31 Infraclavicular Block
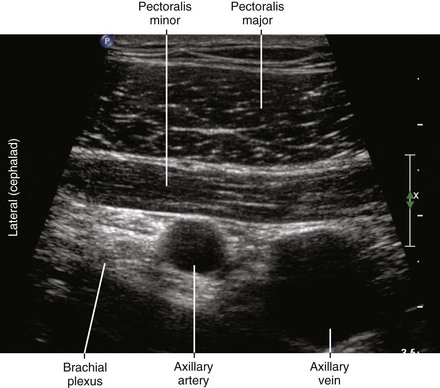
Infraclavicular block of the brachial plexus was developed as a means to achieve complete brachial plexus anesthesia and was one of the first blocks to be described using ultrasound imaging.1,2 This block is performed at the level of the pectoralis minor muscle. In this location the brachial plexus consists of three cords that compactly hug the walls of the second part of the axillary artery.3 The infraclavicular region has the advantage of being a secure place for a catheter that provides complete brachial plexus anesthesia. Another advantage is that anatomic variation is relatively uncommon in this region. In the infraclavicular region, the serratus anterior and subscapularis muscles form the margin of safety between the neurovascular bundle and the chest. Because proximal arm muscles are anesthetized (including the pectoralis and deltoid), infraclavicular blocks produce excellent tourniquet tolerance and conditions for upper extremity surgery.4 The block can be performed with the arm abducted or at the patient’s side (Table 31-1).
Table 31-1 Clinical Considerations for Infraclavicular Block
| Advantages | Disadvantages |
|---|---|
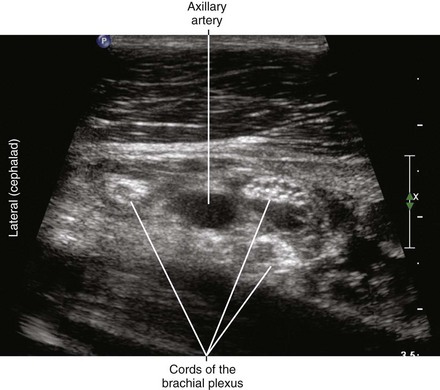
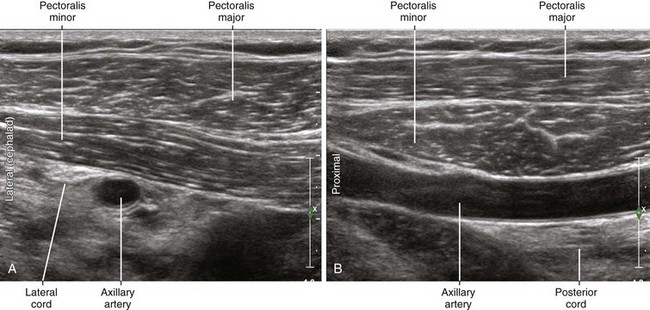
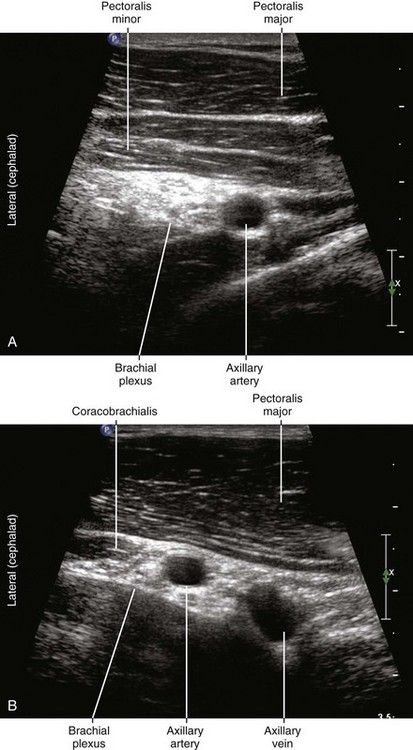
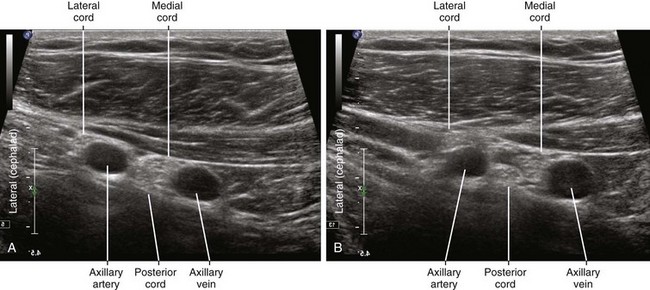
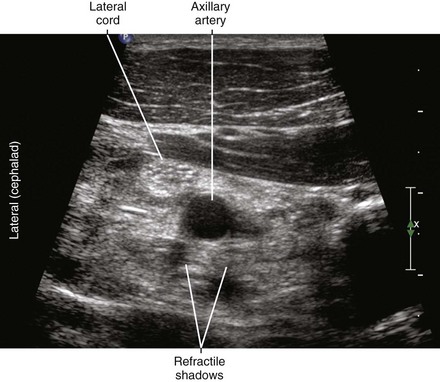
Cord topography changes along the length of the axillary artery in the infraclavicular region.5 Proximally, the cords of the brachial plexus have more of a “supraclavicular” configuration in which all the cords are on the lateral side of the axillary artery. Following distally, the true “infraclavicular” configuration is when all cords surround the axillary artery before the takeoff of the axillary and musculocutaneous nerves. When the transducer is too proximal, the curved inclination of the ribs and pleura can be recognized. When the transducer is too distal, the coracobrachialis muscle and musculocutaneous nerve can be appreciated on the lateral side of artery.
Suggested Technique
Key Points
| Infraclavicular Block | The Essentials |
|---|---|
| Anatomy | The PMi defines the second part of the AA. |
