CHAPTER 18 Inferior Pedicle Breast Reduction Using a Circumvertical Pattern
Introduction
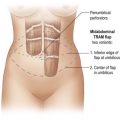
For many years, the preferred method for performing breast reduction has combined the use of an inferiorly based pedicle with an inverted T or ‘Wise’ skin pattern and many reports have documented the success of this technique in reducing the symptomatically enlarged breast.1–6 However, it is possible to combine the inferior pedicle approach with a short scar circumvertical skin pattern to accomplish the same reduction in volume with a much less significant scar burden. This procedure, called the short scar periareolar inferior pedicle reduction or SPAIR mammaplasty7–9 is applicable to breasts of all sizes and provides aesthetic, long-lasting results in a consistent fashion. This chapter will outline the markings, operative technique, and results of this versatile method of breast reduction.
Patient Selection
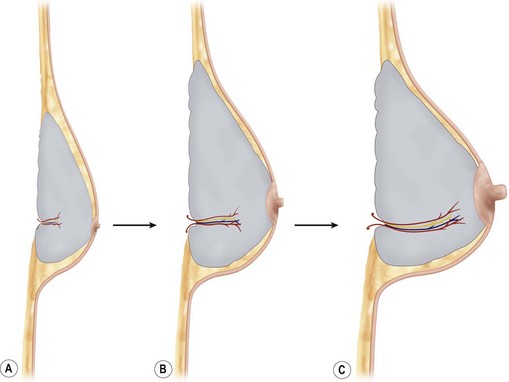
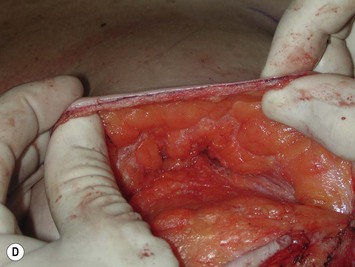
While pedicle length is an important variable that can influence the subsequent development of ischemia to the NAC, another anatomic feature of the breast that directly affects the vascularization of the inferior pedicle relates to the identification and preservation of the internal breast septum.10–12 This septum, which has a cranial and caudal leaf, runs transversely within the breast at the junction of the lower third with the upper two-thirds and most likely represents a traction imbrication as the enlarging breast folds over itself as it hypertrophies (Fig. 18.1). Within this septum run several sizable intercostal perforators that provide direct axial blood flow to the inferior pedicle. As such, the septum functions as a neurovascular mesentery. The septum is easily identified in most patients during skeletonization of the inferior pedicle (Fig. 18.2). Once the redundant tissue is removed from the apex of the pedicle near the base of the breast, the mesenteric space can be seen to present a mobile interface as the cranial and caudal layers slide past one another. Preserving this vascular mesentery becomes a critical technical maneuver when attempting to ensure adequate vascularization of the inferior pedicle.
Operative Technique
Marking
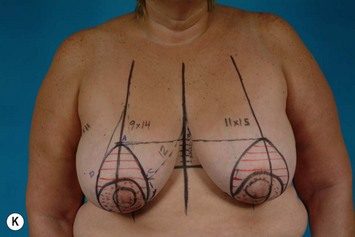
When marking the patient for an inferior pedicle circumvertical procedure, the basic goal is to determine that portion of the redundant skin envelope that will need to be preserved so as to easily wrap around the inferior pedicle in a contoured fashion to create the most aesthetic result. To accomplish this task, four cardinal points are identified that will define that portion of the skin envelope that will be preserved. Initially, basic orientation marks are applied to identify the inframammary fold on each side, the midsternal line and the breast meridian (Fig. 18.3A–D). It should be noted that the breast meridian does not necessarily run through the nipple as often the NAC is malpositioned either medially or laterally. As well, it is a very useful maneuver to draw a line across the midline connecting the two inframammary folds. This allows the location of the fold to be visualized without manipulating and possibly distorting the position of the breast. The first cardinal mark is located by drawing a line that parallels the inframammary fold line 4 cm above the inframammary fold. Where this line intersects the breast meridian on each side represents the top of the periareolar pattern (Fig. 18.3E). The inferior cardinal point is identified by drawing an 8 cm wide pedicle that extends up to the NAC centered on the breast meridian (Fig. 18.3F). The length of this pedicle mark varies slightly with a pedicle length of 8 cm being used for mastopexies and small breast reductions of less than 400 g, and 10 cm being used for larger breast reductions of more than approximately 800 g (Fig. 18.3G). Medially and laterally, the standard breast displacement maneuver used in traditional vertical mammaplasty procedures is used to estimate how much medial and lateral skin will need to be preserved to easily wrap around the breast. By gently rotating the breast first up and out, and then up and in, the breast meridian can be ghosted onto the periareolar pattern to identify the medial and lateral cardinal points (Fig. 18.3H, I). Communicating these four cardinal points into an elongated oval identifies the limits of skin resection that will be required to properly reduce the dimensions of the skin envelope (Fig. 18.3J). The inferior pedicle is drawn in skirting the top of the existing areola by 1–2 cm to complete the pattern (Fig. 18.3K).
