16 Infraorbital / upper and lower eyelids
Summary and Key Features
• Successful periorbital rejuvenation demands close attention to patient’s desires and expectations, general anatomical variations, detection of subtle asymmetries, and individualized treatment
• Careful patient selection requires a thorough exploration into the patient’s desired outcome and concerns, a detailed medical and cosmetic history, and a thorough and comprehensive aesthetic assessment
• Precise placement of injections and accurate / individualized dosing are crucial in obtaining the most beneficial effects and avoiding adverse events
• Small doses in the lower lid can minimize infraorbital rhytides and widen the eye
• BoNT may also be used to correct eyelid malposition, including ptosis and asymmetry
• Poor patient selection, inappropriate injection techniques, and diffusion of the toxin can lead to serious adverse events and complications
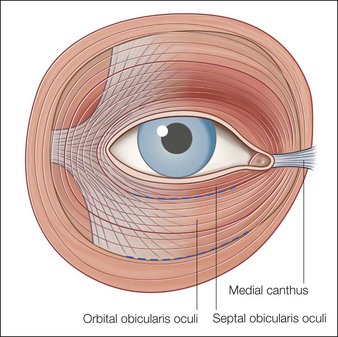
Anatomy of the eye
Complete knowledge and understanding of both dynamic and volumetric changes in the face, as well as the interaction between and function of various facial musculature and the surrounding soft tissue, are critical to ensuring successful outcomes with the use of BoNT in the periorbital region. Although in-depth examinations of facial anatomy have been published elsewhere, this chapter focuses on the anatomy of the eye relevant to the use of BoNT in the upper and lower eyelids (Fig. 16.1).
Patient assessment and selection
A complete medical and ophthalmic history is necessary, including previous experiences with rejuvenation procedures, surgery, and any other conditions that might influence treatment plans or outcome. The degree of rhytides and their potential response to treatment can be assessed via the Glogau photoaging scale (Table 16.1). Moreover, the quality of skin around the eye will also determine a treatment plan: patients with excessive skin above the eye, prominent fat pads in the lower lid, septal fat herniation, or severe elastosis (identified by a positive snap test), may require additional rejuvenating procedures such as laser or light-based therapies or even surgery prior to augmentation. All findings (including any sign of ptosis or asymmetry) should be noted and discussed with the patient, and standard digital photographs taken both before and after any treatments. Photographs should display the face in repose and at maximal expression to document changes on animation.
| Group severity* | Description | Rejuvenation modalities |
|---|---|---|
| II | Moderate; wrinkles in motion | Responds well to BoNT alone |
| III | Advanced; wrinkles at rest | BoNT plus additional correction, such as soft tissue augmentation |
| IV | Severe; only wrinkles | BoNT plus deeper skin resurfacing for maximal improvement |
* Based on the Glogau classification of photoaging.
Not everyone is a candidate for BoNT therapy. Aside from general contraindications (Box 16.1), caution should prevail in patients with a history and especially complications related to previous lower eyelid blepharoplasty and injections avoided in patients with lower lid laxity, due to the risk of scleral show, pre-existing conditions that could be worsened by treatment, such as mid-facial paresis or symptomatic dry eyes, stable or progressive muscular dystrophic conditions causing blepharoptosis, or anyone with already-compromised function of the orbicularis oculi.