| The cords of the BP hug the walls of the second part of the AA. | |
| The BP cords (lateral, posterior, and medial) are named with respect to the second part of the AA | |
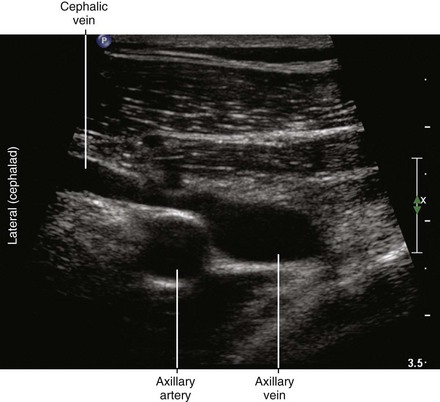
| The cephalic vein (“tadpole sign”) crosses over the AA to enter the AV. | |
| Image orientation | The AV lies medial (caudad) to the AA. |
| Positioning | Supine, with arm abducted if possible |
| A blue foam headrest provides working room. | |
| Operator | Standing on the lateral (cephalad) side of the armboard (for laptop system) |
| At the side of patient (for system with movable display) | |
| Display | Across the armboard (for laptop system) |
| Across the table (for system with movable display) | |
| Transducer | Medium-frequency curved, small footprint |
| Initial depth setting | 40 to 50 mm |
| Needle | 20 to 21 gauge, 70 to 90 mm in length |
| Anatomic location | Begin by scanning halfway between supraclavicular region and axilla. Slide transducer to obtain SAX view of AA underneath PMa and PMi. Perform infraclavicular block at the level of the PMi. |
| The CB (and therefore MCN takeoff) should not be in view. | |
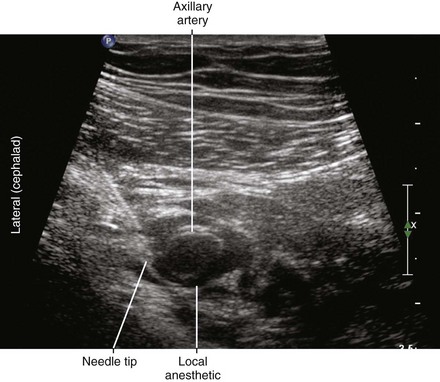
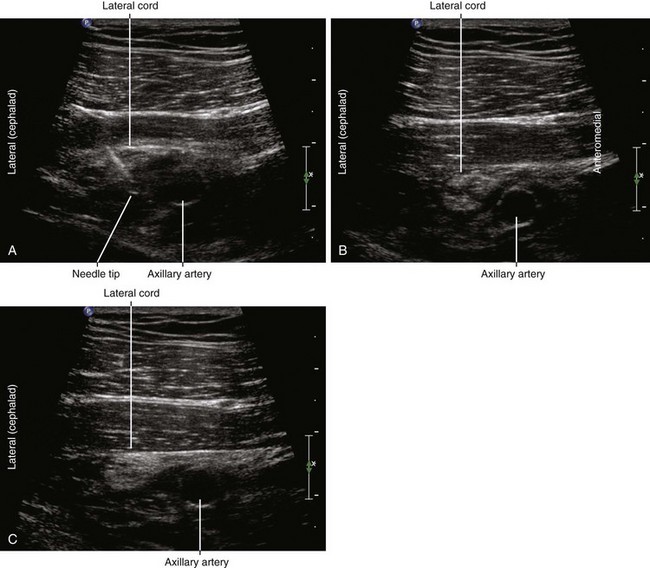
| Approach | SAX view of second part of AA (under PMi), in-plane. |
| Place the needle tip between the cords and AA. | |
| A U-shaped distribution under the AA is desired. | |
| Sonographic assessment | The injection should separate the cords of the BP from the AA. |
| Anatomic variation | Duplicate axillary vein on lateral side of AA is common. |
| “Supraclavicular” configuration to the BP cords is possible. This means all three cords of BP lie on the lateral side of the AA. If this condition is recognized, slide the probe more distally. |
Clinical Pearls
• Infraclavicular block is best performed at the level of the pectoralis minor muscle where the cords of the brachial plexus surround the second part of the axillary artery. If the coracobrachialis muscle is within the field of imaging, there is some potential for takeoff of the musculocutaneous nerve and therefore incomplete block.
