CT: Arises anteromedial to origin of inferior epigastric artery and extends through anterior abdominal wall lateral to rectus muscle
– Contents of inguinal canal (testicular vessels, vas deferens) can be seen as a crescent of density along lateral aspect of hernia as it protrudes
• Indirect inguinal hernia: Hernia passes through internal inguinal ring, down inguinal canal, and emerges at external ring
• Ultrasound: Can scan patient either with Valsalva maneuver or in upright position to precipitate hernia
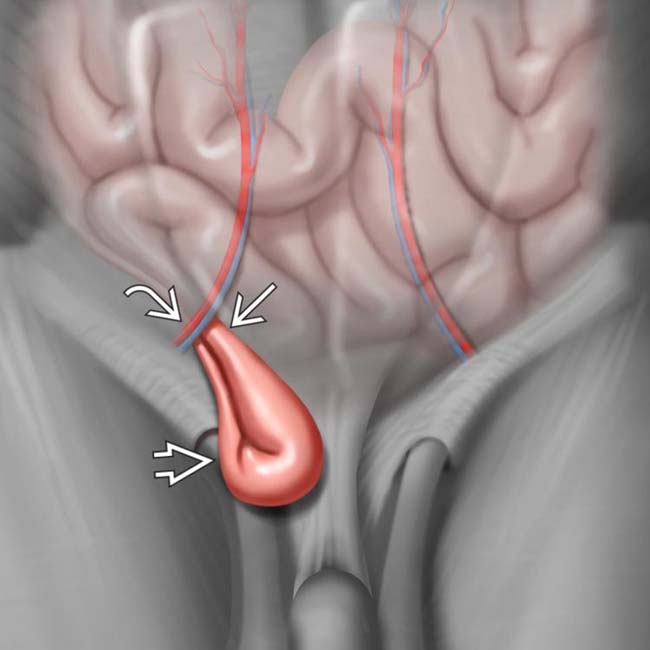
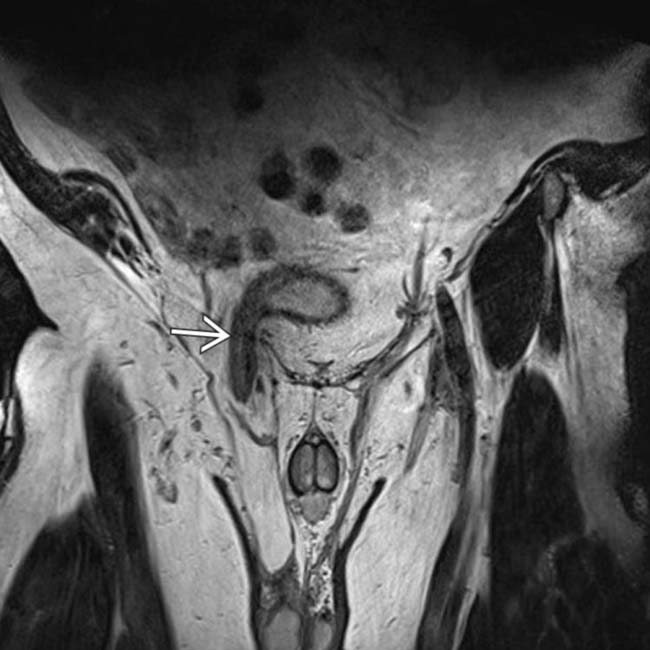
