CHAPTER 21 Injuries to the Triangular Fibrocartilage Complex
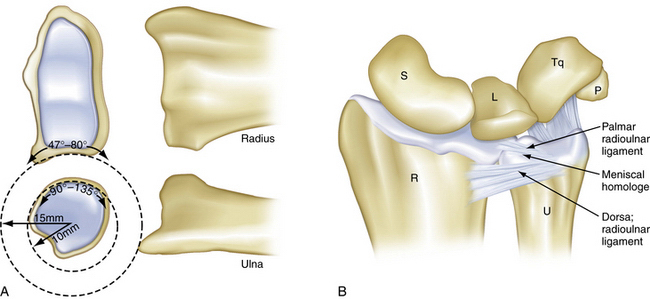
In 1981, Palmer and Werner used the term triangular fibrocartilage complex (TFCC) to describe the set of related structures at the distal ulnar aspect of the wrist.1 The TFCC physically separates the distal radioulnar joint (DRUJ) from the radiocarpal joint. The TFCC must be simultaneously robust and flexible. It must have the strength to transmit 20% of the load of the carpus to the ulna and to stabilize the DRUJ and ulnar carpus in conjunction with the bony architecture of the sigmoid notch. It is must also be supple enough to accommodate the significant, complex motion that occurs during forearm rotation. The motion of the DRUJ is a combination of approximately 150 degrees of rotation and sliding. This occurs because the radius of curvature is 50% larger on the radial side of the DRUJ (15 versus 10 mm) (Fig. 21-1A). The axis of rotation passes through the fovea of the ulnar head, which is a major attachment site for the TFCC.
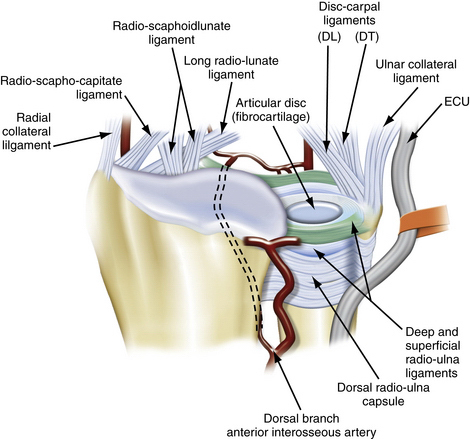
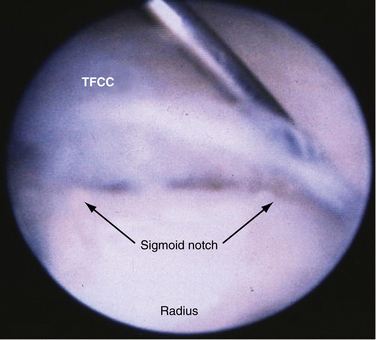
The five structures that comprise the TFCC are the articular disk, the distal radioulnar ligaments (palmar and dorsal), the meniscal homologue, and the extensor carpi ulnaris (ECU) subsheath, which is confluent with the (ulnocarpal collateral ligament (see Fig. 21-1B).2 The central portion of the complex consists of an articular disk called the triangular fibrocartilage (TFC). The disk is composed predominately of type II collagen, which is consistent with its role in distributing compressive forces. It lies in the axial plane and structurally represents an extension of the articular surface of the distal radius. Dorsally and palmarly, the TFC is surrounded by the radioulnar ligaments, which are transverse bands that derive their broad origin from the sigmoid notch of the distal radius and insert on the base of the ulnar styloid. The ulnotriquetral and ulnolunate ligaments form the palmar border of the TFCC, and, although Palmer and Werner did not include them in their original description of the TFCC, they serve an important role in the stability of the ulnar side of the wrist.
The blood supply of TFCC enters from the periphery (Fig. 21-2). Thiru and colleagues evaluated cadaveric specimens and identified three main branches of the TFCC.3 The ulnar periphery of the TFCC has the richest blood supply and, consequently, the greatest potential for healing. It is fed predominantly via the dorsal and palmar radiocarpal branches of the ulnar artery. Dorsal and palmar branches of the anterior interosseous artery supply the more radial part of the complex.
CLASSIFICATION OF TRIANGULAR FIBROCARTILAGE COMPLEX INJURIES
Palmer’s original classification divides injuries of the TFCC into degenerative and acute tears (Box 21-1).4 The classification is anatomically subdivided into radial, central, and ulnar tears. This classification bears consideration, because the vascular anatomy dictates the healing potential and therefore the treatment and prognosis for TFCC tears, similarly to tears of the knee’s meniscus.
Box 21-1 Classification of Triangular Fibrocartilage Complex Injury
From Palmer AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14:594.
