Chapter 10. Injuries to the face, head and spine
Facial injuries
Facial injuries are complex, dangerous and best dealt with by faciomaxillary or plastic surgeons, but they must first be recognized in the accident department.
Nose
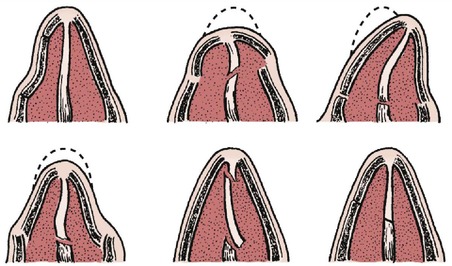
Fractures of the nasal cartilages and nasal bone are common and leave a deformity if not correctly treated. There are several different types of fracture, and not all ‘broken noses’ are the same (Fig. 10.1). If a nasal fracture is suspected, hold the patient’s nose gently and move it slightly. Pain or abnormal movement indicates a fracture.
 |
| Fig. 10.1
Six types of nasal fracture. Each requires slightly different treatment and has a different prognosis.
|
Treatment
Treatment depends on the pattern of the fracture. Dislocations or displaced fractures of the nasal bones need to be repositioned accurately. If a deformity is to be avoided, treatment is best carried out by facial, ENT or plastic surgeons.
Zygoma
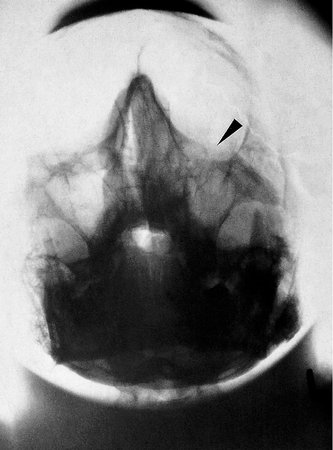
The zygoma can be fractured by a direct blow to the face and the injury is often missed because of soft tissue swelling. A depressed zygoma (Fig. 10.2) can be identified by inspecting the patient’s face from above, bearing in mind that almost every face is slightly asymmetrical, and by palpation.
 |
| Fig. 10.2
A depressed zygoma with an opaque antrum.
|
Untreated, a fractured zygoma leaves a flattened cheekbone, a depression in the floor of the orbit, which can result in diplopia, and damage to the infraorbital nerve. Always look for a fracture of the zygoma if there is a bruise over the cheekbone or a lateral subconjunctival haemorrhage.
Treatment
Once diagnosed, the fragment needs repositioning and sometimes fixation with wires or external fixation.
Orbital fractures
Orbital fractures are difficult to recognize but should be suspected if there has been direct trauma to the orbit or eye. A ‘blow-out’ fracture, in which the small muscles of the eye can be caught in a fracture of the floor of the orbit, is particularly serious. Diplopia and the abnormal position of the eye should lead to the diagnosis.
Treatment
Treatment should be carried out by facial surgeons.
Mandible
Dislocations of the temporomandibular joint can follow direct or indirect trauma, or even a wide yawn. Dislocations can usually be reduced easily, but only if the mandible is intact.
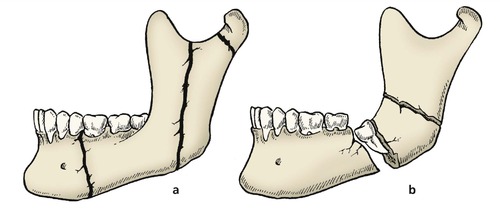
The mandible can fracture through its neck, body, symphysis or ramus (Fig. 10.3), and the fracture can be recognized by tenderness when the mandible is palpated or squeezed gently, and by a deranged dental occlusion. Fractures of the mandible often happen during a fight, sometimes after drinking. Aggressive drunks seldom like their painful jaws being palpated and the fracture can be missed. Radiographs are essential if a fractured mandible is suspected (Fig. 10.4).
 |
| Fig. 10.3
Fractures of the mandible: (a) undisplaced fractures of the ramus, body and neck; (b) displaced fracture with impacted tooth.
|
 |
| Fig. 10.4
Fracture of the mandibular ramus ( arrowed) and the arch of the mandible caused by a blow to the point of the chin.
|
Soft tissue swelling round a fractured mandible can obstruct the airway. This is particularly serious if the patient vomits and lapses into unconsciousness, as inebriated patients often do.
Treatment
Faciomaxillary surgeons are usually responsible for treating these fractures, which may require internal fixation, interdental wiring (Fig. 10.5) or dental treatment.
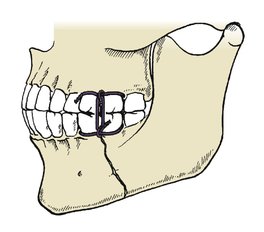 |
| Fig. 10.5
Interdental wiring for fractured mandible.
|
Maxilla
Le Fort classification of maxillary fractures
Maxillary fractures were divided into three main types by Le Fort, a French surgeon of the early 20th century who broke the faces of corpses with a cudgel to study the fracture lines. His classification is as follows (Fig. 10.6):
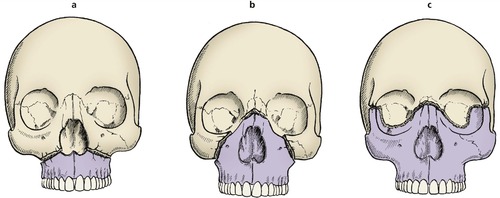 |
| Fig. 10.6
Le Fort facial fractures: (a) Le Fort 1; (b) Le Fort 2; (c) Le Fort 3.
|
• Le Fort 1 – through the maxilla, leaving the nose and orbits intact.
