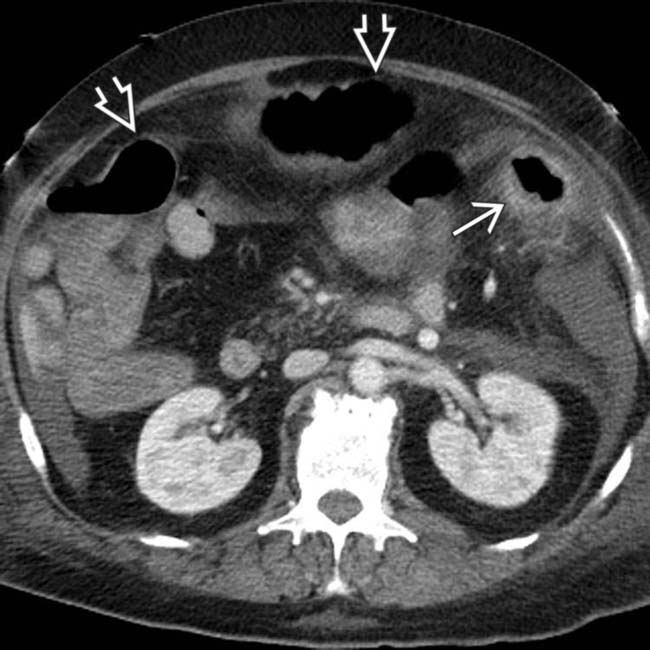
Mucosal hyperenhancement, marked submucosal edema, ascites

 , and ascites. C. difficile colitis typically presents as a pancolitis, as in this example.
, and ascites. C. difficile colitis typically presents as a pancolitis, as in this example.
 and hyperemia of the entire colon and rectum.
and hyperemia of the entire colon and rectum.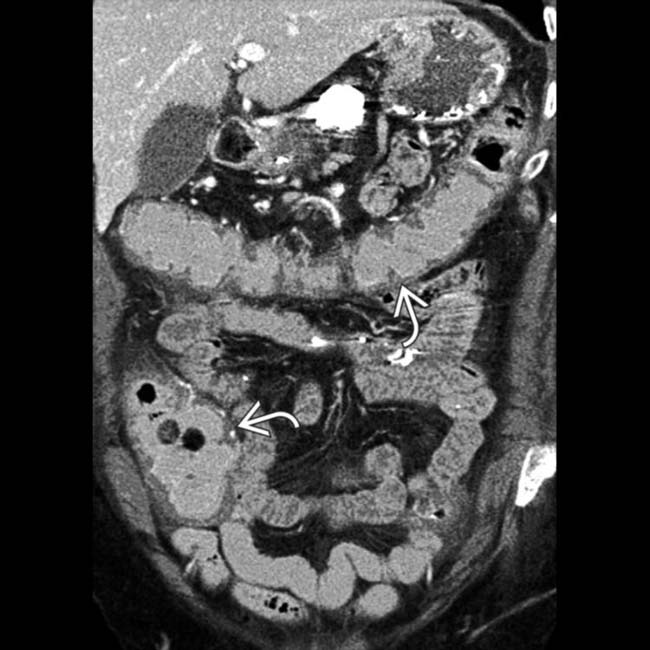
 of the entire colon. C. difficile (pseudomembranous) colitis was confirmed.
