CHAPTER 86 Infections of the Spine
Historic Perspective
The first recorded descriptions of spine infections were those in the Hippocratic texts on tuberculous spondylitis written between the 4th century bc and the 1st century ad. Sir Percival Pott’s description of paralysis in association with tuberculosis of the spine in the 18th century led to the eponym “Pott paraplegia.” His frustration with the inadequate treatment options available to him was shared by physicians for another 150 years: “To attend to a distemper from its beginning through a long and painful course, to its last fatal period, without even the hope of being able to do anything which shall be really serviceable, is of all tasks the most unpleasant.”1
Before the advent of antimicrobial therapy, the treatment of tuberculosis of the spine was based on bed rest, often in a plaster cast, with attention to diet and exposure to fresh air and sunlight. Laminectomy was the mainstay of surgical treatment in the late 1800s and the early part of this century but was later condemned by Seddon and others because it did not address the anterior disease and led to further instability.2 In 1911 Hibbs3 and Albee4 independently described the use of posterior fusion to hasten the recovery. The idea evolved from the demonstration that ankylosis of peripheral joints led to remission of local disease. Unfortunately, posterior fusion did not prevent progressive kyphosis or address the lesion that was causing paralysis, and the technique was later abandoned. The mortality rate for children treated by these various techniques was 40%.5 In 1894 Menard described a series of patients with Pott paraplegia successfully treated with decompression by costotransversectomy.6 The technique fell into disfavor because of a high rate of secondary infection, and it did not gain acceptance until Girdlestone reintroduced it in 1931 with aseptic technique.7
Ito and colleagues8 described the anterior approach to the lumbar spine in 1934 and demonstrated that it provided wider exposure and allowed more radical débridement and fusion. Hodgson and colleagues338,342 popularized the anterior approach for the management of tuberculosis of the spine and stressed radical excision and strut-graft fusion to prevent kyphosis and late-onset paraplegia.
Antituberculous chemotherapy became available in 1945 and was found to be capable of curing the disease even without surgery.9–13 Faced with a number of widely divergent regimens for the treatment of the disease, a group of investigators formed the British Medical Research Council Working Party on Tuberculosis of the Spine. This group set out to perform a number of large-scale, controlled prospective trials of treatment methods. These studies, as well as others to be described later, helped to determine the current treatment recommendations for this disease.
The first recorded description of a pyogenic spine infection was by Lannelongue in 1897.14 Although pyogenic spine infections differ in many ways from tuberculous spondylitis, the surgical treatment of the former has been influenced a great deal by the developments in the management of tuberculosis. The introduction of penicillin and streptomycin revolutionized the treatment of all spine infections. As more powerful antimicrobial agents were developed and combinations and dosages were refined, the relative effectiveness of surgical treatment decreased.
Pyogenic Infections
Vertebral Osteomyelitis
Epidemiology
Although the incidence of tuberculous spondylitis has decreased dramatically in recent years, the incidence of pyogenic vertebral osteomyelitis appears to have increased.15,16 Various reports have stated that vertebral osteomyelitis represents 2% to 7% of all cases of osteomyelitis.17–20 The disease may occur from infancy to old age but has a predilection for the elderly.15,19,21–30 Approximately one half of the patients with spine infections are more than 50 years old and two thirds are male.29 The incidence may be higher in younger patients who are intravenous (IV) drug abusers.2
Etiology
Any condition that causes a bacteremia may lead to hematogenous vertebral osteomyelitis. The most frequent sources are urinary tract infections and the transient bacteremia caused by genitourinary procedures.16,22,24,28,31–33 Of 198 cases in the literature in which the probable source of infection was noted, it was the genitourinary tract in 29%, soft tissue infections in 13%, and respiratory tract infections in 11%; 1.5% of the infections occurred in IV drug abusers,29 but this association is being reported with increasing frequency.29,34–39 Vertebral osteomyelitis may also be caused by direct inoculation of bacteria into the spine by penetrating wounds, spine surgery, chemonucleolysis, or discography.29,40–49 The source of infection could not be identified in 37% of cases.29 Immunocompromised hosts appear to be particularly susceptible to spine infections.22,29,31,33 In particular, diabetics have a high incidence of vertebral osteomyelitis.16,21,31,50 Those who are human immunodeficiency virus (HIV) positive are also predisposed to develop spinal infections even when IV drug users are eliminated from the study group.51 In a recent series of 253 patients from the Cleveland area, 33% of infections were acquired in the hospital. In total, 51% of patients had predisposing extravertebral infections with most due to hematogenous spread from urinary tract, skin and subcutaneous tissues, infected vascular access sites, endocarditis, and bursitis of septic arthritis.52 Kulowski thought that trauma was a predisposing factor in pyogenic vertebral osteomyelitis.27 More recent studies have not supported that association.2,28,31 In Sapico and Montgomerie’s29 review of 207 literature cases in which the presence or absence of blunt trauma was discussed, in only 5% was there a history of trauma.
Bacteriology
In 1931 Hatch reviewed the literature and reported that the causative organism was almost exclusively Staphylococcus aureus.53 There has been an increase in the number of gram-negative bacillary infections.24 In the series from Cleveland, gram-negative bacilli accounted for 23% of infections.52 From data reported in the postantibiotic era, Sapico and Montgomerie29 found that 67% of 222 patients were infected with gram-positive aerobic cocci; S. aureus constituted 55% of the total. The emergence of tolerant S. aureus is a concern, and such strains may become more prevalent with the widespread use of antibiotics.54 The most frequently isolated gram-negative organisms are Escherichia coli, Pseudomonas species, and Proteus species. These are frequently found in association with genitourinary tract infection.24,31,32,55–57 Pseudomonas aeruginosa is frequently isolated from heroin abusers.34,36,38,58–60 In a review of 67 reported cases, gram-negative aerobic bacilli were isolated in 82% of the cases and Pseudomonas was the pathogen in 66%.38 However, one series included 15 IV drug abusers with pyogenic vertebral osteomyelitis and all 11 with positive cultures were infected with S. aureus.22 The likelihood of isolating an organism in the blood is most likely when fever is present. In the absence of a fever, bacteremia can only be detected in 21% of patients.52
Salmonella osteomyelitis is uncommon. It generally occurs after an acute intestinal infection, but the interval between the gastroenteritis and the onset of osteomyelitis may be quite long61; in some cases, no previous infection can be identified.62 Salmonella has a strong tendency to localize in tissues where there is preexisting disease.61,63 Infection with anaerobic bacteria is unusual and is generally associated with foreign bodies, open fractures, infected wounds, diabetes, or human bites.29,64
Infection caused by multiple organisms is encountered in up to 8% of cases.29,65 Infection with Haemophilus species has been reported but is extremely rare in adults.66,67 Low-virulence organisms such as diphtheroids and coagulase-negative staphylococci may cause indolent infections with delayed diagnosis.68 These organisms may grow slowly and cultures should be held for 10 days before they are considered to be negative. Low-virulence organisms should not be dismissed as contaminants in patients suspected clinically to have vertebral osteomyelitis.68 In one series of 111 cases of pyogenic vertebral osteomyelitis, low-virulence organisms caused 48% of the infections in the 61 patients who were 60 years of age or older and 55% of the 44 patients who had an impaired immune system.22
Pathogenesis/Pathology
Although the nucleus pulposus is an avascular tissue, it is relatively active metabolically.69 It receives its nutrition via diffusion across the endplates and from blood vessels at the periphery of the annulus fibrosus.69 In the developing spine, orderly arranged cartilage canals within the endplate contain vascular organs resembling glomeruli.70,71 Earlier studies suggested that blood vessels penetrate the nucleus pulposus in human fetuses and neonates.72 However, elegant studies by Whalen and colleagues71 demonstrated that the nucleus pulposus is always avascular. Coventry and colleagues73 demonstrated that, after birth, the cartilage endplates become progressively thinner and the vessels within the cartilage canals become obliterated. Some persist up to age 30 years, but by adulthood most of the vessels within the endplate itself have disappeared.73
Wiley and Trueta74 demonstrated the rich arterial anastomosis within the vertebral body, with end arterioles in the metaphyseal region. Spinal arteries enter the canal through the intervertebral foramen at the level of the disc. Branches ascend and descend, supplying the vertebral bodies above and below. Through their injection studies, Wiley and Trueta demonstrated how bacteria could easily spread hematogenously to the metaphyseal region of adjacent vertebrae. The infection may also start in the metaphyseal region of one vertebra and either spread across the avascular disc by lysosomal destruction of the nucleus pulposus or through vessels anastomosing on the periphery of the annulus fibrosus.74
It has been suggested that Batson’s plexus may be the route of hematogenous spread of infection. Batson demonstrated, in injection studies, that dye flows into the valveless vertebral venous plexus when pressure is applied to the lower abdominal wall.75 The distribution of veins within the vertebral body is an arborization of vessels. Minute tributaries draining the metaphyseal region empty into large, valveless, venous channels that drain into the loose plexus lining the canal. Wiley and Trueta demonstrated that it takes considerable force to fill the small metaphyseal vessels in a retrograde fashion, compared with the ease of injection of the metaphyseal arterioles; this suggests that the former is an unlikely route of hematogenous seeding.74
Once microorganisms lodge in the low-flow vascular arcades in the metaphysis, infection spreads. The disc is destroyed by bacterial enzymes in a manner similar to the destruction of cartilage in septic arthritis. This is in contrast to tuberculous infections (described later), in which the endplates and bone are destroyed but the disc is frequently better preserved.76 In children, the cartilage canals allow microorganisms nearly direct access to the disc, which probably explains the clinical differences between spine infections in children and adults. In adults, disc space infection may occur by direct inoculation of the disc as a result of surgery, chemonucleolysis, or discography but is unlikely to occur spontaneously.77,78
Some authors have suggested that discitis in adults is a separate entity from vertebral osteomyelitis.26,79 Ghormley and colleagues26,79 stressed the benign nature of this variation, but in Kemp and colleagues’26 series the disease was quite severe with a high rate of irreversible paralysis. It is conceivable that adult discs could receive blood directly through persistent vascular channels in the endplate, degenerative defects in the endplate, or vessels anastomosing on the peripheral annulus fibrosus and perhaps gaining access through rents in the annulus. If adult discitis occurs at all, it appears that hematogenous involvement of the metaphysis is far and away the most common mechanism and, whether the infection begins in the metaphysis and spreads across the disc or vice versa, the clinical manifestations and treatment are the same.