• Le Fort 2 – through the maxilla into the orbits and across the nose, leaving the middle third of the face mobile.
• Le Fort 3 – through the lateral wall of the orbit and across the nose.
All maxillary fractures require urgent attention because the middle third of the face may be unstable and can fall backwards to obstruct the airway. Tracheostomy may be needed.
Because facial injuries are, by definition, head injuries, they are often seen in unconscious patients with brain damage. Always look at the maxillary antrum on the skull radiograph of patients with head injuries; if it is opaque, it is probably full of blood and there is a maxillary fracture.
Treatment
When the airway is secure, the fracture can be treated by the appropriate specialists. External fixation to the skull is often required to hold the displaced fragments in their correct position.
Head injuries
Injuries to the head cause brain damage, the severity of which depends on the energy absorbed by the brain and not by the skull. A skull can be crushed between two fixed objects with surprisingly little brain damage; however, rapid deceleration causing nothing more than an undisplaced linear fracture may be associated with severe brain damage (Fig. 10.7).
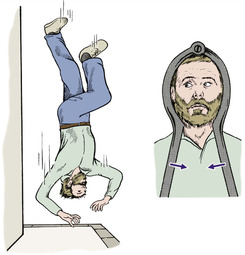 |
| Fig. 10.7
Brain injury and head injuries. Rapid deceleration causes more cerebral damage than a crushing fracture with little deceleration.
|
Pathology
Trauma causes primary and secondary brain damage (Fig. 10.8).
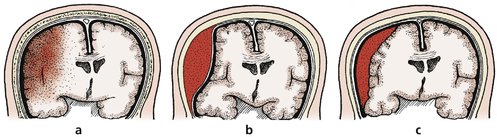 |
| Fig. 10.8
Types of brain damage: (a) brain contusion with bleeding and oedema; (b) extradural haemorrhage; (c) subdural haemorrhage.
|
Primary
• Contusion or laceration caused by violent impact of the brain against the skull, either at the point of injury or directly opposite to it, a contrecoup injury.
• Penetration of the skull and direct damage to the brain.
Secondary
• Oedema of the brain.
• Extradural haemorrhage.
• Subdural haemorrhage.
Clinical presentation
From a clinical standpoint, there are three main types of brain injury: concussion, contusion and compression.
Concussion
Concussion is a transient loss of consciousness following a blow to the head. Recovery is usual. The duration of amnesia following the blow is a good guide to the severity of injury. A boxer who is knocked out in a fight has concussion.
Contusion
There is damage to cerebral tissue from localized bleeding or oedema. Recovery is slower than after concussion and may be incomplete, leaving a neurological deficit.
Compression
Compression is usually caused by bleeding into the skull. As the bleeding continues, the brain is compressed and the clinical condition becomes worse. Decompression and arrest of the bleeding can be life saving.
Patients with concussion and contusion are at their worst immediately after injury and then recover. Compression causes steady deterioration instead of recovery, although there may be a lucid interval.
Management of head injuries
Distinguishing between concussion, contusion and compression depends upon careful monitoring of cerebral function. The level of consciousness and the eye signs are the most reliable clinical signs.
Level of consciousness
The level of consciousness must be recorded carefully so that any deterioration can be identified quickly. It is not enough to record that the patient is ‘awake’ or ‘unconscious’. A fully conscious patient will be alert and oriented in time and space; i.e. will know where he or she is, what time it is, and will be able to hold a normal conversation.
At the other extreme, the patient will be unrousable and not responding to painful stimuli. Between these two extremes, the level of consciousness may be graded as follows:
• Alert and oriented.
• Drowsy.
• Reacts to movement.
• Reacts to painful stimulus.
• Unrousable.
A more accurate assessment is possible with the Glasgow coma scale (Table 10.1).
| Score | ||
|---|---|---|
| Eye opening | Spontaneous | 4 |
| To voice | 3 | |
| To pain | 2 | |
| None | 1 | |
| Verbal response | Oriented | 5 |
| Confused | 4 | |
| Inappropriate words | 3 | |
| Incomprehensible sounds | 2 | |
| None | 1 | |
| Motor response | Obeys command | 6 |
| Localizes pain | 5 | |
| Withdraw (pain) | 4 | |
| Flexion (pain) | 3 | |
| Extension (pain) | 2 | |
| None | 1 | |
| TOTAL | ||
| Glasgow coma scale | ||
| Score | ||
| 14–15 = 5 | ||
| 11–13 = 4 | ||
| 8–10 = 3 | ||
| 5–7 = 2 | ||
| 3–4 = 1 |
Eye signs. Raised intracranial pressure impairs the function of the iris on the side of the lesion. The size of the pupil and its reaction to light is recorded as a sign of intracranial bleeding. A fixed dilated pupil indicates an urgent problem.
Temperature. The thermoregulatory mechanism may be damaged in brain injury and the body temperature may rise. The temperature may need to be controlled by fans or tepid sponging.
Open fractures of the skull
Penetration of the skull always requires exploration by a neurological surgeon to remove dead bone, foreign matter and dead brain. Scalp wounds must not be sutured in the accident department if there is a depressed fracture under the wound.
