CHAPTER 37 Inferior Flaps for Tuberous Breasts
Key Points
Introduction
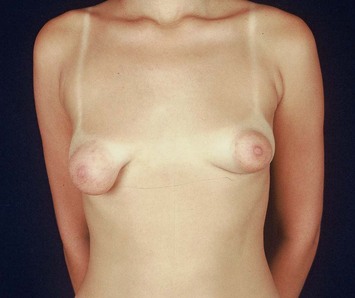
Tuberous breast was first described in 1976 by Rees and Aston1 and received this name because of its resemblance to a ‘tuberous plant root.’ Also called ‘tubular breast,’ ‘snoopy breast’ or ‘herniated areolar complex,’ it represents one of the most challenging surgical conditions of the breast because of its tendency to recur. It is considered the most severe and most typical form of a group of breast anomalies called breast base anomalies (Fig. 37.1).2 Dinner3 considers it a syndrome rather than a single deformity, consisting of: (1) hypertrophy of the nipple–areola complex; (2) pseudoherniation of the breast content into the areola, producing the very typical Snoopy-dog-nose deformity; (3) hypoplasia with commonly related asymmetry with the contralateral side; (4) vertical constriction with the reduced superior inferior diameter; and (5) a constricted transverse base. It is a rare condition, affecting young women unilaterally or bilaterally and its incidence remains unknown.
Patient Selection
Its etiology remains controversial. Recent observations led to two possible theories, both based on anomalies of the fascia superficialis. In the first, it could take the form of strong adherence between the dermis and the muscular plane, which could not be divided by the development of the breast.2 In the second, there is the presence of a constricting fibrous ring in the periphery of the nipple–areola complex, a consequence of a thickening of the superficial fascia.4 In both cases, the result is the impairment of the normal development of the breast, restricting its peripheral expansion, especially in the lower quadrants where the alterations are more intense. As a consequence, narrowing of the breast base with preferential forward development into the areolar area, were the fascia superficialis is absent, occurs, giving the breast its tubular appearance and enlarging the areola. The severity of the deformity parallels the degree of malformation of the fascia superficialis ranging from minor degrees of hypoplasia of the lower medial quadrant to severe breast constriction and pseudoherniation of the areola. Our clinical observations led us to the theory of the presence of the constricting fibrous ring and we consider its disruption as the most important step in the treatment of the disorder.5–8
Indications
The tuberous breast is the most typical form of a group of disorders that are characterized by anomalies of the breast base and that generally involve the lower quadrants. Von Heimburg et al classified it into four types:9
Operative Technique