The upper cervical spine has a peculiar blood supply. Parke and colleagues80 have demonstrated a venous plexus around the odontoid, called the “pharyngeal vertebral vein,” which frequently has lymphovenous anastomoses. This venous plexus may be responsible for hematogenous spread to the upper cervical spine.80,81 Abscesses may drain into the soft tissues surrounding the spine or into the spinal canal itself. In the cervical spine, a retropharyngeal abscess may invade the mediastinum.27,82 In the thoracic spine, an abscess may be paraspinous or retromediastinal.27 Infection in the lumbar spine may cause a psoas abscess or, less commonly, an abscess pointing through Petit triangle.27 Occasionally, an abscess may create a tract through the greater sciatic foramen and appear in the buttock beneath the piriformis fascia, in the perirectal region, or even in the popliteal fossa.27 The more virulent organisms may not follow fascial planes and may extend into visceral structures. They also are more likely to produce spinal deformity. An abscess that enters the spinal canal is considered to be an epidural abscess and is discussed later. Infection may cross the dura, causing a subdural or intradural abscess or meningitis.27,83
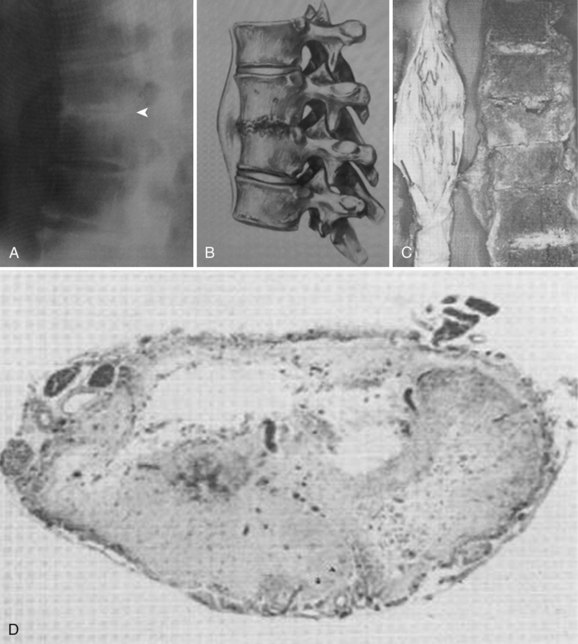
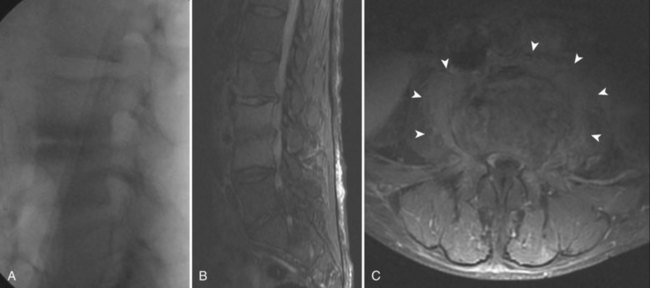
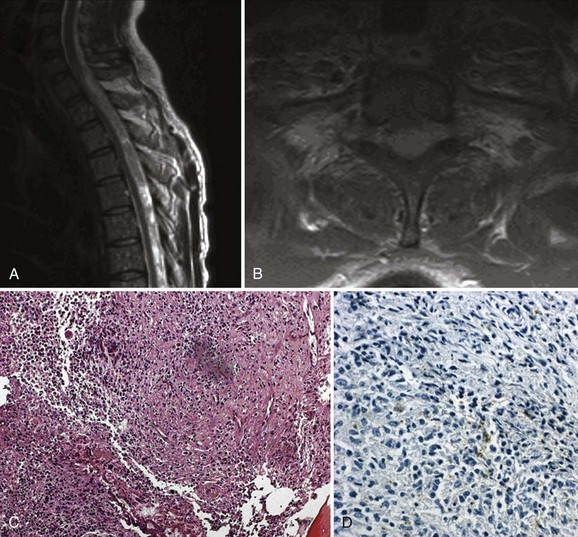
The pathogenesis of neural compromise may be related to direct compression by epidural pus, granulation tissue, or bone and disc from the development of spinal deformity and instability. In addition, the cord or nerve roots may suffer ischemic damage from septic thrombosis or may be damaged by inflammatory infiltration of the dura (Figs. 86-1 and 86-2).26,27,29
An unusual association between vertebral osteomyelitis and compression fractures secondary to osteoporosis has been described. It is theorized that the osteomyelitis may develop as a complication of the fracture because the fracture creates a favorable environment for the hematogenous infection. Alternatively, the osteomyelitis may develop within the central portion of an osteoporotic vertebral body, perhaps because the bone is more hyperemic or because of vascular stasis. Infection may then lead to a pathologic fracture of the vertebra without the usual involvement of the disc space.84
Clinical Presentation
The clinical manifestations of spine infection are determined by the virulence of the organism and the resistance of the host. The presentation may be acute, subacute, or chronic.26,27 Before the antibiotic era, most patients had acute osteomyelitis, and in 68% of the cases the disease was fulminant with severe toxemia.53 The mortality rate ranged from 25% to 71%.27,53 A literature review in 1979 found that only 20% of the patients had symptoms for less than 3 weeks before presentation, 30% had them for 3 weeks to 3 months, and 50% had them for longer than 3 months.29 Greater awareness of the disease and improved diagnostic modalities (especially magnetic resonance imaging [MRI]) have shortened the delay in diagnosis. In one series reported in 1997, 68 of 111 patients were diagnosed within 28 days of the onset of their symptoms and only 8 patients were diagnosed more than 3 months after their symptoms began.22 In an urban setting, the infection is discovered within 1 month in only 28% and the median time to diagnosis is 1.8 months.52
Fever is present in only 52% of the patients overall; pain in the back or neck is a much more common finding, occurring in approximately 90% of patients.29 Patients with acute infection present with fever, local spine pain, severe muscle spasm, and limitation of motion of the spine. With lumbar spine involvement, there may be a positive straight-leg raise test, reluctance to bear weight, and hip flexion contracture due to psoas irritation. Hamstring tightness and loss of lumbar lordosis may be noted. Torticollis and fever may be the only presenting signs with cervical osteomyelitis.81,85
Subacute and chronic infections may be much more insidious, and these patients have a vague history. Pain may be the only symptom, especially with an occult infection by a low-virulence organism.68 Approximately 15% of the patients have atypical symptoms such as chest pain, abdominal pain, hip pain, radicular symptoms, or meningeal irritation.16,29,86 These unusual and often vague complaints have led to unnecessary exploratory laparotomies before the diagnosis has been made.29,86 A significant delay in diagnosis is common with chronic infections.16,21,23–25,29,87,88
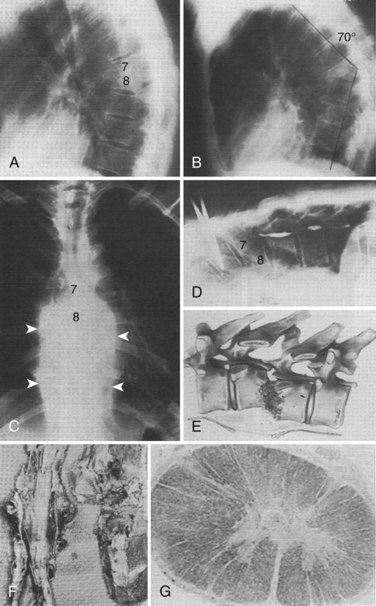
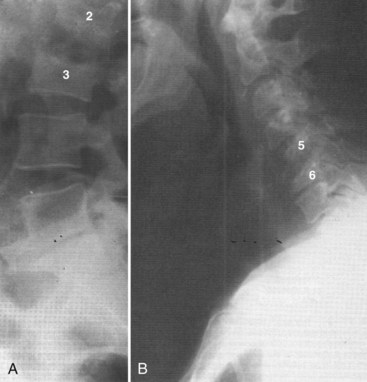
Vertebral osteomyelitis is more common in the lumbar region. In Sapico and Montgomerie’s29 literature review, in 48% of 294 cases the involvement was lumbar, in 35% thoracic, in 6.5% cervical, and in approximately 5% thoracolumbar and lumbosacral. Vertebral osteomyelitis at noncontiguous levels is uncommon (Fig. 86–3). With the advent of antibiotics, significant spine deformity is not as common as it was in the past, but significant kyphosis still may occur.24,27
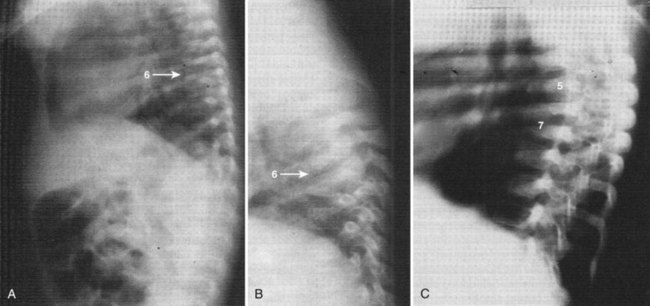
Abscesses are not encountered as frequently now as they were before the antibiotic era but should still be sought, in the paraspinous region, psoas region, and in remote areas.27 A tender or pulsatile abdominal mass may be caused by a mycotic aneurysm, a dilatation of the wall of an artery resulting from an infection.89 In the lumbar spine, abscesses in the psoas muscle are common and help to distinguish spinal infections from other lesions such as tumors or trauma (Fig. 86–4).