Cerebral oedema (Fig. 10.9)
Cerebral oedema follows any major head injury and can be reduced with diuretics, such as a mannitol infusion, or by controlled hyperventilation with the patient paralysed and ventilated. This treatment is best conducted in a dedicated neurosurgical unit.
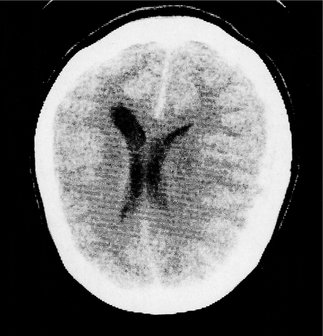 |
| Fig. 10.9
CT scan showing displacement of the midline from cerebral oedema.
|
Extradural haematoma
The classic story of an extradural haematoma is the patient who walks into hospital after a minor head injury and gives a clear, sensible history. The radiograph shows a small temporal fracture. The patient is discharged home, lapses into unconsciousness and is found dead the following morning. This is a constant nightmare for those who treat head injuries. Extradural haemorrhage can be caused by damage to the middle meningeal artery. As the artery bleeds, a haematoma develops and the brain is gradually compressed. The level of consciousness slowly deteroriates until the patient becomes unrousable. If the diagnosis is made soon enough, the haematoma should be evacuated through a burr hole and the artery tied.
In days gone by, it was safer to drill burr holes than risk missing an extradural bleed but with the advent of CT scanning this complication should not take the surgeon by surprise. CT scanning is now an essential part of the management of head injuries and will show areas of brain damage as well as extradural haematomas and the position of the falx (Fig. 10.10).
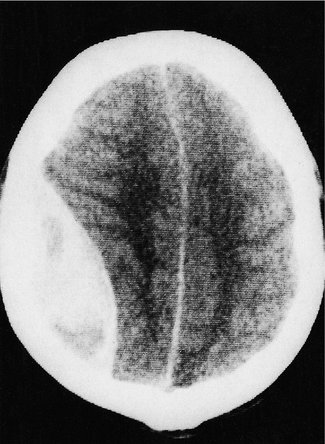 |
| Fig. 10.10
CT scan showing an extradural haematoma, with shift of the midline to the opposite side.
|
Although these investigations are reliable, ligation of the middle meningeal artery can be life saving and the correct site for the burr hole should be memorized by everyone who may be exposed to the treatment of patients with an extradural haematoma. The middle meningeal artery crosses the pterion, which lies two fingers above the zygoma and three fingers behind the orbit (also see Fig. 10.11). The artery can be found either by exposing the fracture and nibbling away the edges of the skull, or by making a burr hole at the pterion itself.
 |
| Fig. 10.11
The pterion. The middle meningeal artery crosses the pterion; it can be identified with the thumb and fingers as indicated.
|
Subdural haemorrhage
Acute subdural haematomas usually accumulate slowly and cause more gradual loss of consciousness than an extradural haematoma. The cause is the gradual enlargement of a blood clot beneath the dura. As the clot liquefies, serum is drawn into its centre and it gradually increases in size. A chronic subdural haematoma is not a clinical emergency but any patient whose level of consciousness deteriorates in the weeks following a head injury should have a CT scan.
Post-traumatic amnesia
The fact that a patient appears alert and oriented does not exclude brain damage. It is by no means uncommon to find that patients who have been unconscious for only a few minutes are unable to recall events for several days after their accident.
The period of post-traumatic amnesia is a reliable guide to the severity of the head injury:
1. Patients with less than 24 h post-traumatic amnesia can expect complete recovery.
2. Those with a post-traumatic amnesia of 1 week usually have some permanent impairment.
CSF rhinorrhoea and otorrhoea
Cerebrospinal fluid (CSF) can leak from nose or ears if the fracture enters the subdural space. The leak usually ceases spontaneously but if it is profuse or persists for more than 2 weeks the defect in the dura may need to be patched with fascia.
Late sequelae
The long-term results of brain damage include continued neurological deficits, personality change, epilepsy, and serious physical disabilities requiring long-term care and rehabilitation.
Decisions in management
There are three very practical decisions in the management of head injury: when to request a skull radiograph, when to admit the patient and when to consult a neurosurgeon.
Skull radiograph
Indications for requesting a skull radiograph:
• Loss of consciousness or amnesia at any time.
• Abnormal neurological symptoms or signs.
• Suspected penetrating injury, swelling or scalp bruising but not a simple laceration.
• Intoxication.
• Difficulties in assessment, e.g. epilepsy, mental subnormality and the very young.
Indications for admission following head injury
Admission is indicated in the following circumstances:
• Confusion or impaired consciousness at the time of examination.
• Skull fracture.
• Abnormal neurological signs, headache or vomiting.
• Difficulties in assessment, e.g. epilepsy, mental subnormality and the very young.
• Other medical conditions, e.g. haemophilia.
• Bad social conditions or lack of responsible adult or relative.
Neurosurgical assistance
A neurosurgeon should be consulted in the following circumstances:
• Skull fracture and (1) confusion and impaired consciousness, or (2) focal neurological signs, or (3) fits.
• Confusion or neurological signs lasting more than 12 h.
• Coma continuing after resuscitation.
• Suspected open fracture of the vault or base of the skull.
• Depressed skull fracture.
• Deterioration in the level of consciousness or neurological signs.
Cervical spine injuries
A ‘broken neck’ has sinister connotations but not all cervical spine injuries have serious complications. Some are undisplaced and a few lucky patients sustain a potentially serious fracture without neurological damage.