Box 16.1
Contraindications and precautions to periocular BoNT treatment
| Contraindications | Precautions |
|---|---|
Indications and techniques
Hypertrophic orbicularis, infraorbital rhytides, and widening of the eye
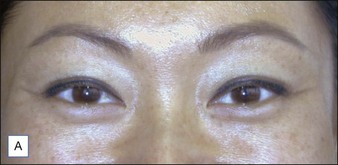
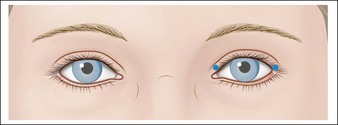
Infraorbital rhytides radiating below the eyes toward the cheek arise from concentric contraction of the orbicularis oculi peripheral to the lines. Moreover, such hypertrophy of the pretarsal portion of the orbicularis oculi contributes to the perception of lower eyelid bags (a ‘jelly roll’ appearance) and a narrowing of the palpebral aperture, particularly when the patient smiles. A series of studies conducted by Flynn & Carruthers have shown that 2 U BoNT placed subdermally in the lower eyelid in the midpupillary line, 3 mm below the ciliary margin (Fig. 16.2) can relax and flatten the pretarsal orbicularis, improving the appearance of the lower lid. Similar injections in the lower lid with concomitant treatment of the lateral canthal rhytides (three injections of 4 U each, for a total of 12 U) can produce increases of approximately 2–3 mm in the vertical palpebral aperture at rest and full smile, respectively, giving the lower eyelid a more rounded appearance (Fig. 16.3). Further examination by Flynn & Carruthers demonstrated a clear dose response when the lower lid was treated alone; however, higher doses led to an increase in side effects and did not further enhance the size of the palpebral aperture. The authors therefore recommend a conservative approach with the smallest dose (1–2 U at two sites) in the lower lid, with retreatment after 2–4 weeks if necessary.
A healthy 32-year-old Filipino-Canadian woman presented complaining of a ‘jelly roll’ underneath her eyes when she smiled. She requested a more western wide-eyed look and reduction of the ‘jelly roll’. Figure 16.2A demonstrates a hypertrophic orbicularis oculi. A ‘snap-test’ demonstrated excellent elasticity, which, in conjunction with the youthful tone and texture of the skin, indicated that the patient was a suitable candidate for infraorbital BoNT-A treatment. In order to achieve a wider aperture and flattening of hypertrophic orbicularis oculi (Fig. 16.2B) 2 U of BoNT-A were injected in the mid-pupillary line 4 mm below the lid margin bilaterally. Figure 16.2C demonstrates the injection site and technique.
Lid ptosis, malposition, and asymmetry
BoNT is an effective treatment for the temporary management of mild-to-moderate upper lid ptosis, malposition, and eyelid-fissure asymmetry. Research by Fagien indicates that correct placement, dosing, and careful patient selection will determine predictability of response. Typically, eyelid malposition of any etiology has been treated by surgical correction of the underlying cause, with nonsurgical options for upper lid ptosis limited to adrenergic topical ophthalmic drops. Low-dose subdermal injection of BoNT (0.5–1.5 U) into the extreme medial and lateral aspects of the pretarsal region of the orbicularis just above the lash line (Figs 16.4 and 16.5) allows unopposed activity of the levator palpebrae and Müller’s muscle, and a return to symmetry.
Adjunctive treatments for the lid
Adverse events
More serious adverse effects can occur, usually due to inappropriate dosing or injection technique (Table 16.2). Some patients describe a temporary feeling of ‘fullness’ in the lower lid following treatment. In rare cases, but particularly in patients with excessive lower lid laxity, this may manifest as edema that is worse in the morning. It is believed that this results from inactivity of the orbicularis oculi, which aids in the drainage of lymphatic fluid. Rare complications in the periocular area include lower eyelid laxity, scleral show, epiphora, ectropion, diplopia, dry eye, incomplete eyelid closure, and ptosis. Careful patient selection and attention to anatomical features of the periorbital region can aid in avoiding most of these side effects, all of which eventually disappear over time due to the transient effect of BoNT. Goldman reported a case of prominent festoon formation after 2 U 2–3 mm below the ciliary margin in the mid-pupillary line and 10 U (single injection) in the mid-lateral canthal region. Only at the follow-up visit did the patient admit to a previous facelift, forehead lift, and lower eyelid blepharoplasty 8 years previously. This case scenario emphasizes the importance of pre-treatment history and physical examination of the lower eyelid structure and function before treatment with even small doses of BoNT. Upper eyelid complications can also be avoided by careful thought, injection technique, and placement. Mild lagophthalmos can be induced in the upper eyelid by greater than necessary dosages and can generally be avoided with doses less than 1.5 U. This too, stresses the need for an initial conservative approach that can be titrated to the most effective dose.
| Cause | Complication |
|---|---|
| Treatment of lower lid pretarsal orbicularis in patients with severe elastosis and retraction | Ectropion, scleral show; accentuation of drooping or rhytides in lower lid; lower lid fat herniation |
| Diffusion of toxin behind orbital septum | Eyelid Ptosis |
| Injections near trochlea in upper or lower eyelid | Diplopia |
| Paralysis of orbicularis oculi | Epiphora; ectropion |
Balikian RV, Zimbler MS. Primary and adjunctive uses of botulinum toxin type A in the periorbital region. Otolaryngology Clinics of North America. 2007;40:291–303.