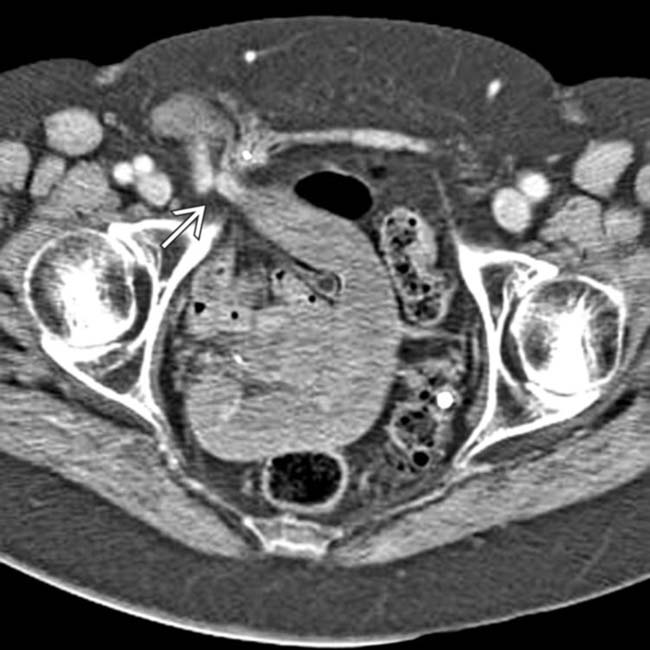
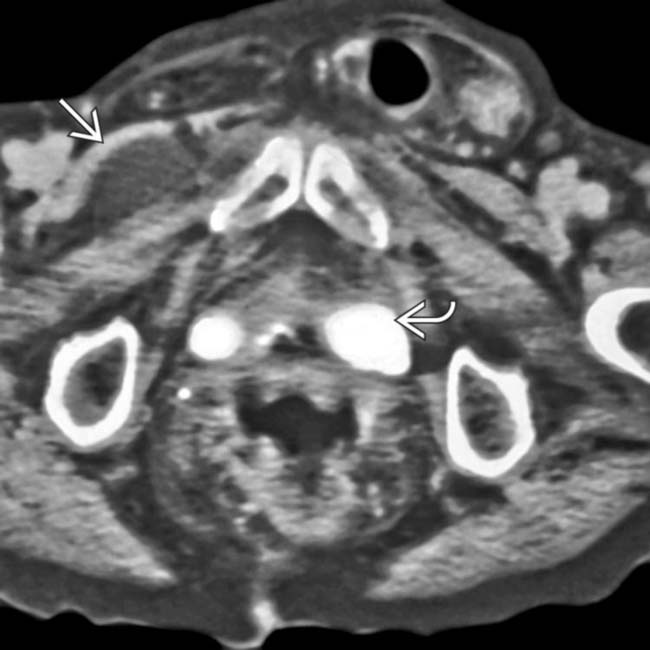
 , with the hernia neck
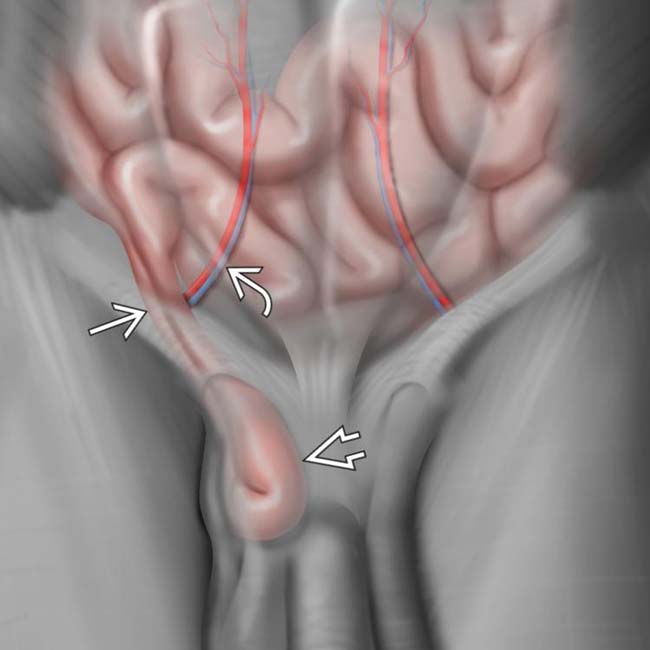
, with the hernia neck  located medial to the inferior epigastric artery and vein
located medial to the inferior epigastric artery and vein  .
.
 , with the hernia neck
, with the hernia neck  located lateral to the inferior epigastric artery and vein
located lateral to the inferior epigastric artery and vein  . The inferior epigastric vessels serve as the key landmark in distinguishing direct and indirect inguinal hernias.