Fractures of the spine are managed just as fractures elsewhere but the consequences of displacing the fragments are more serious.
Handling the patient with a cervical spine injury must be done cautiously to prevent further damage to the cervical cord. Even though the greatest damage occurs at the moment of impact, when the neck has been subjected to enough force to break bones and tear soft tissues, careless movements must be avoided.
It is very unlikely that careful handling can do more harm than the original injury if the patient is conscious and there is protective muscle spasm. Damage to the cervical cord following a spinal injury is unusual in the conscious patient.
This is not true for the unconscious patient. Many neurologically intact patients have probably been rendered paraplegic by careless handling and enthusiastic first aid.
Cervical injuries can be caused in four ways:
|
1. Flexion.
2. Extension.
|
3. Vertical compression.
4. Rotation.
|
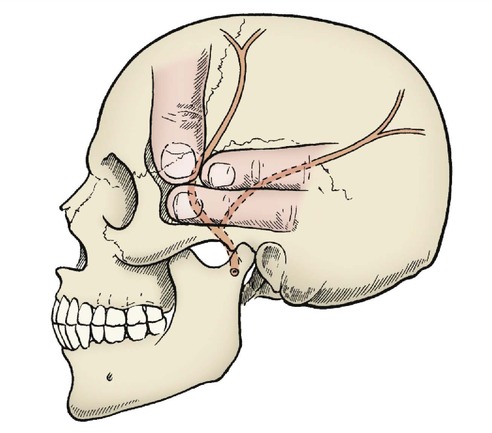
Flexion injuries
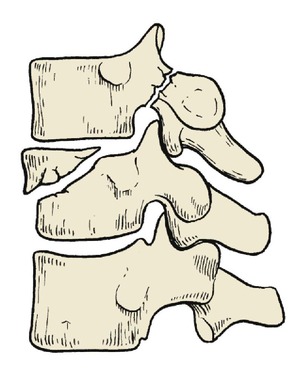
Flexion is involved in the commonest and most serious cervical injuries, usually seen in the lower part of the cervical spine. The following are the commonest lesions (Fig. 10.12):
 |
| Fig. 10.12
Injuries of the cervical spine: (a) a flexion injury with crush fracture of the vertebral body and rupture of the supraspinous ligament; (b) locked facets; (c) locked facets with fracture of the vertebral body.
|
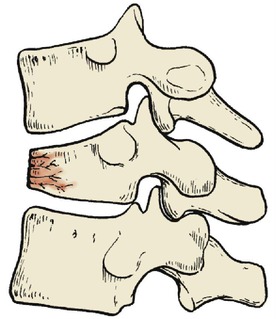
• Crush fracture of the vertebral body (Fig. 10.13).
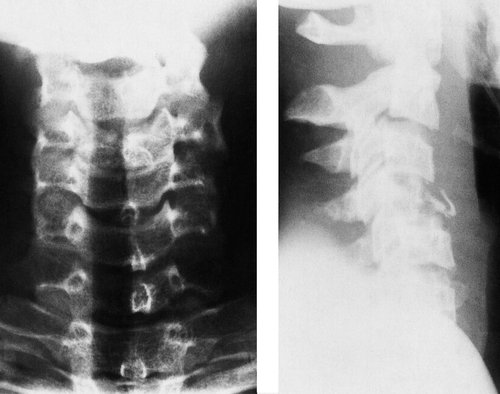 |
| Fig. 10.13
Anteroposterior and lateral views of a crush fracture of the vertebral body. Note (1) that the cervical spines do not form a straight line and (2) the split in the body of C3 on the anteroposterior view.
|
• Rupture of the supraspinous ligament, making the spine unstable.
• Dislocation of the posterior facets.
• Dislocation with fracture of the vertebral body.
Crush fractures
Crush fractures are the result of vertical compression as well as flexion. They are stable but cause severe pain in the neck.
Treatment. Symptomatic relief with a four-post collar or cast and analgesia for approximately 6 weeks is all that is required (Fig. 10.14).
 |
| Fig. 10.14
A four-post collar.
|
Rupture of the supraspinous ligament
Violent flexion of the neck can tear the supraspinous ligament or avulse a spinous process. The fact that the radiographs may show little bony injury is deceptive. The posterior part of the cervical spine may be grossly unstable and neurological damage can occur if the flexion force is repeated.
Treatment. A supporting collar to hold the cervical spine in extension while the soft tissues heal is adequate.
Dislocations
Forward flexion with rotation may cause one or both of the posterior facet joints to ‘jump’ over the edge of the facet below and dislocate (Fig. 10.15). The dislocation cannot occur without associated soft tissue injury but neurological damage is unusual after a simple facet dislocation.
 |
| Fig. 10.15
Locked facets. A line drawn down the front of the vertebral bodies has a sharp step between C5 and C6.
|
Treatment. A simple dislocation can be treated either by traction or careful manipulative reduction, but this should only be done by an experienced surgeon with special knowledge of spinal disorders.
Fracture dislocations
Fracture dislocations in which the vertebral bodies and the facet joints are disrupted often lead to paraplegia and are usually caused by a fall onto the head, e.g. falling off a horse.
Treatment. The fracture must be reduced and held stable, either by traction or fixation, until it has united. Radiographs taken in flexion and extension are useful in determining the progress of bone union. These views should not be attempted within 6 weeks of injury in case the cervical cord is damaged.