Surgical technique
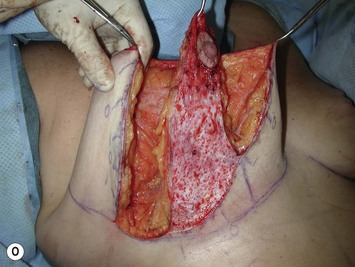
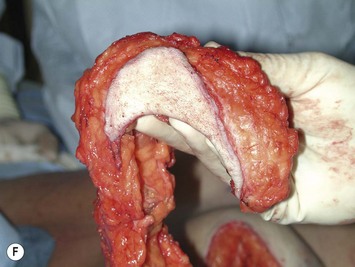
At surgery, a breast tourniquet is applied to place the areola under maximum stretch and a 40–44 mm areolar diameter is marked with the aid of a circular template (Fig. 18.4A). The inferior pedicle is de-epithelialized as is a rim of dermis around the periareolar pattern (Fig. 18.4B). The dermis is divided around the periareolar opening taking care to leave a 5 mm dermal shelf that will eventually hold the purse-string suture (Fig. 18.4C). Medial, and superior flaps are then developed by initially dissecting just under the dermis and then curving smoothly downward creating a progressively thicker flap until the pectoralis major muscle is reached (Fig. 18.4D, E). In this fashion, the flaps are developed in such a way that the thinner leading edges of the flaps will smoothly redrape around the periareolar opening once the purse-string suture is cinched down without creating any tissue crowding; however, enough tissue is left behind at the base of the breast to create smooth even contours around the periphery of the reduced breast. Laterally the flap must be thinner and dissection is performed at the junction of the lateral skin flap with the breast fascia. If the lateral breast flap is made thicker than this, the breast will appear overly wide. It is important to note that the inframammary fold is not disrupted during this dissection and all the normal attachments of the fold are preserved to prevent postoperative bottoming out. Once the flaps have been developed, the inferior pedicle is skeletonized being careful not to undermine the pedicle in any way and potentially divide the breast septum. The specimen that is then removed is in the shape of a horseshoe with lateral limb being slightly longer than the medial limb (Fig. 18.4F, G).
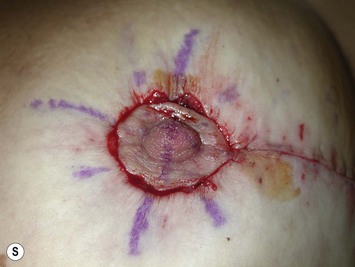
To apply the circumvertical pattern, traction is applied to the tip of the inferior pedicle by grasping the dermis above the areola and pulling upward. As a result, the periareolar opening will then be seen to buckle on either side of the pedicle and these two points are grasped and temporarily stapled together to form the key staple point (Fig. 18.4H, I). Hemostats are then applied to the dermis at this point and upward traction is applied to the inferior skin envelope. As a result of this maneuver, the skin of the lower pole will be seen to fold inward (Fig. 18.4J). This imbrication line is then likewise stapled together until a rounded and pleasing lower pole contour is created (Fig. 18.4K). The areola is temporarily stapled into the remaining periareolar defect and the shape of the breast is assessed with the patient upright (Fig. 18.4L). Further tightening or even loosening of the vertical plication pattern can be performed as needed to create the desired breast shape. Once the extent of the vertical component has been finalized, the edges are marked with a surgical pen and the staples removed (Fig. 18.4M, N). The inferior pedicle is de-epithelialized and the redundant medial and lateral wedges of tissue on either side of the pedicle are removed (Fig. 18.4O) and the vertical incision is closed in layers with 4-0 absorbable monofilament suture (Fig. 18.4P). Once again the patient is placed upright and the shape of the remaining periareolar defect is assessed. If it is not perfectly circular, a surgical marker is used to mark a perfect circle and the redundant skin is removed, keeping in mind the need to leave behind a small dermal shelf. The areola is then inset into the periareolar defect using a CV-3 polytetrafluoroethylene (PTFE) suture placed in an interlocking fashion.13 In this technique, eight evenly spaced bites of dermis are incorporated into a standard periareolar purse string suture to join the dermal edges of the areola to the like edges of the periareolar