CHAPTER 30 Inguinal Hernias and Hydroceles
Inguinal Hernias
Step 1: Surgical Anatomy
 The patent processus vaginalis develops from a diverticulum of peritoneum, which attaches to the descending testicle at 7 to 8 months’ gestation.
The patent processus vaginalis develops from a diverticulum of peritoneum, which attaches to the descending testicle at 7 to 8 months’ gestation.Step 2: Preoperative Considerations
Step 3: Operative Steps
Inguinal Hernia Repair Technique
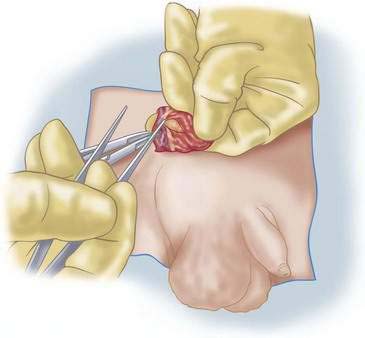
Male Patients
Female Patients
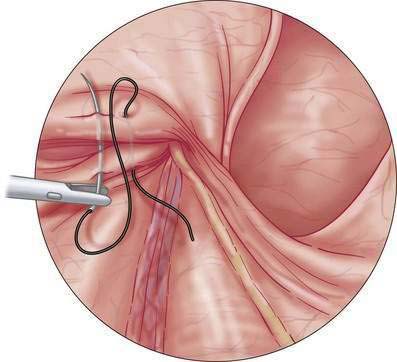
Laparoscopic Inguinal Hernia Repair (Fig. 30-13)
Step 4: Postoperative Care
Step 5: Pearls and Pitfalls
Hydrocele of the Tunica Vaginalis
Step 1: Surgical Anatomy
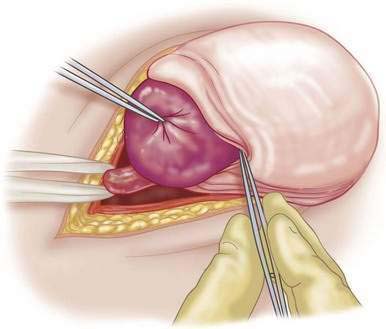
Step 3: Operative Steps
Step 5: Pearls and Pitfalls
Cox JA. Inguinal hernia of childhood. Surg Clin North Am. 1985;65:1331-1342.
Harper RG, Garcia A, Sia C. Inguinal hernia: a common problem of premature infants weighing 1000 grams or less at birth. Pediatrics. 1975;56:112-115.
Ozgediz D, Roayaie K, Lee H, et al. Subcutaneous endoscopically assisted ligation (SEAL) of the internal ring for repair of inguinal hernias in children: report of a new technique and early results. Surg Endosc. 2007;21:1327-1331.
Schier F. Laparoscopic inguinal hernia repair—a prospective personal series of 542 children. J Pediatr Surg. 2006;41(6):1081-1084.
Tackett LD, Breuer CK, Luks FI, et al. Incidence of contralateral inguinal hernia: a prospective analysis. J Pediatr Surg. 1999;34:684-687.