Carruthers J, Carruthers A. Adjunctive botulinum toxin type A: fillers and light-based therapies. International Ophthalmology Clinics. 2005;45:143–151.
Carruthers J, Fagien S, Matarasso SL, Botox Consensus Group. Consensus recommendations on the use of botulinum toxin type a in facial aesthetics. Plastic Reconstructive Surgery. 2004;114(6 suppl):S1–S22.
Cohen JL. Enhancing the growth of natural eyelashes: the mechanism of bimatoprost-induced eyelash growth. Dermatologic Surgery. 2010;36:1361–1371.
Fagien S. Botox for the treatment of dynamic and hyperkinetic facial lines and furrows: adjunctive use in facial aesthetic surgery. Plastic Reconstructive Surgery. 1999;103:701–713.
Fagien S. Botulinum toxin type A for facial aesthetic enhancement: role in facial shaping. Plastic and Reconstructive Surgery. 2003;112(5 suppl):S6–S18.
Fagien S. Temporary management of upper lid ptosis, lid malposition, and eyelid fissure asymmetry with botulinum toxin type A. Plastic and Reconstructive Surgery. 2004;114:1892–1902.
Fagien S, Brandt FS. Primary and adjunctive use of botulinum toxin type A (Botox) in facial aesthetic surgery: beyond the glabella. Clinics in Plastic Surgery. 2001;28:127–148.
Fagien S, Raspaldo H. Facial rejuvenation with botulinum neurotoxin: an anatomical and experiential perspective. Journal of Cosmetic and Laser Therapy. 2007;9(suppl 1):23–31.
Fagien S. Management of hypotrichosis of the eyelashes: Focus on bimatoprost. Cosmetic, Clinical, and Investigational Dermatology. 2010;3:1–10.
Flynn TC. Periocular botulinum toxin. Clinics in Dermatology. 2003;21:498–504.
Flynn TC, Carruthers JA, Carruthers JA. Botulinum-A toxin treatment of the lower eyelid improves infraorbital rhytides and widens the eye. Dermatologic Surgery. 2001;27:703–708.
Flynn TC, Carruthers JA, Carruthers JA, et al. Botulinum A toxin (BOTOX) in the lower eyelid: dose-finding study. Dermatologic Surgery. 2003;29:943–950.
Glaser DA, Patel U. Enhancing the eyes: use of minimally invasive techniques for periorbital rejuvenation. Journal of Drugs in Dermatology. 2010;9:S118–S128.
Glavas IP, Purewal BK. Noninvasive techniques in periorbital rejuvenation. Facial Plastic Surgery. 2007;23:162–167.
Glogau RG. Aesthetic and anatomic analysis of the aging skin. Seminars in Cutaneous Medicine and Surgery. 1996;15:134–138.
Goldman MP. Festoon formation after infraorbital botulinum A toxin: a case report. Dermatologic Surgery. 2003;29:560–561.
Harris PA, Mendelson BC. Eyelid and midcheek anatomy. In: Fagien S, ed. Putterman’s Cosmetic Ocuplasticsurgery. 4th edn. Philadelphia: WB Saunders; 2007:45–63.
Matarasso SL, Matarasso A. ‘M’ marks the spot: update on treatment guidelines for botulinum toxin type A for the periocular area. Plastics and Reconstructive Surgery. 2003;112:1470–1472.
Smith S, Fagien S, Whitcup S, et al. Eyelash growth in subjects treated with bimatoprost: A multicenter, randomized, double-masked, vehicle-controlled, parallel group study. Journal of the American Academy of Dermatology. 2011. Sep 5 [Epub ahead of print]