of the entire colon. C. difficile (pseudomembranous) colitis was confirmed.IMAGING
General Features
Fluoroscopic Findings
• Contrast enema
 Small nodules or inflammatory polyps ± diffuse mucosal granularity (may simulate ulcerative colitis)
Small nodules or inflammatory polyps ± diffuse mucosal granularity (may simulate ulcerative colitis)
 Possible extrinsic mass with inflammatory changes → distortion, short strictures (may simulate carcinoma)
Possible extrinsic mass with inflammatory changes → distortion, short strictures (may simulate carcinoma)
 Tuberculosis
Tuberculosis
 Small nodules or inflammatory polyps ± diffuse mucosal granularity (may simulate ulcerative colitis)
Small nodules or inflammatory polyps ± diffuse mucosal granularity (may simulate ulcerative colitis) Possible extrinsic mass with inflammatory changes → distortion, short strictures (may simulate carcinoma)
Possible extrinsic mass with inflammatory changes → distortion, short strictures (may simulate carcinoma) Tuberculosis
Tuberculosis
– Oval/circumferential transverse ulcers; loss of demarcation between distorted terminal ileum and ascending colon
CLINICAL ISSUES
Presentation
• Most common signs/symptoms
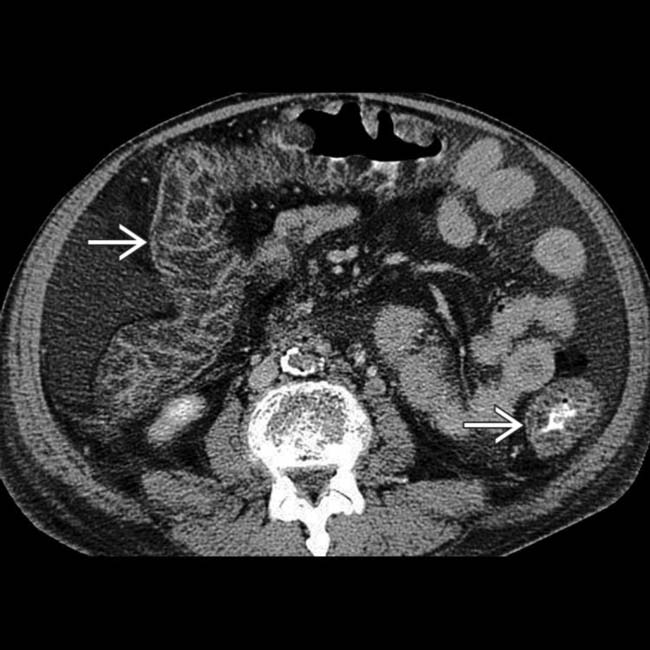
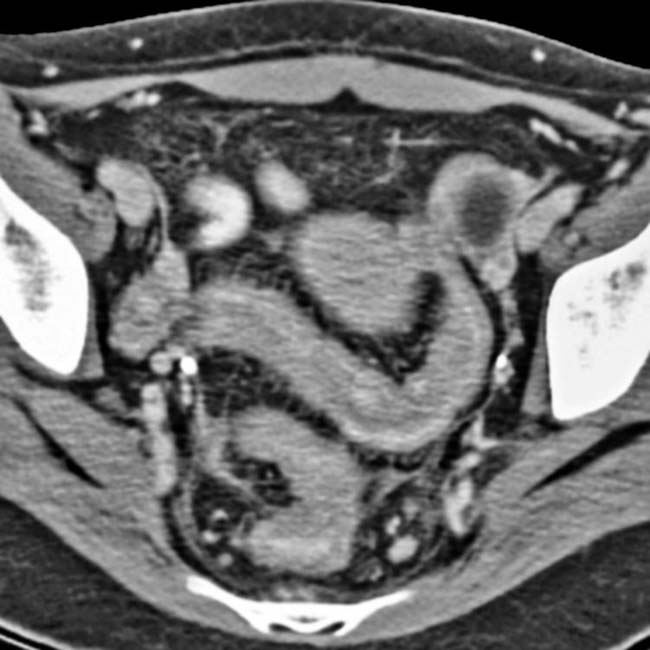
 affecting both the ascending colon and distal ileum. A small amount of ascites
affecting both the ascending colon and distal ileum. A small amount of ascites  is also seen.
is also seen.
 . The etiology was C. difficile infection, an unusual cause of small bowel inflammation.
. The etiology was C. difficile infection, an unusual cause of small bowel inflammation.
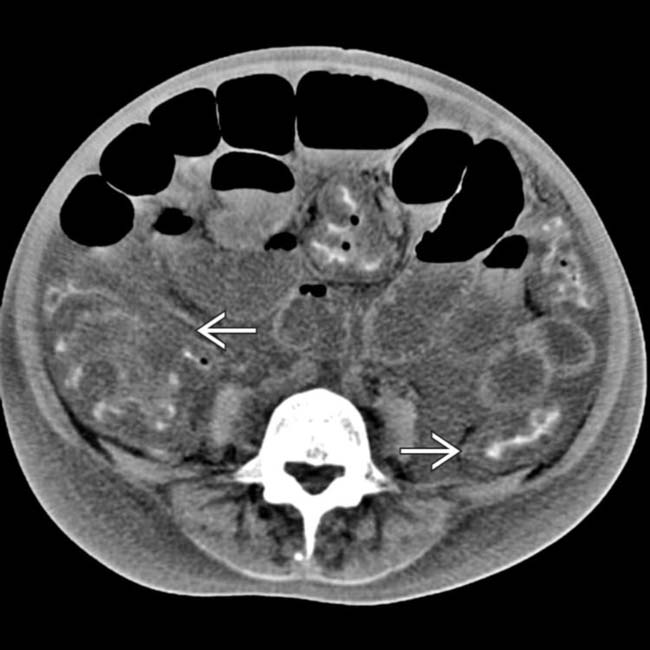
 . The splenic flexure shows mucosal hyperenhancement and submucosal edema
. The splenic flexure shows mucosal hyperenhancement and submucosal edema  .