Palmer class 1 injuries are acute, traumatic injuries. They are subdivided into four types, based on the site of injury (Fig. 21-3):
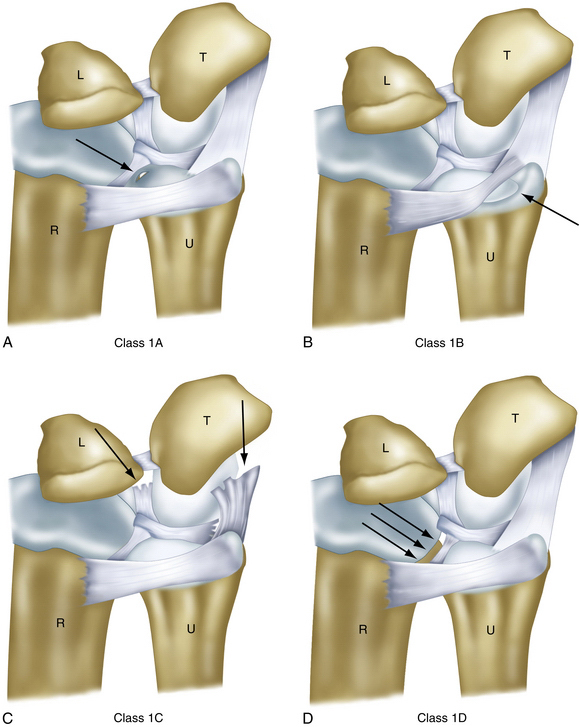
FIGURE 21-3 Four types of class 1 lesions of the triangular fibrocartilage complex. L, lunate; R, radius; T, triquetrum; U, ulna.
(Modified from Palmer AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14:594-606.)
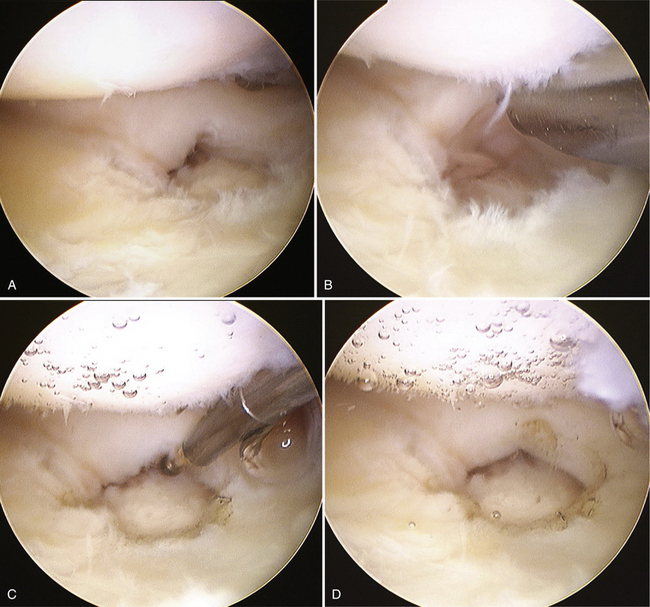
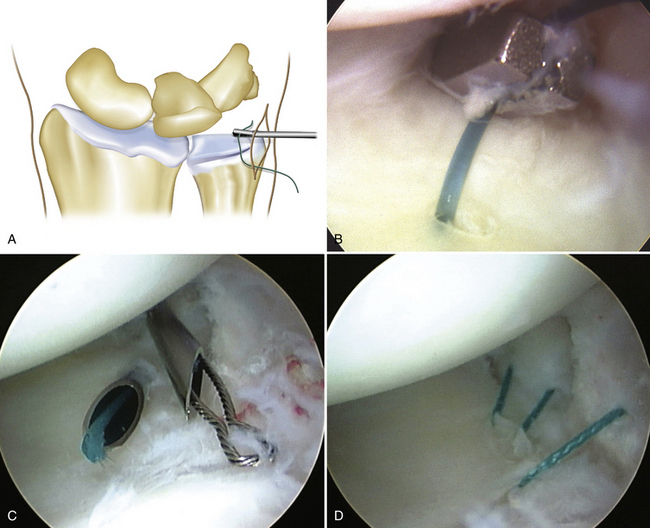
FIGURE 21-4 Arthroscopic treatment of type 1A lesions involving the central avascular portion requires débridement of the central tear to remove any flaps that may impede movement. A, Lesion in the central portion of the triangular fibrocartilage complex (TFCC). B, Central tear of the TFCC is débrided using a 2.5-mm arthroscopic shaver. C, Ablation at the edge of the lesion using a small joint radiofrequency probe. D, Smooth surface of the lesion after débridement.
Degenerative TFCC lesions (Palmer class 2) all involve the central portion and are staged from A to E, depending on the presence or absence of a TFCC perforation, lunate and ulnar chondromalacia, a lunotriquetral ligament perforation, or degenerative radiocarpal arthritis. These degenerative lesions usually arise from ulnar abutment. Class 2 lesions usually are not amenable to surgical repair and are treated with débridement.
TFCC tears can be further subdivided by their acuteness. The chronicity has prognostic implications, and addressing tears in the acute phase usually provides better results.5–7
The incidence of asymptomatic TFCC tears increases with age. Wright and coworkers, in a study of 62 wrists from cadavers of individuals whose average age at death was 78 years and found a tear of the TFCC in 33 wrists (11 lesions were central, and 21 were vertical radial).9–11 Mikic observed an age-related correlation with disk perforation in his cadaveric study of 180 wrists from fetuses to the elderly. He found the prevalence of perforations to be zero among patients younger than 20 years; 7.6% among those in the third decade; 18.1% in the fourth decade; 40.0% in the fifth decade; 42.8% in the sixth decade, and 53.1% (26 wrists) among patients older than 60 years.9 These degenerative changes correlated with magnetic resonance imaging (MRI) findings from healthy volunteers.12 This illustrates the necessity of correlating imaging with history and examination findings in these patients.