In order to correct the deformity, it is necessary to disrupt the constricting ring. This is done in our technique by the creation of a inferiorly based dermal–adipose–glandular flap, also called inferior ‘pedicle’, that was created by the senior author in 1973.10 Another key maneuver is the redistribution of the mammary tissue, to allow the filling of the inferior quadrants and the enlargement of the constricted base of the breast. The procedure is easily performed and may also include an implant placement.6–8
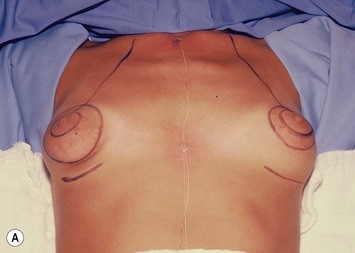
Markings
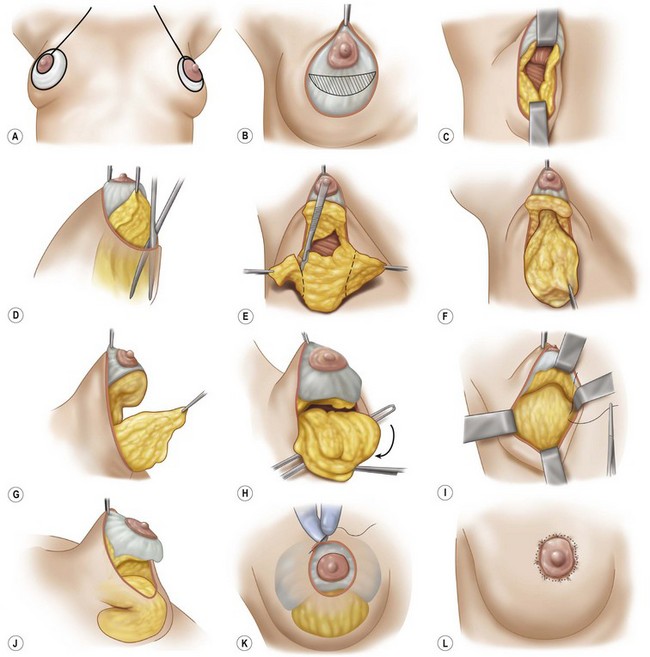
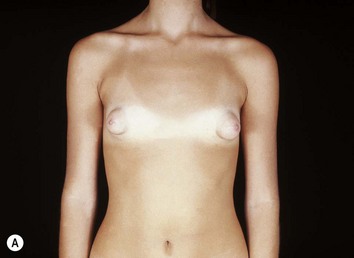
With the patient in supine and half-seated position, the new areola is drawn with a diameter of 4 cm. The external limit of the areola is also drawn, demarcating the excess areola to be removed. The submammary sulcus is marked, and this represents the inferior limit of dissection of the inferior flap to be created. In cases of highly hypoplastic lower quadrants we discard the actual position of the sulcus and mark it more inferiorly in a new desired position. It is important to mention that asymmetry is frequently present, so the markings are made independently (Figs 37.2A and 37.3A).
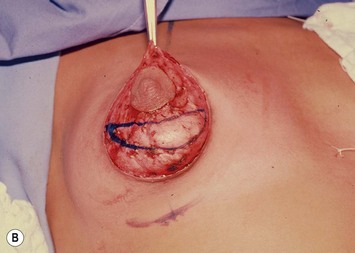
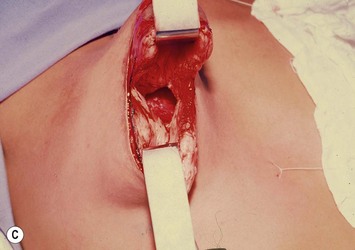
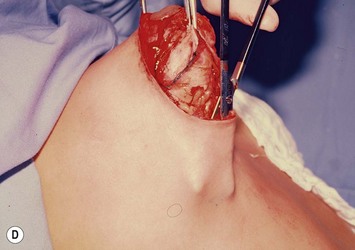
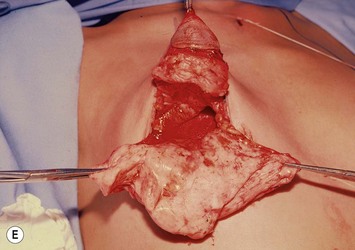
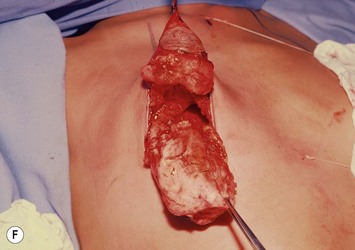
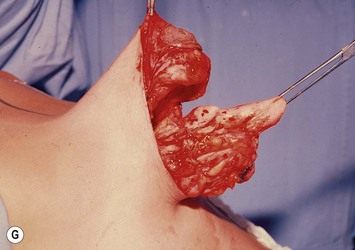
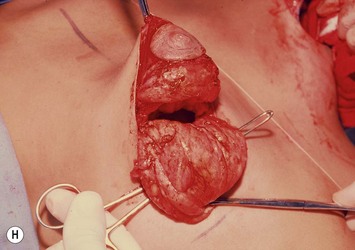
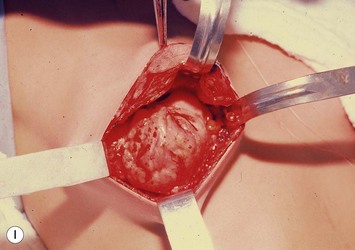
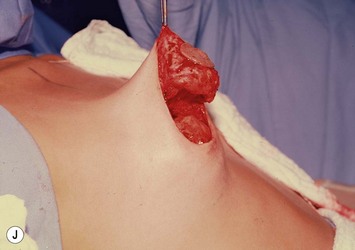
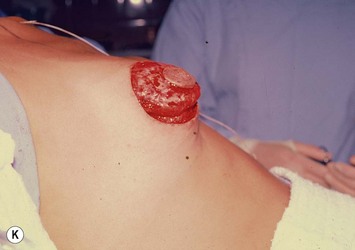
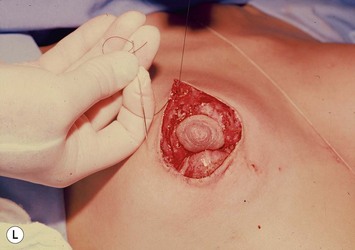



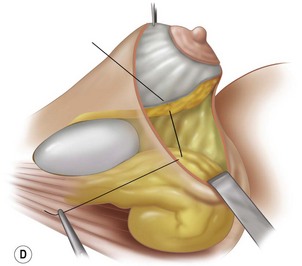
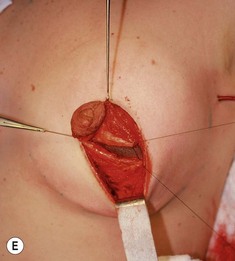
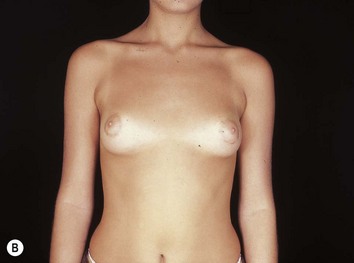
Fig. 37.3 A Markings. New areola with 4 cm diameter, excess halo and a new inframammary fold are drawn (illustrated in Figure 37.2A). B Circumareolar region already de-epithelialized and drawing of the reference line for gland division into upper and lower hemispheres and creation of the inferior flap. (Illustrated in Figure 37.2B.) C Complete breast gland division up to the muscular plane (illustrated in Figure 37.2C). D Undermining of the inferior pole with scissors (illustrated in Figure 37.2D). E Inferior pole completely freed from its skin (illustrated in Figure 37.2E). F Inferior flap created after resection of the lateral and medial prolongations (illustrated in Figure 37.2F). G Lateral view of the upper pole with the areola and the inferior flap (illustrated in Figure 37.2G). H Starting the fixation of the flap on the thoracic wall. The flap is bent over itself, inferiorly to its base, so that the