. The inferior epigastric vessels serve as the key landmark in distinguishing direct and indirect inguinal hernias.
 and medial to the inferior epigastric vessels
and medial to the inferior epigastric vessels  , identifying it as a direct inguinal hernia.
, identifying it as a direct inguinal hernia.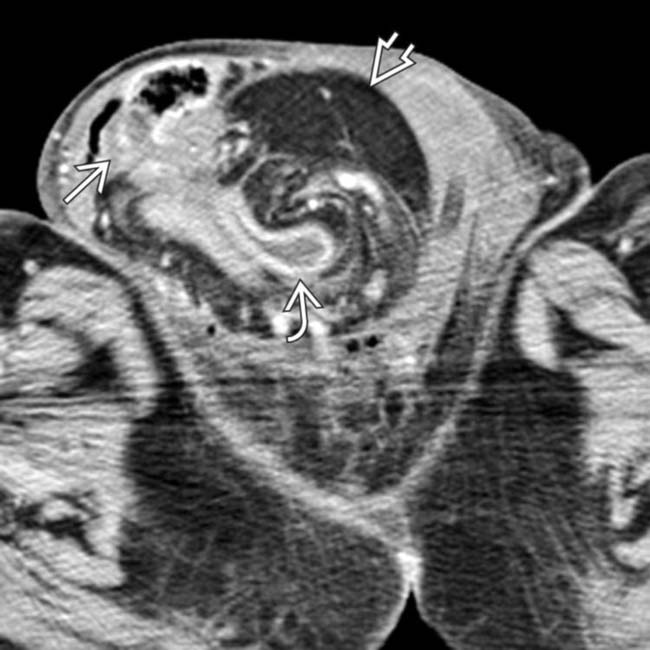
 , colon
, colon  , and omentum
, and omentum  .
.IMAGING
General Features
• Location
 Indirect IH: Hernia passes through internal inguinal ring, down inguinal canal, and emerges at external ring
Indirect IH: Hernia passes through internal inguinal ring, down inguinal canal, and emerges at external ring
 Indirect IH: Hernia passes through internal inguinal ring, down inguinal canal, and emerges at external ring
Indirect IH: Hernia passes through internal inguinal ring, down inguinal canal, and emerges at external ring
CT Findings
• Some IH, particularly when small, have tendency to reduce when patient is supine and may be missed on CT
• Primary landmark is inferior epigastric artery, which arises opposite to origin of deep circumflex iliac artery from external iliac artery
• Direct hernia: Arises anteromedial to origin of inferior epigastric artery, extends through anterior abdominal wall lateral to rectus muscle, and courses below inferior epigastric artery
• Indirect hernia: Arises superolateral to inferior epigastric vessels and extends lateral to medial within inguinal canal
• Direct and indirect hernias can very rarely be visualized in same groin: “Saddlebag” or “pantaloon” hernia (combined-type hernia)
• CT very helpful for identifying contents of hernia sac (omental fat, bowel, bladder) and identifying complications (bowel obstruction, ischemia, perforation, etc.)
