CHAPTER 77 Injuries of the Lower Cervical Spine
Cervical spine injuries occur in 3% to 4% of all trauma patients.1 Spinal cord injury is much rarer occurring in only about 12,000 people per year in the United States. Because of the association with traumatic brain injury, the risk of spinal injury can be stratified by level of consciousness, occurring in only 2.8% of alert compared with 7.7% of nonevaluable patients.2 It is estimated that about 40% of these injuries will be unstable with potential for neurologic injury.
The importance of the evaluation and protection of the cervical spine is underscored by continued reports of neurologic deterioration that occurs after patients are admitted to hospitals. Levi and colleagues3 retrospectively reviewed 24 cases of patients who deteriorated after admission to level I trauma centers. Neurologic deterioration occurred overall in 0.026% of all trauma patients and 0.21% of patients with known spinal injuries. The common cause was inadequate radiographs, misreading, and poor-quality studies.
Positive changes documenting improvement of the overall care of spinal cord–injured patients have occurred. The time of admission to rehabilitation centers decreased from 23 to 7 days.4 A fivefold decrease in rehabilitation duration has occurred due to better overall management and greater financial constraints. Functional impairment at discharge has seen improvement for three consecutive decades. This is also consistent with decreasing admission of compete quadriplegia compared with increased incomplete quadriplegics. Overall mortality (occurring within the first year postinjury) decreased over 65% from the 1970s to 1990s.5
Many of these improvements resulted from better initial accident care, earlier diagnosis, improved resuscitation methods, and modern surgical techniques. The emergency care of the spinal cord–injured patient is discussed in Chapter 81. This chapter reviews the evaluation of the cervical spine in a trauma patient, new classification systems of lower cervical spine injuries, and their application to surgical decision making.
Anatomy
The anatomy of the cervical spine is reviewed in detail in Chapter 2. These remarks are aimed at the anatomy specific to cervical injuries and their treatment. The subaxial cervical spine is highly mobile but protective of its soft tissue contents, namely the spinal cord, nerve roots, and vertebral arteries. Each vertebra from C3 to 7 is progressively larger and is connected both above and below by three articulations, the disc complex and the paired lateral pillars. These form three columns that are essential for the weight-bearing function of the spine. The anterior column is connected to each lateral pillar by pedicles, and the lateral pillars are connected by the lamina. Thus the lamina and pedicle act as tie-rod connectors. The large spinous processes are levers for attachment of the paraspinal muscles and ligaments. These combined with the nuchal ligaments form the posterior ligamentous complex. which is essential to maintaining stability against flexion and anterior shear forces.
Biomechanics and Kinematics
Kinematically each segment of the subaxial spine normally has approximately 11, 5, and 5 degrees of movement in flexion-extension, lateral bending, and rotation.6 Small amounts (1 to 2 mm) of translation occur in both anterior-posterior and lateral directions. Normal passive motion requires little application of load, which is measured by the neutral zone. Injury will increase the dimension of the neutral zone and when this exceeds certain thresholds such that the neural structures are at risk, the spine is deemed unstable.
Anatomic Considerations for Surgery
Screw fixation into the lateral masses requires identification of a proper starting point and screw direction. The lateral mass is first examined and its borders defined. The cranial and caudal borders are the corresponding facet joints, the lateral border is the edge of the lateral mass, and the medial border is the valley at the junction of the lamina and lateral mass. Several starting points have been described.7–9 However, with modern fixation most authors use a modified technique where the starting point is 1 to 2 mm medial to center of the lateral mass. The author marks this point with a small burr so that when a pilot hole is started it is located at the selected point. The pilot hole is oriented upward attempting to be parallel to the facet articulations and outward about 15 to 30 degrees. This outward orientation is essential to avoid injury to the vertebral artery, which lies directly anterior to the starting point as seen on axial images. The outward angulation is often limited by the next caudal spinous process.
Assessment
Clinical Examination
The clinical examination is an essential component of the evaluation process. It depends on cooperation between examiner and patient, requiring normal mentation. Sensitivity is reduced by the patient’s inability to report symptoms due to conditions such as distracting pain, mild head injuries, or intoxication.10 The clinical examination is performed by reviewing the history of injury and symptoms of cervical pain, numbness, weakness, or paresthesias. The examination assesses spinal tenderness, which is best achieved by carefully logrolling the patient and palpating from the occiput to sacrum. Tenderness, swelling, hematoma, and gaps between spinous processes are indications for further evaluation.
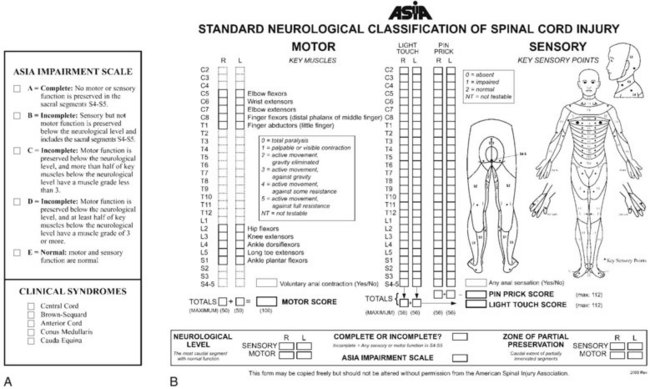
The neurologic examination is performed using standards established by the American Spinal Injury Association (Fig. 77–1).11 These should be recorded in the medical record in a timely manner. The neurologic examination includes testing of cranial nerves, motor and sensory function, and perineal function. Motor function of key muscle groups in the arms and legs are assessed from grades 0 to 5 (Table 77–1). Several sensory functions including pinprick, light touch, and proprioception or vibratory function are tested in both the upper and lower extremities. Sensory function is graded 0, 1, or 2 (absent, hypoesthesia, and normal, respectively). Deep tendon and pathologic reflexes are determined. Hyperreflexia and findings of clonus, Babinski signs, or Hoffmann signs are indications of spinal cord compression, although in cases of acute spinal cord injury areflexia is initially common. The level of spinal cord injury is defined as the lowest-functioning root level with at least grade 3 motor function. Complete spinal cord injuries are defined as the absence of any motor or sensory function including sacral roots distal to the zone of injury. Incomplete cord syndromes have some retained motor or sensory function and have a significantly better prognosis than complete lesions. The overall impairment is graded by the modified Frankel (ASIA) scale: A—motor and sensory complete; B—motor complete with sensory sparing; C—motor and sensory sparing but not functional strength; D—motor and sensory sparing with functional strength; E—normal motor and sensory.11
| Upper Extremity | |
| Biceps | C5 |
| Wrist extension | C6 |
| Triceps | C7 |
| Finger flexion | C8 |
| Finger abduction | T1 |
| Lower Extremity | |
| Iliopsoas | L2 |
| Quadriceps | L3 |
| Anterior tibialis | L4 |
| Extensor hallucis longus | L5 |
| Gastrocsoleus | S1 |
Clearing the Cervical Spine
Patient Presentation
After the clinical examination, a decision is made whether radiologic studies are indicated. To determine the proper course, patients can be divided into one of four groups: asymptomatic; temporarily nonevaluable but asymptomatic; symptomatic; and obtunded. Asymptomatic patients are those who have no pain, no cervical tenderness, neurologic signs and symptoms and who are awake, alert, and nonintoxicated.1 Additionally, they do not have any distracting injuries that may preclude pain assessment of a potential cervical spine injury. Distracting injuries include long bone fractures, burns, visceral injury, dislocations, and craniofacial or thoracic trauma. The temporarily nonevaluable patient is otherwise asymptomatic but is either intoxicated where sobriety is expected within 24 hours or will have resolution of other painful injuries through reduction or fixation. It is hypothesized that these patients can be evaluated similar to the asymptomatic patients in a delayed fashion.12 Symptomatic patients have cervical pain, tenderness, or neurologic symptoms such as paresthesias, weakness, or numbness. The obtunded patient is one who will not be able to fully participate in the clearance process and at the same time is at highest risk for injury. Included in this group are disabled and infant patients.
Asymptomatic Patient
Multiple large multicenter prospective trials, institutional prospective studies, systematic reviews, and meta-analyses demonstrate conclusively that the asymptomatic patient can be cleared after clinical assessment and does not require radiographic evaluation.13–17 Designation as asymptomatic will clear 99.8% of patients without radiographs and use of such protocol only rarely misses a significant injury.13 In more than 62,000 cases, no neurologic complication occurred after clearance of asymptomatic patients on clinical grounds.