inferior quadrants are fulfilled (illustrated in Figure 37.2H). I The fixation of the flap is done with non-absorbable sutures (illustrated in Figure 37.2I). J Lateral view of the inferior flap in position after being fixed to the thoracic wall. Note the filling of the inferior quadrants (illustrated in Figure 37.2J). K The upper hemisphere is left to lay over the inferior flap, promoting an enlargement of the entire breast base (illustrated in Figure 37.2K). L The round-block (Peled–Benelli) suture technique (illustrated in Figure 37.2K). M The round-block suture completed (illustrated in Figure 37.2K). N Operative final view. The areola is sutured with nylon 6-0 separate stitches (illustrated in Figure 37.2L). O Immobilization of the breast with Micropore tape. It is left in place for 7 days. Note the suction drain exiting through the axilla (illustrated in Figure 37.2L).
Surgery without breast implants
The circumareolar region is de-epithelialized (Figs 37.2B and 37.3B). Creation of the inferior based flap is started by the division of the gland in two halves with an incision in the infra-areolar region perpendicular to the thoracic wall and reaching the pectoral fascia (Figs 37.2C and 37.3C). This creates the superior hemisphere which keeps the nipple–areola complex and the inferior hemisphere from which the inferior flap will be made. The inferior portion of the gland is freed from its skin with the use of a scissor limiting the dissection to the sulcus previously marked (Figs 37.2D and 37.3D). The lateral and medial prolongations of the gland are freed and resected with care being taken not to injure the perforating vessels from the fourth and fifth intercostal vessels (Figs 37.2E and 37.3E). The creation of this flap will lead to the disruption of the constricting ring which is responsible for the herniation (Figs 37.2F, G and 37.3F, G). Mounting of the breast begins with the fixation of the inferior flap on the thoracic wall. The distal end of the flap is fixed inferiorly to its base, bending it over itself, using non-absorbable sutures (Figs 37.2H, I and 37.3H, I). This maneuver is important to fill the inferior quadrants that generally are hypoplastic (Figs 37.2J and 37.3J). The upper portion is left to fall naturally over the inferior flap causing the mammary base to become enlarged (Fig. 37.3K). The breast is closed using a periareolar suture by the technique of Peled and Benelli11,12 performed with 2-0 nylon (Figs 37.2K and 37.3L, M). The areolar suture is done with separate stitches using 6-0 nylon (Figs 37.2L and 37.3N). Suction drains are left for 24 hours. Immobilization of the breast with Micropore tape is important and remains for 7 days (Fig. 37.3O).