Traction applied with a halter is a useful temporary measure but the pressure on the jaw is uncomfortable for long periods and prevents the patient eating. Skull traction, like skeletal traction in general, is much more acceptable to the patient and is applied through tongs attached to the skull.
Hyperextension must be avoided and traction should be applied in the line of the dislocated segment, not the normal line of the neck.
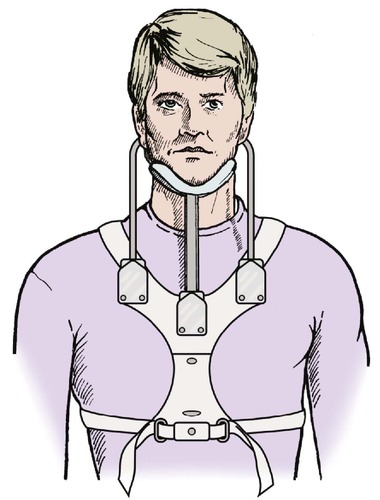
External fixation can be applied to the neck with a halo screwed to the outer cortex of the skull and supported on metal rods attached to a rigid ‘vest’ (‘vest’ is American for waistcoat) (Fig. 10.16). ‘Halo-vest’ traction is used for unstable fractures, but those which are less unstable may be treated in a firm four-post collar.
 |
| Fig. 10.16
‘Halo-vest’ traction. A halo fixed to the skull and attached to bars mounted on a chest piece.
|
Internal fixation may be required to fix the unstable levels of the cervical spine. The operation must be carefully planned so that the exposure does not make the cervical spine completely unstable. If, for example, a hyperextension injury has occurred, the tissues in the front of the cervical spine will be damaged and exploring the spine from behind will weaken the posterior structures as well, leaving little to hold the vertebrae together and the head with no visible means of support.
Cast immobilization of the neck is also possible but is now largely historical (Fig. 10.17). A Minerva cast was used, named after the incident when the demigod Vulcan (himself reputed to have a club foot) split Jupiter’s skull to relieve his headache. Minerva sprang out, fully armed, wearing a heavy metal helmet and singing triumphantly.
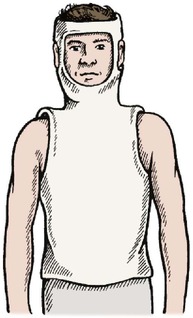 |
| Fig. 10.17
Minerva cast.
|
The cast was modelled on the helmet and was applied to the head rather like a balaclava helmet extending down onto the chest, but it was heavy and restricted movement of both chest and jaw. A four-post collar is both more effective and more comfortable.
Extension injuries
Extension injuries are far more common in the upper cervical spine. The range of flexion is limited by the chin striking the chest but extension has no such natural protection.
Extension injuries are generally less serious than flexion injuries, but serious injuries can occur. The four commonest injuries are:
1. Fracture of the odontoid process.
2. Hangman’s fracture.
3. Kinking of the posterior longitudinal ligament, which can damage the anterior spinal artery and cause anterior spinal artery syndrome.
4. Fracture of the vertebral body with disc prolapse (Fig. 10.18).
 |
| Fig. 10.18
Fracture of the vertebral body with disc prolapse. A hyperextension injury.
|
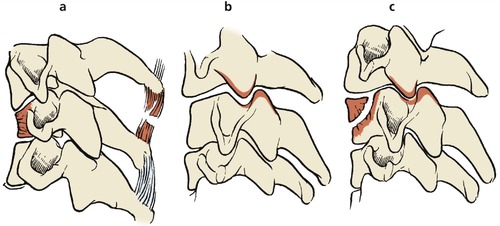
Fracture of the odontoid process
Fractures of the odontoid process, or dens, are difficult to diagnose and are often missed in accident departments. The fracture causes a feeling of unsteadiness in the neck and pain at the base of the skull. These symptoms should suggest the diagnosis.
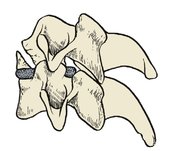
There are three types of fracture (Fig. 10.19). Type II fractures, in the middle of the dens, have a roughly 50% incidence of non-union and may need atlantoaxial fusion to stabilize the neck.
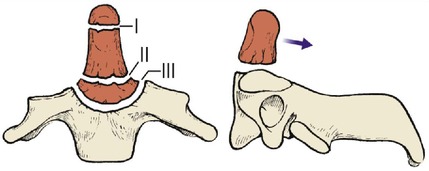 |
| Fig. 10.19
Fracture of the odontoid process. Three types of fracture are seen, involving the base, middle and apex.
|
Hangman’s fracture
Judicial hanging fractures the spine by distraction and hyperextension. Similar forces can be applied in falls or by patients slipping under seat-belts. The fracture usually occurs through the pedicles of C2 and is a traumatic spondylolisthesis of C2 on C3 (Fig. 10.20).
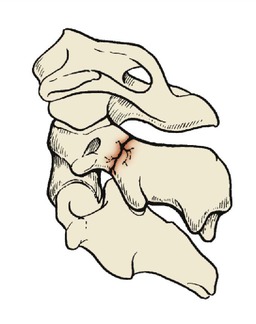 |
| Fig. 10.20
Hangman’s fracture. A fracture through the pars interarticularis of the second cervical vertebra.
|
Treatment. The fracture should be managed by holding the head steady, with the minimum of traction. Too much traction can cause neurological damage: that is how hanging kills.