Symptomatic Patients
Symptomatic patients are at significant risk of cervical injury and all authorities agree that imaging is required.14,15 In cases of obvious cervical cord injury, this may be by means of a lateral radiograph so that traction can be instituted immediately if a fracture dislocation is present. More commonly, a multidetector CT (MDCT) is performed. MDCT allows acquisition of thin-slice thicknesses (1.25 to 1.5 mm) and affords high-resolution reconstruction in all three planes. Compared with plain radiographs, it has significantly increased sensitivity and is cost effective if CT imaging of other body parts are required.18 Magnetic resonance imaging (MRI) is indicated after CT or plain radiographs when there are unexplained neurologic defects, progressive deterioration, preoperatively, and in cases of facet dislocation of neurologically intact patients. Further, MRI with fat suppression is useful to identify ligamentous disruption, which may aid surgical decision making.
Obtunded Patients
No agreement has been reached as to the best method to evaluate the cervical spine of cognitively impaired patients. However, all stakeholders agree that radiologic evaluation is warranted in this high-risk group.15 Current recommendation is divided into two groups: MDCT alone19,20 and MDCT with MRI.21 MDCT is easy to perform and likely identifies all osseous injuries. However, ligamentous injury may be missed if the spine is reduced in normal alignment. If restrictions are released, then displacement may occur when the patient is no longer immobilized. Given the high resolution of MDCT compared with older CT studies, proponents of this modality believe the risk of this is small. The latter technique takes advantage of both MCDT, which identifies osseous injury, and MRI, which is sensitive for ligamentous injury. A recent meta-analysis shows that MRI has a 100% negative predictive value, indicating that a negative study excludes any significant injury.1 However, there is a high false-positive rate, meaning that many patients will be treated unnecessarily. In the absence of proof of the superiority of either approach, the author recommends that each institution develop and use a protocol to evaluate these patients.
Classification
Classification of spinal injuries is difficult due to the complex anatomy of vertebrae, the presence of a three-joint complex, and the many ligamentous structures responsible for stability. Classification systems can be broadly categorized as morphologic, mechanistic, and by stability. Morphologic systems use common names that describe the pathoanatomy such as burst fracture or facet dislocation. These are useful but do not help to define treatment or imply prognosis. Mechanistic systems attempt to identify force vectors that cause injury.22 Using these, potential treatment strategies can be induced, usually by reversing the vector direction. Stability is hard to define but implies the ability of the spine to withstand physiologic loads. This is well grounded in sound biomechanical principles but is more difficult to use clinically. All of these classification systems have many limitations including not being comprehensive, not aiding treatment decision making, not using modern imaging, and lacking reliability and validity.
Stability and neurologic status are the most important factors when treating patients with cervical spine trauma. Stability was initially described by Nicoll, who identified patterns of injury that were associated with poor functional outcomes (i.e., inability to return to work as a miner).23 He found that posterior ligamentous injuries and dislocations were “unstable patterns.” Stability has been defined by White and Panjabi6 as “ability of the spine under physiologic loads to maintain a relationship between vertebral segments in such a way that there is neither damage nor subsequent irritation of the spinal cord or nerve roots, and, in addition, there is no development of incapacitating deformity or pain due to structural changes.” Stability as thus defined is dichotomous when in fact stability is a continuous variable with many shades of gray. In an effort to quantify clinical stability and thus make it useful for traditional decision making, White and Panjabi6 developed a checklist. Points are assigned for injury to anterior or posterior columns, translation, excessive angulation, distraction, and neurologic injury. Higher scores indicate greater degrees of instability. This concept is well founded with biomechanical studies but has not proven useful as a clinical tool or even been tested for validity.
White and colleagues24 performed elegant biomechanical studies on cadaveric spines with serial ligamentous sectioning. After each ligament was divided, loads were applied and motion measured. They found that the cervical spine developed excessive motions when all elements of one column (anterior or posterior) and one other ligament were sectioned. The amount of displacement at this time was 3.5 mm of translation and 11 degrees of greater angulation than adjacent levels. These parameters were exceeded only after injury and are accepted as rendering the spine unstable clinically. Practically, however, the cases most difficult to assess for stability do not have displacements or angulation exceeding these limits.
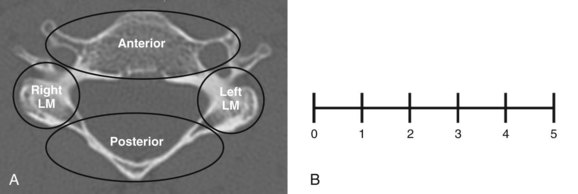
Cervical Spine Injury Severity Score
The Cervical Spine Injury Severity Score (CSISS) is based on independent analysis of four columns (anterior, posterior, right column, and left lateral column) (Table 77–2).25 The anterior column includes the body, disc including the annulus, anterior and posterior longitudinal ligaments, and transverse processes. Each lateral column is scored separately and includes the facet projections, lateral mass, pedicles, and facet joint capsules. The posterior column includes the lamina, spinous process, ligamentum flavum, and nuchal ligaments (Fig. 77–2A).
| CSISS Analog Score | |
|---|---|
| Anterior column | 0-5 |
| Right pillar | 0-5 |
| Left pillar | 0-5 |
| Posterior column | 0-5 |
| Total | 0-20* |
* Scores < 5 are generally treated nonoperatively. Scores > 7 are usually treated surgically.
Each column is scored using a 0-5 analog scale (Fig. 77–2B). Fractional scores can be used. Scores increase proportional to either displacement of fracture fragments or separation as a result of soft tissue injury. For example, a nondisplaced fracture is scored 1 while the worst injury possible for that column (e.g., facet fracture dislocation with 10-mm displacement) is a 5. Each column is scored independently and summed, giving the CSISS ranging 0-20.
Anderson and colleagues25 assessed reliability in 34 cases with 15 examiners. Both intraobserver and interobserver reliability were excellent. Construct validity was also good as all patients with scores equal to 7 had surgery, whereas only 15% less than 5 had surgery (Fig. 77–3). Caput and colleagues26 retrospectively correlated CSISS score to surgical approach in 70 patients. They found a significant correlation with high CSISS scores (>11) to a posterior or combined anteroposterior approach. The anterior approach had lower scores with a mean 6.3, indicating that anterior surgery was used for less severe injuries, in accordance with well-known biomechanical studies.
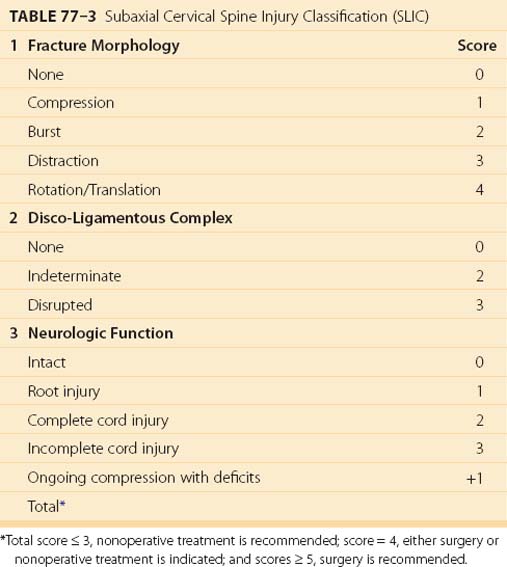
Subaxial Cervical Spine Injury Classification
The Subaxial Cervical Spine Injury Classification system (SLIC) evaluates fracture morphology, the discoligamentous complex, and neurologic function, creating a comprehensive system to aid treatment decision making (Table 77–3).27 The system assigns points for each domain and if the score exceeds a threshold, surgery would be indicated.
Overall Subaxial Cervical Spine Injury Classification Score
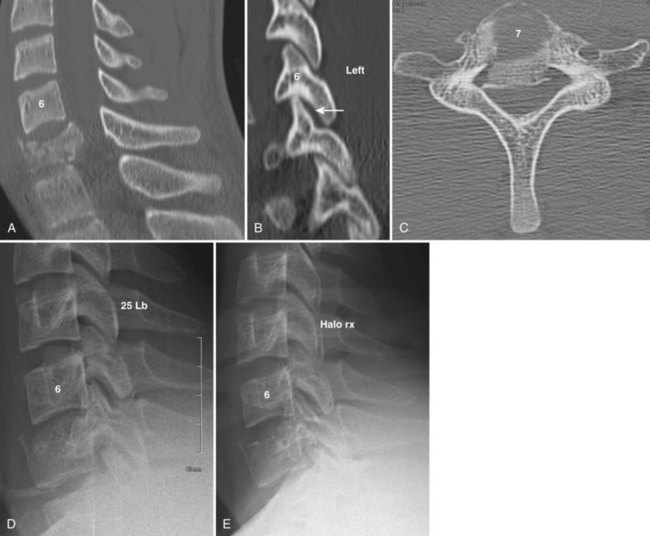
The SLIC score is the sum of the individual components. A patient with an SLIC score equal to 3 is treated nonoperatively, whereas surgery is recommended in a patient with a score equal to 5 (Fig. 77–4). Scores of 4 can be treated either operatively or nonoperatively.