Ultrasonographic Findings
• Some debate in literature regarding efficacy of US in diagnosing hernias: Various studies have shown sensitivities ranging from 29-100%
• Typically high-frequency transducer (> 10 MHz) best, since IH are superficial, but lower frequencies may be utilized in more obese patients
• Patient initially scanned supine, but advantage of US is ability to scan patient either with Valsalva maneuver or in upright position to precipitate hernia (if hernia not seen at rest in supine position)
• Primary sonographic landmarks are pubic tubercle and inferior epigastric artery (identified along lateral border of rectus abdominis and can be traced back to external iliac artery)
Radiographic Findings
• Radiography
 Soft tissue density or gas-containing mass overlying obturator foramen on affected side suggests presence of hernia
Soft tissue density or gas-containing mass overlying obturator foramen on affected side suggests presence of hernia
 Presence of dilated bowel loops with convergence of distended intestinal loops toward inguinal region suggests bowel obstruction due to inguinal hernia
Presence of dilated bowel loops with convergence of distended intestinal loops toward inguinal region suggests bowel obstruction due to inguinal hernia
 Soft tissue density or gas-containing mass overlying obturator foramen on affected side suggests presence of hernia
Soft tissue density or gas-containing mass overlying obturator foramen on affected side suggests presence of hernia Presence of dilated bowel loops with convergence of distended intestinal loops toward inguinal region suggests bowel obstruction due to inguinal hernia
Presence of dilated bowel loops with convergence of distended intestinal loops toward inguinal region suggests bowel obstruction due to inguinal herniaDIFFERENTIAL DIAGNOSIS
Femoral Hernia
PATHOLOGY
General Features
CLINICAL ISSUES
Presentation
• Most common signs/symptoms
• Physical exam: Recumbent and upright position; may be reducible; audible bowel sounds; ± tenderness

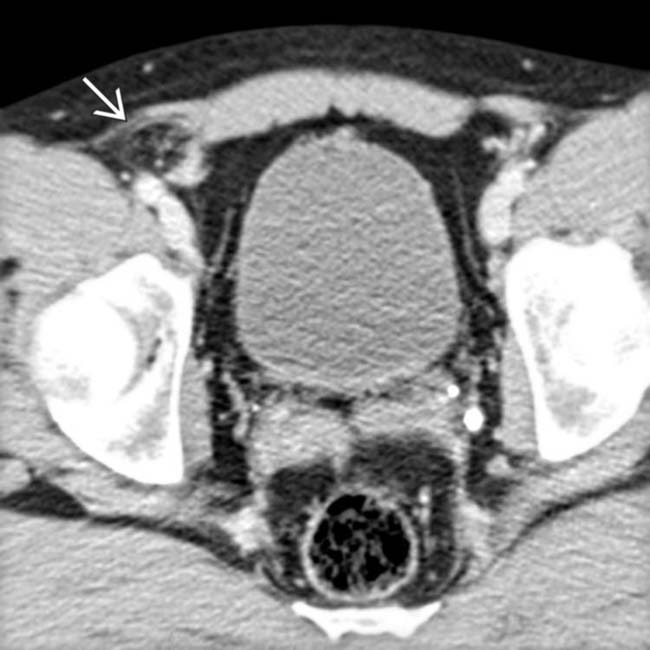
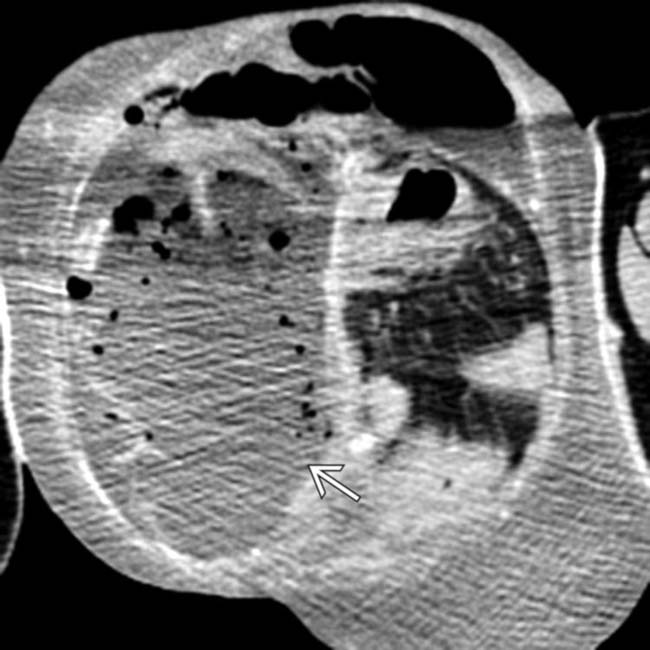
 in the pelvis, compatible with small bowel obstruction.