Anterior spinal artery syndrome
Hyperextension in the degenerate cervical spine of the elderly may kink the posterior longitudinal ligament and this can compress the anterior spinal artery (Fig. 10.21), leading to central cord damage. The result is weakness and sensory symptoms in the upper limbs with sparing of the lower limbs, sometimes accompanied by poor bladder control.
 |
| Fig. 10.21
Anterior spinal artery compression. Kinking of the posterior longitudinal ligament in an elderly patient can cause pressure on the front of the spinal cord and damage to the anterior spinal artery.
|
Treatment. Immobilization in a collar is all that can be offered.
Fracture of vertebra with disc prolapse
These lesions may cause permanent damage to the spinal cord.
Treatment. Urgent decompression and stabilization is required in cases where CT scans confirm the diagnosis.
Fractures caused by vertical compression
True axial compression is an uncommon force. Most impacts are either just in front of the axis of rotation and cause flexion, or just behind, when they cause extension. Two fractures can be caused by vertical forces.
Fracture of the atlas (Fig. 10.22)
The ring of the atlas can be disrupted by a vertical compressive force, often caused by something landing on the head or the patient falling directly onto the vertex.
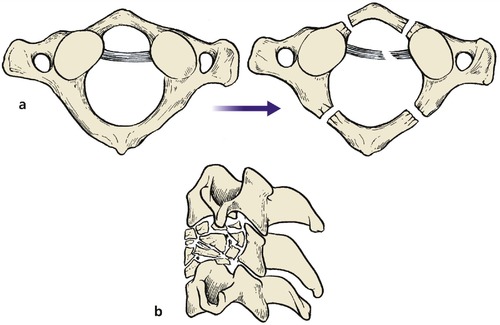 |
| Fig. 10.22
Burst fracture of the atlas (a) and axis (b).
|
Treatment. The fracture should be immobilized in a halo-vest for approximately 6 weeks, followed by a collar for another 2 weeks.
Burst fracture
Vertical compression can disrupt the vertebral bodies, and causes severe pain. The fracture must be distinguished from a wedge compression or crush fracture.
Treatment. If there is no neurological damage, a halo-vest for 6 weeks and then a collar is sufficient – as for a fracture of the atlas. If there is neurological damage, the halo-vest is still needed but the paraplegia must also be treated and rehabilitation begun as soon as possible.
Rotation injuries
Most injuries are the result of a combination of forces rather than a simple sagittal or vertical force. Rotational forces are involved in many flexion injuries, particularly those caused by falls onto the head and neck.
Treatment depends on the stability of the fracture and neurological involvement. Fractures with no neurological damage need a halo-vest for 6 weeks and then a collar, while those with a neurological deficit need the same fixation and early rehabilitation for the problems of paraplegia.
‘Whiplash’ (combined extension–flexion) injury
Combined extension–flexion injuries, often called whiplash injuries, are common in road traffic accidents.
When a vehicle is ‘shunted’ from behind, the head of the victim is thrown backwards and the neck hyperextended (Fig. 10.23). In severe cases the anterior longitudinal ligament may be torn and there is bleeding between the ligament and the vertebrae. This may cause enough retropharyngeal swelling to cause dysphagia a few hours after the injury. Head restraints limit the range of hyperextension and minimize the effects of this injury.
 |
| Fig. 10.23
Combined extension–flexion (whiplash) injury of the cervical spine. Movement of the head is limited by a head restraint.
|
In accidents where the vehicle decelerates rapidly at the moment of impact, the head is thrown forward and the cervical spine flexed. The chin will then hit the chest, which limits flexion, and there will be little damage unless the forward movement of the head is so great that there is a longitudinal distraction as well, a little like hanging. This can cause neurological damage. In the recoil from impact the victim is thrown backwards and hyperextension can occur.
Clinical features
There may be no symptoms until 6 or even 12 h after the injury, but patients involved in road traffic accidents are sometimes brought to hospital immediately after the accident before the symptoms have developed. The radiograph is usually normal and the patient may be discharged from the casualty department with a normal X-ray before the onset of symptoms. This may be difficult to explain to sceptical lawyers if the accident becomes the subject of litigation, as many do.
The leading symptoms are pain and stiffness in the neck, accompanied by aching across the shoulders and down the arms, and sometimes dysphagia. Neurological symptoms such as tingling or numbness are sometimes present but usually transient.
The prognosis is notoriously unpredictable. Ninety per cent of patients are free of symptoms within 2 years, but in a very small proportion the symptoms can last for many years. Some patients may be unable to turn the head enough to reverse a car, which may have a serious impact on everyday life and ability to work.
Unfortunately, many patients seeking compensation for their injuries without demonstrable pathology complain of identical symptoms.
Treatment
A soft supporting collar and analgesics have been advocated in the first few days after injury but the collar should be discarded as soon as possible and physiotherapy begun to restore neck movement. If this is not done, the cervical spine may remain stiff and painful.