PATIENT EVALUATION
History, Signs, and Symptoms
Ulnar-sided wrist pain has been referred to as the low back pain of the hand surgeon. The multitude of structures and diagnoses that can contribute to a patient’s symptoms are often subtle and require precise physical examination and correlation with history and imaging. Causes of ulnar-sided wrist pain are listed in Box 21-2.
Box 21-2 Common Causes of Ulnar-Sided Wrist Pain
DRUJ, distal radioulnar joint; ECU, extensor carpi ulnaris; TFCC, triangular fibrocartilage complex.
Chronic attritional injuries and degenerative changes of the ulnocarpal joint, including the TFCC, result from repetitive overloading. Ulnar deviation of the wrist, along with forearm supination and power grasp, increase the damage from axial loads. Patients with acquired ulnar positive variance, discussed in greater detail later, are at higher risk for degenerative changes and recurrent injury from minor trauma.
TFCC tears have been associated with distal radius fractures on imaging and direct arthroscopy. The incidence ranges between 13% and 60%.13–17 The literature does not clearly indicate, in the absence of frank DRUJ instability, which tears should be fixed and by which methods, in part because it is unclear how many of these tears become symptomatic. It is likely that many of these tears are effectively treated by treatment of the concomitant fracture.14 Nevertheless, several authors have endorsed the use of arthroscopy in the setting of distal radius fracture fixation to identify and treat concomitant soft tissue injuries. Varitimidis and associates reported that 60% of their patients with distal radius fracture had TFCC tears, half of which were ulnar sided.17 All TFCC tears underwent débridement; 20% (2 of 12) had arthroscopic repair, and 1 patient required open repair. The arthroscopic group demonstrated improved ROM and Mayo wrist scores, compared with those treated with traditional external fixation. In 2003, Ruch and colleagues demonstrated good or excellent results with acute repair of the TFCC at the time of distal radius operative treatment in 56 patients, with only 2 patients with transient ulnar dorsal sensory irritation, but they lacked a control group.18
Lindau and coworkers reported that 10 of 11 patients with a documented complete peripheral TFCC tear associated with a distal radius fracture exhibited DRUJ instability at a 1-year follow-up examination, compared with 22% of those with no peripheral tear or only a partial tear.19 This instability was correlated with worse clinical outcome.
Physical Examination
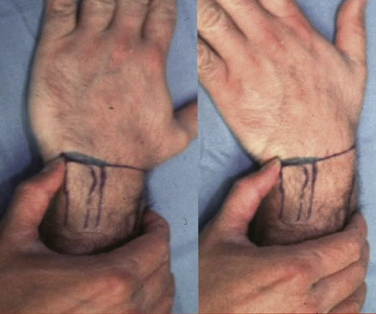
Patients with acute TFCC injuries frequently present with ulnar-sided wrist swelling that may reverse the normal convex shape of the ulnar wrist border. The soft, ballotable region between the ulnar styloid and the triquetrum can frequently be point tender (Fig. 21-7). Clicking can often be elicited with passive and active circumduction of the wrist. Specialized tests to distinguish TFCC injuries from other ulnar wrist injuries include the TFCC compression test, the ulnar impaction test, and the piano key test. Significant pain from axial loading of the TFCC, in conjunction with ulnar deviation, is a positive compression test. Similarly, pain with the combination of wrist hyperextension and the previous maneuvers indicates a positive ulnar impaction test.20 Comparison of any dorsal-volar plane instability of the DRUJ with the normal contralateral side is the piano key test (Fig. 21-8). This should be performed in neutral position, in supination, and in pronation. The DRUJ typically has the most anteroposterior translation in the neutral position. Volar subluxation of the distal ulna with wrist supination can be appreciated by dimpling of the skin of the dorsal ulnar border (Fig. 21-9). Lunotriquetral ballottement tests ligament stability (Fig. 21-10). Pisotriquetral manipulation should be performed to rule out arthrosis of this joint.
Diagnostic Imaging
Acute or chronic ulnar-sided wrist pain warrants posteroanterior, lateral, and oblique radiographs of the wrist. True neutral rotation, posteroanterior radiographs are taken with the shoulder in 90 degrees of abduction and the elbow in 90 degrees of flexion. The ulnar styloid should be visible at the far ulnar portion of the distal ulna in a true posteroanterior view, in contradistinction to its location in the midportion of the distal ulna on radiographs taken in a supinated or pronated position. Others advocate the use of the pisiform’s relationship to the scaphoid as a landmark, citing the variability of the position of the ulnar styloid. In a true lateral view, the pisiform should lie between the palmar surface of the scaphoid distal pole and the capitate.