Vaccaro and colleagues27 tested the reliability of the SLIC system. Interobserver reliability was only moderate, and both injury morphology and discoligamentous complex scores were only fair. Intraobserver reliability was excellent for overall and individual components. Similar to the CSISS, the system was valid when tested against treatment decisions. The SLIC system predicted accurately what the individual observers would recommend in 91% of cases.
Specific Injury Types
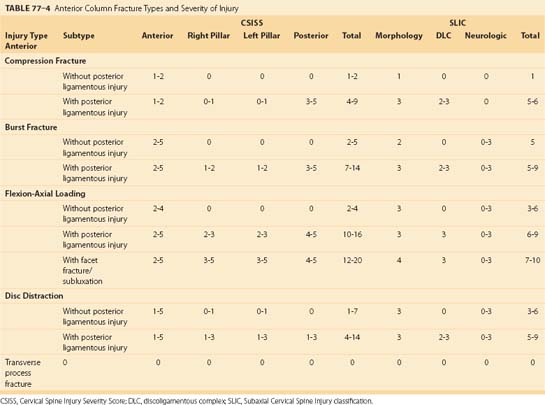
Anterior Column Injuries
Anterior column injuries include compression fractures, burst fractures, flexion axial loading injury, and disc distraction injuries (Table 77–4). Transverse process fractures are included in this group, although they have no effect on spinal stability but may be associated with vertebral artery injury. Most anterior column injuries are easily recognizable on plain radiographs or CT. When present, they suggest a hyperflexion mechanism and a search for a concomitant injury to the posterior ligamentous complex should ensue. The notable exception is the disc-distraction injury resulting from opposite forces (i.e., extension and posterior shear). These injuries can be subtle, especially in patients with preexisting spondylosis.
Anterior Compression Fractures
Mechanism of Injury
Anterior compression fractures, like burst fractures, occur from hyperflexion and/or axial loading forces. During this loading, the disc is pressurized, resulting in failure of the endplate and creating wedging of the vertebral body. This usually occurs along the superior endplate. During hyperflexion the posterior ligaments may be strained beyond physiologic limits, causing disruption. This injury pattern has been termed “hidden flexion injury” and often fails nonoperative treatment.28
Assessment
Isolated compression fractures without posterior or lateral mass involvement almost always score low CSISS (0-2) and SLIC (1) scores (see Table 77–4). When associated with posterior ligamentous injury or facet perching, CSISS and SLIC scores range 7 to 10 and 5 to 6, respectively, indicating a moderate degree of instability.
Burst Fractures
Radiographic Assessment
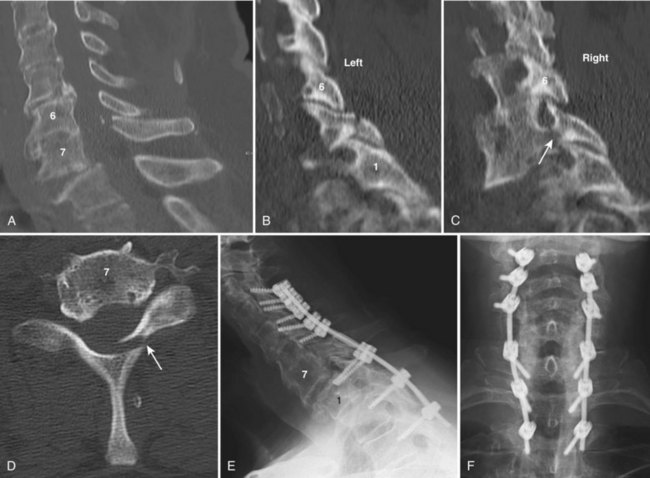
Burst fractures occur most commonly at C6 and C7 rather than the mid or upper cervical spine (see Fig. 77–4). On lateral views, both anterior and posterior vertebral body heights are shortened and a small fragment from the posterior superior body is rotated into the spinal canal. Interspinous widening or facet perching or subluxation, when present, indicate posterior ligamentous injury.
Flexion Axial Loading Injury
Mechanism of Injury
Flexion/axial loading injuries, also called tear drop fractures, are devastating injuries due to the propensity for neurologic injury and often are the result of diving or other sports-related activities. The injury occurs from a compression force obliquely applied in a downward and posterior direction. Forces are concentrated in the anterior inferior corner of the vertebral body, which is sheared off, giving the injury its name (see Fig. 77–3). The remaining part of the vertebral body shears through the disc space and rotates posteriorly into the spinal canal, crushing the spinal cord. Varying amounts of flexion strain occur in the posterior ligamentous complex, which accounts for a wide presentation of stability with this injury.
Assessment
In cases without posterior ligamentous disruption, CSISS scores range from 3 to 5 because of anterior displacement with minimal injury to lateral masses or posterior ligamentous complex. The SLIC score is 3 for a distraction injury with increasing scores being based on neurologic involvement. When associated with posterior ligamentous complex injury or facet fractures/subluxation, high scores on both CSISS and SLIC are present (see Fig. 77–3).
Transverse Process Fractures
Transverse process fractures are quite common, occurring in isolation or in association with other more severe injuries. These fractures are not involved with spinal stability and therefore are not significant in treatment decision making for the spine. However, transverse process fractures at C6 and above may warn of possible vertebral artery injury.29 No consensus has been reached regarding whether routine vascular evaluation and subsequent treatment with anticoagulants are required in patients with these injuries. This topic is discussed in detail in Chapter 82.
Disc-Distraction Injury
Radiographic Analysis
MRI is useful to identify questionable cases. Classic findings are increased signal in anterior soft tissues both rostral and caudal to the injured disc. Increased signal intensity across the disc space transversing the anterior annulus and anterior longitudinal ligament is pathognomonic (Fig. 77–5). Rarely the posterior longitudinal ligament will be involved. Disc herniation and spinal cord compression from stenosis or malalignment may be present as well. Posterior increased signal in the facet joints and ligamentum flavum are indicative of more extensive injury and greater instability.
Treatment of Anterior Column Injuries
Anterior column injuries with low SLIC or CSISS scores can be treated non-operatively (Table 77–5). These include compression injuries, stable forms of burst fractures and flexion/distraction injuries, and most disc-distraction injuries (see Fig. 77–4). Less significant injuries can be treated with a cervical collar, while burst fractures and flexion/axial loading injuries can be treated with a cervical thoracic orthosis (CTO) or halo vest.
| Injury Type | Subtype | Treatment Options |
|---|---|---|
| Compression Fracture | ||
| Without posterior ligamentous injury | COLLAR, CTO | |
| With posterior ligamentous injury | Collar, CTO POSTERIOR FUSION |
|
| Burst Fracture | ||
| Without posterior ligamentous injury | Collar, CTO HALO VEST Posterior fusion Anterior fusion |
|
| With posterior ligamentous injury | Collar, CTO Halo vest Posterior fusion ANTERIOR FUSION Anteroposterior fusion |
|
| Flexion-Axial Loading | ||
| Without posterior ligamentous injury | Collar, CTO HALO VEST Posterior fusion Anterior fusion |
|
| With posterior ligamentous injury | Collar, CTO Halo vest Posterior fusion ANTERIOR FUSION Anteroposterior fusion |
|
| With facet fracture/ subluxation | Collar, CTO Halo vest Posterior fusion Anterior fusion ANTEROPOSTERIOR FUSION |
|
| Disc Distraction Injury | ||
| Without posterior ligamentous injury | COLLAR, CTO | |
| With posterior ligamentous injury | Collar, CTO Halo vest Posterior fusion ANTERIOR FUSION |
|
| Transverse Process Fracture | ||
| No vertebral artery injury | OBSERVATION | |
| Vertebral artery injury | Observation ANTICOAGULATION |
|
CTO, cervicothoracic orthosis.
Authors’ recommendations are in bold capitals.
Surgical indications for anterior column injuries are those with evidence of disruption of the posterior ligamentous complex as demonstrated by high CSISS and SLIC scores (see Table 77–5). In the case of compression fractures when surgery is warranted, the author recommends posterior fusion because a single-level anterior fusion may fail in the face of a vertebral fracture at the location of caudal screw fixation. Burst fractures and flexion/axial loading injuries can be reduced or significantly improved with tong traction. Although both anterior and posterior approaches may be used, the authors recommend addressing pathology at its major location (i.e., anteriorly) (see Fig. 77–3). After strut grafting or insertion of a cage, an anterior plate is applied. Although a rigid locked plate has theoretical advantages over a translational plate, the author has not observed any clinical differences in outcomes between the two plates. In rare cases of extensive comminution, associated facet dislocations, or those having residual displacement of lamina fractures, combined anterior and posterior approaches are indicated.