• Abducting the arm retracts the clavicle, thereby allowing more space to place the block needle for a shallower angle of approach to infraclavicular block.5,6 Furthermore, the neurovascular bundle is straightened, thereby making imaging easier. In this position the brachial plexus lies closer to the skin surface and farther from the pleura compared with other arm positions.
• In the infraclavicular region the axillary artery and vein are separated when the medial cord of the brachial plexus lies between them. This gap can be identified on ultrasound imaging and indicates wall-hugging cords of the brachial plexus (rather than cords that lie on the lateral side of the axillary artery). Performing infraclavicular block where the cords surround the axillary artery is desired for complete brachial plexus anesthesia.
• Although debate continues, most clinical studies have suggested that brachial plexus anesthesia can be achieved with a single injection of local anesthetic under the second part of the axillary artery for infraclavicular block.7
1 Raj PP, Montgomery SJ, Nettles D, et al. Infraclavicular brachial plexus block: a new approach. Anesth Analg. 1973;52:897–904.
2 Sandhu NS, Capan LM. Ultrasound-guided infraclavicular brachial plexus block. Br J Anaesth. 2002;89(2):254–259.
3 Sauter AR, Smith HJ, Stubhaug A, et al. Use of magnetic resonance imaging to define the anatomical location closest to all three cords of the infraclavicular brachial plexus. Anesth Analg. 2006;103:1574–1576.
4 Chin KJ, Singh M, Velayutham V, et al. Infraclavicular brachial plexus block for regional anaesthesia of the lower arm. Anesth Analg. 2010;111(4):1072.
5 Bigeleisen P, Wilson M. A comparison of two techniques for ultrasound guided infraclavicular block. Br J Anaesth. 2006;96:502–507.
6 Auyong DB, Gonzales J, Benonis JG. The Houdini clavicle: arm abduction and needle insertion site adjustment improves needle visibility for the infraclavicular nerve block. Reg Anesth Pain Med. 2010;35(4):403–404.
7 Fredrickson MJ, Wolstencroft P, Kejriwal R, et al. Single versus triple injection ultrasound-guided infraclavicular block: confirmation of the effectiveness of the single injection technique. Anesth Analg. 2010;111(5):1325–1327. Epub 2010, Aug 12