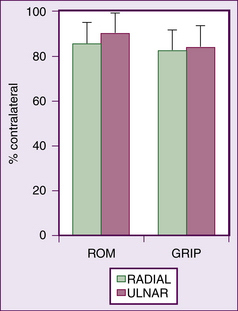
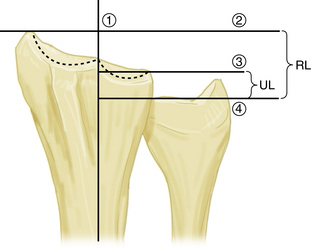
Ulnar variance is the difference between the length of the ulna and the length of the radius at the wrist. Specifically, this distance is measured between lines drawn perpendicular to the shaft of the radius and the ulnar corner of the radius and a line drawn along the distal articular surface of the ulna. Ulnar-positive or -negative variance is defined as a distal ulna that is longer or shorter, respectively, than the radius (Fig. 21-11). This is clinically important for several reasons. Anatomically, Palmer showed that ulnar variance is inversely correlated with the thickness of the central portion of the TFC.21 Cystic changes in the lunate and the distal ulna, especially in conjunction with ulnar-neutral or -positive variance, can be the hallmark of excessive loading through the ulnar carpus, as is the case with ulnar impaction syndrome (see Fig. 21-19). These changes may suggest the need for off-loading procedures, such as an ulnar shortening osteotomy, in conjunction with TFCC treatment. In this setting, encouraging results have been achieved by combining these treatments. Trumble and associates demonstrated significant relief of pain.7 Grip strength and ROM averaged approximately 80% of the uninjured side. Central TFCC tears treated in the setting of ulnar-positive variance with ulnar shortening osteotomy alone showed 50% healing on second-look arthroscopy, with a spectrum of greatest to least healing on the more vascular ulnar side, compared with the less vascular radial side.22
Radiography
Plain radiographs are undoubtedly important to rule out alternative causes of wrist pain, but the correlation between specific radiographic findings and injuries to the TFCC itself remains contentious. Although Geissler and colleagues concluded that TFCC tears had occurred in 26 of 60 patients in their series, representing the most common intracarpal soft tissue lesion found. They believed that radiographs were most helpful in the setting of scapholunate ligament injury and least helpful in TFCC tear. Nevertheless, radiographic findings of DRUJ dislocation and ulnar styloid fracture were the best surrogates to infer TFCC injury. Of the 25 patients with ulnar styloid fracture, 16 had TFCC tears, 14 of which were ulnar sided.16 This finding was corroborated by Lindau and coworkers.19 On the other hand, Richards and colleagues22a found no correlation between ulnar styloid fractures and TFCC injuries. Instead, tears were related to greater shortening and dorsal angulation of the distal radius on the preoperative radiographs in their study of 118 intra-articular and extra-articular wrist fractures. In 2008, Bombaci and associates compared MRI findings of TFCC tears with plain radiographs.23 MRI revealed that 27 (45%) of the 60 patients had TFC lesions. No correlation was found between TFCC injury and the Melone classification system, the presence of an ulnar styloid fracture, comminution of the articular surface of the distal radius, more than 20 degrees of dorsal angulation of the distal radius, or subluxation or dislocation of the DRUJ on the plain radiographs. However, Frykman subtypes with distal radius fracture that extended to the DRUJ and/or the radiocarpal joint with an ulnar styloid fracture did have a statistically higher incidence of TFCC tears, compared with the remaining Frykman subtypes of injury after distal radial fractures.23
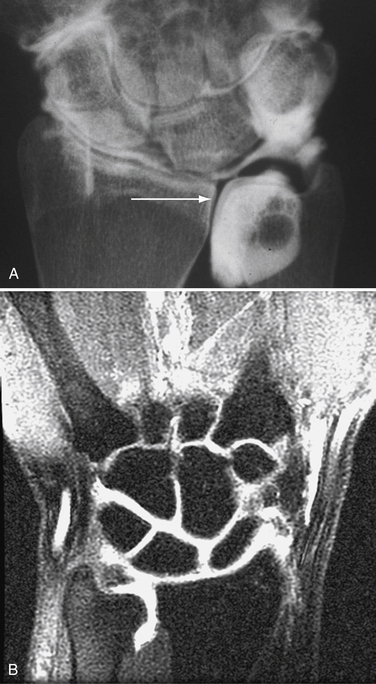
Arthrography
Wrist arthrography can be used to help diagnose tears of the scapholunate and lunotriquetral interosseous ligaments.24–27 After midcarpal row injection, the contrast agent is injected into the radiocarpal joint. Contrast extravasation into the DRUJ indicates perforation of the TFCC (Fig. 21-12A). Injection directly into the DRUJ can demonstrate smaller tears and those with an overlying flap. Arthrograms more reliably diagnose TFCC radial detachment and lunotriquetral ligament tears than ulnocarpal ligament injuries and ulnar TFCC detachments.24,25,28 Single-injection arthrograms have a high incidence of positive findings in asymptomatic patients.24 It is important to correlate the presences of symptoms with the suspected findings on the study.
Magnetic Resonance Imaging
MRI for the diagnosis of TFCC injuries is a controversial issue. The specificity and sensitivity of MRI for detection of central and radial detachments vary but can be improved by dedicated musculoskeletal radiologists using specialized equipment such as wrist surface coils and higher Tesla magnets.29 Golimbu and colleagues,30 Joshy and associates,31 Skahen and coworkers32 detected TFCC injuries with an accuracy between 74% and 95%. In the study by Joshy and asociates,31 in which patients underwent arthroscopy after MRI arthrography, the positive predictive value was 0.95, but the negative predictive value was only 0.50. This study used a 1.0-T magnet, whereas a Mayo clinic study using 3.0-T magnets showed improved accuracy.33 Compared with arthroscopy for definitive diagnosis, MRI appears to understage some TFCC pathology, specifically the proximal and distal radioulnar ligaments, while overstaging others, such as radial-sided and disk tears.29,34 In our experience, magnetic resonance arthrograms have been the most efficient and accurate nonoperative means of evaluating ulnar wrist pain (see Fig. 21-12B).