Outcomes: Anterior Column Injuries
Two nonrandomized clinical trials have compared outcomes of halo vest with anterior decompression and stabilization with a plate for the treatment of cervical burst fracture and flexion distraction injuries. Fisher and colleagues30 noted better radiologic alignment but no differences in pain and function and could not correlate greater kyphosis in the halo group to long-term problems. Approximately 20% of halo patients failed and subsequently required surgery. Koivikko31 found significantly improved neurologic recovery presumably due to the better decompression in operatively managed patients over the halo vest. Toh and colleagues32 compared anterior with posterior stabilization for these injuries. They found better decompression and improved neurologic outcomes in the anterior group. In all of these trials single-stage anterior decompression and plate fixation resulted in successful fusion, satisfactory alignment, and better neurologic recovery.
Vaccaro and colleagues retrospectively reviewed outcomes of 24 patients with disc distraction injuries, 16 of whom were treated surgically by anterior fusion.33 All surgical patients fused, although three patients developed neurologic deterioration from overdistraction of the disc space. These results were similar to those published in a systematic review by Hadley.34 Mortality rate was 38% in operative and 63% in conservatively treated patients secondary to an aged population that sustained spinal cord injuries.
Posterior Column Injuries
Isolated injuries to the posterior column are less common than those that are combined with other fractures. Isolated injuries include spinous process and lamina fractures and disruption of the posterior ligamentous complex without facet subluxation (Table 77–6).
Posterior Ligamentous Injury without Subluxation
Mechanism of Injury
Posterior ligamentous disruptions occur from hyperflexion and are worsened with any rotation.
Treatment of Posterior Column Injuries
Management of isolated spinous process and lamina fractures is with simple collar immobilization (Table 77–7). Because they may be associated with complete posterior ligamentous complex disruption, kyphosis or progressive subluxation may occur. Patients should be informed that spinous process fractures may not heal due to the displacement from muscle contractions, although this rarely leads to chronic pain or further surgical treatment.
| Injury Type | Treatment Options |
|---|---|
| Spinous process fracture | COLLAR, CTO |
| Lamina fracture | COLLAR, CTO |
| Posterior ligamentous injury without subluxation | COLLAR, CTO Posterior fusion Anterior fusion |
CTO, cervicothoracic orthosis.
Authors’ recommendations are in bold capitals.
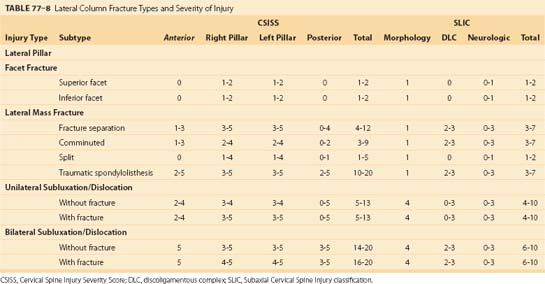
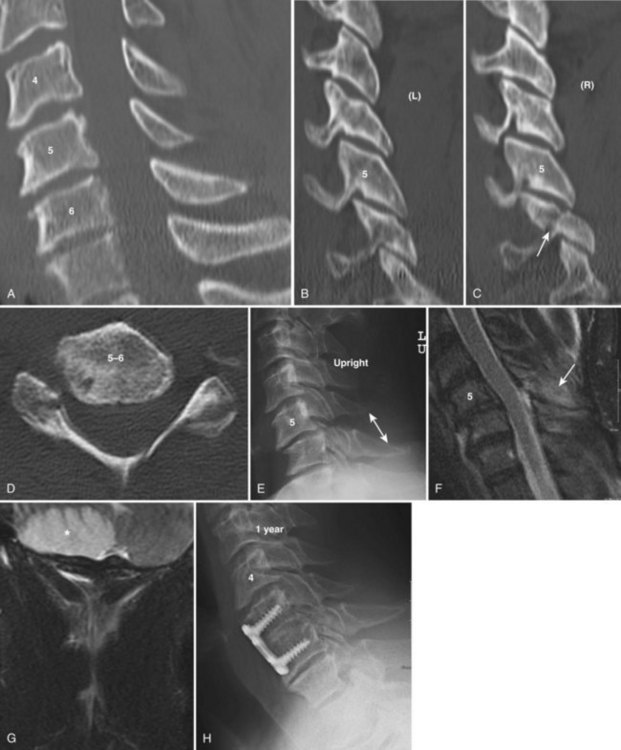
Lateral Column Injuries
Injuries to the lateral column are being recognized more frequently, likely due to better restraint systems that are preventing the more serious injuries and by increasing recognition from the use of diagnostic CT. Anatomically the lateral column consists of the lateral masses with their superior and inferior articular process projections. Lateral column injuries include a wide variety of fracture types including isolated facet fractures without subluxation, lateral mass fractures, and unilateral and bilateral dislocation with and without fractures (Table 77–8).
Isolated Facet Fractures
Mechanism of Injury
Isolated facet fractures occur from forced impaction against the neighboring facet, usually with a component of anterior shear. Thus these may result in loss of the stabilizing buttress to anterior shear and should always be evaluated with the suspicion that greater instability is present (Fig. 77–6).
Lateral Mass Fractures
Radiographic Characteristics
Kotani and colleagues35 identified four types of lateral mass fractures. Type I is a fracture separation. In this injury there is an ipsilateral pedicle and lamina fracture, usually at its junction with the lateral mass creating a free floating lateral mass. Thus separated and free floating, the lateral mass can rotate forward, which allows for anterior subluxation at both cranial and caudal articulations, rendering two motion segments unstable. Type II lateral mass fractures are highly comminuted also with a similar potential as type I for instability. Type III is a vertical fracture in the coronal plane with invagination of the superior facet into the cranial lateral mass. Type IV fractures are traumatic spondylolisthesis, which usually occurs at C7 or T1. This is caused by bilateral fractures of the pedicles or pars interarticularis and vertebral subluxation. Despite significant translation, spinal cord injury may be absent or minimal as the spinal canal opens due to separation of the anterior and posterior components.
Bilateral Facet Dislocation
Mechanism of Injury
Bilateral facet dislocations occur from hyperflexion with or without rotation. There will always be associated disruption of the posterior ligamentous complex. Another potential mechanism has been shown to be cranial impaction with the head slightly flexed, which transmits flexion loads causing facet dislocation.36
Radiographic Analysis
Bilateral facet dislocations result in a minimum of 50% vertebral body translation. Fractures of the facets, lamina, and spinous processes are common. Posterior interspinous widening is usually present. The disc may be inappropriately narrowed, suggesting posterior herniation. The spinal canal is significantly narrowed, accounting for the high incidence of quadriplegia. Disc disruption is almost always present, and nuclear herniation may be present in up to 65% of cases.37
Treatment of Lateral Column Injuries
Isolated Facet Fractures
Isolated facet fractures can be treated nonoperatively with a collar or CTO (Table 77–9). Upright radiographs after bracing should be assessed for increasing kyphosis or subluxation (see Fig. 77–6).
| Injury Type | Subtype | Treatment Options |
|---|---|---|
| Facet Fracture | ||
| Superior | COLLAR, CTO Halo vest |
|
| Inferior | COLLAR, CTO Halo vest |
|
| Lateral Mass Fracture | ||
| Fracture separation | Collar, CTO Halo vest POSTERIOR FUSION Anterior fusion Anteroposterior fusion |
|
| Comminuted | COLLAR, CTO Halo vest Posterior fusion Anterior fusion |
|
| Split | COLLAR, CTO Halo vest Posterior fusion Anterior fusion Anteroposterior fusion |
|
| Traumatic spondylolisthesis | Collar, CTO Halo vest POSTERIOR FUSION Anterior fusion Anteroposterior fusion |
|
| Unilateral Facet Subluxation/Dislocation | ||
| Without fracture | Collar, CTO HALO VEST Posterior fusion Anterior fusion |
|
| With fracture | Halo vest POSTERIOR FUSION ANTERIOR FUSION |
|
| Bilateral Facet Subluxation/Dislocation | ||
| Without disc herniation | POSTERIOR FUSION Anterior fusion Anteroposterior fusion |
|
| With disc herniation | Posterior fusion ANTERIOR FUSION Anteroposterior fusion |
|
CTO, cervicothoracic orthosis.
Authors’ recommendations are in bold capitals.
