CHAPTER 35 Inguinal field block
Clinical anatomy
The iliohypogastric nerve is situated cephalad to the ilioinguinal nerve. At the level of the iliac crest, the iliohypogastric nerve divides into two terminal branches, the lateral cutaneous branch and medial cutaneous branches. The lateral cutaneous branch perforates the internal and external oblique and supplies the skin over the ventral part of the buttocks. This innervated area is behind that innervated by the subcostal nerve. The medial cutaneous branch continues ventrally until it pierces the internal oblique muscle above the anterior superior iliac spine, slopes downward between the internal oblique and external oblique muscles (Fig. 35.1), then pierces the external oblique aponeurosis 3 cm above the superficial inguinal ring, and ends by innervating skin over the lower part of the rectus abdominis and front of the pubis.
The ilioinguinal nerve runs ventrally, caudad to, and in a deeper plane than the iliohypogastric nerve. It perforates the transversus abdominis at the level of the anterior superior iliac spine and continues ventrally deep to the internal oblique (Fig. 35.2). Gradually, it pierces both internal and external oblique to reach the lower border of either the spermatic cord (in males) or the round ligament of the uterus (in females), where it finally reaches the inguinal canal. It contributes fibers to the internal oblique, the skin of the upper medial part of the thigh, and either the skin of the upper part of the scrotum and the root of the penis or the skin covering the labium majus and the mons pubis.
Ilioinguinal/iliohypogastric nerve block
Surface anatomy
The important bony structure for the ilioinguinal/iliohypogastric nerve block is the anterior superior iliac spine. The needle insertion site for ilioinguinal and iliohypogastric nerve blocks is 1 cm medial and 1 cm inferior to the anterior superior iliac spine (i.e. above the inguinal ligament) (Fig. 35.3).
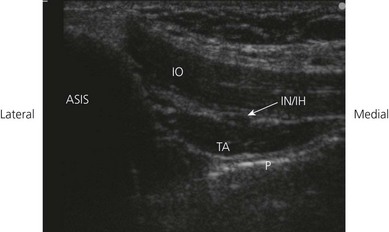
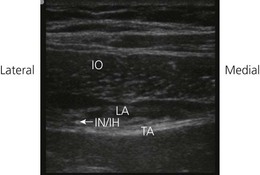
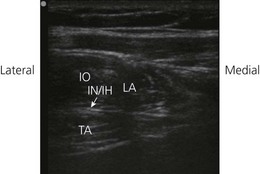
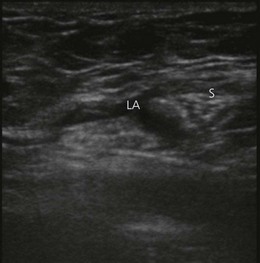
Sonoanatomy
Perform a systematic anatomical survey from the iliac crest to the lower abdomen. The abdominal wall is scanned about 5 cm cranial to the anterior superior iliac spine. A sagittal oblique transducer orientation is used (Fig. 35.4). At this point, all three muscle layers of the abdominal wall can easily be identified by ultrasound and facilitate orientation (Fig. 35.5). The peritoneum and bowel are seen deeper to these (Fig. 35.5). The nerves appear as hypoechoic fascicular structures with hyperechoic rims sandwiched between the layers of muscle (Fig. 35.6). Trace the course of the nerves from above ASIS and distally towards the inguinal region. The iliohypogastric and ilioinguinal nerves consistently lie between the internal oblique and transversus abdominis muscles here. The recommended injection site for landmark-based approaches is situated medial to the anterior superior iliac spine. At this site, both nerves are often penetrating the internal oblique muscle. Performing a ‘blind’ technique here may result in difficulty for the injected local anesthetic to reach both nerves if they are not lying in the same compartment. This is a possible explanation for the high failure rates of 20–30%. It is more likely to reach both nerves with local anesthetic using the landmark-based approach where the nerves are lying in the same layer of the abdominal wall. Small vessels are frequently seen to accompany nerves within the plane.
Technique
Landmark-based approach
The patient lies supine. The operator stands at the side to be anesthetized. The ilioinguinal and iliohypogastric nerves are anesthetized at a single injection site (Fig. 35.3). A 35-mm 21-G needle is inserted through the skin 1 cm medial and 1 cm inferior to the anterior superior iliac spine. The needle is held lightly between the fingers and slowly advanced in an incremental fashion; the ‘clicks’ of the abdominal wall are best appreciated with this technique. Resting the ulnar border of the injecting hand on the patient can help steady it, to prevent overshooting the target.