in the pelvis, compatible with small bowel obstruction.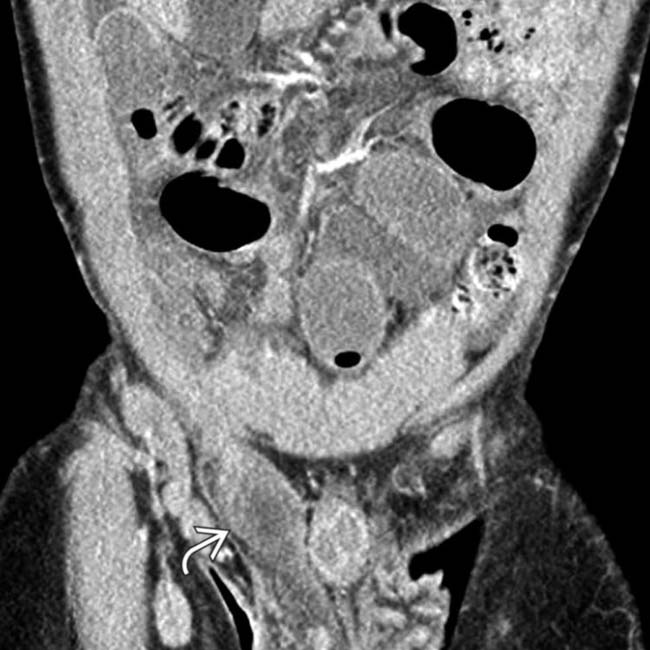
 with a transition point in the hernia sac. This incarcerated hernia could not be manually reduced, and urgent surgery was performed for repair.
with a transition point in the hernia sac. This incarcerated hernia could not be manually reduced, and urgent surgery was performed for repair.
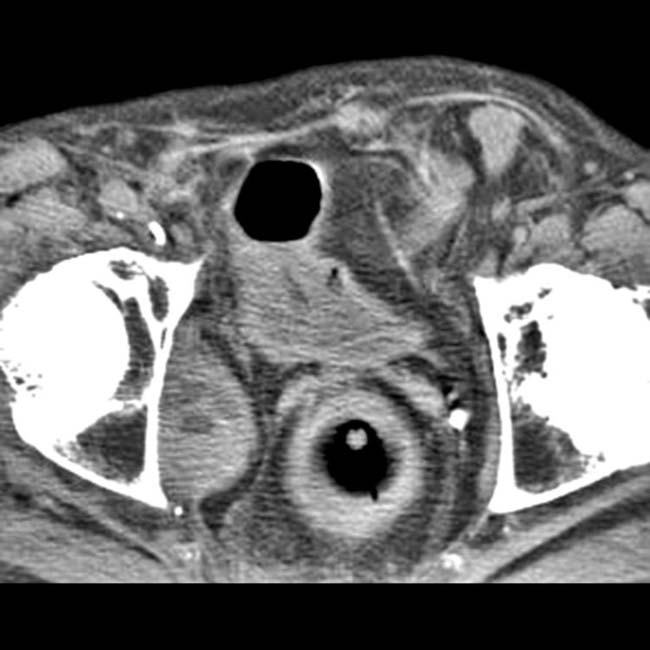
 in the right scrotal sac
in the right scrotal sac  . Note the contralateral left scrotum and testis
. Note the contralateral left scrotum and testis  .
.
 . Sliding inguinal hernias contain portions of partially retroperitoneal structures, such as the bladder, and care must be taken at surgery to avoid damage to these structures or their supplying vessels.
. Sliding inguinal hernias contain portions of partially retroperitoneal structures, such as the bladder, and care must be taken at surgery to avoid damage to these structures or their supplying vessels.
 lying over the right femoral head. Note the constriction of the bowel
lying over the right femoral head. Note the constriction of the bowel  as it passes through the inguinal ring.