incision (Fig. 18.4Q–S). In doing so, the tendency for the areola to spread postoperatively is minimized. The PTFE suture is used preferentially for this purpose due to the handling qualities of the material and the fact that it slides so easily through the dermal framework, thus allowing the diameter of the areolar opening to be easily controlled. The areola is then inset using a single subcuticular 4-0 absorbable monofilament. No deep intradermal sutures are used to avoid inadvertent cutting of the interlocking PTFE suture. At the conclusion of the case, the shape of the breast should be reasonably aesthetic (Fig. 18.4T). Certainly the breast should not have an intentionally distorted appearance as noted with some vertical techniques. In the ideal situation, the lower pole of the breast should appear mildly flattened to allow for postoperative resolution of swelling and mild stretching of the skin envelope. Most importantly, however, is the fact that the position of the inframammary fold does not change postoperatively, a fact that contributes greatly to the long term stability of the result.
Results
The results using this technique are reliably obtained and long lasting. The shape created at the time of surgery is aesthetic and the mild settling of the breast that occurs over time tends to only improve the overall result. By the 6 month postoperative visit, the result has stabilized for most patients. The technique is best used for patients who require breast reductions of 400–800 g (Figs 18.5 and 18.6). Below this, the smaller periareolar defect can mildly limit exposure and above this, the resection and redraping of the skin envelope can present a technical challenge. Despite these factors, the results obtained for a wide range of patients ranging from mastopexy alone to reductions of greater than 1500 g can demonstrate an aesthetic breast shape with few complications.
1 Courtiss EH, Goldwyn RM. Reduction mammaplasty by the inferior pedicle technique. An alternative to free nipple and areola grafting for severe macromastia or extreme ptosis. Plast Reconstr Surg. 1977;59(4):500-507.
2 Robbins TH. A reduction mammaplasty with the areola-nipple based on an inferior dermal pedicle. Plast Reconstr Surg. 1977;59(1):64-67.
3 Georgiade NG, Serafin D, Morris R, Georgiade G. Reduction mammaplasty utilizing an inferior pedicle nipple-areolar flap. Ann Plast Surg. 1979;3(3):211-218.
4 Robbins TH. Inferior pedicle breast reduction technique. Plast Reconstr Surg. 1984;73(2):325.
5 Mandrekas AD, Zambacos GJ, Anastasopoulos A, Hapsas DA. Reduction mammaplasty with the inferior pedicle technique: early and late complications in 371 patients. Br J Plast Surg. 1996;49(7):442-446.
6 O’Grady KF, Thoma A, Dal Cin A. A comparison of complication rates in large and small inferior pedicle reduction mammaplasty. Plast Reconstr Surg. 2005;115(3):736-742.
7 Hammond DC. Short scar periareolar inferior pedicle reduction (SPAIR) mammaplasty. Plast Reconstr Surg. 1999;103(3):890-901.
8 Hammond DC. The SPAIR mammaplasty. Clin Plast Surg. 2002;29(3):411-421.
9 Hammond DC, Alfonso D, Khuthaila DK. Mastopexy using the short scar periareolar inferior pedicle reduction technique. Plast Reconstr Surg. 2008;121(5):1533-1539.
10 Würinger E, Mader N, Posch E, Holle J. Nerve and vessel supplying ligamentous suspension of the mammary gland. Plast Reconstr Surg. 1998;101(6):1486-1493.
11 Würinger E. Refinement of the central pedicle breast reduction by application of the ligamentous suspension. Plast Reconstr Surg. 1999;103(5):1400-1410.
12 Würinger E, Tschabitscher M. New aspects of the topographical anatomy of the mammary gland regarding its neurovascular supply along a regular ligamentous suspension. Eur J Morphol. 2002;40(3):181-189.
13 Hammond DC, Khuthaila DK, Kim J. The interlocking Gore-Tex suture for control of areolar diameter and shape. Plast Reconstr Surg. 2007;119(3):804-809.