TREATMENT
Indications
Equipment and Implants
Required items include the following:
Optional items include the following:
Although several authors contend that most TFCC tears, in the absence of DRUJ instability, can be treated nonoperatively, there is not strong support from the literature.35 After a reasonable period of activity modification, steroid injections, and immobilization, if the patient’s symptoms are unresolved, surgical intervention is warranted.
Arthroscopic Techniques and Results
Type 1A
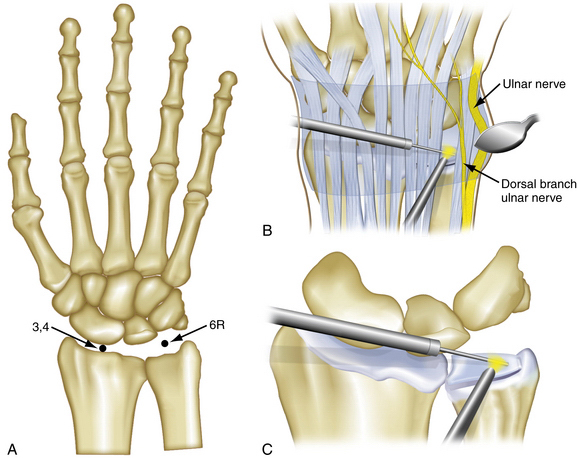
A wrist distraction tower is used to suspend the hand and wrist by means of finger traps with 10 to 15 pounds applied. Lidocaine with epinephrine is injected to distend the radiocarpal joint through the area of the planned 3-4 portal. The 3-4 portal is placed between the extensor pollicis longus (EPL) tendon and the extensor digitorum communis (EDC) tendon, 1 cm distal to Lister’s tubercle between the scaphoid and the lunate. For the initial diagnostic examination, the arthroscope is placed into the 3-4 portal, and a small probe is placed into the 4-5 portal between the EDC and the extensor digiti minimi (EDM) (Fig. 21-13). A 2.7-mm Linvatec arthroscope is used with a 2.5-mm small-joint débrider (Stryker, Sunnyvale, CA) that has a full-radius blade for synovectomies and débridement of the central tear.
The goal in treating central tears is to débride the tear back to a stable rim. Various methods of doing so (e.g., shaver, thermal, laser) are available but have not been compared for efficacy. The results of treatment are good or excellent in 66% to 87% of patients with traditional débridement or with laser and radiofrequency probe ablation.36 Results decline in patients with ulnar positivity, leading to failure rates as high as 60%, most likely because of sustained higher loads across the TFCC.37 Hulsizer and colleagues demonstrated that even in the absence of ulnar positivity, good results can still be salvaged from patients who have poor results after TFCC débridement by performing a subsequent ulnar shortening osteotomy.38
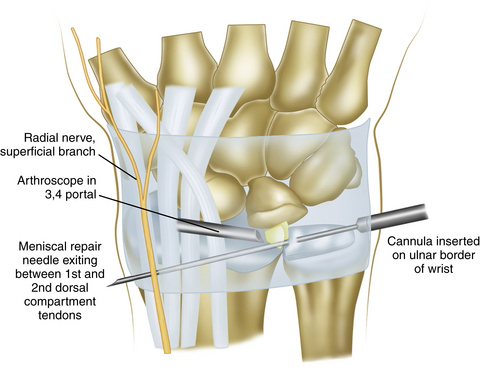
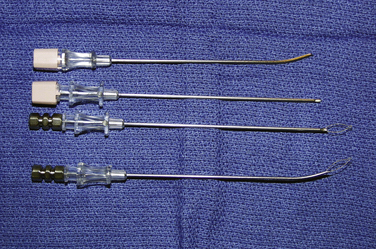
Types 1B and 1C
The inside-out technique is occasionally used for small volar or peripheral tears. Diagnostic arthroscopy is performed in a similar fashion as for TFCC detachment from the radius. With the use of a small probe, the diagnosis of peripheral detachment is made by the trampoline test of the TFCC, as described by Hermansdorfer and Kleinman.39 The normal TFCC should be taut when tested with the probe. If the TFCC is redundant and wavy when compressed by the arthroscopic probe (Fig. 21-14), a peripheral or ulnar-sided tear is indicated. In these cases, the arthroscope is placed in the 6-R portal. The arthroscopic shaver is placed into the 3-4 portal to débride any excess synovium that may be blocking the view needed for suture passage. The shaver should also be used to débride the frayed portions of the TFCC in the region of the tear. An arthroscopic cannula is then placed into the 3-4 portal to facilitate passage of the 2-0 Maxon meniscal repair sutures. A small longitudinal incision is made at the 6-U portal. The wrist capsule should be exposed but not incised, to avoid leakage of the intra-articular solution used to distend the joint. The ulnar nerve is identified and protected with the use of a retractor. The sutures are placed through the cannula and brought out through the ulnar incision. Two or three sets of sutures are used for repair of the peripheral detachment (Fig. 21-15). Tension is then placed on the sutures to re-establish the normal tension of the TFCC and obliterate any gapping between the meniscal homologue and portions of the peripheral capsule. The patient’s hand is then taken out of the traction device, and the sutures are tied with the wrist in neutral rotation and slight ulnar deviation. In type IC lesions, the repair is almost directly under the flexor carpi ulnaris, and close to the ulnar nerve, so the use of a protective retractor is critical.