Approximately 17% of the patients present with a neurologic deficit secondary to nerve root or spinal cord involvement.29 Eismont and colleagues identified several factors that predisposed patients to paralysis including diabetes,16,27,50,90 rheumatoid arthritis,90 increased age,90,91 and a more cephalad level of infection.37,90 Patients on systemic steroid therapy are more likely to be paralyzed, and those infected with S. aureus seem to have the most severe degree of paralysis.90 Some authors have noted that neurologic involvement is uncommon in patients infected with Pseudomonas.58,60
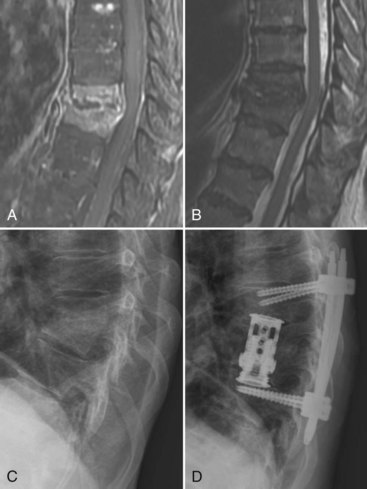
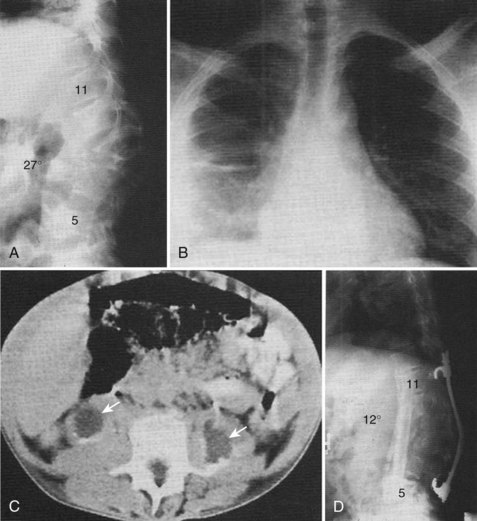
Infants and IV drug abusers are two subsets of patients who have slightly different presentations. Infants generally present acutely with high temperature, septicemia, and generalized signs of systemic illness.91,92 The radiographic findings of vertebral osteomyelitis in infants is striking, with almost complete dissolution of the involved vertebral bodies and nearly normal adjacent endplates. The late radiographic appearance may be identical to that of congenital kyphosis (Fig. 86–5). Heroin abusers also present earlier than most patients. In a review of the literature, 81% of heroin abusers presented within 3 months after the onset of their symptoms, compared with 50% in the general population with vertebral osteomyelitis.29,38,91,92 The authors postulated that the earlier presentation may be related to infection with more virulent organisms or the fact that their patients have less tolerance to pain or may be using their back pain as an excuse to receive more narcotics (Fig. 86–6).38
Diagnostic Evaluation
Laboratory Evaluation
The erythrocyte sedimentation rate (ESR) and Gram stain and culture are commonly used laboratory tests in the diagnosis of pyogenic spine infections.23,29,31,77 The leukocyte count is increased on presentation in only 42% of cases and is usually normal in patients with chronic disease.29,31,77 Conversely, the sedimentation rate was increased in 92% of 184 patients reported in the literature.29 It is a nonspecific test, however, and the rate may be increased in pregnancy, malignancy, other infections, dysproteinemias, and connective tissue diseases. In addition, it is influenced by serum levels of fibrinogen and globulin.29 The sedimentation rate may be normal in occult infections with low-virulence organisms.68
C-reactive protein (CRP) has been shown to be helpful in the diagnosis of postoperative discitis 93 and has supplanted ESR as the laboratory study of choice for assessing the presence of infection. CRP was discovered in 1930 by Tillett and Francis in their studies of pneumonia. This acute phase protein is a 187 amino peptide that can precipitate the C-fraction polysaccharide from Streptococcus pneumonia.94 With the onset of an infection, or other inflammatory process, the CRP level increases within 4 to 6 hours, doubling every 8 hours, and peaking at about 36 to 50 hours.94 The half-life of CRP is 24 to 48 hours. The degree of increase can be up to 10,000-fold higher than normal, while ESR increases only 10- to 100-fold.95 The ESR begins to increase only several days after onset of infection and peaks at 7 to 8 days.94 An additional limitation of the ESR is the long period of recovery. The ESR has been useful in follow-up to assess the response to treatment.15,23,24,26,29,96,97 In one small series, the sedimentation rate decreased to at least two thirds of the original value at the completion of successful antibiotic therapy in all patients and decreased to half of the original value in the majority.29 In another series of 30 cases, the sedimentation rate returned to normal after resolution of the infection.23 However, the ESR remains elevated for more than 3 weeks postinfection.98 The CRP, in contrast, decreases more rapidly and returns to normal levels in 10 days. In cardiac patients, elevated preoperative CRP increases the risk of postoperative infectious complications.99 Similar to ESR, the CRP unfortunately suffers from low specificity because any infectious or inflammatory process will elevate these values.100 After routine spinal surgery, the CRP returns to normal in 5 to 14 days, whereas the ESR takes 21 to 42 days to return to normal.101 Thus an abnormal increase in CRP 1 to 2 weeks after spinal surgery may represent onset of postoperative infection. In all cases, a blood culture should be obtained because it remains a convenient, readily accessible means of identifying an organism. In most cases the identification of the offending organism correlates well with biopsy results. In a study of 29 cases of pyogenic spondylitis, O’Daly and colleagues102 found a 100% correlation between blood cultures and vertebral cultures when both were positive.
Imaging Studies
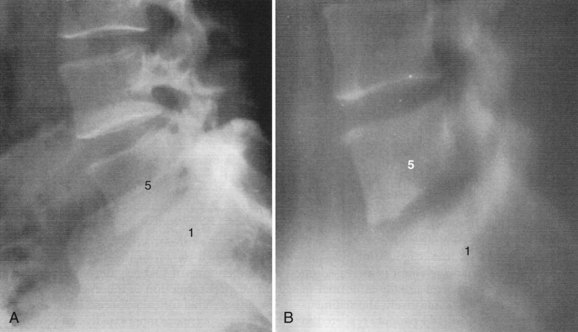
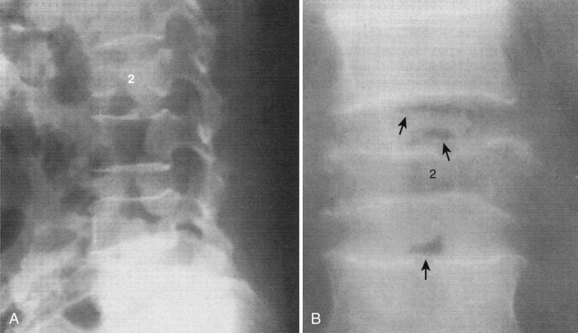
The findings on plain radiographs are characteristic but do not appear for at least 2 to 4 weeks.23,28,30,31,56,76 The earliest and most constant radiographic finding, narrowing of the disc space, is present in 74% of patients at presentation.29 Tomograms show abnormalities earlier than plain radiographs (Fig. 86–7) and may show local osteopenia of the endplates at 10 to 14 days, but tomography has largely been supplanted by computed tomography (CT).31 Widening of the retropharyngeal space in the cervical spine, enlargement of the paravertebral shadow in the thoracic spine, or changes in the psoas shadow in the lumbar spine may indicate either abscess or granulation tissue surrounding the infection. After 3 to 6 weeks, destructive changes in the body can be noted, usually beginning as a lytic area in the anterior aspect of the body adjacent to the disc and diffusely in the endplate.
Reactive bone formation and sclerosis are present in 11% of patients on presentation, and most patients will have sclerosis when the disease heals.29 Depending on the virulence of the organism and the response to treatment, progressive bony destruction, collapse, and kyphosis may develop. The radiographic findings generally lag behind the clinical response by 1 to 2 months. With healing, new bone formation and hypertrophic changes at the vertebral margins eventually may produce spontaneous fusion. Fusion occurs in just over 50% of the cases29,103 but may take up to 5 years.104 If a solid fusion does not occur, a fibrous ankylosis may be achieved.24,103
Although the radiographic findings are characteristic, they are not specific and a definite diagnosis is possible only by biopsy.103 An unusual radiographic finding that may help with the diagnosis is gas in the disc space; this may represent infection with a gas-forming organism (Fig. 86–8).65 However, the most common cause of gas in the disc space in adults is due to degenerative disease.
An atypical presentation of vertebral osteomyelitis was reported by McHenry and colleagues.84 They described a series of six patients with osteomyelitis in an osteoporotic vertebral compression fracture. The vertebral endplates were intact on the initial plain radiographs.84 This presentation occurred in 13% of all hospitalized patients with vertebral osteomyelitis and 2.4% of inpatients with osteoporotic compression fractures at one institution over a 5-year period.105 Chest radiographs may reveal atelectasis, pleural effusion, and soft tissue masses that may be confused with a tumor.87
Radionuclide studies are useful for early detection and localization of infection, before plain films become positive.24,26,30,88,97,106–108 Clinical studies have suggested that gallium scans become positive before technetium scans do,106 and this has been confirmed in experimental studies.109 Technetium scans show increased uptake diffusely in the region of the infection, whereas gallium scans may show increased uptake in a butterfly area around the infected spine.110 Gallium scanning has been found to have a sensitivity of 89%, a specificity of 85%, and an accuracy of 86% in the diagnosis of disc space infections.106 In a separate study,107 technetium scans were found to have a sensitivity of 90%, a specificity of 78%, and an accuracy of 86%. The accuracy of combined technetium and gallium scans was 94%.107 These two scans combined are currently the authors’ preferred nuclear medicine studies.
In experimental disc space infection, bone scans were positive in 23% at 3 to 5 days, in 29% at 6 to 8 days, and in 71% at 13 to 15 days.111 The probability of technetium bone scans becoming abnormal increases with the duration of symptoms, to almost 100%, but false-negative scans have been reported in young children and also in the elderly. This has been postulated to be the result of regional ischemia.68
The major mechanism of gallium localization is thought to be neutrophil labeling followed by migration to the inflammatory focus. False-negative gallium scans have been reported in leukopenic patients.108 Both technetium and gallium scans may be negative with occult infection by low-virulence organisms.68 Two cases have been reported in which the technetium scan was negative but the gallium scan was positive, and the authors postulated that this represented pyogenic discitis without vertebral osteomyelitis.112 Technetium scans remain positive for a long time after resolution of the disease, whereas gallium scans become normal during healing and, therefore, may be useful in following the response to treatment.113