Summary of surgical steps
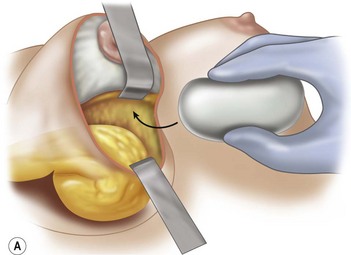
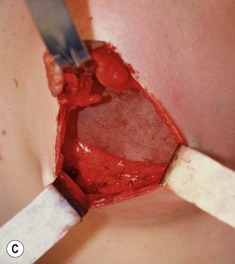
Surgery with breast implants
The surgery is performed in the same way except that the silicone prosthesis is inserted after the fixation of the inferior flap to the thoracic wall. The pocket is made between the superior hemisphere and the inferior flap and the implant is inserted into the existing space (Fig. 37.4A, B). After the introduction of the implant (Fig. 37.4C), the space is closed with separate stitches fixing the inferior border of the superior segment to the superior border of the inferior flap (Fig. 37.4D, E). The skin is closed in the same way as described (Fig. 37.4F).
Conclusion
The abundance of techniques available in the literature for the correction of the tuberous breast attests to the great challenge of treating this deformity. The periareolar approach with de-epithelialization of the excessive areola and its closure with a round-block suture are common to various techniques. The main feature of our technique, and what separates it from others, is the prevention of recurrence by dividing the gland in two halves and creating the inferiorly based glandular flap. Both of these maneuvers account for the disruption of the constricting ring. Our technique has successfully corrected this deformity (Figs 37.5–37.7), which can affect the patients so severely from a psychological standpoint, with pleasing aesthetic results and no recurrence.
1 Rees TD, Aston SJ. The tuberous breast. Clin Plast Surg. 1976;3:339.
2 Grolleau JL, Lanfrey E, Lavigne B, Chavoin JP, Costagliola M. Breast base anomalies: treatment strategy for tuberous breasts, minor deformities, and asymmetry. Plast Reconstr Surg. 1999;104(7):2040.
3 Dinner MI. Discussion. Tuberous breast: a new approach. Plast Reconstr Surg. 1998;101(1):51.
4 Mandrekas AD, Zambacos GJ, Anastasopoulos A, Hapsas D, Lambrinaki N, Ioannidou-Mouzaka L. Aesthetic reconstruction of the tuberous breast deformity. Plast Reconstr Surg. 2003;112(4):1099.
5 Ribeiro L, Canzi W, Buss AJr, Accorsi AJr. Tuberous breast: a new approach. Plast Reconstr Surg. 1998;101(1):42.
6 Ribeiro L, Accorsi AJr, Buss A, Pessôa MCM. Short scar correction of the tuberous breast. Clin Plast Surg. 2002;29(3):423.
7 Ribeiro L, Accorsi AJr, Argencio V. Tuberous breast: a periareolar approach. Aesth Surg J. 2005;25:398.
8 Ribeiro L, Accorsi AJr. Mama tuberosa. In: Rietjens M, Urban CA, editors. Cirurgia da Mama, Estética e Reconstrutora. Rio de Janeiro: Revinter; 2007:191-201.
9 von Heimburg HD, Exner K, Kruft S, Lemperle G. The tuberous breast deformity: classification and treatment. Br J Plast Surg. 1996;49:339.
10 Ribeiro L, Baker E. Mastoplastia con pedículo de seguridad. Rev Esp Cir Plast. 1973;16:223.
11 Peled IJ, Zagher U, Wexler MR. Purse string suture to reduction and closure of skin defects. Ann Plast Surg. 1985;14(5):465.
12 Benelli L. Technique personnelle de plastie mammaire periareolaire: le round block. Cah Chir. 1991;77:15.