.
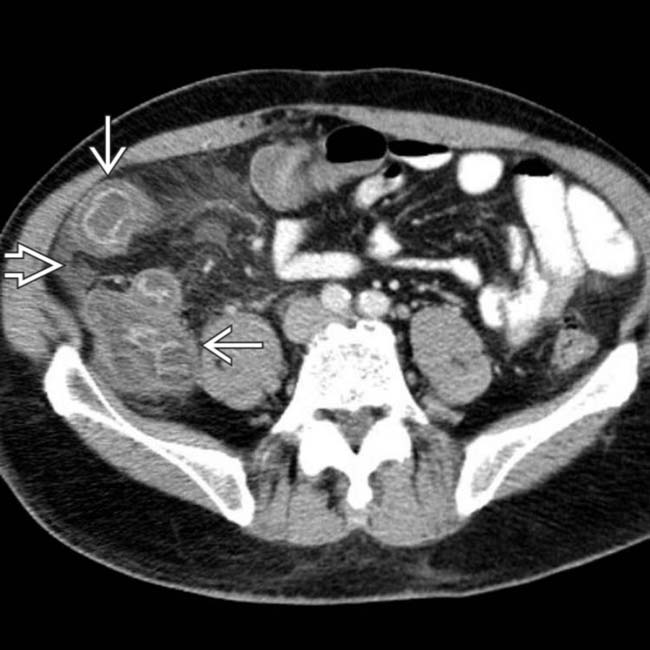
 . These colonic segments seem to have a thin wall, while others are thick walled
. These colonic segments seem to have a thin wall, while others are thick walled  .
.
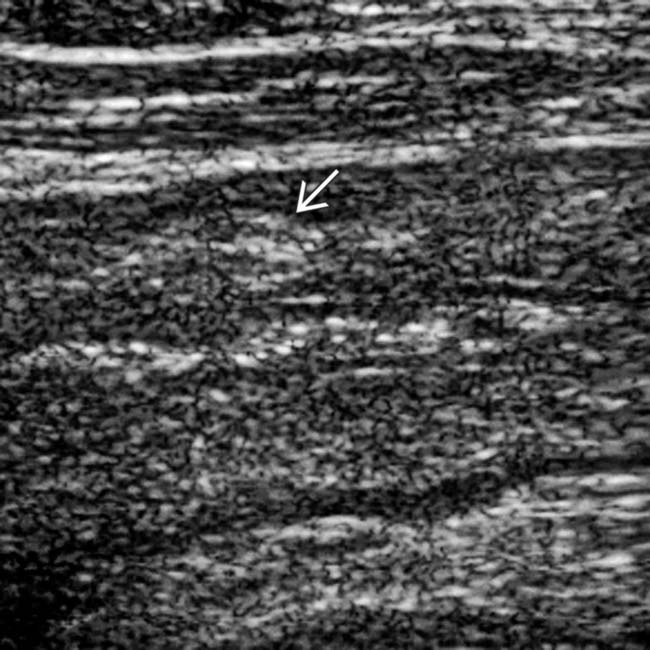
 with loss of normal transverse folds.
with loss of normal transverse folds.

 causing an “accordion” appearance of the colonic wall.
causing an “accordion” appearance of the colonic wall.
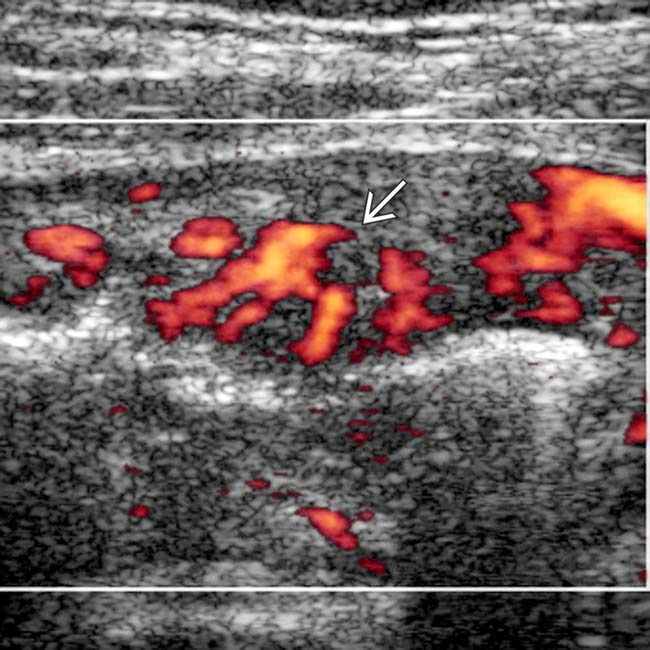
 but not the small bowel. Campylobacter colitis was the final diagnosis.