Indium-111-labeled leukocyte imaging has been found to be helpful in the evaluation of sepsis in the appendicular skeleton.114 Unfortunately, it is not sensitive in the spine.115–117 This may be related to the fact that most cases of vertebral osteomyelitis are chronic by the time the patients are studied, and the inflammatory response may have fewer leukocytes. The overall sensitivity of indium scanning for infections of the spine is 17%, the specificity is 100%, and the accuracy is only 31%.116 A correlation was found between prior antibiotic therapy and false-negative indium scans and photon-deficient indium uptake.116 Photon-deficient lesions may be detected by indium-111-labeled leukocyte imaging in many other conditions including previous surgery, radiation therapy, or metastatic disease.118 Palestro and colleagues119 reported that the specificity was 52% and the sensitivity was 54% when decreased activity was the criteria for osteomyelitis with indium-111 scanning. Single-photon emission computed tomography (SPECT) is a sensitive bone scintigraphic modality for early detection of spondylitis. It is more sensitive than planar scintigraphy and has the advantage of increased contrast resolution and the capability of three-dimensional localization.120 Scintigraphy with technetium and gallium are now often performed with SPECT. Love and colleagues121 compared three-phase bone technetium SPECT, with gallium SPECT, and MRI in 11 patients with spinal infections. Gallium SPECT and MRI were comparable in accuracy and superior to technetium SPECT. Thus gallium SPECT may be useful in patients in whom MRI is contraindicated or in cases where the diagnosis is uncertain. A positive technetium SPECT, in the setting of a negative gallium scan, points toward noninfectious cases of back pain such as degeneration disease or pseudarthrosis.122
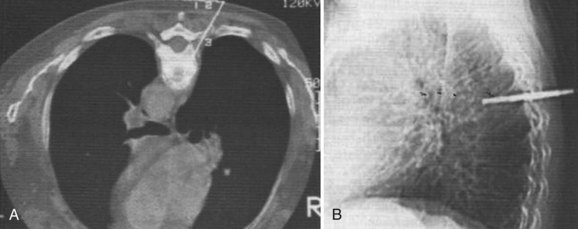
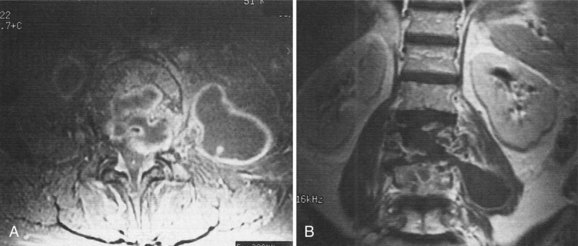
CT may show cystic changes in the bone, as well as soft tissue masses, gas in the soft tissues or within the bone and disc, and, later, lytic destruction of the body.123–125 The prevertebral soft tissue involvement seen on CT usually completely surrounds the spine anteriorly, and the destruction of the vertebra is generally an osteolytic process around the disc space (see Fig. 86–6). This is in contrast to neoplasms, which are characterized by no or only partial paravertebral soft tissue swelling and by changes that may be osteoblastic and more likely to involve the posterior elements than in infection.126
CT is valuable in differentiating pyogenic spondylitis from a tuberculous or fungal infection; in the latter, the soft tissue components tend to be more prominent.127 The finding of disc hypodensity on CT is relatively specific for infection in the lumbar spine but is less useful in the thoracic and cervical region.125 A relatively unique feature of tuberculous infection is vertebral fragmentation and paraspinal calcifications.128,129 The destruction tends to extend into the pedicle, which is uncommon in pyogenic infections. CT with contrast medium is helpful to delineate the boundary between abscesses and swollen paravertebral muscles.123–125 CT after intrathecal administration of metrizamide provides exquisite detail for the spinal canal.127 CT-guided biopsies of the spine have been shown to be safe and can be done at all levels of the spine (Fig. 86–9).123,130–132 Myelography and postmyelography CT are indicated in cases of neurologic deficit and radicular pain to rule out epidural and subdural abscesses. Cerebrospinal fluid (CSF) should also be examined to rule out meningitis.83
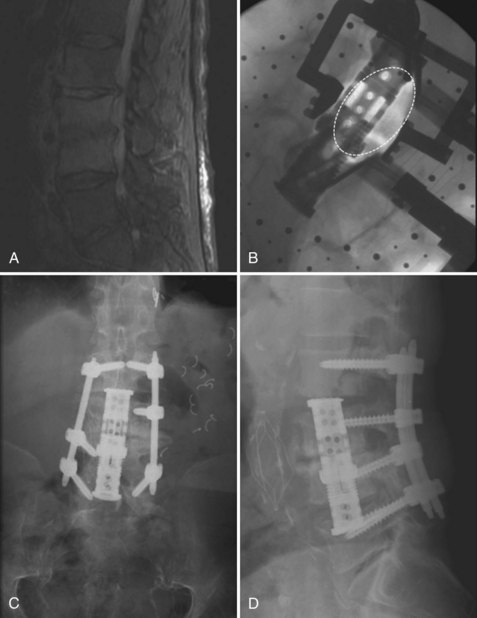
The imaging modality of choice for the evaluation of spine infections is MRI. MRI permits early diagnosis of infection and recognition of paravertebral or intraspinal abscesses without the risk associated with myelography.133,134 In a prospective study of 37 patients suspected clinically of having vertebral osteomyelitis, MRI was found to be at least as accurate and as sensitive as gallium and bone scanning combined: MRI had a sensitivity of 96%, a specificity of 93%, and an accuracy of 94%.107 MRI has the advantage of providing more anatomic information than radionuclide studies and is capable of differentiating degenerative and neoplastic disease from vertebral osteomyelitis.135 The changes on MRI occur at about the same time as the changes on gallium scans.107
Disadvantages of MRI are that it is more sensitive to motion degradation, and there are problems with patient positioning and claustrophobia. MRI has a limited field of view, whereas radionuclide scans can image the entire skeleton. MRI may be falsely negative in cases of epidural abscess without involvement of the adjacent bone because the signal intensity of the inflammatory exudate is similar to that of CSF.107,136
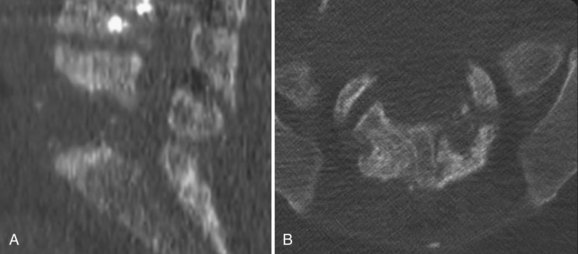
The MRI changes in vertebral osteomyelitis are characteristic (Fig. 86–10). On T1-weighted sequences, there is a confluent decreased signal intensity of the vertebral bodies and adjacent disc, making the margin between the two structures indistinct. On T2-weighted sequences, the signal intensity of the vertebral bodies and the involved disc is higher than normal, and there is generally an absence of the intranuclear cleft normally seen within the adult disc.107,133 The extent of the infection is best seen, however, using gadolinium contrast enhancement. The disc and the involved portions of the vertebral bodies reveal a marked increased signal intensity that delineates the margins of the infection (see Fig. 86–10C).137 The typical T1 changes in the vertebral body and endplates and the T2 changes in the disc space were seen in 95% of the 37 cases of vertebral osteomyelitis described by Dagirmanjian and colleagues.138 Only 56% of their cases had typical T2 vertebral body changes. Isointense or decreased signal in the vertebral body on T2-weighted images is consistent with infection if the other typical findings are present. In a more recent study by Ledermann and colleagues,139 46 patients with culture or histologic-positive spinal infections were systematically evaluated with gadolinium-enhanced MR imaging. The most sensitive MRI criteria was the presence of paraspinal or epidural inflammation (97.7% sensitivity), followed by disc enhancement (95.4% sensitivity). Hyperintensity or fluid-equivalent disc signal intensity on T2-weighted MRI was 93.2% sensitive, erosion or destruction of at least one vertebral endplate was 84.1% sensitive, and effacement of the nuclear cleft was 83.3% sensitive. When the infection is confined to a single vertebral body, spread of infection occurs in a subligamentous path.140 Interestingly, the spread of infection tends to be more commonly in a cephalad direction, affecting the superior disc space more commonly than the inferior disc space. The cause of the signal intensity changes seen in vertebral osteomyelitis is uncertain but is thought to parallel the pathogenesis of the disease. The earliest changes are thought to be related to ischemia and the increased water content of the inflammatory process. As the infection crosses the endplate, a confluent signal intensity occurs on MRI. The normal finding of an intranuclear cleft within adult discs is thought to be related to fibrous tissue within the nucleus pulposus. This cleft is lost at the time of inflammatory involvement of the disc.107
In an elegant study comparing MRI findings of pyogenic vertebral osteomyelitis with tuberculous osteomyelitis, Chang and colleagues141 identified five key distinguishing features that help to differentiate between the two disease entities. A retrospective study of 33 patients with confirmed tuberculous spondylitis were compared with 33 randomly selected patients with known pyogenic osteomyelitis. The key distinguishing features were (1) degree of bone destruction; (2) degree of disc preservation; (3) paraspinal abscess appearance; (4) abscess with postcontrast rim enhancement; and (5) postcontrast enhancement pattern of the vertebral body. As expected, the degree of vertebral body and disc destruction were the two most distinguishing differences found. Most patients in the tuberculous (TB) group (82%) had near complete destruction of at least one vertebral body, whereas less than one third (30%) in the pyogenic group had severe vertebral body destruction. Conversely, the disc was preserved in more than one half (57%) of TB group, whereas only 3% of the pyogenic group had a preserved disc space. Thus the credo that TB spondylitis “skips the disc space” is relatively well supported. However, a more accurate distinguishing feature would be better stated that pyogenic vertebral osteomyelitis differs from TB spondylitis by severe disc space destruction with relative preservation of the vertebral body.
Chang and colleagues went to further show that there were marked differences in the imaging pattern of the vertebral body itself.141 In the TB group, the enhancement pattern of the vertebral body was always focal and heterogeneous, with rim-enhancing abscesses. In contrast, the enhancement pattern of the vertebral body in the pyogenic group was nearly always (94%) diffuse and homogeneous. A discreet rim enhancement intraosseous abscess was never observed in the pyogenic group. The paraspinal soft tissue imaging patterns provide further distinguishing features. In the TB group, the paraspinal soft tissues revealed well-defined rim-enhancing lesions. In contrast, the pyogenic infections tended to show more diffuse, ill-defined areas of enhancement.
In a comparison of MRI, bone scans, and plain radiographic evaluations in an animal model of disc space infection, MRI was found to have a sensitivity of 93%, a specificity of 97%, and an accuracy of 95%, corresponding well to results of clinical studies in humans.107,111 The findings are time related. In one study, scans of rabbits made 3 to 5 days after injection of bacteria all showed a decreased signal from the nucleus pulposus on both T1-weighted and STIR (short T1-inversion recovery) sequences. Scans at 6 to 8 days also showed increased signal from the adjacent endplates on the STIR sequence and blurring of the disc margins on the T1 image. Scans at 13 to 18 days showed more florid endplate changes, and in several scans at 21 days there was increased signal from the vertebral endplates and the disc on STIR sequences.111 The MRI findings slowly return to normal after successful treatment of vertebral osteomyelitis.107 Gallium scans revert to normal much more rapidly and are better indications of appropriate therapy. Post and colleagues137 noted that abnormal gadolinium enhancement of the disc, vertebral bodies, and paraspinal soft tissues progressively decreases with successful treatment of the infection. Gillams and colleagues142,143 described some patients who were improving clinically and had stable or increasing enhancement patterns and concluded that such findings should not be interpreted as treatment failure.
