Chapter 34 Infertility and Assisted Reproductive Technologies
 Physiology of Conception
Physiology of Conception
Conception requires the juxtaposition of the male and female gametes at the optimal stage of maturation, followed by transportation of the conceptus to the uterine cavity at a time when the endometrium is supportive of its continued development and implantation (see Chapter 4). For these events to occur, the male and female reproductive systems must be both anatomically and physiologically intact, and coitus must occur with sufficient frequency and at the proper time (preferably a few hours before) to the release of the oocyte from the follicle. Even when fertilization occurs, it is estimated that more than 70% of resulting embryos are abnormal and fail to develop or become nonviable shortly after implantation.
 Basic Evaluations
Basic Evaluations
To keep the status of the evaluation in mind, it is helpful to arrange the workup under a series of five categories that can be mentally reviewed at each visit. Table 34-1 shows the approximate incidence and the tests involved in the evaluation of each category. Box 34-1 summarizes the treatment options for infertility. In 5% to 10% of couples, no explanation can be found (idiopathic infertility).
| Factor | Incidence (%) | Basic Investigations |
|---|---|---|
| Male, coital | 40 | Semen analysis |
| Postcoital test | ||
| Ovulatory | 15-20 | Urinary luteinizing hormone self-test∗; serum progesterone∗ |
| Cervical | 5 | Postcoital test |
| Uterine, tubal | 30 | Hysterosalpingogram |
| Laparoscopy | ||
| Peritoneal | 40 | Laparoscopy |
∗ Investigations only when menses are regular (every 22 to 35 days); oligomenorrhea generally requires treatment.
 Etiologic Factors
Etiologic Factors
MALE COITAL FACTOR
Investigations
A semen analysis should be performed following a 2- to 4-day period of abstinence. The entire ejaculate should be collected in a clean, nontoxic container. Until relatively recently, the full range of normal variation was not appreciated. Characteristics of a normal semen analysis are shown in Table 34-2.
| Characteristics | Quantity |
|---|---|
| Semen volume | 2-5 mL |
| Sperm count | Greater than 20 million/mL |
| Sperm motility | Greater than 50%∗ |
| Normal forms | Greater than 30% standard morphology or greater than 14% “strict” morphology |
| White blood cells | Fewer than 10 per high-power field or 1 × 106/mL |
OVULATORY FACTOR
Treatment
In women whose menses are less frequent than every 35 days (oligomenorrhea), it is helpful to induce more frequent ovulation, thus increasing the opportunity for pregnancy and improving the ability to time coitus. Ovulation induction should always be preceded by a thorough workup, as discussed in Chapter 32, because conditions causing anovulation may be worsened by pregnancy or may complicate it. In addition, ovarian failure seldom responds to attempts to induce ovulation.
UTERINE OR TUBAL FACTOR
Abnormalities of the uterine cavity are seldom the cause of infertility. Large submucosal myomas or endometrial polyps, as seen in Figure 34-1, may be associated with infertility and first-trimester spontaneous abortions. The role of intramural myomas is not clear, although myomectomy has been associated with conception in 40% to 50% of couples in uncontrolled series, and some studies with IVF have shown reduced conception with intramural myomas. Subserous fibroids do not affect fecundity.
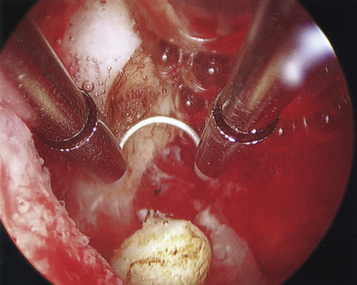
FIGURE 34-1 Photograph of a significant submucous polyp (bottom center) seen at the time of hysteroscopy.
Investigations
Tubal abnormalities may be diagnosed by HSG or laparoscopy. To perform HSG, an occlusive cannula is placed in the cervix, and the instillation of a radiopaque dye is followed with image intensification under fluoroscopy. Selected radiographs are taken for permanent documentation (Figure 34-2). Anesthesia generally is not required. A water-soluble dye is used initially to confirm tubal patency because of the adverse effects of sequestration of an oil-based dye within the lumen of an occluded tube. If patency is confirmed, an oil-based dye may then be instilled because of its prominent therapeutic effect in women with unexplained infertility. If only one tube fills with dye, the hysterosalpingogram should be considered normal because this finding is usually, although not invariably, caused by the dye following the path of least resistance.
PERITONEAL FACTOR
Treatment of endometriosis depends on its extent and is discussed further in Chapter 25. If substantial adhesions or endometriomas are present, laparoscopic surgery is preferable because these conditions generally do not respond to medical management. With advanced operative laparoscopic techniques, most endometriosis can be removed or ablated without laparotomy by using advanced instrumentation, lasers, or fulguration.
 Assisted Reproductive Technologies
Assisted Reproductive Technologies
The last resort for infertile couples with any of the aforementioned factors and failure of lesser treatments is the procedure of IVF and embryo transfer (Figure 34-3). In most cases of tubal occlusion in which the rate of success with tubal repair is low (<30%), IVF is preferable to surgery because of the more rapid conception rate and the lower ectopic pregnancy rate. Even severe male factors can be effectively treated with IVF by using intracytoplasmic sperm injection, with high fertilization rates of injected oocytes and pregnancy rates similar to those of non–male-factor IVF (30% to 35%).
Gambone J.C.L. Are adverse pregnancy and fetal outcomes more common with assisted reproductive technologies? What should patients be told? Clin Obstet Gynecol. 2006;49:123-133.
Mayo Clinic: Infertility. Retrieved February 6, 2008, from http://www.mayoclinic.com/health/infertility/DS00310.
Meldrum D.R. Low dose follicle-stimulating hormone therapy for polycystic ovarian disease. Fertil Steril. 1991;55:1039.
Meldrum D.R. Assisted reproductive technologies: Clinical aspects. In: Carr B.R., Blackwell R.F., Azziz R., editors. Essential Reproductive Medicine. New York: McGraw-Hill; 2006:535-560.

 General Principles of Evaluation
General Principles of Evaluation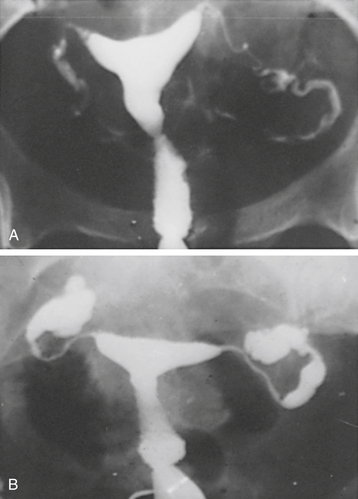
 Unexplained Infertility
Unexplained Infertility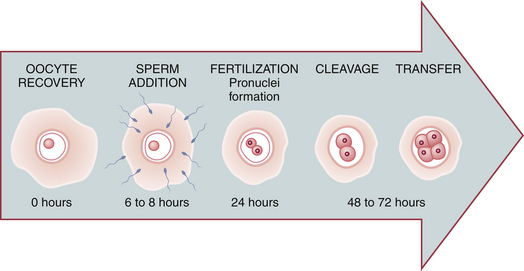
 Overall Success of Infertility Therapy
Overall Success of Infertility Therapy