but not the small bowel. Campylobacter colitis was the final diagnosis.
 .
.
 is massively thickened. On endoscopy (not shown) the colonic mucosa was ischemic and biopsy showed cytomegalovirus (CMV) infiltrating the colonic wall and inducing hemorrhagic necrosis.
is massively thickened. On endoscopy (not shown) the colonic mucosa was ischemic and biopsy showed cytomegalovirus (CMV) infiltrating the colonic wall and inducing hemorrhagic necrosis.
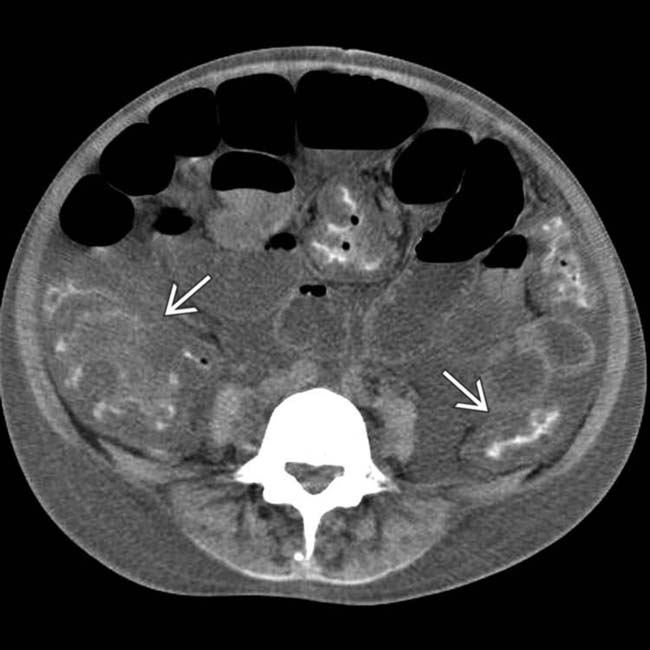
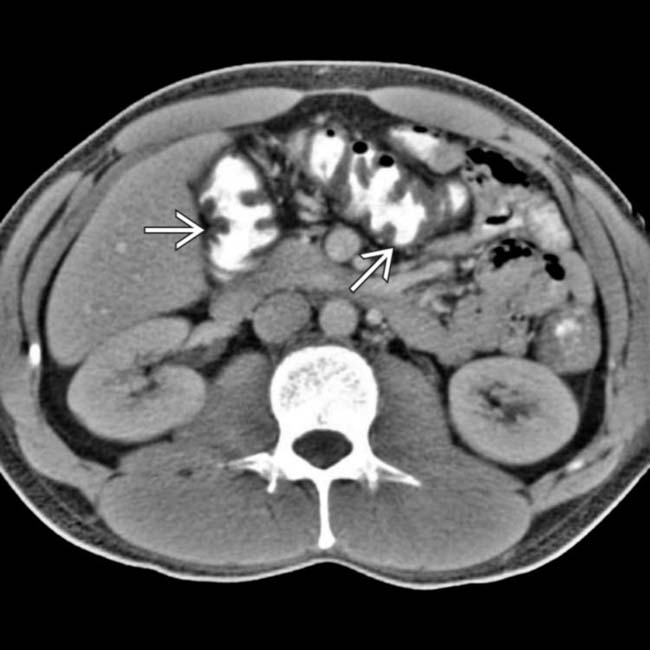
 and RLQ lymphadenopathy
and RLQ lymphadenopathy  .
.
 and additional enlarged nodes
and additional enlarged nodes  . This is a typical example of Yersinia enterocolitis with mesenteric adenitis. Most forms of infectious colitis spare the distal small bowel.