Unfortunately, even MRI may be negative in surgically documented occult infections by low-virulence organisms.68 Despite the accuracy of MRI, an absolute diagnosis must be based on bacteriologic or microscopic examination of the tissue.27,144,145 The only situation in which the diagnosis can be made without a tissue biopsy is when a positive blood culture is obtained from a patient with signs and symptoms of spondylitis. Blood cultures are positive in 24% to 59% of patients with pyogenic spine infections.22,29 Urine cultures are less reliable because patients with vertebral osteomyelitis may have a coexistent urinary tract infection with a different organism.22,24
Biopsy
Needle biopsy of the spine was first reported by Ball in 1934. In 1956 Craig described a set of instruments designed to increase the percentage of successful closed-needle biopsies, especially in sclerotic or softened bone, discs, or fibrous tissue.146 Needle biopsies have been shown to be safe in the cervical and thoracic spine, as well as in the lumbar spine.147,148 A definite diagnosis is possible by closed-needle biopsy in 68% to 86% of cases.29,31,132,148,149 CT-guided closed biopsy of the spine should provide a margin of safety and allow biopsy of the area most likely to yield the diagnosis. In a series of 22 patients with a mass or destructive lesion who underwent this procedure, 17 biopsies provided a definite diagnosis; only one was false negative and in four cases the specimens were insufficient. All areas of the spine were sampled including one lesion at C2. The patient with the C2 lesion had a transient increase in quadriparesis but returned to baseline, and no other complications were reported.130
Closed biopsies of the spine are often false negative in patients who are being treated with antibiotics at the time of the biopsy. If a biopsy is nondiagnostic, it would be reasonable to observe the patient off the antibiotic regimen and repeat the biopsy if the clinical situation allows such a delay. If the second closed biopsy is also nondiagnostic, an open biopsy should be considered. This will provide larger tissue samples and selection of grossly pathologic tissue and should have a lower false-negative rate. In their review of the literature, Sapico and Montgomerie29 found that 30% of needle biopsy specimens and aspirates were sterile, compared with only 14% of surgical specimens. The technique of transpedicular biopsy allows for larger bony samples to be obtained. The transpedicular approach is safely performed with either fluoroscopy or CT. For general biopsies including tumor, the accuracy rate is over 92%.150–152 In the setting of infection, this technique yields better results than traditional needle biopsy. Hadjipavlou and colleagues153 examined 28 patients with suspected spinal infections diagnosed by a combination of laboratory test, MRI, and scintigraphy. Positive cultures were obtained in 71% of the biopsies.153
The differential diagnosis of pyogenic vertebral osteomyelitis includes tuberculosis, fungal infections, metastatic carcinoma, multiple myeloma, localized Scheuermann disease, trauma, degenerative disease, epidural abscess, and fractures associated with osteoporosis.15,29,84,154 Less common disorders in the differential diagnosis are leukemia, perinephric abscess, neuropathic spinal arthropathy, and sarcoidosis, as well as erosive arthritides in rare cases of facet joint involvement.28,77,92,155–157 With such a wide variety of diseases that can present with signs and symptoms similar to those of vertebral osteomyelitis, diagnostic acuity is important. As Kulowski said in 1936, “Knowledge of the disease is the primary factor in the diagnosis.”27
Management
Before the advent of antibiotic therapy, treatment of pyogenic vertebral osteomyelitis involved drainage of abscesses, rest on a frame or plaster bed, and attention to nutrition and general hygiene. The mortality rate with this approach was between 25% and 70%.27,53 The use of antibiotics has drastically changed the prognosis with this disease, but attention to good general medical care is still a vital part of the treatment. Associated conditions that compromise wound healing or immune response should be managed aggressively. Attention to proper nutrition and the reversal of metabolic deficits and hypoxia are essential. Diabetes and other systemic illnesses should be brought under control.90 Any underlying focus of infection in the urinary tract, lungs, skin, or elsewhere must be treated concurrently with the spine infection.158
Daly and colleagues159,160 have demonstrated that antibiotic penetration of osteomyelitic bone parallels serum concentrations for all classes of antibiotics. The penetration of antibiotics into inflammatory exudates and the intervertebral disc is less certain.161–166 Vancomycin, gentamycin, tobramycin, clindamycin, and teicoplanin all penetrate the nucleus pulposus reasonably well.161,167 The data regarding cephalosporins are inconclusive, but if penetration does occur, it appears to be at a relatively low level.162,165,166 The penetration of cephalosporins into inflammatory exudates appears to be inversely proportional to the degree of serum protein binding.163 Riley and colleagues168 have shown that the penetration and distribution of antibiotics into the nucleus pulposus is significantly influenced by the charge of the antibiotic with positively charged molecules penetrating the best.
The route of administration of the antibiotics and the duration of therapy are somewhat empiric because little research has been done to clarify these topics. At present, it is recommended that parenteral antibiotic therapy be used in maximal dosage for 6 weeks and followed with an oral course of antibiotics until resolution of the disease. It may be reasonable to switch from parenteral to oral therapy at 4 weeks.24 Parenteral therapy for less than 4 weeks results in a higher rate of failure.29 Oral ciprofloxacin therapy has been used successfully in the management of patients with chronic osteomyelitis of the tibia or femur.169 It is possible that ciprofloxacin and other new agents for oral use may supplant parenteral treatment of vertebral osteomyelitis in the future, but general use of these agents should await evidence of their effectiveness.
The erythrocyte sedimentation rate has been found to be a reasonable guide to the response to therapy15,23,24,26,29,96,97 and can be expected to decrease to half to two thirds of pretherapy levels by the completion of successful treatment.29 If the sedimentation rate does not decrease with treatment, consideration should be given to a repeat biopsy. CRP is a more useful laboratory test to follow resolution of the infection, as described earlier. However, it is still unclear at what point to discontinue antibiotics on the basis of CRP levels. Further studies are necessary to correlate CRP levels with the duration of antibiotic treatment. Currently, at least 6 weeks of parenteral antibiotics is used empirically. Antibiotic administration must be carefully monitored to avoid toxicity, especially in diabetics and other who might have impaired renal function.50
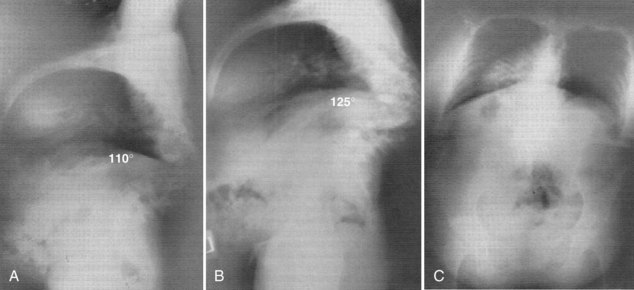
Patients should be immobilized for pain control and prevention of deformity or neurologic deterioration. The length of time a patient should remain at bed rest, the type of orthosis, and the duration of its use all depend on the location of the infection in the spine, the degree of bone destruction and deformity, and the response to treatment. Thoracic and thoracolumbar lesions may require bed rest on a RotoRest or similar device if there is undue pain. Rigid bracing with a thoracolumbosacral orthosis (TLSO) suffices in most cases to allow mobilization of the patient. Thoracic and thoracolumbar lesions are more likely to cause deformity and, if neurologic deficits occur, the prognosis is worse with these lesions than with lumbar spine involvement.24,90
Cervical and cervicothoracic lesions may be immobilized with a halo device if there is significant instability or deformity. In most cases external bracing is sufficient, and often better tolerated by the patient. Upper thoracic lesions are best immobilized in a TLSO device with a chin piece, and lower thoracic and lumbar lesions should be immobilized in a TLSO device without a chin piece. Frederickson and colleagues24 found that immobilization was most important in those patients with destruction of greater than 50% of a vertebra and recommended immobilization for the first 3 months. In 5 of their 17 cases, significant deformity developed in the first 6 to 8 weeks, all at the thoracolumbar junction or above; those patients with the greatest deformity had 50% or more vertebral body destruction at presentation.106 Most authors recommend bracing for at least 3 to 4 months. Garcia and Grantham31 recommended that the duration of immobilization should be individualized and based on the response to treatment.
Surgical Treatment
Surgery is indicated in the following circumstances: (1) to obtain a bacteriologic diagnosis when closed biopsy is negative or deemed unsafe; (2) when a clinically significant abscess is present (spiking temperatures and septic course); (3) in cases refractory to prolonged nonoperative treatment, where the ESR and/or CRP remain high or pain persists; (4) in cases with spinal cord compression causing a neurologic deficit; and (5) in cases with significant deformity or with significant vertebral body destruction, especially in the cervical spine.90,170,171 Upper cervical osteomyelitis is rare but generally requires fusion because of the associated instability.81
In cases of lumbar lesions with root deficits, the final outcome is satisfactory with or without surgical treatment, but patients with spinal cord compression have a better prognosis with surgery.90 Surgery should be carried out as soon as possible in these cases, but when doubt exists regarding the chances of a reversible spinal cord lesion, decompression should be carried out because recovery has been noted in patients with paralysis who underwent decompression as late as 5 months after the onset of weakness.90
In most cases the spine should be approached anteriorly because this allows direct access to the infected tissues and adequate débridement. Anterior exposure allows stabilization of the spine by bone grafting, which promotes rapid healing without collapse and assists rehabilitation (Fig. 86–11).90,172–176 Laminectomy without anterior débridement and reconstruction is contraindicated in most cases because it may lead to neurologic deterioration and increased instability.90,173,177 The situation is similar to that in acute trauma.178 Laminectomy may be performed in the lumbar spine below the level of the conus, provided there is no psoas abscess or extensive anterior destruction of the bodies that would require débridement.
Anterior approaches to the spine have been described elsewhere174,179 and are reviewed in Chapters 17, 18, and 19. For lesions in the thoracic or thoracolumbar spine, the transthoracic approach has the advantage of better exposure, allowing more extensive débridement and better decompression of the cord and more effective bone grafting.172,176,180,181 The disadvantage is the potential increased morbidity after a thoracotomy in the presence of a purulent infection. After débridement of the infected focus, anterior strut grafting can be performed during the same procedure. The graft should extend from healthy bone above to healthy bone below.172,176,180,181 Autogenous bone grafting after vertebral body resection in the presence of active infection was first reported by Wiltberger in 1952 and has since been demonstrated to be safe and effective regardless of the causative organism.30,182 Grafting with iliac crest is generally better than grafting with rib.172,175,183 If a good-quality rib is excised in the process of a transthoracic approach, however, it is often adequate as long as a large segment does not need to be spanned and there is no significant kyphotic deformity.183 Revascularization of a cortical graft may not be complete even after 1 year.184 Vascularized rib grafts have been used with good success for the stabilization of kyphosis.185 Louw has reported successful fusions in 95% of cases at 6 months and 100% at 1 year when vascularized rib grafts were used for TB kyphosis.186 Fibular grafts have been shown to be effective for reconstruction of multiple-level anterior decompressions of the cervical spine187; however, the large amount of cortical bone in fibular grafts makes them less ideal in the presence of infection. In cases with significant kyphotic deformity, anterior reconstruction with autogenous bone grafts after débridement should be carried out as a first stage.172,176,183 Posterior stabilization and fusion can be performed in a second-stage procedure if necessary (see Fig. 86–11D).172,173,183,184,188 Posterior instrumentation has been shown to be safe and effective after anterior débridement and fusion.22,189 The use of titanium mesh cages may provide better anterior column support because their structural integrity is not affected by degradative enzymes present in an infected environment.190 The addition of posterior instrumentation provides even better deformity correction and faster rates of fusion.190 The addition of posterior instrumentation does not appear to increase the risk of infection.191 The anterior and posterior surgeries can be performed on the same day with good results. Safran and colleagues192 reported on 10 consecutive patients with lumbar osteomyelitis treated with same day anterior decompression and strut fusion with posterior instrumented fusion. All 10 patients achieved solid fusion with eradication of infection. Single-stage anterior and posterior surgery has been shown to be safe and effective using titanium implants. Interestingly, bacteria have a lower propensity to adhere to titanium compared with stainless steel.193,194–197 Kuklo and colleagues198 retrospectively reviewed 21 consecutive patients with pyogenic vertebral osteomyelitis treated with anterior and posterior surgery on a single day with titanium mesh cages. Most patients (16 of 21) had a significant reduction of pain. Radiographically, they averaged 12 degrees of improvement in segmental kyphosis (preoperatively 11.5 degrees to 0.8 degrees postoperatively) with an average of 2.2-mm cage settling (range, 0 to 5 mm) on latest follow-up. There were no instrumentation failures, signs of chronic infection, or rejection, but two patients required a second surgery during the same admission for persistent wound drainage at the posterior wound. Both patients were successfully treated with irrigation and débridement. These findings are supported by previous studies showing the safety and efficacy of single-stage surgical débridement and reconstruction.192,199,200
In the past, cervical spine vertebral osteomyelitis was managed effectively without bone grafting by drainage, antibiotics, and skull traction for 6 to 12 weeks.37 Prolonged hospitalization can be avoided by débridement, bone grafting, halo immobilization, and outpatient antibiotics. Posterior stabilization performed as a second stage may be reasonable in order to avoid a halo. Today, most cervical spine infections refractory to nonoperative treatment are treated with anterior plate fixation at the time of débridement and strut grafting.201
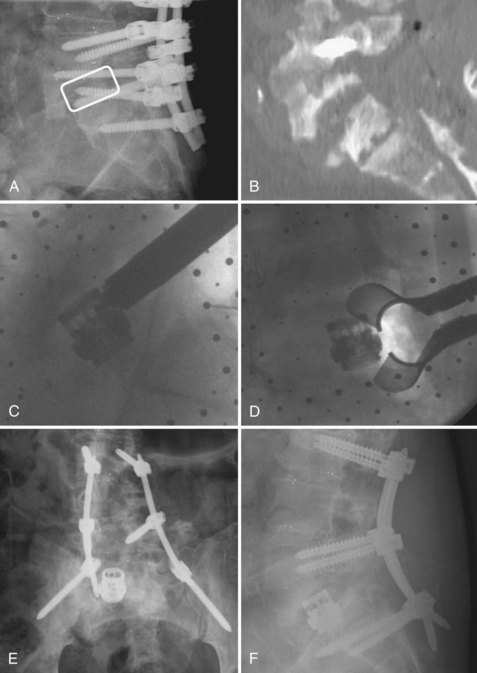
When vertebral osteomyelitis occurs in a patient who has undergone a surgical procedure on the spine or sustained a penetrating trauma of the spine, a fistula should be suspected. Depending on the level of the spine infection, the appropriate imaging study (barium swallow or gastrointestinal series) or endoscopic examination should be ordered to rule out a fistula. If a fistula is identified, it must be repaired along with treatment of the spine infection (Fig. 86–12).