Facet Dislocations
No consensus has been reached as to the treatment of unilateral facet dislocations.38 Several issues are important to consider. The injury includes disruption of the annulus in almost all cases, and disc herniation occurs in 56% of unilateral and 82.5% of bilateral dislocations.37 These disc herniations have been reported to persist behind the cranial vertebral body, increasing spinal cord compression and neurologic deterioration after reduction.39 To avoid this, several strategies have been recommended. One strategy is to obtain an MRI before any attempt at reduction in the neurologically intact or incomplete patient. If a disc herniation is present, then anterior discectomy is recommended before reduction (Fig. 77–7). In this case, an open reduction can be performed anteriorly with interbody fusion and plate. Alternatively, another strategy in an awake, alert, and cooperative patient is to attempt a closed skeletal reduction before MRI. Both strategies are well accepted methods of treatment. Cranial tong traction can be used with the protocol described as follows. Following any closed reduction, an MRI must always be performed before surgical intervention to access for the presence of a traumatic disc herniation or other space-occupying lesion. In patients with facet dislocations and spinal cord injury, early reduction is recommended before obtaining MRI to assess the disc state.
In patients with reduced unilateral facet dislocations, nonoperative care using a halo vest or CTO can be attempted. If the dislocations cannot be reduced, then open reduction is easily achieved with a posterior approach. Unilateral facet fracture-dislocations are best managed operatively. Recurrence of displacement is likely to occur even after successful closed reduction. This is especially true if the length of the facet fracture exceeds 40% of the total facet height.40 Either anterior discectomy and fusion or posterior fusion can be performed (see Fig. 77–6). In cases of associated vertebral body fractures, posterior surgery is warranted, whereas if comminution is posterior then an anterior fusion should be considered.
In almost all cases bilateral facet dislocations should be treated surgically. Biomechanical studies confirm the advantages of posterior instrumentation over anterior plates. However, this has not been shown to be important clinically.41 Both anterior and posterior fixation with screw fixation is adequate and rarely combined anterior-posterior surgery is necessary. The choice of approach is often dictated by the presence of disc herniation or posterior comminution, which would favor an anterior approach (see Fig. 77–7). Alternatively, the presence of vertebral body fractures would favor a posterior approach. Combined anterior-posterior procedures are indicated when comminution will prevent solid fixation or in cases of extreme ligamentous avulsion such as distraction injury.
Outcomes of Lateral Column Injuries
Long-term outcomes of unilateral facet fracture-dislocations have been investigated. In retrospective case series, Beyer and colleagues correlated pain to residual deformity, which was more common in nonoperatively treated patients.42,43 Lee and Sung compared rotational unstable lateral mass fractures treated nonoperatively with those treated with anterior fixation.44 He found that 12 of 15 patients treated conservatively failed and underwent surgery. Surgical results were excellent except in three cases of type I lateral mass fractures (fracture separations) that had only a single segment fusion and then developed subluxation at adjacent level. Dvorack and colleagues45 reviewed 90 patients (72 operative and 18 nonoperative) at 2 years using health-related quality-of-life assessments. Both groups had more pain and disability than normative subjects adjusted for age. However, operatively treated patients had significantly better SF-36 scores than nonoperatively treated patients. Kwon and colleagues46 performed a randomized controlled trial of unilateral facet dislocations comparing anterior with posterior fixation. He found no significant differences except in higher rates of wound infections in the posterior group and dysphagia in the anterior group. Anterior plate fixation, however, may be associated with failure when used in the presence of vertebral endplate fracture.47
Current management of bilateral facet dislocations is primarily operative, although past descriptions of successful halo-vest treatment have been reported.34 In these series, up to 30% of patients had recurrent deformity and required surgery. Comparisons between operative and nonoperative treatment using modern patient-centered outcomes are not available. Both anterior plate fixation and posterior lateral mass fixation are associated with satisfactory radiologic outcomes.7,34,41,48,49
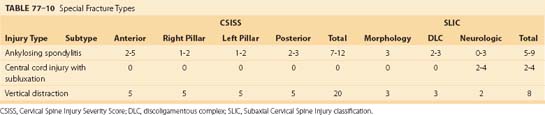
Special Injury Types
Several patterns of injury do not fit conveniently into anatomic categories. These include fractures in ankylosed spines, injuries in patients resulting in central cord syndrome, vertical distraction injuries, and fractures in the elderly (Table 77–10). Fractures in pediatric patients are discussed in Chapter 28.
Ankylosed Spines
Mechanism of Injury
Fractures in patients with ankylosed spines are most commonly caused by hyperextension secondary to frontal impact to the head and face. Preexisting kyphosis places the head forward to the trunk, making the face the first impact location. The resultant hyperextension is translated by the long lever arms to the fused spine in the midcervical area, where the anterior column fails in tension. Compressive forces are then created posteriorly, resulting in fractures of the spinous processes and lamina. Extension also creates posterior vertebral body displacement and, in severe cases, spinal cord injury. In 20% of cases there are concomitant noncontiguous fractures in the thoracic or lumbar spine.50
Central Cord Syndrome
Mechanism of Injury
Patients are most commonly injured from hyperextension or axial compression. This causes infolding of the ligamentum flavum and bulging of the disc creating a pincer to the spinal cord. The spinal canal is narrow before injury, usually less than 10 mm in anteroposterior diameter. The transient compression leads to ischemia in the central region of the cord and eventually necrosis. Annular and anterior longitudinal ligament disruption occurs commonly and is now being more recognized with MRI as a significant finding.51 Compression of the posterior elements may lead to fracture of the spinous processes and lateral column.
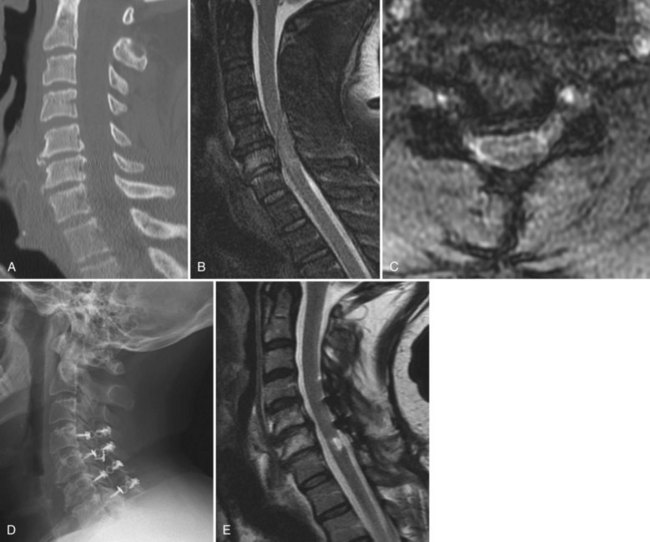
Radiographic Characteristics
Patients with central cord syndrome secondary to hyperextension injury have small spinal canals with midsagittal diameters less than 10 mm. This may be focal, especially at C3-4, or involve the entire subaxial cervical spine. The spine is generally spondylolytic with loss of disc height and osteophytes at multiple levels (Fig. 77–8). Signs of discoligamentous injury include endplate avulsion, retrolisthesis (thought to be preexisting), and disc distraction or hyperlordosis. The latter may be inaccurately thought to be normal. Retropharyngeal swelling is suggestive of hyperextension injury and should elicit concern for a discoligamentous injury. Posterior displacement of even small amounts may critically narrow spinal canals when stenosis is present. Various findings of posterior column injury may be present. If vertebral body displacement occurs, the facet joints will demonstrate diastases greater than 2 mm, indicating capsular disruption. Spinous process and lamina fractures secondary to impaction injury are suggestive of a hyperextension injury.
Treatment of Special Injury Types (Table 77–11)
Ankylosed Spines
| Fracture Type | Subtype | Treatment Options |
|---|---|---|
| Vertebral diastasis | Posterior fusion Anterior fusion ANTEROPOSTERIOR FUSION |
|
| Ankylosing spondolytic | POSTERIOR FUSION | |
| Central Cord Syndrome without Significant Skeletal Injury | ||
| Localized 1-2 levels stenosis | ANTERIOR DECOMPRESSION AND FUSION Laminoplasty |
|
| Multilevel stenosis | Anterior decompression and fusion LAMINOPLASTY |
|
CTO, cervicothoracic orthosis.
Authors’ recommendations are in bold capitals.
The treatment of subaxial fractures in patients with ankylosing spondylitis is surgical unless medically contraindicated.52 The aggressive approach is warranted by the high incidence of displacement and resultant neurologic injury or kyphosis that can occur with nonoperative treatment.53 Traction is generally not recommended because there are no ligaments to be used to guide reduction or restrain overdistraction. If necessary, a two-vector technique has been described for these patients.54 The surgical treatment is best performed with posterior instrumentation over many segments because there is no concern over fusing many segments. If possible, we recommend three levels above and below the injured segment. In the thoracic spine pedicle screws are used, while lateral mass screws are used in the cervical spine. Bone graft is not necessary, although local bone graft can be added at the fracture site.