Ultrasound-guided approach
Injection point is 5 cm cranial and posterior to the anterior superior iliac spine. The nerves are kept in the center of the field of view, and the needle entry site is at the center of the linear transducer (out-of-plane) (Fig. 35.7).
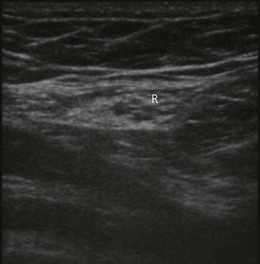
Once the needle has been placed within the correct muscular plane adjacent to the nerves, 3–5 mL of local anesthetic solution is injected. Needle placement in the correct plane is indicated by fluid expansion in a space bounded by the hyperechoic fascial sheath of the internal oblique and transverse abdominis muscle layers (hydro dissect) (Fig. 35.8). Incorrect needle placement will result in intramuscular fluid during hydrodissection (Fig. 35.9).
Genitofemoral nerve block
Surface anatomy
The important bony structure for genitofemoral nerve block is the pubic tubercle. The pubic tubercle can be palpated 3 cm from the midline. The needle insertion site for block of the genital branch of genitofemoral nerve is 2 cm laterally and 2 cm cephalad from the pubic tubercle (Fig. 35.10).
Sonoanatomy
A high frequency linear transducer is used. The orientation of the transducer is perpendicular to the inguinal ligament. The final position of the transducer is 2 cm lateral to the pubic tubercle. The spermatic cord, which is oval or circular in shape with 1 or 2 arteries within it (the testicular artery and the artery to vas deferens), is identifed. In the female, the round ligament is identified (Fig. 35.11). It is possible also to start scanning with the transducer at the internal inguinal ring, at which the femoral artery can be visualized in the longitudinal scan (along the length of the femoral artery). By moving the ultrasound transducer in the cephalad direction, the artery is seen diving deep toward the inguinal ligament. At this point, an oval or circular structure can easily be seen superficial to the femoral artery. The transducer is then moved slightly in the medial direction away from the femoral artery. The genital branch of the genitofemoral nerve is not easily identified.
Technique
Landmark-based approach
The genital branch is blocked by inserting a 35-mm 23-G needle 2 cm lateral and 2 cm superior to the pubic tubercle (Fig. 35.10). The needle is passed medially until the pubic tubercle is contacted, withdrawn slightly, and injection of 4–5 mL of local anesthetic made in a fan-shaped manner. A vertical injection in the midline at the pubis is made to block overlapping innervation from the contralateral side.
Ultrasound-guided approach
An out-of-plane technique is also used, with the needle approaching the skin from the lateral aspect of the transducer (Fig. 35.12). Local anesthetic without epinephrine is used to avoid the possible vasoconstriction effect on the testicular artery. Because of the anatomical anomalies found with the location of the genital branch in the genitofemoral nerve, 5 mL of local anesthetic is injected inside and another 5 mL outside the spermatic cord (Fig. 35.13).
Adverse effects
Amid PK, Shulman AG, Lichtenstein IL. Local anesthesia for inguinal hernia repair: step-by-step procedure. Ann Surg. 1994;220:735-737.
Amory C, Mariscal A, Guyot E, et al. Is ilioinguinal/iliohypogastric nerve block always totally safe in children? Paediatr Anaesth. 2003;13(2):164-166.
Ghani KR, McMillan R, Paterson-Brown S. Transient femoral nerve palsy following ilio-inguinal nerve blockade for day case inguinal hernia repair. J R Coll Surg Edinb. 2002 Aug;47(4):626-629.
Gucev G, Yasui GM, Chang TY, Lee J. Bilateral ultrasound-guided continuous ilioinguinal-iliohypogastric block for pain relief after cesarean delivery. Anesth Analg. 2008;106(4):1220-1222.
Vaisman J. Pelvic hematoma after an ilioinguinal nerve block for orchialgia. Anesth Analg. 2001;92:1048-1049.
Van Schoor AN, Boon JM, Bosenberg AT, et al. Anatomical considerations of the pediatric ilioinguinal/iliohypogastric nerve block. Paediatr Anaesth. 2005;15(5):371-377.
Willschke H, Marhofer P, Bosenberg A, et al. Ultrasonography for ilioinguinal/iliohypogastric nerve blocks in children. Br J Anaesth. 2005;95(2):226-230.