Costotransversectomy or the slightly more extensive lateral rachiotomy described by Capener is recommended when a spine biopsy or minimal decompression with limited grafting is necessary or when gross purulence is expected.202 This approach is being used more frequently with the advent of improved spinal reconstruction devices such as expandable cages. Lu and colleagues203 reported on 36 patients with known vertebral osteomyelitis treated with anterior débridement and reconstruction with an expandable titanium cage. In four of those cases, a transpedicular approach was used to perform débridement anteriorly followed by insertion of an expandable cage from the same posterior exposure. All four patients had an excellent clinical result. The transpedicular approach has several advantages. First, the entire surgery can be completed in a single stage. In the treatment of burst fractures, single-stage surgery leads to shortened total operative time and decreased total blood loss.204 Mochida and colleagues205 described the treatment of osteoporotic compression fractures through a transpedicular approach. This strategy is better described in the treatment of metastatic spinal tumors.206 Senel and colleagues207 described good results with transpedicular tumor resection in seven patients with spinal metastases from breast, prostate, and thyroid cancer. Similarly, Bilsky and colleagues208 described 25 patients who underwent posterior-only transpedicular procedures when comorbidities precluded an anterior approach or when the tumor was likely inaccessible entirely from an anterior approach. More recently, this technique has been used by Lee and colleagues209 for the correction of late traumatic thoracic and thoracolumbar kyphotic spinal deformities in 28 patients. In light of the advantages of single-stage surgery, it appears that anterior-only single-stage surgery may be less advantageous. In the study by Lu and colleagues,203 there was a difference in terms of postoperative pain among various procedures. Only 60% of the patients who underwent an anterior-only approach reported being pain free, as compared with 81% of patients who had anterior-posterior surgery and 100% of the patients who had a transpedicular approach. Furthermore, one of two recurrent infections at the site of previous débridement occurred in the anterior-only patient.203 Historically, much concern for the fate of the hardware has prompted removal of the retained instrumentation once a fusion is obtained. However, in the authors’ experience, the need for instrumentation removal due to recurrent infection at the original site of infection is uncommon. Routine removal of retained spinal instrumentation placed for vertebral osteomyelitis is not recommended.
Recent advances in minimally invasive spine (MIS) techniques offer alternative methods of surgical treatment. Staatz and colleagues210 reported on 21 patients treated with catheters inserted into abscess cavities adjacent to the vertebral body via CT-guidance. Two patients went on to surgery; however, the remainder were successfully treated with catheter drainage and parenteral antibiotics. Percutaneous suction-irrigation systems combined with posterior external fixation have also been shown as effective, minimally invasive treatment.211 However, the use of external fixators in the spine has not gained wide acceptance. Percutaneous débridement of the infected disc such as via automated percutaneous lumbar discectomy212 or endoscopic discectomy213–215 holds promise as a means of hastening antibiotic treatment when infection is identified before significant bony collapse, abscess formation, and deformity develops. Such techniques would be used when antibiotic treatment alone is likely to be insufficient, but the infection is not severe enough to warrant major spinal surgery. Korovessis and colleagues216 showed in a small number of patients that anterior débridement and reconstruction with titanium mesh cages followed by posterior MIS screw fixation led to decreased blood loss and shortened operative time. In a series of 24 consecutive patients, the last 8 cases were treated with posterior fixation and intertransverse fusion using bilateral paramedian intermuscular approaches. Intraoperative blood loss for their initial open posterior surgeries was 540 mL (range, 350 to 750 mL). With the MIS technique, blood loss averaged only 70 mL (range, 50 to 100 mL). This difference was statistically significantly (P < 0.001).
The combined used of expandable titanium cages and a minimally invasive posterior transpedicular approach provides another method of surgical treatment. Kim and colleagues217 have described a unilateral paramedian (Wiltse-type) approach to expose the posterior aspect of the involved vertebral body. A subtotal vertebrectomy can then be performed using the transpedicular technique, followed by insertion of an expandable cage that can be placed in a smaller collapsed form and thereafter expanded to the proper size in situ (see Fig. 86–12). Similarly, the use of MIS direct lateral interbody fusion (DLIF/XLIF) techniques shows promise for the treatment of frail patients with vertebral osteomyelitis (Fig. 86–13).
The recent advent and commercialization of bone morphogenetic proteins (BMPs) provides another adjunctive treatment. In both human and animal studies of infected long bone defects, the use of BMP led to improved bone healing in the presence of active infection.218,219 Several studies in humans shows similar efficacy in the treatment of vertebral osteomyelitis. Garfin and colleagues220 reported on 14 patients treated by anterior reconstruction using structural allograft or titanium cages filled with BMP-2. Despite the presence of active infection, all 14 patients went on to solid fusion and eradication of infection. In 8 of the 14 cases, treatment was successful even when the anterior and posterior surgeries were performed on the same day. Similar results have been reported by other groups. O’Shaughnessy and colleagues221 reported on the successful treatment of 20 patients with at least 2-year follow-up. Aryan and colleagues222 showed successful treatment in 15 patients. On the basis of the mechanism of action and histologic studies of BMP in animal models, it is hypothesized that BMP increases vascular ingrowth and recruitment of immunologic cells to the site of infection.220 BMP has not been proven to be safe or effective in large-scale studies of infection, and its use in this setting would be considered to be a physician-directed (off-label) use by the Food and Drug Administration.
Prognosis
Relapse of infection is uncommon if antibiotics are administered for more than 28 days.29,90 Nonoperative treatment has a higher failure rate in patients with an impaired immune system.22 The mortality rate is less than 5% to 16% depending on the average age and comorbidities of patients in the series. Death is much more likely in the elderly and in those with an underlying disease.22,29,31,90 In one series, S. aureus infection was associated with a higher mortality rate than infection with other pathogens.22
Factors that have been found to predispose a patient to paralysis include increased age, a more cephalic level of infection, and a history of diabetes mellitus or rheumatoid arthritis.90 In one series, a neurologic deficit occurred in 45% of the 44 patients who had an impaired immune system, whereas only 19% of the remaining 67 patients developed a deficit.22 Less than 7% to 15% of patients overall have residual neurologic deficits.22,29 Diabetics are more likely to have permanent neurologic deficits, and patients with thoracic involvement are the least likely to recover.29,90 Eismont and colleagues90 described the results of operation in 14 patients with spinal cord paralysis. Three of the seven patients who underwent a laminectomy deteriorated, and four remained unchanged. In contrast, half of the patients treated by an anterior procedure recovered normal or nearly normal function, and no patient was made worse by the procedure. The patients with root lesions alone had an excellent outcome with or without operation.
In selected patients who require surgical treatment for pyogenic osteomyelitis, the prognosis is very good after the anterior débridement and primary bone grafting in conjunction with a full course of antibiotics. In a series of 21 patients, of whom 6 had neurologic deficits, there were no deaths and no relapses and all of the patients with neurologic deficit recovered. All but one of the patients who underwent fusion had a solid fusion, and one of the two patients who did not have a graft had spontaneous fusion. The mean increase in kyphosis was 3 degrees.170
Garcia and Grantham31 found that spontaneous interbody fusion was the rule and occurred in less than 1 year in most patients and in 2 years in almost all other cases. Some studies have found that the chance of spontaneous fusion in patients treated nonoperatively is 50% or less.24,29,103 Fortunately, those who do not develop a bony union achieve a fibrous ankylosis, which is generally painless.24,31,103,104 Occasionally, a patient complains of persistent back pain from localized degenerative changes at the site of previous infection.24,31,103
The more cephalad the level of infection, the higher the rate of spontaneous fusion; almost all cases of cervical infection will fuse spontaneously.15,37 In one series, 6 of 6 cervical lesions went on to solid interbody fusion, compared with 22 of 29 thoracic lesions and 5 of 21 lumbar lesions.15 One of the patients with cervical infection and one with thoracic involvement had undergone posterior fusion. Fifteen of the patients with thoracic disease underwent costotransversectomy, and five patients with lumbar involvement had anterior débridement without fusion.15
Although deformities are much less common with pyogenic infection than with TB infection, they still may occur.24,223 Deformities have been reported to occur in the cervical spine223 but are more common in the thoracic and thoracolumbar areas and in those cases with involvement of more than 50% of one or more vertebral bodies.24 Interestingly, IV drug abusers have an excellent prognosis. Ninety-two percent responded to parenteral antibiotic therapy for 4 weeks or more, and relapses responded to a second course. In 67 cases reported in the literature, there were no deaths or permanent neurologic sequelae.38
Overall, the long-term outcome of patients with vertebral osteomyelitis is relatively poor compared with the normal population. O’Daly and colleagues assessed the long-term functional outcome of patients with pyogenic spinal infection using the Oswestry disability index (ODI) and the SF-36 survey to measure health-related quality of life (HRQOL).102 Twenty-nine patients with a median follow-up of 61 months (range 37 to 104 months) were examined. IV drug use was not reported in the study population. Eight patients (28%) underwent operative treatment and 21 (72%) were managed nonoperatively with antibiotics alone. “Recovery” was classified as survival and disappearance of all signs and symptoms of active infection with no residual disability. “Adverse outcome” was classified as survival and disappearance of all signs and symptoms of infection, but persistence of clinically significant residual disability or pain, or death caused by or associated with persistent infection at any time before follow-up. Nineteen patients (66%) had an “adverse outcome” as defined by this study. As expected, there were marked differences in SF-36 between these patients and the normative population. However, the “recovery” group patients had SF-36 physical function scores and ODI scores that were comparable with the normative values. There was no correlation between SF-36 bodily pain and general health measures and the ODI. Forty-eight percent of patients reported being pain free. Due to the small number of patients, no statistically significant difference was found between patients who underwent surgery compared with patients treated nonoperatively. Delay in diagnosis (>8 weeks) and neurologic deficit at diagnosis were independent risk factors for an “adverse outcome.” Advanced age was a risk factor for acute death, and previous surgery at the site of initial infection was a risk factor for recurrent infection.