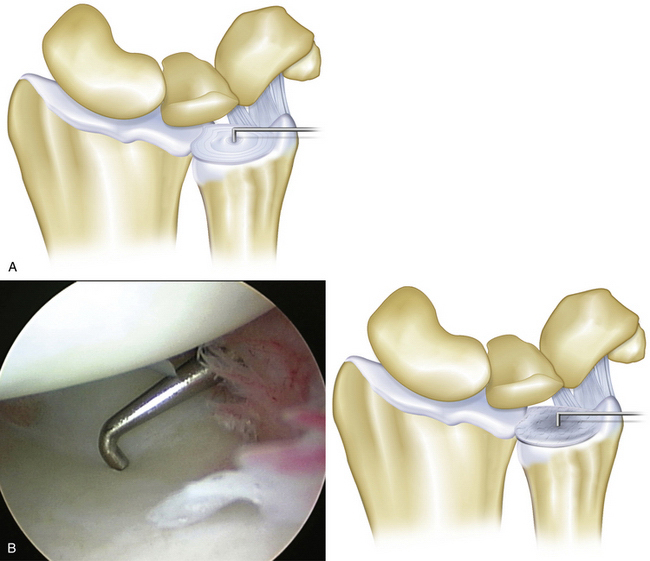
FIGURE 21-14 A, The trampoline test uses the arthroscopic probe to differentiate between the normal, taut triangular fibrocartilage complex (TFCC) (left) and the loose, redundant TFCC with a peripheral or ulnar-sided TFCC tear (right). B, During the arthroscopic examination of the ulnar-sided TFCC tear, the loose, redundant TFCC can be detected by the trampoline test.
(A, Modified from Trumble TE. Distal radioulnar joint and triangular fibrocartilage complex. In: Trumble TE, ed. Principles of Hand Surgery and Therapy. Pennsylvania, PA: WB Saunders; 1999:136.)
The repair suture is threaded into an 18-guage needle (Kendall, Argyle, NY) or a special passing needle and inserted into the wrist joint through the 6-U portal under arthroscopic control. The needle passes through the torn edge of the TFCC just radial to the edge (Fig. 21-16). The suture is threaded out through the needle and grasped with a small arthroscopic grasping forceps or wire suture grasper (Smith & Nephew, Inc., Andover, MA) (Fig. 21-17) placed through the 6-U portal. Two or three sutures are passed by this technique (Fig. 21-18). The incision for the portal is enlarged so that all the suture ends can be brought out through the 6-U portal incision and tied over the capsule under direct vision. This exposure helps to protect the small branches of the dorsal sensory branch of the ulnar nerve.
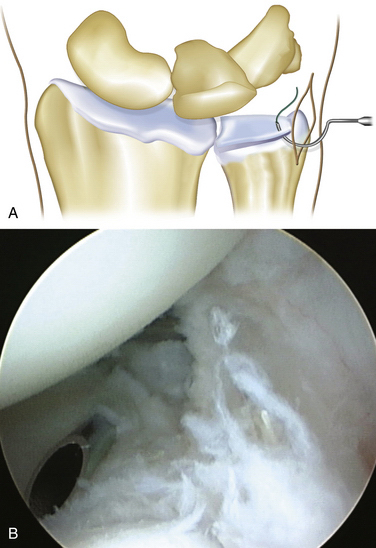
FIGURE 21-16 A, The outside-in technique for repairing peripheral tears of the TFCC is performed by placing an 18-gauge needle or curved suture cannula in the 6-U portal so that it pierces the detached edge of the triangular fibrocartilage complex (TFCC). B, During the arthroscopy, the hollow needle cannula is placed through the rim of the TFCC tear to pass the repair suture.
(A, Modified from Trumble TE. Distal radioulnar joint and triangular fibrocartilage complex. In: Trumble TE, ed. Principles of Hand Surgery and Therapy. Pennsylvania, PA: WB Saunders; 1999:137.)
Ulnar-sided peripheral tears can be addressed with either open or arthroscopic techniques. Corso and associates reported that 42 (93%) of the 45 patients in their multicentered trial had a satisfactory outcome, with an average of 75% of the grip strength of the contralateral hand 3 years after repair.40 However, 27 patients in that study had additional wrist injuries, including distal radius fractures and scapholunate ligament tears. Patients without these injuries would likely have improved outcomes. In 2002, Millants and colleagues published an outcome study of 35 patients who had arthroscopic surgical repair of ulnar-sided tears.41 Patients were assessed using a visual analog scale the Disabilities of the Arm, Shoulder, and Hand (DASH) score. According to the DASH score, 29 patients had good results, 5 had fair results, and 1 had a poor result. Degreef and colleagues corroborated these results, showing 80% grip strength and minimal to no pain in 47 of 52 patients after ulnar-sided repair.42
Results of type 1C injuries have not been specifically addressed in the literature. These lesions are uncommon and represent injuries to the extrinsic volar ulnar-sided ligaments caused by high-energy trauma. In 2007, Estrella and coworkers studied 35 patients with all subtypes, 5 of whom had type 1C; overall, 75% had good or excellent results and averaged 88% and 82% motion and grip strength, respectively.43
Type 1D
The technique for treatment of type 1D lesions was modified from the that described by Cooney for open repairs using sutures placed through the radius.28 A wrist distraction tower and portals as previously described are used. The 2.5-mm, full-radius, small-joint débrider is used to prepare for the reattachment of the TFC.
