
Fractures of the acetabulum disrupt the hip joint (Fig. 11.17). Major disruption will often lead to osteoarthritic degeneration in the long term. The major goal of treatment is to limit the chance of this and to retain early active movement of the hip joint.
 |
| Fig. 11.17
Plain radiograph of a fractured acetabulum.
|
Accurate assessment of the fracture is necessary in order to formulate an appropriate treatment plan. Plain radiographs do not give sufficient detail of the acetabulum to classify the type of fracture or the degree of displacement of the fracture fragments. Specialized X-rays (Judet views) or CT scans are required. Fractures can be classified according to their location in the acetabulum. There are anterior or posterior column fractures, or a combination of both (Fig. 11.18).
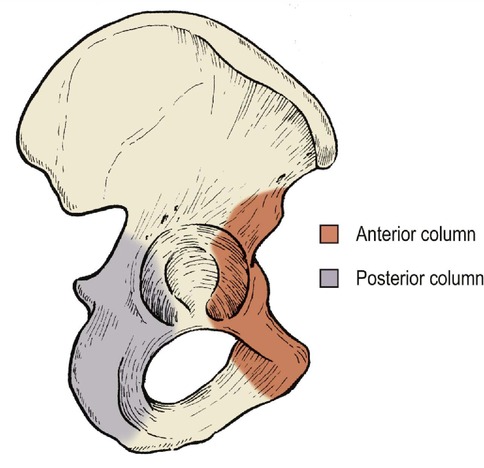 |
| Fig. 11.18
The anterior and posterior columns of the pelvis.
|
Treatment
In those that are undisplaced, early rapid movement is essential in order to regain the mobility of the hip joint (Fig. 11.19). Initially, patients can be treated in bed for the first few days to allow the pain to settle, then they should be mobilized with a non-weight-bearing regimen for a minimum of 6 weeks.
 |
| Fig. 11.19
Fracture of the right ilium extending into the acetabulum with minimal displacement.
|
In those fractures that are significantly displaced, there is a need to reduce the fracture fragments and this is best achieved by open reduction and internal fixation. Undoubtedly, some fractures are so convoluted that this is impossible and then patients may be treated with traction and early active mobilization while on traction.
Damage to the bladder and urethra/rectum
Bladder
Direct trauma to the pelvis can rupture the bladder, particularly if it is full at the time of injury. The injury to the bladder will usually be extraperitoneal unless there is an associated penetrating wound of the abdomen.
Urethra
The urethra can be damaged in any major injury of the pelvis and urethral damage should always be suspected. If there is a discharge of blood from the urethra or a boggy swelling in the perineum a urologist is required.
Treatment
The urologists should be involved at an early stage and a catheter should not be passed until they have been consulted.
Rectum
The rectum can also be damaged and a rectal examination is always recommended. This will assess not only the rectum but also the urogenital tract.
Posterior dislocation of the hip
Posterior dislocation of the hip is common in head-on road traffic accidents in which the hip and knee are both flexed (Fig. 11.20). This dislocation should be suspected in any patient involved in such an injury. The impact is transmitted via the patella, patellofemoral joint, femur and hip joint to the posterior lip of the acetabulum, which is a thin bone and not designed for such impact (Fig. 11.21 and Fig. 11.22).
 |
| Fig. 11.20
Bilateral posterior dislocation of the hips with a fracture of the posterior lip on the right.
|
 |
| Fig. 11.21
Posterior fracture dislocation of the hip.
|
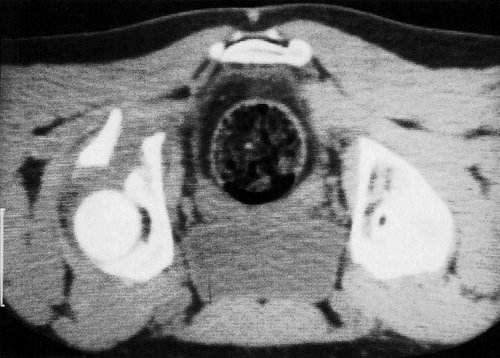 |
| Fig. 11.22
CT scan of the pelvis showing a displaced fracture of the posterior lip of the acetabulum.
|
The injury is often associated with fracture of the patella, rupture of the posterior cruciate ligament and fracture of the femur (Fig. 11.23).
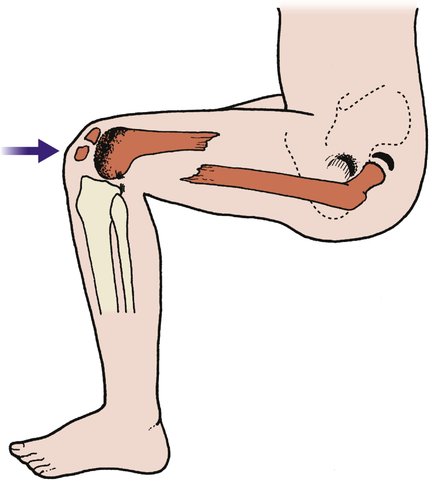 |
| Fig. 11.23
Injuries caused by a blow to the patella with the hip and knee flexed: (i) fracture of the patella; (ii) damage to the articular surface of the femur; (iii) ruptured posterior cruciate ligament; (iv) fractured femur; (v) fracture dislocation of hip.
|
Until the dislocation is reduced, the femoral head lies behind the pelvis and the leg is internally rotated and shortened (p. 182).
There may also be a segmental or ‘slice’ fracture of the femoral head. The fragment may become jammed in the hip joint and prevent reduction or, worse, the sciatic nerve may be caught between the femoral head fragment and damaged when the hip is reduced (Fig. 11.24).