Central Cord
The treatment of patients with central cord syndrome remains controversial. Decisions are based on the initial severity of neurologic deficit, injury type, degree of instability, and location of residual cord and root compression. Classically, initial nonoperative treatment was employed, stating that patients will likely demonstrate slow neurologic recovery.55 If recovery was not satisfactory, then a late decompression was performed.56 More recently an aggressive surgical approach has been advocated with the goals to speed recovery, shorten hospitalization, and reduce morbidity. It appears that the surgical treatment is safe and may offer better neurologic recovery, although adequate studies are lacking (see Fig. 77–8).55
Patients with unstable injuries should be treated surgically. Stabilization can be performed either anteriorly or posteriorly depending on where decompression is required. Those patients with focal (one to two levels) cord compression are good candidates for anterior decompression and fusion. Patients with multilevel disease can be treated with posterior decompression by laminoplasty or laminectomy. Fusion is indicated for cases with instability (CSISS > 7 or SLIC > 5) (see Fig. 77–8).
General Principles of Treatment
The goals of treatment are to protect the neural elements, reduce and stabilize injuries, create an environment for maximum neurologic recovery, and have a long-term stable functional spine (Table 77–12). Treatment decisions are based on the following determinants:
Emergency Treatment
Patients with spinal cord injuries and those with significant instability require urgent treatment. These principles are discussed in Chapter 81. Specific management of the cervical spine includes a consideration of whether a reduction with tong traction or early surgery is required. Rapid reduction of fracture dislocations in patients with spinal cord injury within a few hours of injury may reverse the neurologic injury and should be considered early in such cases, even without obtaining advanced imaging.57 Other indications for traction include displaced fractures, unstable injuries with a goal to protect the neural elements, and in some cases of central cord syndrome in patients who have malalignment. Contraindications to tong traction are skull fractures and defects, distraction injuries cranially in the spine, and distraction injuries across the disc space. The use of traction in patients with ankylosing spondylitic patients may be dangerous with the potential for overdistraction or introduction of shear.
Application of Tongs
The safety and efficacy of traction has been reported by Grant and colleagues,58 who retrospectively reviewed 82 patients with unilateral or bilateral facet dislocations treated by cranial tong reduction. All but two patients achieved reduction and most had improved ASIA scores within 24 hours. Only one case of neurologic deterioration involving a single nerve root level occurred. Hadley and colleagues59 reported less satisfactory results with reduction being achieved in only 78% of cases and neurologic improvement in 58%. Star and colleagues60 reported two cases of root deterioration in 57 cases while 93% of patients improved neurologically. Notably, up to 70% of body weight was safely used in these patients.60
Nonoperative Treatment
Indications for Nonoperative Treatment
Orthotic Options
The use of these is discussed more extensively in Chapter 84. Soft collars slightly decrease overall neck range of motion but should be used only for comfort or in patients with trivial injury patterns. The hard collar, when properly fit and worn, provides good stability against flexion and extension and rotation in the midcervical spine. An advantage is that padding can be changed to allow bathing activities while maintaining immobilization. Hard collars are less effective for injuries near the cervicothoracic junction. CTOs have anterior and posterior chest plates with rigid connections to the occiput and submandibular pads. Usually the orthosis is stabilized with straps over the shoulders and under the axilla. In general, CTOs provide improved stabilizing properties over collars but less patient comfort. The halo vest is the most rigid, with excellent reduction of intersegmental rotation, lateral bending, and flexion/extension. However, it does not provide resistance to axial loading or from a snaking deformation. Further, fracture site motion of up to 7 degrees angulation and 2-mm translation can occur between upright and supine positions.61
The orthosis is applied by a certified orthotist for fit, padding, and prevention of skin breakdown. Improperly sized or loose cervical orthoses are associated with increased range of motion.62 After the patient has been mobilized, anteroposterior and lateral radiographs in the upright position are obtained. These are analyzed for increasing translation or angulation at the fracture. If acceptable, the patient is discharged with follow-up at 2 weeks. Patients are instructed in full-time use and given extra pads for shower activities, except in the case of the halo vest. An occupational therapy consult can help teach activities of daily living. At 2 weeks, repeat neurologic examination and upright radiographs are obtained. Excessive pain or any new neurologic symptoms may indicate fracture displacement and should be thoroughly investigated. Most injuries of the subaxial cervical spine will heal in 8 to 10 weeks. At that time, the orthosis is removed and flexion/extension radiographs are obtained. The patient is then encouraged to increase activities, but sporting activities where falls are possible such as skiing are prohibited for 6 months.
Surgical Treatment
Indications
Surgical indications include failure of nonoperative treatment, unstable injuries, and the presence of neurologic compression in patients with ongoing deficits, and rarely in patients who cannot tolerate orthotic devices (Table 77–13).
TABLE 77–13 Surgical Indications in Subaxial Cervical Spine Trauma
| Failure of Nonoperative Management |
| Unstable Injuries |
| CSISS ≥ 7 |
| SLIC ≥ 5 |
| Neurologic Compression in Patients with Deficits |
| Inability to Tolerate Orthotic Management |
| Facial trauma Multiple injuries Noncontiguous spinal trauma |
Some patients with multiple injuries or medical comorbidities are not candidates for orthotic management and surgical stabilization is warranted. Examples are patients with severe facial injuries, mandibular fractures, or chest wall injuries. Spinal stabilization in these cases may be warranted to minimize complications related to those other injuries. Very obese patients, those with hypognathia, or those who have significant pulmonary deficit may not be braceable, especially with the halo vest. Elderly patients may have difficulty initiating swallowing and even aspirate with cervical immobilization, which may be avoidable with surgery and minimal postoperative bracing. Noncontiguous spinal fractures can alter normal treatment protocols. Upper cervical fractures, especially C2 fractures, are common in patients with subaxial fractures and may warrant surgical intervention for both injuries. Cervical orthoses usually extend to the thoracolumbar junction, where orthotic devices for management of cervical injuries may concentrate forces, which is undesirable. Persistent spinal cord and root compression in patients with persistent neurologic deficit is an indication for late decompression even up to 12 to 18 months later.56,63
Timing of Surgery
The timing of surgical intervention in patients with spinal cord injuries remains controversial due to lack of adequately designed clinical trials. Strong experimental evidence suggests that early decompression results in improved neurologic recovery.64–66 Further, there may be a short window of opportunity when spinal cord injury can be reversed or prevented.57 These observations are confirmed by careful study of the pathophysiologic changes that occur after spinal cord trauma as discussed in Chapter 75. However, to date it is unknown whether these observations apply to humans, although it is likely.
Fehlings and Perrin67 performed a systematic review of the timing of surgery in spinal cord injuries. They found that early surgery (<24 hours) can be performed safely. The evidence for benefits of acute surgical decompression (<24 hours) is weak due to lack of nonoperative controls. Fehlings and Perrin67 recommend this as only an option. The same authors are the principle investigators of an ongoing study that is comparing early versus delayed decompression. Early results show improved neurologic recovery in the group treated within 24 hours of injury; however, because of inadequate study power, the results are not statistically significant at this time.
In some cases such as bilateral facet dislocations or burst fractures, decompression can be achieved by immediate reduction with tong traction.57 Case reports of reduction of bilateral facet dislocations have demonstrated immediate neurologic recovery. These, along with large case studies, demonstrate safety and efficiency of closed reduction in these cases. Fehlings and Perrin76 recommend urgent decompression in incomplete quadriplegia at the level of a guideline. Another potential advantage of early surgery is that it allows immobilization and avoidance of potential problems of bed immobilization in critically injured patients. Results of comparison between early and delayed (>72 hours) surgical intervention in spinal cord injuries is inconclusive. Mirza, Mckinley, and colleagues have shown fewer complications and shorter hospitalizations and length of stay, whereas others such as Vaccaro, Waters, and Fehlings have shown no differences.68–72
Surgical Approaches
Both anterior and posterior approaches have been shown to be effective for the treatment of cervical spine fractures. The details of surgical techniques relative to anterior and posterior decompression and fusion with instrumentation are given in detail in Chapter 70. Many factors should be considered when choosing between these approaches. Most important is the need to decompress the neural elements, which will dictate the approach. In most cases this will be anterior, although displaced lamina or facet fractures occasionally require posterior decompression. Secondly, the bony structure where internal fixation (screws or wires) is to be applied should be considered. Fracture at fixation sites risks failure or may require larger constructs, thus making the opposite approach more efficacious. An example is a facet dislocation associated with a vertebral body endplate fracture that is best treated from a posterior approach, whereas a comminuted facet fracture may be better treated by an anterior discectomy and fusion. The approach should allow the fewest segments fused as possible. This would favor an anterior approach except when multiple fractures are present. Other considerations are patient’s comorbidities, disc injuries, bone quality, and forms of postoperative bracing.