. This is a typical example of Yersinia enterocolitis with mesenteric adenitis. Most forms of infectious colitis spare the distal small bowel.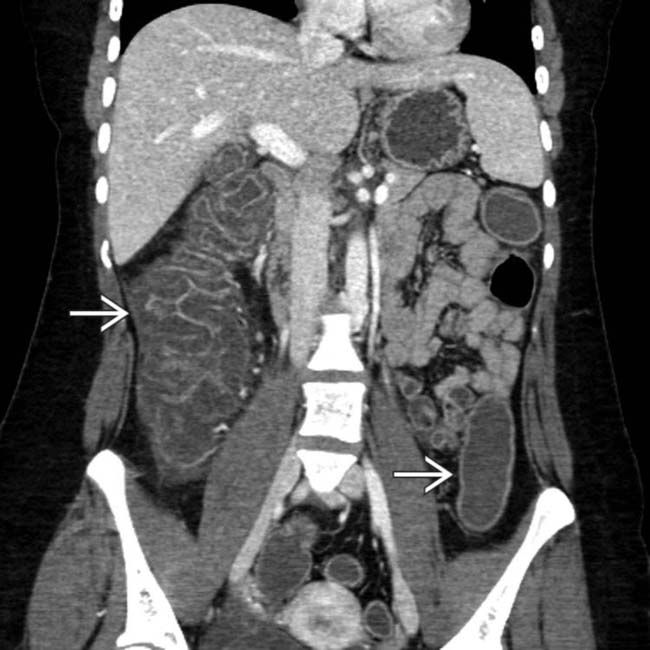
 .
.
 throughout the colon. The small bowel was spared.
throughout the colon. The small bowel was spared.
 primarily affecting the ascending colon. Note that the presence of dense contrast material within the colon impairs evaluation for mucosal inflammation.
primarily affecting the ascending colon. Note that the presence of dense contrast material within the colon impairs evaluation for mucosal inflammation.
 . The left side of the colon seems uninvolved. Preferential involvement of the right colon is characteristic of Salmonella (typhus), which is endemic in some populations.
. The left side of the colon seems uninvolved. Preferential involvement of the right colon is characteristic of Salmonella (typhus), which is endemic in some populations.
 and adjacent mesenteric hyperemia
and adjacent mesenteric hyperemia  . The rectum and small bowel were spared. Campylobacter colitis was confirmed.
. The rectum and small bowel were spared. Campylobacter colitis was confirmed.
 .
.
 is massively thickened. The biopsy showed cytomegalovirus infiltrating the colonic wall and inducing hemorrhagic necrosis.
is massively thickened. The biopsy showed cytomegalovirus infiltrating the colonic wall and inducing hemorrhagic necrosis.
 . Yersinia tends to involve the right colon preferentially, and almost always involves the terminal ileum, unlike most causes of acute infectious colitis.
. Yersinia tends to involve the right colon preferentially, and almost always involves the terminal ileum, unlike most causes of acute infectious colitis.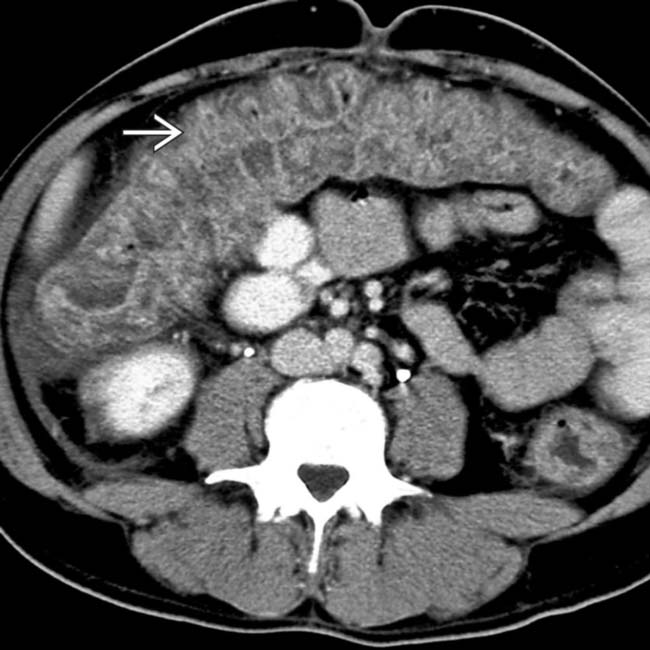
 of the transverse colon.
of the transverse colon.
 .
.

















































































 .
.
 .
.
 .
.

 .
.