as it passes through the inguinal ring.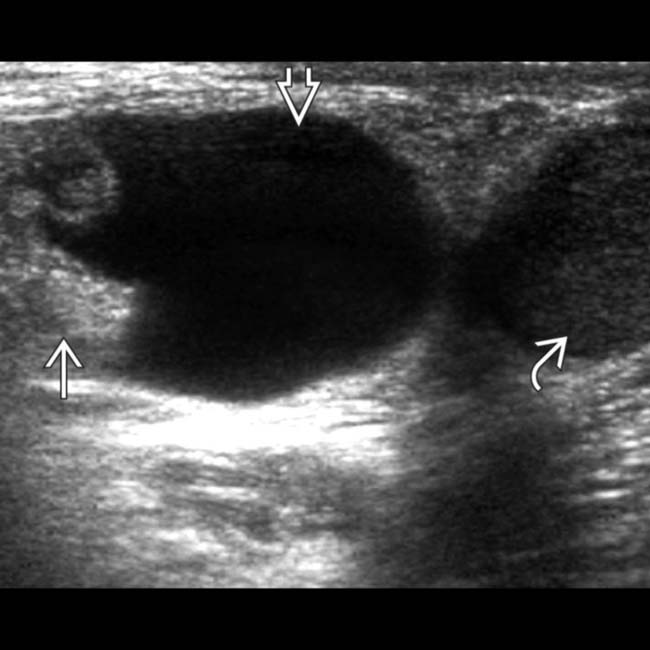
 herniating into the inguinal canal. Note the fluid
herniating into the inguinal canal. Note the fluid  within hernia sac and inferiorly displaced ipsilateral testis
within hernia sac and inferiorly displaced ipsilateral testis  . Omental fat on US is echogenic or slightly hypoechoic tissue without peristalsis.
. Omental fat on US is echogenic or slightly hypoechoic tissue without peristalsis.
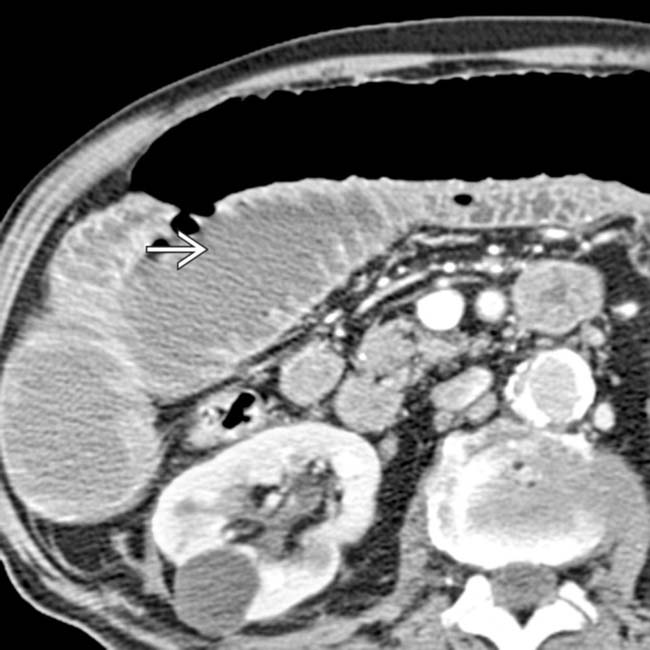
 lying anterior to the right femoral vessels. A contrast-opacified small bowel is present within the hernia, but no sign of bowel obstruction is seen.
lying anterior to the right femoral vessels. A contrast-opacified small bowel is present within the hernia, but no sign of bowel obstruction is seen.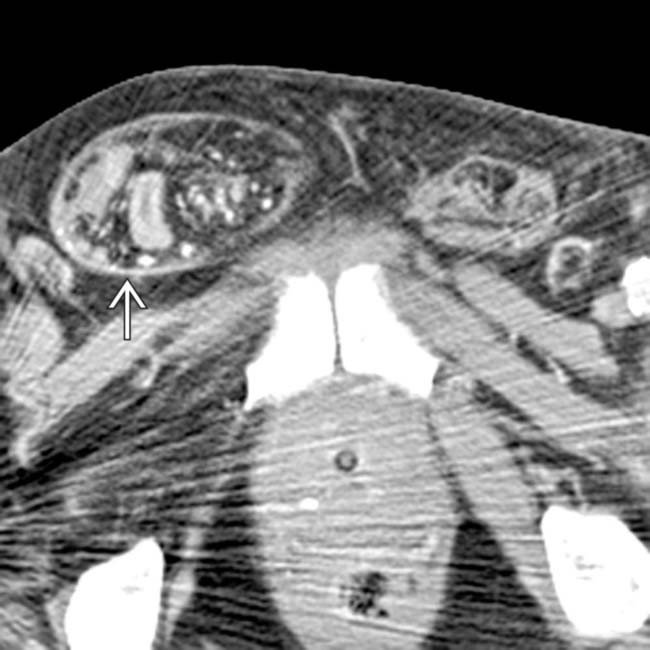
 .