Outcomes of Surgical Treatment
Several randomized trials, cohort analyses, and systematic reviews have compared outcomes between anterior and posterior fusion techniques. This discussion focuses on recent studies that use modern internal fixation devices. In 2002 Hadley34 performed a systematic review and concluded that both anterior and posterior approaches are options when surgical management is required. Brodke41 reported results in a randomized controlled trial comparing anterior with posterior plate fixation of three-column injuries after reduction by tong traction. No significant differences in outcomes were present between groups; however, nonunion only occurred in the anterior group, although this was not statistically significant. Kwon46 enrolled 42 patients having unilateral facet injuries in a randomized controlled trial comparing anterior with posterior fixation. The primary outcome variable was time to potential discharge, which favored anterior fixation by 0.75 days, although this was not significant. More infections occurred posteriorly and dysphagia anteriorly. The authors concluded that either approach is an option. Song51 compared anterior plates with combined anterior-posterior fixation in bilateral facet dislocations. He found that results were no different and concluded that the combined approach was not warranted for bilateral facet dislocations. All of these studies consistently show little difference in outcomes between modern rigid anterior and posterior fixation. Therefore both approaches are an option, and decisions should be based on the need for decompression, presence and absence of comminution, and to limit fusion levels.
Adverse Events
Cervical spinal injuries, especially those with cord involvement, are associated with significant morbidity and mortality. Death within the first year after spinal cord injury has decreased over the past 3 decades by 67%.5 Common causes may be preventable including pneumonia, sepsis, and pulmonary embolism. Neurologic deterioration occurs in up to 5% of patients.73–75 Risk factors include delayed diagnosis, hypotension, sepsis, and vertebral artery injury. Levi and colleagues emphasized the risk of inadequate radiologic assessment in trauma patients reporting 28 patients who deteriorated after admission to level 1 trauma centers.3 This represented 0.025% of patients admitted and 0.21% of all cervical spine injuries. Delay in diagnosis due to inadequate radiographs occurred in the majority of patients. Marshall reported in 1987 that early surgery (<72 hours) was a risk factor for deterioration.73 However, more recent studies in which patients are adequately medically optimized demonstrate that early surgery can be performed safely.76
Adverse events following surgery are more common in injured patients than in elective spine operations. This is caused by the inherent instability, multisystem trauma, and severity of neurologic injury. Kasmatis and colleagues reported the complications associated with anterior surgery for spinal injuries.77 The major events were dysphagia, screw loosening, increased kyphosis, deformity, and nonunion. Posterior fixation using lateral mass screws was associated with relatively high rates of infection 10%, radiculopathy from misplaced screws (6% to 10%), and rarely loss of fixation.7,46,78
Conclusions
Pearls
Key Points
1 Daffner RH, Hackney DB. ACR Appropriateness Criteria on suspected spine trauma. J Am Coll Radiol. 2007;4:762-775.
2 Anderson PA, Moore TA, Davis KW, et al. Cervical spine injury severity score. Assessment of reliability. J Bone Joint Surg Am. 2007;89:1057-1065.
3 Vaccaro AR, Hulbert RJ, Patel AA, et al. The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine. 2007;32:2365-2374.
4 Kwon BK, Fisher CG, Boyd MC, et al. A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. J Neurosurg Spine. 2007;7:1-12.
5 Brodke DS, Anderson PA, Newell DW, et al. Comparison of anterior and posterior approaches in cervical spinal cord injuries. J Spinal DisordTech. 2003;16:229-235.
6 Fehlings MG, Perrin RG. The timing of surgical intervention in the treatment of spinal cord injury: a systematic review of recent clinical evidence. Spine. 2006;31:S28-S35.
1 Muchow RD, Resnick DK, Abdel MP, et al. Magnetic resonance imaging (MRI) in the clearance of the cervical spine in blunt trauma: a meta-analysis. J Trauma. 2008;64:179-189.
2 Milby AH, Halpern CH, Guo W, et al. Prevalence of cervical spinal injury in trauma. Neurosurg Focus. 2008;25:E10.
3 Levi AD, Hurlbert RJ, Anderson P, et al. Neurologic deterioration secondary to unrecognized spinal instability following trauma—a multicenter study. Spine. 2006;31:451-458.
4 National spinal cord injury statistical center BA. Annual Report for the Model Spinal Cord Injury Care Systems. Birmingham: Alabama; 2006.
5 DeVivo MJ, Krause JS, Lammertse DP. Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil. 1999;80:1411-1419.
6 White AAIII, Panjabi MM. The clinical biomechanics of the occipitoatlantoaxial complex. Orthop Clin North Am. 1978;9:867-878.
7 Anderson PA, Henley MB, Grady MS, et al. Posterior cervical arthrodesis with AO reconstruction plates and bone graft. Spine. 1991;16:S72-S79.
8 Jeanneret B, Magerl F, Ward EH, et al. Posterior stabilization of the cervical spine with hook plates. Spine. 1991;16:S56-S63.
9 Roy-Camille R, Saillant G, Laville C, et al. Treatment of lower cervical spinal injuries–C3 to C7. Spine. 1992;17:S442-S446.
10 Gonzalez RP, Fried PO, Bukhalo M, et al. Role of clinical examination in screening for blunt cervical spine injury. J Am Coll Surg. 1999;189:152-157.
11 American College of Surgeons. American College of Surgeons Committee on Trauma. Advanced Trauma Life Support: ATLS Chicago. 7th ed. 2004.
12 Harris MB, Kronlage SC, Carboni PA, et al. Evaluation of the cervical spine in the polytrauma patient. Spine. 2000;25:2884-2891.
13 Tontz W, Anderson PA, Resnick DK. Clearance of the Asymptomatic Cervical Spine: A Meta-Analysis. Spine Journal. 2006;6:60S.
14 Hadley MN. Radiographic assessment of the cervical spine in symptomatic trauma patients. Neurosurgery. 2002;50:S36-S43.
15 Daffner RH, Hackney DB. ACR Appropriateness Criteria on suspected spine trauma. J Am Coll Radiol. 2007;4:762-775.
16 Hoffman JR, Mower WR, Wolfson AB, et al. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343:94-99.
17 Stiell IG, Wells GA, Vandemheen KL, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001;286:1841-1848.
18 Holmes JF, Akkinepalli R. Computed tomography versus plain radiography to screen for cervical spine injury: a meta-analysis. J Trauma. 2005;58:902-905.
19 Como JJ, Thompson MA, Anderson JS, et al. Is magnetic resonance imaging essential in clearing the cervical spine in obtunded patients with blunt trauma? J Trauma. 2007;63:544-549.
20 Schuster R, Waxman K, Sanchez B, et al. Magnetic resonance imaging is not needed to clear cervical spines in blunt trauma patients with normal computed tomographic results and no motor deficits. Arch Surg. 2005;140:762-766.
21 Menaker J, Philp A, Boswell S, et al. Computed tomography alone for cervical spine clearance in the unreliable patient—are we there yet? J Trauma. 2008;64:898-903.
22 Allen BLJr, Ferguson RL, Lehmann TR, et al. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine. 1982;7:1-27.
23 Nicoll EA. Fractures of the dorsolumbar spine. Journal of Bone and Joint Surgery. 1949;31B:376-394.
24 White AAIII, Johnson RM, Panjabi MM, et al. Biomechanical analysis of clinical stability in the cervical spine. Clin Orthop Relat Res. 1975:85-96.
25 Anderson PA, Moore TA, Davis KW, et al. Cervical spine injury severity score. Assessment of reliability. J Bone Joint Surg Am. 2007;89:1057-1065.
26 Chaput C, Barber R, Dominguez D, et al. Injury Severity Score (ISS) Correlates with Surgical Approach in Subaxial Cervical Trauma. The Spine Journal. 2007;7:129S-130S.
27 Vaccaro AR, Hulbert RJ, Patel AA, et al. The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine. 2007;32:2365-2374.
28 Webb JK, Broughton RB, McSweeney T, et al. Hidden flexion injury of the cervical spine. Journal of Bone & Joint Surgery—Br. 1976;58:322-327.
29 Woodring JH, Lee C, Duncan V. Transverse process fractures of the cervical vertebrae: are they insignificant? J Trauma. 1993;34:797-802.
30 Fisher CG, Dvorak MF, Leith J, et al. Comparison of outcomes for unstable lower cervical flexion teardrop fractures managed with halo thoracic vest versus anterior corpectomy and plating. Spine. 2002;27:160-166.
31 Koivikko MP, Myllynen P, Karjalainen M, et al. Conservative and operative treatment in cervical burst fractures. Arch Orthop Trauma Surg. 2000;120:448-451.