Thoracic spine injuries
The thoracic spine has little mobility and this rigidity gives it some protection from injury. Combined flexion–extension injuries and dislocation of the facet joints do not occur in the thoracic spine. Although rarer than injuries to other parts of the spine, thoracic spine injuries are generally severe and often cause paraplegia (Fig. 10.24). There are two reasons for this:
1. The spinal canal is narrow relative to the spinal cord.
2. The displacement of the fragments at the fracture may be considerable and this damages the cord.
 |
| Fig. 10.24
A transverse fracture of the thoracic spine. The displacement of the fragments was accompanied by complete transection of the spinal cord.
|
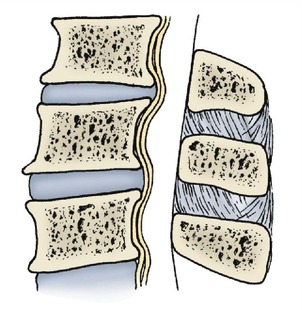
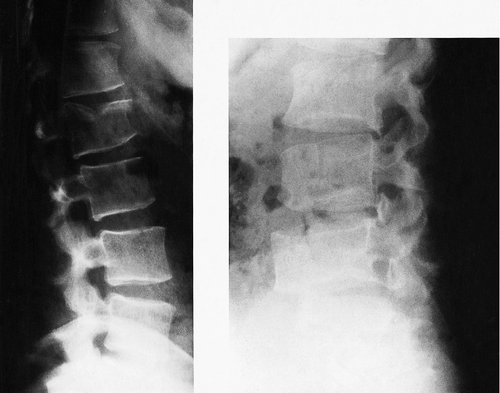
Compression fractures
Compression, or crush, fractures occur at the thoracolumbar junction where the thoracic kyphosis ends and the lumbar lordosis begins. They are caused by a vertical force just in front of the midline of the spine which compresses the anterior lip of the affected vertebra (Fig. 10.25 and Fig. 10.26).
 |
| Fig. 10.25
Compression fracture of a thoracic vertebra.
|
 |
| Fig. 10.26
(a), (b) Two examples of compression fractures of the lumbar vertebrae with less than 50% loss of vertebral height.
|
The injury is commonest in elderly patients with porotic bone who slip and land on their bottom, but it can also occur in younger patients who fall from a height and land on their heels, an injury which also causes a crush fracture of the calcaneum. Pilots who eject from jet aircraft also suffer from this fracture because the upward force of the rockets in the ejector seat is enough to crush the vertebra.
Treatment. The deformity can usually be accepted but if more than 50% of the anterior vertebral height is lost, distraction and internal fixation may be needed (Fig. 10.27). Even in slight deformities, back pain may persist for 2 or more years after injury and sometimes indefinitely.
 |
| Fig. 10.27
Crush fracture of a thoracic vertebra with 50% loss of vertebral height.
|
If there is less than 50% loss of vertebral height, the patient can be mobilized rapidly within the limits of pain.
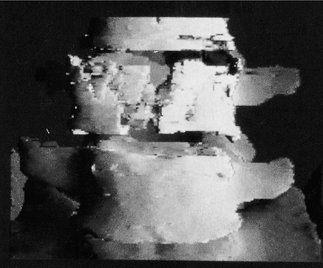
Burst fractures
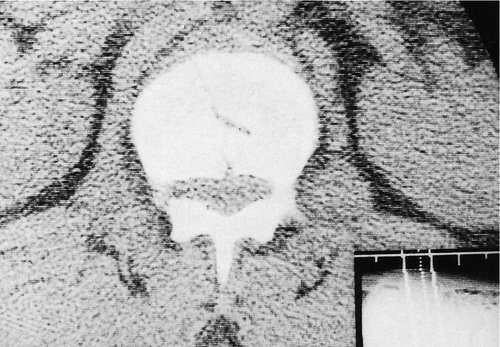
A crush fracture is caused by axial compression of the anterior margin of the vertebra but a burst fracture is the result of a pure axial force. The sides of the vertebra are pushed outwards and disc material may be forced into the vertebral body or the spinal canal (Fig. 10.28). CT scans are invaluable (Fig. 10.29 and Fig. 10.30).
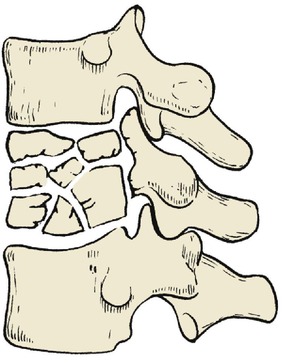 |
| Fig. 10.28
Burst fracture of a thoracic vertebra.
|
 |
| Fig. 10.29
A burst fracture of a vertebral body.
By kind permission of Philips Medical Systems.
|
 |
| Fig. 10.30
CT scan of a burst fracture of a thoracic vertebra with bone fragments pushed backwards into the spinal canal.
|
Burst fractures may be stable or unstable, depending on the pattern of the fracture. They are often associated with neurological damage from backward displacement of the vertebral body or its fragments.
Treatment. Unstable fractures can be treated by bed rest for 6 weeks, brace immobilization or operative fixation. Stable fractures can be mobilized more rapidly, as soon as pain permits.
Seat-belt fractures (flexion–distraction fractures)
Rapid deceleration in a road traffic accident throws the victim forwards against the seat-belt and may cause a flexion–distraction injury. The vertebral body may be split, and displacement can be severe.
Fracture dislocations
Combined flexion, compression and rotational forces occur in many injuries, including the fall of masonry onto the flexed spine and falls from a height (Fig. 10.31). The vertebral body is split, or the pedicles fractured and the facet joints may be dislocated. Paraplegia is usual.
 |
| Fig. 10.31
A fracture of the thoracic spine with oblique fracture of the vertebral body and disruption of the pedicles.
|
Treatment. Fracture dislocations may be treated conservatively or operatively. If the patient is paraplegic, early spinal fusion allows the patient to begin rehabilitation at the earliest possible moment. The onset of paraplegia is a terrible experience for the patient and early rehabilitation helps to give a sense of purpose.