.
 from obstruction.
from obstruction.
 contains herniated fat. The fat is somewhat “dirty” or infiltrated in appearance, suggesting incarceration or ischemia of herniated fat.
contains herniated fat. The fat is somewhat “dirty” or infiltrated in appearance, suggesting incarceration or ischemia of herniated fat.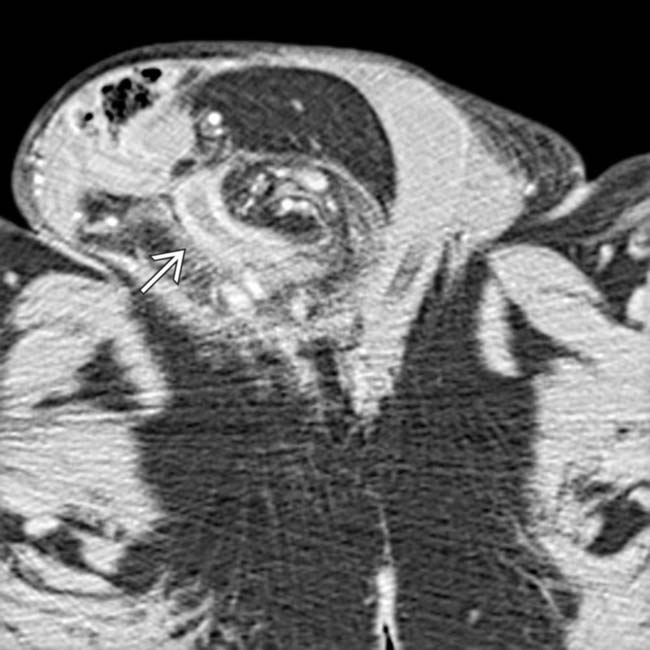
 .
.
 .
.
 .
.


 in a patient who reported a long history of a growing bulge in the groin. The hernia contains multiple small bowel loops, portions of the colon, and small ascites
in a patient who reported a long history of a growing bulge in the groin. The hernia contains multiple small bowel loops, portions of the colon, and small ascites  .
.




























































 .
.

 , and pessary
, and pessary  .
.
 from perforated incarcerated bowel within an inguinal hernia.
from perforated incarcerated bowel within an inguinal hernia.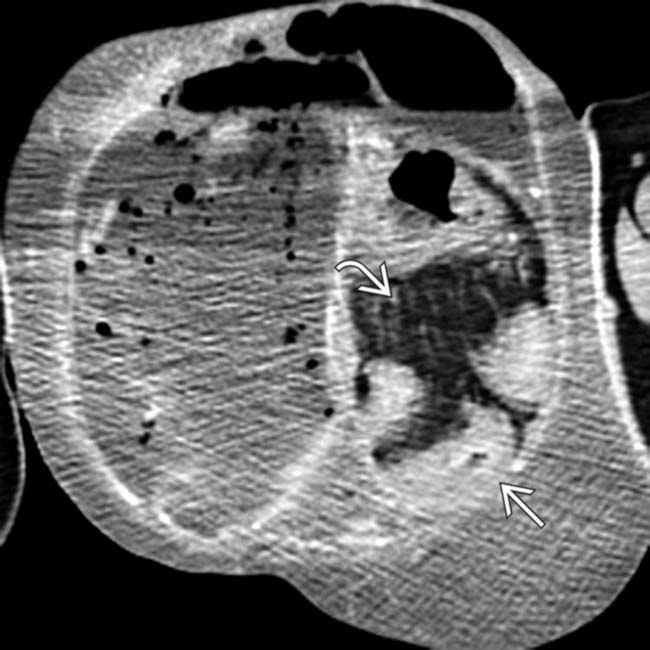
 and omental fat
and omental fat  within the hernia sac.
within the hernia sac.