32 Toh E, Nomura T, Watanabe M, et al. Surgical treatment for injuries of the middle and lower cervical spine. Int Orthop. 2006;30:54-58.
33 Vaccaro AR, Klein GR, Thaller JB, et al. Distraction extension injuries of the cervical spine. J Spinal Disord. 2001;14:193-200.
34 Hadley MN. Treatment of subaxial cervical spinal injuries. Neurosurgery. 2002;50:S156-S165.
35 Kotani Y, Abumi K, Ito M, et al. Cervical spine injuries associated with lateral mass and facet joint fractures: new classification and surgical treatment with pedicle screw fixation. Eur Spine J. 2005;14:69-77.
36 Shono Y, McAfee PC, Cunningham BW. The pathomechanics of compression injuries in the cervical spine. Nondestructive and destructive investigative methods. Spine. 1993;18:2009-2019.
37 Vaccaro AR, Madigan L, Schweitzer ME, et al. Magnetic resonance imaging analysis of soft tissue disruption after flexion-distraction injuries of the subaxial cervical spine. Spine. 2001;26:1866-1872.
38 Nassr A, Lee JY, Dvorak MF, et al. Variations in surgical treatment of cervical facet dislocations. Spine. 2008;33:E188-E193.
39 Eismont FJ, Arena MJ, Green BA. Extrusion of an intervertebral disc associated with traumatic subluxation or dislocation of cervical facets. Case report. J Bone Joint Surg Am. 1991;73:1555-1560.
40 Spector LR, Kim DH, Affonso J, et al. Use of computed tomography to predict failure of nonoperative treatment of unilateral facet fractures of the cervical spine. Spine. 2006;31:2827-2835.
41 Brodke DS, Anderson PA, Newell DW, et al. Comparison of anterior and posterior approaches in cervical spinal cord injuries. J Spinal Disord Tech. 2003;16:229-235.
42 Beyer CA, Cabanela ME, Berquist TH. Unilateral facet dislocations and fracture-dislocations of the cervical spine. Journal of Bone & Joint Surgery—British Volume. 1991;73:977-981.
43 Rorabeck CH, Rock MG, Hawkins RJ, et al. Unilateral facet dislocation of the cervical spine. An analysis of the results of treatment in 26 patients. Spine. 1987;12:23-27.
44 Lee SH, Sung JK. Unilateral lateral mass-facet fractures with rotational instability: new classification and a review of 39 cases treated conservatively and with single segment anterior fusion. J Trauma. 2009;66:758-767.
45 Dvorak MF, Fisher CG, Aarabi B, et al. Clinical outcomes of 90 isolated unilateral facet fractures, subluxations, and dislocations treated surgically and nonoperatively. Spine. 2007;32:3007-3013.
46 Kwon BK, Fisher CG, Boyd MC, et al. A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. J Neurosurg Spine. 2007;7:1-12.
47 Johnson MG, Fisher CG, Boyd M, et al. The radiographic failure of single segment anterior cervical plate fixation in traumatic cervical flexion distraction injuries. Spine. 2004;29:2815-2820.
48 Koller H, Reynolds J, Zenner J, et al. Mid- to long-term outcome of instrumented anterior cervical fusion for subaxial injuries. Eur Spine J. 2009;18:650-653.
49 Lambiris E, Kasimatis GB, Tyllianakis M, et al. Treatment of unstable lower cervical spine injuries by anterior instrumented fusion alone. J Spinal Disord Tech. 2008;21:500-507.
50 Heyde CE, Fakler JK, Hasenboehler E, et al. Pitfalls and complications in the treatment of cervical spine fractures in patients with ankylosing spondylitis. Patient Saf Surg. 2008;2:1-15.
51 Song KJ, Kim GH, Lee KB. The efficacy of the modified classification system of soft tissue injury in extension injury of the lower cervical spine. Spine. 2008;33:E488-E493.
52 Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J. 2009;18:145-156.
53 Einsiedel T, Schmelz A, Arand M, et al. Injuries of the cervical spine in patients with ankylosing spondylitis: experience at two trauma centers. J Neurosurg Spine. 2006;5:33-45.
54 Cotler JM, Herbison GJ, Nasuti JF, et al. Closed reduction of traumatic cervical spine dislocation using traction weights up to 140 pounds. Spine. 1993;18:386-390.
55 Aarabi B, Koltz M, Ibrahimi D. Hyperextension cervical spine injuries and traumatic central cord syndrome. Neurosurg Focus. 2008;25:E9.
56 Bohlman HH, Anderson PA. Anterior decompression and arthrodesis of the cervical spine: long-term motor improvement. Part I—Improvement in incomplete traumatic quadriparesis. J Bone Joint Surg Am. 1992;74:671-682.
57 Cowan JAJr, McGillicuddy JE. Images in clinical medicine. Reversal of traumatic quadriplegia after closed reduction. N Engl J Med. 2008;359:2154.
58 Grant GA, Mirza SK, Chapman JR, et al. Risk of early closed reduction in cervical spine subluxation injuries. J Neurosurg. 1999;90:13-18.
59 Hadley MN, Fitzpatrick BC, Sonntag VK, et al. Facet fracture-dislocation injuries of the cervical spine. Neurosurgery. 1992;30:661-666.
60 Star AM, Jones AA, Cotler JM, et al. Immediate closed reduction of cervical spine dislocations using traction. Spine. 1990;15:1068-1072.
61 Anderson PA, Budorick TE, Easton KB, et al. Failure of halo vest to prevent in vivo motion in patients with injured cervical spines. Spine. 1991;16:S501-S505.
62 Bell KM, Frazier EC, Shively CM, et al. Assessing range of motion to evaluate the adverse effects of ill-fitting cervical orthoses. Spine J. 2009;9:225-231.
63 Anderson PA, Bohlman HH. Anterior decompression and arthrodesis of the cervical spine: long-term motor improvement. Part II—Improvement in complete traumatic quadriplegia. J Bone Joint Surg Am. 1992;74:683-692.
64 Dimar JR, Glassman SD, Raque GH, et al. The influence of spinal canal narrowing and timing of decompression on neurologic recovery after spinal cord contusion in a rat model. Spine. 1999;24:1623-1633.
65 Carlson GD, Gorden CD, Oliff HS, et al. Sustained spinal cord compression: part I: time-dependent effect on long-term pathophysiology. J Bone Joint Surg Am. 2003;85-A:86-94.
66 Delamarter RB, Sherman J, Carr JB. Pathophysiology of spinal cord injury. Recovery after immediate and delayed decompression. J Bone Joint Surg Am. 1995;77:1042-1049.
67 Fehlings MG, Perrin RG. The role and timing of early decompression for cervical spinal cord injury: update with a review of recent clinical evidence. Injury. 2005;36(Suppl 2):B13-B26.
68 Kerwin AJ, Griffen MM, Tepas JJIII, et al. Best practice determination of timing of spinal fracture fixation as defined by analysis of the National Trauma Data Bank. J Trauma. 2008;65:824-830.
69 Mirza SK, Krengel WFIII, Chapman JR, et al. Early versus delayed surgery for acute cervical spinal cord injury. Clin Orthop Relat Res. 1999:104-114.
70 Waters RL, Meyer PRJr, Adkins RH, et al. Emergency, acute, and surgical management of spine trauma. Arch Phys Med Rehabil. 1999;80:1383-1390.
71 McKinley W, Meade MA, Kirshblum S, et al. Outcomes of early surgical management versus late or no surgical intervention after acute spinal cord injury. Arch Phys Med Rehabil. 2004;85:1818-1825.
72 Vaccaro AR, Daugherty RJ, Sheehan TP, et al. Neurologic outcome of early versus late surgery for cervical spinal cord injury. Spine. 1997;22:2609-2613.
73 Marshall LF, Knowlton S, Garfin SR, et al. Deterioration following spinal cord injury. A multicenter study. J Neurosurg. 1987;66:400-404.
74 Harrop JS, Sharan AD, Vaccaro AR, et al. The cause of neurologic deterioration after acute cervical spinal cord injury. Spine. 2001;26:340-346.
75 Colterjohn NR, Bednar DA. Identifiable risk factors for secondary neurologic deterioration in the cervical spine-injured patient. Spine. 1995;20:2293-2297.
76 Fehlings MG, Perrin RG. The timing of surgical intervention in the treatment of spinal cord injury: a systematic review of recent clinical evidence. Spine. 2006;31:S28-S35.
77 Kasimatis GB, Panagiotopoulos E, Gliatis J, et al. Complications of anterior surgery in cervical spine trauma: an overview. Clin Neurol Neurosurg. 2009;111:18-27.
78 Heller JG, Silcox DHIII, Sutterlin CEIII. Complications of posterior cervical plating. Spine. 1995;20:2442-2448.