17 Infective endocarditis
Salient features
History
• Fever, malaise, anorexia, weight loss, rigors: non-specific symptoms of inflammation
• Progressive heart failure: caused by valve destruction (can be dramatic)
• Stroke, pulseless limb, renal infarct, pulmonary infarct: caused by embolization of vegetations
• Arthralgia, loin pain: caused by immune-complex deposition
• Obtain a history of recent dental procedures
• History of valvular heart disease, history of IV drug abuse
Examination
• Look for the following signs:
• Listen to the heart for murmurs and look for signs of cardiac failure.
• Examine the fundus for Roth’s spots (vasculitic phenomena).
• Examine the abdomen for splenomegaly.
• Look for embolic phenomena: stroke, viscera or occlusion of peripheral arteries.
• Test urine for microscopic haematuria (vasculitic phenomena).
• Remember that ostium secundum atrial septal defects almost never have infective endocarditis.
Questions
How would you investigate such a patient?
• Test the urine for microscopic haematuria.
• Take a FBC to show normocytic, normochromic anaemia and raised white cell count.
• Test for raised erythrocyte sedimentation rate (ESR).
• Blood culture: take three samples from different sites in 24 h. It is the most important test for diagnosing endocarditis and cultures are negative in >50% of cases of fungal aetiology.
• Transthoracic echocardiography may show vegetations. A negative study does not rule out endocarditis as vegetations <3–4 mm in size cannot be detected. Furthermore, all the leaflets of the aortic, tricuspid and pulmonary valves may not be visualized in every patient. Transoesophageal echocardiography is usually indicated in infective endocarditis.
What are the major categories of infective endocarditis?
What do you know about the pathogenesis of this condition?
1 The primary event is bacterial adherence to damaged valves. This occurs within minutes during transient bacteraemia and involves valve tissue and bacterial factors.
2 The second step involves persistence and growth of bacteria within the cardiac lesions, usually associated with local extension and tissue damage.
3 Third step is the dissemination of septic emboli to kidney, spleen and brain
What are the major manifestations of bacterial endocarditis?
• Manifestations of a systemic infection: fever, weight loss, pallor, splenomegaly.
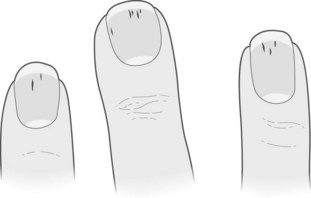
• Manifestations of vasculitic phenomenon: cardiac failure, changing murmurs, petechiae, Roth’s spots, Osler’s nodes, Janeway lesions, splinter haemorrhages, stroke, infarction of viscera, mycotic aneurysm.
• Manifestations of immunological reactions: arthralgia, finger clubbing, uraemia.
Note: Mnemonic to remember Duke’s criteria for bacterial endocarditis, BE FEVER:
Advanced-level questions
What do you know of prosthetic valve endocarditis?
• Early: occurring within 2 months of surgery. It develops as a result of intraoperative contamination of the prosthetic valve or as a consequence of a postoperative nosocomial infection, such as sternotomy infection, postoperative pneumonia, urinary tract infection or intravenous catheter-related insertion. The clinical features may be masked by the ordinary events in the postoperative course or by another infection. Cutaneous signs are not common.
• Late: develops >2 months after valve surgery. It can occur after transient bacteraemia as in minor skin or upper respiratory tract infections or following dental or urinary manipulations. The non-cardiac manifestations resemble those of native valve infective endocarditis.
What are the complications of infective endocarditis?
• Congestive heart failure: may develop acutely or insidiously; it portends a grave prognosis
• Conduction disturbances caused by abscesses in ventricular septum
• Valve destruction: acute regurgitation, pulmonary oedema, heart failure
• Embolism: occurs in 22–50% of cases, leading to infarction in any vascular bed, including lungs, coronary arteries, spleen, bowel, renal (flank pain and haematuria) and extremities
• Local extension of infection: purulent pericarditis, aortic root abscess (may cause sinus Valsalva fistula), myocardial abscess (conduction disturbance)
• Septic emboli to vaso vasorum: may lead to mycotic aneurysms anywhere on vascular tree; most worrying in cerebral vessels, resulting in cerebral haemorrhage
• Distal infection (metastatic): caused by septic emboli, e.g. brain abscess, cerebritis
• Candidal endocarditis: may be manifest by fungal endophthalmitis
• Glomerulonephritis: there are two types of renal lesion in subacute bacterial endocarditis (SBE), a diffuse proliferative glomerulonephritis and a focal embolic glomerulonephritis. This is associated with low complement levels and immune complexes.
What are the indications for surgery?
• Positive blood cultures or relapse after several days of the best available antibiotic therapy indicates the need for valve replacement
• Drainage of myocardial or valve ring abscesses
• Patients with aortic valve endocarditis who develop second- or third-degree heart block
• Prosthetic valve replacement for non-streptococcal endocarditis, valve dysfunction, valve dehiscence or myocardial invasion
What are the recommendations for prophylaxis?
According to NICE guidelines (March 2008).
• acquired valvular heart disease with stenosis or regurgitation
• structural congenital heart disease, including surgically corrected or palliated structural conditions, but excluding isolated atrial septal defect, fully repaired ventricular septal defect or fully repaired patent ductus arteriosus, and closure devices that are judged to be endothelialized