In the 2007 study of Estrella and colleagues,43 only 1 of 35 patients had a type 1D tear. Results were not given for that patient specifically.43 In a 2002 study by Shih and colleagues, 8 of the 37 patients had type 1D tears and “showed the same results” as those with type 1B tears on Mayo wrist scores with 2-year follow-up.44 Newer techniques are being developed that utilize a mini Push-lock anchor (Arthrex, Naples, FL) in a fully arthroscopic technique. Use of the mini-suture lasso and small arthroscopic cannulas to assist in passage of the anchor into the sigmoid notch can facilitate the technique.
Type 2 Tears
Most of Palmer’s class 2 attritional lesions result from excessive loading of the distal ulna, triquetrum, and/or lunate (Fig. 21-19). After an TFCC tear has been identified by arthroscopic evaluation, non-reparable lesions can be débrided with the use of the 2.5-mm, full-radius shaver, with the device placed in the 6-R portal and the arthroscope in the 3-4 portal. In cases of positive ulnar variance, an ulnar shortening osteotomy in conjunction with TFCC débridement is recommended. The shortening osteotomy decompresses the ulnar side of the wrist by decreasing the impaction between the distal ulna and the carpus.

FIGURE 21-19 Coronal, T2-weighted MRI shows ulnar impaction syndrome with significant edema within the lunate and distal ulna.
Although poor results have been associated with DRUJ arthritis, chronicity of symptoms, and worker’s compensation claims, Bernstein and coworkers demonstrated that ulnar shortening osteotomy resulted in increased Mayo wrist scores, improved grip, better motion, and high patient satisfaction.45,46
CONCLUSIONS
TFCC tears are among the numerous causes of ulnar-sided wrist pain. Although tears often can be treated nonoperatively, early diagnosis is helpful for patients with ulnar-sided wrist pain that does not improve despite initial conservative efforts. Correlating the patient’s history and symptoms with findings on the magnetic resonance arthrogram is critical to accurate diagnosis. After identification, peripheral tears on the radial or the ulnar side can be repaired, whereas central tears and class 1A tears benefit from débridement. If arthroscopic treatment fails to provided relief, ulna shortening can improve the symptoms.
1. Palmer AK, Werner FW. The triangular fibrocartilage complex of the wrist: anatomy and function. J Hand Surg Am. 1981;6:153.
2. DiTano O, Trumble TE, Tencer AF. Biomechanical function of the distal radioulnar and ulnocarpal wrist ligaments. J Hand Surg Am. 2003;28:622.
3. Thiru RG, Ferlic DC, Clayton ML, et al. Arterial anatomy of the triangular fibrocartilage of the wrist and its surgical significance. J Hand Surg Am. 1986;11:258.
4. Palmer AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14:594.
5. Trumble TE, Gilbert M, Vedder N. Arthroscopic repair of the triangular fibrocartilage complex. Arthroscopy. 1996;12:588.
6. Trumble TE, Gilbert M, Vedder N. Isolated tears of the triangular fibrocartilage: management by early arthroscopic repair. J Hand Surg Am. 1997;22:57.
7. Trumble TE, Gilbert M, Vedder N. Ulnar shortening combined with arthroscopic repairs in the delayed management of triangular fibrocartilage complex tears. J Hand Surg Am. 1997;22:807.
8. Labosky DA, Waggy CA. Oblique ulnar shortening osteotomy by a single saw cut. J Hand Surg Am. 1996;21:48.
9. Mikic ZD. Age changes in the triangular fibrocartilage of the wrist joint. J Anat. 1978;126:367.
10. Mikic ZD. Treatment of acute injuries of the triangular fibrocartilage complex associated with distal radioulnar joint instability. J Hand Surg Am. 1995;20:319.
11. Wright TW, Del Charco M, Wheeler D. Incidence of ligament lesions and associated degenerative changes in the elderly wrist. J Hand Surg Am. 1994;19:313.
12. Metz VM, Schratter M, Dock WI, et al. Age-associated changes of the triangular fibrocartilage of the wrist: evaluation of the diagnostic performance of MR imaging. Radiology. 1992;184:217.
13. Geissler WB. Arthroscopically assisted reduction of intra-articular fractures of the distal radius. Hand Clin. 1995;11:19.
14. Geissler WB. Intra-articular distal radius fractures: the role of arthroscopy. Hand Clin. 2005;21:407.
15. Geissler WB, Freeland AE. Arthroscopic management of intra-articular distal radius fractures. Hand Clin. 1999;15:455.
16. Geissler WB, Freeland AE, Savoie FH, et al. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78:357.
17. Varitimidis SE, Basdekis GK, Dailiana ZH, et al. Treatment of intra-articular fractures of the distal radius: fluoroscopic or arthroscopic reduction. J Bone Joint Surg Br. 2008;90:778.
18. Ruch DS, Yang CC, Smith BP. Results of acute arthroscopically repaired triangular fibrocartilage complex injuries associated with intra-articular distal radius fractures. Arthroscopy. 2003;19:511.
19. Lindau T, Arner M, Hagberg L. Intraarticular lesions in distal fractures of the radius in young adults: a descriptive arthroscopic study in 50 patients. J Bone Joint Surg Br. 1997;22:638.
20. de Araujo W, Poehling GG, Kuzma GR. New Tuohy needle technique for triangular fibrocartilage complex repair: preliminary studies. Arthroscopy. 1996;12:699.
21. Palmer AK, Glisson RR, Werner FW. Relationship between ulnar variance and triangular fibrocartilage complex thickness. J Hand Surg Am. 1984;9:681.