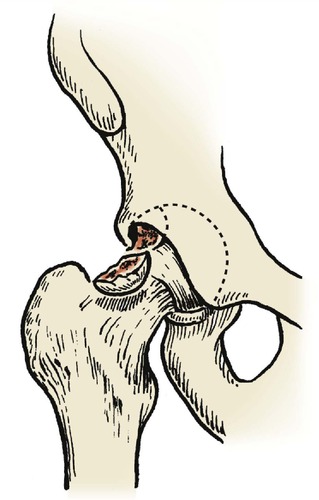 |
| Fig. 11.24
Osteochondral fracture of the femoral head. This lesion often accompanies a dislocation of the hip.
|
Complications
Posterior dislocation of the hip has a high incidence of complications (Fig. 11.25).
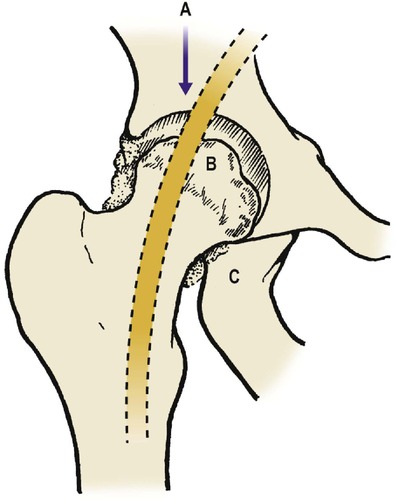 |
| Fig. 11.25
Complications of posterior dislocation of the hip: ( A) damage to the sciatic nerve; ( B) aseptic necrosis of the femoral head; ( C) ectopic ossification around the hip.
|
Treatment
The dislocation should be reduced as soon as possible and certainly within the first 4–6 h post-injury. Reduction is usually easy, but be careful if there is an associated fracture of the femoral head or neurological damage. Always record the neurological function before and after reduction.If reduction is not easy, open reduction is needed to avoid damage to the sciatic nerve.
Definitive management depends on the stability of the reduction. If the hip is stable and the acetabular fragment is small, bed rest for 2–3 weeks with early mobilization is sufficient.
If the fracture is unstable but the fragments are in good position, bed rest for 6–8 weeks is advisable. If there is a large single fragment or a fragment in poor position and the hip is unstable, the fragment should be replaced and internally fixed.
Anterior dislocation of the hip
Anterior dislocation is rare but may follow violent abduction, although such a force is more likely to fracture the femur.
Complications
Complications include aseptic necrosis of the femoral head and osteoarthritis.
Treatment
Treatment is by closed reduction.
Sacral fractures
Sacral fractures are uncommon and usually associated with fractures of the pelvis.
Treatment
Treatment depends upon the associated pelvic fractures but internal fixation is hazardous and seldom needed.
Fractures of the coccyx
Fractures of the coccyx result from a direct blow to the bottom from a fall onto the coccyx. They are exceedingly painful.
Treatment
No specific treatment is required apart from analgesics and a soft cushion. The pain may be very slow to resolve and can lead to lasting disability.
Case reports
The management of pelvic injuries can be difficult. The following two cases highlight some of these difficulties.
Patient A
A 30-year-old pedestrian was involved in a road traffic accident when hit by a car travelling at speed. The mechanism of injury was unknown and the patient was brought to the accident and emergency department conscious and haemodynamically unstable with a painful abdomen.
The initial clinical review confirmed a normal Glasgow coma scale, increased respiratory rate, blood pressure of 110/40 and tachycardia. On palpation the abdomen was tender, maximally in the suprapubic area. There was marked bruising of the scrotum and blood at the external meatus. Both legs lay in slight external rotation and there was an abrasion over the skin of the lower abdomen.
Despite vigorous fluid rehydration with crystalloids and colloids the patient remained haemodynamically unstable. Radiographs were obtained of the cervical spine, abdomen and pelvis. The pelvic X-rays confirmed wide diastases of the pelvis. A CT of the abdomen confirmed no liver or splenic injury but fluid within the pelvis and the diastases.
The urologists reviewed the patient and confirmed the urethra had been disrupted but the patient did not have a large bladder at that time. Because the patient remained haemodynamically unstable a traction sling was applied around the pelvis to attempt to ‘close the open book’. This failed to alter the haemodynamic state and the patient was then taken to theatre and an external fixator applied across the front of the pelvis to stabilize it.
Stabilizing the pelvis in such cases reduces the intrapelvic volume and tamponades the posterior arterial and venous structures, thereby causing haemostasis.
Patient B
An 18-year-old student, depressed by a poor examination performance, jumped from a three-storey building, landing predominantly on the right leg. He sustained injuries to the leg and pelvis.
When reviewed in the casualty department it was noted that he had bruising of the right heel, no pain within the knee, but pain with all movements of the right hip and low back pain.
Radiographic review confirmed a fractured calcaneum, a vertical sheer fracture of the right hemipelvis with a disruption of both posterior and anterior columns, but no thoracolumbar injury.
Cardiovascular status remained satisfactory and the patient remained haemodynamically stable. The patient was treated with bed rest and traction to allow the hemipelvis to heal and subsequently made a good recovery.
Moral
When assessing a pelvic fracture it is important to remember the mechanism of injury. Different types of fracture are associated with different complications. ‘Open book’ injuries are often associated with urological complications and patients may have significant hypovolaemia. Urgent surgery may be required to stabilize the pelvis to restore the haemodynamic state.
Lateral compression or vertical sheer fractures may not have the same morbidity but, because of the severity of the injury to the pelvis and the associated injuries to other parts of the skeleton, may have a more long-term effect with prolonged patient pain, immobility and dysfunction.