Woertgen and colleagues224 compared the outcome of operative and nonoperative treatment using the 36-item short form health survey (SF-36). The authors retrospectively investigated 62 patients suffering from pyogenic spinal infections: 28 patients (45%) underwent nonoperative treatment and 34 (55%) underwent surgery. As seen in the study by O’Daly and colleagues,102,224 most patients continued to suffer some sort of pain and various SF-36 measures did not reach normative levels. Despite different indications, the surgically treated patients experienced a slightly better QOL, self-reported satisfaction levels, and better clinical outcomes than patients treated nonoperatively. These results support the current recommendations that surgery should be pursued in those patients with progressive neurologic deficits, in those with obvious spinal instability, and in cases in which medical therapy has failed.
Epidural Abscess
Epidemiology
An epidural abscess is a bacterial infection of the spine that results in the accumulation of purulent fluid or infected granulation tissue in the epidural space. Most cases occur in adults (mean age, 57 years; range, 2 to 81 years).225 Occurrence in children younger than age 12 years is rare.226 The male-to-female ratio is approximately 1 : 1.225 The incidence of the disease is 0.2 to 1.2 per 10,000 hospital admissions per year.227 At the University of Miami/Jackson Memorial Hospital Medical Center, 137 spine infections were treated by the orthopedic service over an 8-year period and, of these, epidural abscess occurred in 10 (7.3%).136
Danner and Hartman225 noted an increased frequency at their hospital between 1971 and 1982. This increase was disproportionate to the small increase in admissions and laminectomies performed at that hospital. The authors’ proposed explanations were an increased use of medical instrumentation, an increase in frequency of IV drug abuse, and an aging population.225 Other investigators have also documented an increasing incidence in the condition.228,229
Etiology
The primary source of infection can be identified in approximately 60% of the cases.225 Infection may occur by hematogenous spread from a remote focus of infection,225,227,230–233 by spread from a contiguous focus of vertebral osteomyelitis or a disc space infection,136,225,227,232,234 or from direct inoculation at the time of operation, epidural steroid injection, lumbar puncture, or epidural catheterization.40,225,227,232,235–237 In 136 cases compiled from five series in the literature, skin and soft tissue infections were thought to be the source in 21%, bone or joint infections in 13% (up to 28% if vertebral osteomyelitis is included), spine surgery or other procedures in 10%, upper respiratory tract infection in 6%, abdominal sources in 4%, urinary tract infection in 2%, and IV drug abuse in 4%.3,225,227,231,233 The incidence of epidural abscess after catheter insertion is about 0.001%.238 Although this risk is low, the increased use of epidural analgesia as a method of postoperative pain control is increasing.
Factors that may be associated with a higher incidence of infection include diabetes mellitus, human immunodeficiency virus (HIV) infection, IV drug abuse, prior back trauma, and pregnancy.51,136,225,227,234 Between 12% and 30% of patients reported an episode of trauma preceding the infection.225,227,234 A review of 75 patients from Baltimore revealed an increase in the incidence of epidural abscess over the prior 10-year period.239 This increase may in part be due to better diagnostic techniques, particularly with gadolinium-enhanced MRI. This study population may be at higher risk of this disease. In this series of 75 patients, 33% had a history of IV drug abuse.
Bacteriology
In 1948 Heusner reported on 20 patients with an epidural abscess; S. aureus was the pathogen in all of the cases in which the organism was known.232 In more recent series, S. aureus accounts for approximately 60% of cases in which the organism is known.225,227,233 From the results in 166 patients from five series, S. aureus accounted for 62%, aerobic streptococci for 8%, Staphylococcus epidermidis for 2%, aerobic gram-negative rods for 18%, anaerobes for 2%, and other bacteria for 1%; 6% of the organisms were unidentified.225,227,231–233 Gram-negative organisms have been reported with increasing frequency.227,230,233 One study found that IV drug abusers were frequently infected with gram-negative organisms233; in another series, 12 of 18 IV drug abusers were infected with S. aureus and only one with Pseudomonas.35 A meta-analysis of 915 patients by Reihsaus and colleagues240 showed that S. aureus accounted for 73%, other staphylococcal species 9.3%, aerobic streptococci for 7.7%, Enterobacteriaceae (mainly E. coli) 4.9%, Pseudomonas species 4.9%, mixed bacterial infections 3.6%, and fungi 1.7%.
Pathogenesis/Pathology
The epidural space is filled with fat and loose areolar tissue containing numerous veins.241 The size and shape of this space is determined by the variations in size of the spinal cord. In the cervical region, this is a potential space with almost no fat between bone and dura. The epidural space exists only dorsal to the origin of the spinal nerves. Ventrally, the dura is closely applied to the canal from C1 to S2. Posteriorly, the space begins to appear at C7 and gradually deepens along the thoracic vertebrae to a depth of 0.5 to 0.75 cm between T4 and T8. The space tapers again and becomes shallow between T11 and L2 and attains its greatest depths below L2. Below S2, the epidural space surrounds the dura on all sides.242 The epidural space communicates with the retroperitoneal and posterior mediastinal spaces through the intervertebral foramina.243 As would be expected by this description of the anatomy, most epidural abscesses are in the thoracic and lumbar spine and are generally posterior.225,227,231–233,244–246
In several series, the thoracic spine was involved in 51% of cases, the lumbar spine in 35%, and the cervical spine in 14%.225,227, 232,233,244,245 The abscess was anterior in 21% and posterior in 79% of the 133 patients from four series in which the location was recorded.225,227,231,232 An abscess is more likely to be located anteriorly if the infection is in the lumbar spine and if it is secondary to vertebral osteomyelitis.225,231 Because there is no anatomic boundary within the space, the infection may extend the entire length of the canal but generally covers only three or four segments.136,225,226,232,233,245
The pathogenesis of the neurologic manifestations is related either to direct compression from epidural pus or granulation tissue or to disruption of the intrinsic circulation of the cord.227,232,234,241 A microangiographic study in a rabbit model demonstrated that the initial neurologic deficit is related to compression rather than to ischemia. The spinal arteries and epidural venous plexus remained patent in cases of mild to moderate spinal cord compression. The vessels became occluded only with extreme spinal cord compression.247 On the basis of postmortem examinations, Russell and colleagues234,246 identified thrombosis and thrombophlebitis of the veins of the cord and epidural space without involvement of the arteriolar supply. However, others have found thrombosis of the arteriolar supply and veins.227
Several authors have identified a correlation between the duration of infection and the gross appearance at operation or postmortem examination. Corrandini and colleagues described an early presuppurative phase in which the inflammatory lesion was characterized by an epidural mass of swollen, red, friable fat without any gross pus.248 In patients who have had symptoms for less than 2 weeks, gross pus with varying amounts of red granulation tissue has been identified.225,227,234,246,248 Above and below the level of the pus, the epidural fat may undergo reactive changes and appear swollen and necrotic.234 In patients with symptoms of longer duration, granulation tissue is often identified on the dura. Small beads of pus embedded in the granulation tissue are frequently observed.225,227,246,248 In delayed cases with symptoms for 150 days or longer, grayish-white granulation tissue or maturing fibrous tissue has been found.246 Some authors have thought that it is not always possible to predict whether pus or granulation tissue is likely to be found at operation.231–233 Hancock described patients in whom granulation tissue was found 1 day after the onset of symptoms and other patients who had had symptoms for up to 4 weeks and had no granulation tissue at operation.231 Subdural extension of infection is possible but uncommon.83,227 With spinal cord involvement, there may be evidence of vessel thrombosis, inflammatory response of glial cells, and myelomalacia with liquefaction and vacuolization of the white matter.234,241
Clinical Presentation
Patients with an epidural abscess have a highly variable presentation, which causes initial misdiagnosis in approximately 50% of cases.225 The difficulty in making the correct diagnosis frequently leads to significant delays between presentation and definitive treatment.* Patients who present acutely and who have had symptoms for less than 2 to 3 weeks generally have a better-defined syndrome than do patients with chronic disease. The differentiation between acute and chronic disease is somewhat arbitrary and probably relates to the virulence of the organism, the resistance of the host, and the type of treatment received before definitive diagnosis. Most patients with an acute epidural abscess present with fever, back pain, and spine tenderness. These signs and symptoms may be lacking in patients with chronic disease.136,231,232,234,244–246 The most common presenting symptoms are spinal pain (89%), neurologic deficit (80%), and fever/chill (67%). Local tenderness (48%) and paresthesia (28%) are less common.251 Patients with a history of IV drug use, diabetes, or multiple medical problems are particularly susceptible.239
Without treatment, the disease frequently progresses through four stages. The patients complain of local spine pain initially, followed by radicular pain and weakness and, finally, by paralysis. Heusner is frequently given credit for defining these stages of progression; however, Browder described the same syndrome in 1937, and a number of other authors reiterated the pattern before Heusner’s report in 1948.232,234,248,250,252 The transition from one stage to another is highly variable, and weakness or paralysis may not develop for many months or may occur suddenly and unpredictably in a matter of hours.136,225,245 The location of the pain depends on the site of disease and, therefore, pain is more common in the thoracic than in the lumbar or cervical spine.