22. Tatebe M, Horii E, Nakao E, et al. Repair of the triangular fibrocartilage complex after ulnar-shortening osteotomy: second-look arthroscopy. J Hand Surg Am. 2007;32:445.
22a. Richards RS, Bennett JD, Roth JH, Milne KJr. Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. J Hand Surg Am. 1997;22:772.
23. Bombaci H, Polat A, Deniz G, et al. The value of plain x-rays in predicting TFCC injury after distal radial fractures. J Hand Surg Eur. 2008;33:322.
24. Brown JA, Janzen DL, Adler BD, et al. Arthrography of the contralateral, asymptomatic wrist in patients with unilateral wrist pain. Can Assoc Radiol J. 1994;45:292.
25. Cerofolini E, Luchetti R, Pederzini L, et al. MR evaluation of triangular fibrocartilage complex tears in the wrist: comparison with arthrography and arthroscopy. J Comput Assist Tomogr. 1990;14:963.
26. Levinsohn EM, Palmer AK, Coren AB, et al. Wrist arthrography: the value of the three compartment injection technique. Skeletal Radiol. 1987;16:539.
27. Levinsohn EM, Rosen ID, Palmer AK. Wrist arthrography: value of the three-compartment injection method. Radiology. 1991;179:231.
28. Cooney WP, Linscheid RL, Dobyns JH. Triangular fibrocartilage tears. J Hand Surg Am. 1994;19:143.
29. Tanaka T, Amadio PC, Zhao C, et al. Effect of wrist and ulna head position on gliding resistance of the extensor digitorum minimi and extensor digitorum communis III tendons: a cadaver study. J Orthop Res. 2006;24:757.
30. Golimbu CN, Firooznia H, Melone CPJr, et al. Tears of the triangular fibrocartilage of the wrist: MR imaging. Radiology. 1989;173:731.
31. Joshy S, Ghosh S, Lee K, et al. Accuracy of direct magnetic resonance arthrography in the diagnosis of triangular fibrocartilage complex tears of the wrist. Int Orthop. 2008;32:251.
32. Skahen JR3rd, Palmer AK, Levinsohn EM, et al. Magnetic resonance imaging of the triangular fibrocartilage complex. J Hand Surg Am. 1990;15:552.
33. Anderson ML, Skinner JA, Felmlee JP, et al. Diagnostic comparison of 1.5 Tesla and 3.0 Tesla preoperative MRI of the wrist in patients with ulnar-sided wrist pain. J Hand Surg Am. 2008;33:1153.
34. Fulcher SM, Poehling GG. The role of operative arthroscopy for the diagnosis and treatment of lesions about the distal ulna. Hand Clin. 1998;14:285.
35. Osterman A, Bednar M, Gambin K, et al. The natural history of untreated symptomatic tears in the triangular fibrocartilage. Paper presented at the 51st annual meeting of the American Society for Surgery of the Hand. Nashville, TN: Osterman A, Bednar M, Gambin K; October 1996.
36. Blackwell RE, Jemison DM, Foy BD. The holmium:yttrium-aluminum-garnet laser in wrist arthroscopy: a five-year experience in the treatment of central triangular fibrocartilage complex tears by partial excision. J Hand Surg Am. 2001;26:77.
37. Minami A, Ishikawa J, Suenaga N, et al. Clinical results of treatment of triangular fibrocartilage complex tears by arthroscopic debridement. J Hand Surg Am. 1996;21:406.
38. Hulsizer D, Weiss AP, Akelman E. Ulna-shortening osteotomy after failed arthroscopic debridement of the triangular fibrocartilage complex. J Hand Surg Am. 1997;22:694.
39. Hermansdorfer JD, Kleinman WB. Management of chronic peripheral tears of the triangular fibrocartilage complex. J Hand Surg Am. 1991;16:340.
40. Corso SJ, Savoie FH, Geissler WB, et al. Arthroscopic repair of peripheral avulsions of the triangular fibrocartilage complex of the wrist: a multicenter study. Arthroscopy. 1997;13:78.
41. Millants P, De Smet L, Van Ransbeeck H. Outcome study of arthroscopic suturing of ulnar avulsions of the triangular fibrocartilage complex of the wrist. Chir Main. 2002;21:298.
42. Degreef I, Welters H, Milants P, et al. Disability and function after arthroscopic repair of ulnar avulsions of the triangular fibrocartilage complex of the wrist. Acta Orthop Belg. 2005;71:289.
43. Estrella EP, Hung LK, Ho PC, et al. Arthroscopic repair of triangular fibrocartilage complex tears. Arthroscopy. 2007;23:729.
44. Shih JT, Lee HM, Tan CM. Early isolated triangular fibrocartilage complex tears: management by arthroscopic repair. J Trauma. 2002;53:922.
45. Baek GH, Chung MS, Lee YH, et al. Ulnar shortening osteotomy in idiopathic ulnar impaction syndrome. J Bone Joint Surg Am. 2005;87:2649.
46. Bernstein MA, Nagle DJ, Martinez A, et al. A comparison of combined arthroscopic triangular fibrocartilage complex debridement and arthroscopic wafer distal ulna resection versus arthroscopic triangular fibrocartilage complex debridement and ulnar shortening osteotomy for ulnocarpal abutment syndrome. Arthroscopy. 2004;20:392.