If the patient is not paraplegic, the aim of treatment should be stabilization of the spine to prevent neurological damage. Stabilization can be achieved by immobilization in bed for an extended period of time or by operative fixation to support the spine until union has occurred.
Lumbar spine injuries
Like the cervical spine, the lumbar spine has some mobility and both major and minor fractures occur.
Avulsion of the transverse processes
The transverse processes have powerful muscles attached to them and can be avulsed by violent twisting or flexing movements or by violent muscle spasm such as an epileptic fit. An avulsed transverse process is not a serious injury but the pain and muscle spasm last for 6–8 weeks.
Compression fractures
Compression or crush fractures at the thoracolumbar junction are described on page 159.
Flexion–rotation fractures
Twisting and rotational forces disrupt vertebrae in the lumbar spine (Fig. 10.32), as they do in the thoracic spine (p. 156), and cause neurological damage. Because the spinal cord does not extend below the first lumbar vertebra, only the lower motor neurone and sensory nerves are involved and the neurological problem is very different from the cord injuries of the cervical and thoracic spines.
 |
| Fig. 10.32
Fracture of the pars interarticularis of L5. This is a traumatic spondylolisthesis.
|
Treatment. As in other situations, treatment may be conservative or operative but conservative treatment is the rule because the cauda equina is involved in this region and nerve roots are more robust than the spinal cord. Cauda equina lesions have a much better prognosis than cord lesions.
The large mass of cancellous bone and muscle makes non-union of such fractures unusual but fixation may be required to stabilize an unstable fracture (Fig. 10.33). Details of management depend upon the anatomy and the CT scan.
 |
| Fig. 10.33
CT scan of a fractured vertebra with minimal displacement.
|
Paraplegia
The management of a paraplegic patient is described in many textbooks but must be included here because many paraplegic patients are admitted first to an orthopaedic ward.
Level of the lesion
It is important to establish the neurological level of the lesion. This does not correspond to the vertebral level because the spinal cord is shorter than the spinal column. Nerve roots damaged at the fracture site will have lower motor neurone lesions, and the roots leaving the cord below the fracture site will have upper motor neurone lesions (Fig. 10.34).
 |
| Fig. 10.34
Relationship of spinal cord nerve roots and vertebrae. The spinal cord ends at L1 and injuries below that level involve nerve roots only.
|
The degree of damage must be assessed carefully as soon as possible after injury and reassessed three times each day because the damage may worsen as the spinal cord and soft tissues swell in the days following injury.
Root escape
One of the difficulties in determining the final result is ‘root escape’. The nerve roots are tougher than the spinal cord and it is possible for the cord to be crushed or severed while the roots that cross the fracture remain intact. Surviving roots may not work normally at first because of oedema, axonotmesis or neurapraxia, but recovery from these conditions is possible. The lower the lesion, the more roots are likely to escape damage.
Prognosis
The prognosis depends on the neurological findings 48 h after injury. Patients with complete cord loss at 48 h do not recover but those with some cord function may continue to improve for up to 2 years after injury.
The bladder in paraplegia
There are two main types of bladder dysfunction in paraplegic patients.
Complete denervation
The completely denervated bladder distends without the patient being aware of it and retention with overflow develops. If this is not recognized, back pressure on the kidneys and renal failure may follow. Urinary infection is a serious problem and every care must be taken to prevent it by catheterization with strict sterile technique and careful management.
The automatic bladder
If the bladder retains some autonomic activity, there may be reflex spasm of the detrusor muscle and unexpected emptying of the bladder. As with the completely denervated bladder, the automatic bladder must be catheterized with full sterile precautions.
In the later stages of rehabilitation, the voiding reflex can sometimes be put to good use if it can be initiated by a simple manoeuvre such as pressure on the lower abdomen.
Skin care
Pressure sores occur quickly in areas of insensitive skin. If a paraplegic patient lies immobile for more than 2 h the skin at the point of contact with the bed dies and a pressure sore results. If weight is not taken off the affected area, the subcutaneous tissues also perish, until the skeleton is exposed (Fig. 10.35).
 |
| Fig. 10.35
Deep pressure sore in a paraplegic patient. The femoral head is visible.
|
To prevent this disaster the patients must be turned regularly, at least every 2 h. This involves much heavy lifting, and in some paraplegic units a full-time ‘turning team’ moves around the wards, turning the patients at regular intervals.
Joint stiffness
If joints are not moved regularly, they become stiff. This is a particular problem in paraplegic patients because stiffness makes it impossible to restore movement even if recovery occurs. All the joints must therefore be put through their full range of movement every day to avoid serious contractures.
Muscle spasm is another problem. Muscles with an upper motor neurone lesion contract violently and cause severe cramp-like pain. Muscle relaxants sometimes help but surgical denervation may be required.
Fractures
For reasons that are not known, fractures in paralysed limbs throw out an unusually large mass of new bone and this may restrict joint motion (Fig. 10.36).
 |
| Fig. 10.36
Massive new bone formation around a fracture in a denervated limb.
|
Rehabilitation
The rehabilitation of a paraplegic patient involves not only the body but morale as well. A clear programme of events is essential, and demonstrable progress is more encouraging than anything else. The prospect of a return to competitive sport is especially helpful, and wheelchair games are invaluable (Fig. 10.37).
 |
| Fig. 10.37
A wheelchair race.
|