If the abscess penetrates the dura, a subdural abscess or meningitis may result.83,227 Many patients with an epidural abscess have nuchal rigidity, and this sign is not helpful in differentiating an epidural abscess from meningitis.227 Fraser and colleagues83 suggested that a patient with a subdural abscess presents exactly like one with an epidural abscess, except that often there is no spinal percussion tenderness. Butler and colleagues253 reviewed 16 patients with subdural abscesses described in the literature and found that only four had spinal tenderness. Unfortunately, this feature is not pathognomonic because not all patients with an epidural abscess have spine tenderness.231,244
Heusner thought that it was possible to differentiate patients with acute hematogenous epidural abscess from those whose abscess developed secondary to vertebral osteomyelitis: The latter patients had a predictable delay between the phases of spine pain and radicular pain followed by rapid progression of the illness.232
Diagnostic Evaluation
Patients with an acute epidural abscess generally have more systemic illness than those with vertebral osteomyelitis. Despite this, the initial diagnosis is incorrect in most cases.251 The leukocyte count and the erythrocyte sedimentation rate are generally increased. In a meta-analysis of 915 patients, the mean erythrocyte sedimentation rate (ESR) was 77 (range 1 to 150 mm) and the mean leukocyte count was 15,700/µL (range, 1500 to 42,000/µL).240 Patients with chronic disease usually have less systemic illness and display leukocyte counts that are often normal.227
C-reactive protein (CRP) is a sensitive marker for infection. In a study of 26 patients with epidural abscesses treated without surgery, the initiation of antibiotic therapy led to a rapid drop in CRP within 5 to 10 days.254 CRP values returned to normal on average at 25.5 days. The definitive diagnosis is based on identification of the organism. Pus from the abscess is positive in approximately 90% of the cases, blood cultures are positive in 60%, and cultures of spinal fluid yield the organism in approximately 17%.225,227,231–233
Imaging Studies
Plain radiographs are frequently normal unless vertebral osteomyelitis or disc space infection is present and enough time has elapsed for the radiograph to become positive.35,246 Radionuclide studies are often helpful but nonspecific and may be falsely negative.35 The gallium scan may be slightly more sensitive than the technetium scan.35
In the past, myelography was the standard imaging tool for the diagnosis of an epidural abscess, but now it is used only if the patient is unable to undergo MR imaging or if spinal fluid is necessary for diagnostic testing. The puncture should be performed at a level remote from the expected area of infection. It may be necessary to perform injections at two sites in order to demonstrate both the cranial and caudal extents of compression. The findings are those of an extradural mass, and generally there is a high-grade or complete block. The lateral myelogram will demonstrate whether the abscess is anterior or posterior.227,233,246 In one series, myelography was accurate to within one vertebral level in both the cephalic and caudal extents of the abscess in 10 of 12 cases compared with findings at operation.136
The needle should be inserted slowly and, if pus is encountered, a specimen should be taken for culture without entering the thecal sac; myelography can then be performed at a different level. At the time of myelography, CSF should be studied for cell total and differential counts, glucose, protein, and culture and sensitivities. The CSF findings generally reflect a parameningeal infection with markedly increased protein content and no bacteria unless there is an associated subdural abscess or meningitis.227,233,246 If a CT scan can be done expeditiously after the myelogram is performed, the degree of neural compression will be defined more accurately.
Plain CT scans may be helpful if they demonstrate an extradural mass.35 Plain CT has a high false-negative rate, and in one study it was diagnostic in only four of nine cases.225 The CT scan may demonstrate hypodense tissue in the epidural space.235 If gas-forming organisms are present, gas may be seen within the epidural space.255 When positive, CT could be useful to guide epidural puncture for isolation of the organism.256 Contrast-enhanced CT has been found to be helpful by some authors.256–259 Positive findings include the loss of physiologic epidural fat and fixation of contrast at the level of the dura surrounded by an area of higher density between the bone and the dura.256 One major limitation of CT without a preceding myelogram is that the area of interest may be missed unless a large number of cuts are taken.
MRI has proved extremely useful and is the imaging study of choice.136,257,260,261 It is noninvasive and safe and is able to visualize the degree of cord compression and extent of abscess in all directions. In addition, it has the capability of diagnosing disc space infection or vertebral osteomyelitis. Areas of infection have characteristically high signal intensity on T2-weighted images (Fig. 86–14). One potential disadvantage of MRI is that the CSF also has high signal intensity on T2-weighted images; therefore there is little contrast between the CSF and the epidural abscess. This has led to false-negative MRI results, especially with long abscesses that do not have a discrete abnormality.136 MRI may also be falsely negative in patients with concomitant epidural abscess and meningitis because the signal changes in the abscess may not be distinct from those in the infected CSF.134
The sensitivity of MRI at detecting an epidural abscess is increased by administration of gadolinium.137,239,262 The pus in the epidural space will enhance with gadolinium, whereas the CSF will have a low signal intensity on the T1-weighted sequence. Patients who have abundant epidural lipomatous tissue may have false-negative scans because fat has a bright signal on T1-weighted images before administration of gadolinium and the contrast enhancement of the epidural pus may be obscured.262 The epidural venous plexus normally enhances with gadolinium administration and may be mistaken for an epidural abscess.262 The plexus is characteristically more prominent in the cervical spine, and it should be symmetrical and extend into the neural foramens.
Myelography followed by CT should be performed in patients with negative MRI scans if they are suspected clinically to have an epidural abscess.134 Injection of contrast via a lateral C1-2 approach has been advocated as a means of avoiding the abscess pocket (Rigamonti and colleagues239). A repeat MRI with gadolinium enhancement may also detect an infection missed on the first study because there is a short time delay between the onset of clinical symptoms and the MRI appearance of an abnormality on MRI.142,262
Two other conditions to consider in the differential diagnosis of an epidural abscess are epidural metastasis and subdural abscess. It is much more critical to make the appropriate diagnosis in the case of epidural metastasis because the treatment of the two disorders is distinctly different. Subdural abscesses are uncommon. A review of the literature in 1988 revealed only 16 reported cases.253 Myelography will reveal an intradural extramedullary filling defect, usually with a complete spinal block, and may demonstrate defects at several levels.83,253,263,264 CT with intrathecal contrast provides better definition of the process than does myelography alone.35,264 The definitive diagnosis is based on identification of the organism. Pus from the abscess is positive in approximately 90% of the cases, blood cultures are positive in 60%, and cultures of spinal fluid yield the organism in approximately 17%.225,233
Management
An epidural abscess accompanied by a neurologic deficit is a medical and surgical emergency. The goals of treatment are eradication of infection, preservation or improvement of the neurologic status, relief of pain, and preservation of spinal stability. The standard approach to an epidural abscess in the early part of the 20th century was immediate laminectomy for spinal decompression. In 1941 Browder and Meyers241 suggested that chemotherapy might be a helpful adjunct to surgery. Heusner232 found survival rates of 63% in patients managed surgically without antibiotics and 90% in those who received antibiotics in addition. A review of the literature from 1970 to 1990265 revealed 37 cases of epidural abscess that had been treated conservatively. Sixty-three percent of the cases had a successful result; however, some of the patients had poor outcomes.225,227,232,249,252 Nonoperative management of epidural abscesses is recommended only in selected cases: (1) poor surgical candidates, (2) abscess involves a considerable length of the vertebral canal, (3) no significant neurologic deficit, and (4) complete paralysis for more than 3 days.266,267 Surgical decompression and débridement is strictly recommended when there is emerging or worsening neurologic deficit or sepsis.
Nonoperative Treatment in the Neurologically Intact Patient
With increased use of MRI and a heightened awareness of this disorder, more patients are diagnosed early in the course of the disease. Recent reports show many patients present with no neurologic deficits. In this subset of patients, nonoperative treatment appears to be efficacious. In a retrospective review of 30 cases, Sorensen showed that all 8 patients without neurologic deficit were successfully treated with antibiotic therapy alone.254 Liem and colleagues268 reported on 21 patients with thoracic epidural abscesses. Three patients had no neurologic deficit. These patients were treated with antibiotics alone with good results. Mampalam and colleagues267 showed good results in six patients without neurologic deficit treated with 4 to 6 weeks of IV antibiotics. The causative organism was identified by blood cultures. All patients became afebrile within 48 hours after initiation of antibiotic therapy. Most patients also noticed a marked diminution in pain. In most series, antibiotic therapy lasted at least 4 weeks and up to 12 weeks.
Recently, Siddiq and colleagues269 compared the outcomes of patients treated with antibiotics alone (25 patients), antibiotics with percutaneous CT-guided drainage (7 patients), or surgery (28 patients). Nearly half of the nonsurgical group had neurologic deficits. Despite this, the overall treatment outcome was comparable with the surgical group. The only predictor of outcome was neurologic abnormality at the time of hospital admission. This is consistent with previous findings where patients with little or no neurologic deficit had good overall results with nonoperative treatment.265 To date, no randomized study directly comparing prophylactic surgery and medical therapy has been performed. However, it is clear that once neurologic deficits appear, surgical decompression and débridement must be timely. When surgery is performed within 24 hours after the onset of neurologic symptoms, overall good results can be obtained in 53% to 80% of cases.239,268 If surgery is performed after 24 hours, the success rate is 10%.
Thus nonoperative treatment should be pursued with extreme caution. If an epidural abscess is discovered before the onset of neurologic symptoms, the patient should be hospitalized for close clinical follow-up. Identification of the organism is a critical step in the treatment regimen. Often this can be done through blood cultures. If the infection begins in the disc space or vertebral body, a percutaneous biopsy in that area can be performed along with drainage. Once cultures are obtained, IV antibiotics should be initiated promptly and serial physical examination and daily CRP values should be assessed.270 The fever curve and CRP levels should trend downward within 24 to 48 hours. Pain may decrease to some extent. If the baseline leukocyte count was elevated, a downward trend will also be appreciated. In approximately 5 to 10 days, the CRP should be dramatically decreased and is often near normal ranges. Antibiotic therapy should be started immediately on the basis of the Gram stain results and the known bacteriologic basis of the disease. Gram-negative organisms should be suspected if there is a history of a spinal procedure or in IV drug abusers. S. epidermidis should also be considered after spinal procedures.225 The definitive antibiotic therapy should be based on the culture and sensitivity results. Antibiotics should be given in maximal dosages for at least 2 weeks, and most authors recommend 3 to 4 weeks of parenteral therapy.225,227 Antibiotics must be administered parenterally for at least 6 to 8 weeks for coexistent vertebral osteomyelitis.225,227
If the patient remains neurologically intact and afebrile, outpatient treatment can be instituted in the reliable patient. Initially, weekly follow-up examinations and laboratory studies should be performed. Such outpatient therapy is reserved for patients who can reliably return to appointments and can readily respond to changes in their symptoms. In our institution, we typically treat with IV antibiotics for at least 6 weeks. Surgical treatment in this patient population is pursued for the following indications: (1) lack of response to medical treatment, (2) onset of systemic infection (sepsis), and/or (3) development of neurologic signs and symptoms. A lack of response to medical treatment often follows a relatively slow course. There is a lack of decline in the fever curve and CRP levels. Pain may persist or increase. Often this is evident after 5 to 10 days of medical treatment.270 When systemic infection (sepsis) or neurologic deficits emerge, surgical treatment becomes urgent.
Surgical Treatment
It is clear that in a small proportion of patients, a rapid neurologic decline can occur despite the initiation of appropriate antibiotics.265 This can be a devastating event and for this reason, surgical decompression and débridement remain the treatment of choice in nearly all patients. The surgical approach depends on the location of the abscess. Because the abscess is posterior in most cases, laminectomy is generally the treatment of choice.227,232 The facet joints should be left intact for spinal stability. Intraoperative ultrasonography after laminectomy allows localization of epidural masses and differentiation of them from the adjacent spinal cord.134 When the abscess is secondary to vertebral osteomyelitis, it may be necessary to perform both anterior and posterior decompression. Instrumentation and fusion may be necessary in those cases in which spinal stability has been compromised by the decompression. Such extensive reconstruction can be staged at a time subsequent to an initial decompression and débridement in patients who have active comorbidities.
The wound may be closed over drains.225,227,232 Garrido and Rosenwasser271 recommended closure of the wound and continuous suction-irrigation for 5 days after decompressive laminectomy. Baker and colleagues227 recommended open wound treatment in cases with gross purulence followed by closure of the wound only when granulation tissue is identified. If the wound is left open, delayed closure may be carried out when the leukocyte count, sedimentation rate, and temperature return to normal and the wound shows good granulation tissue.232 Closure with wound vacuum-assisted closure therapy (V.A.C., Kinetic Concepts Inc.) may be considered, although no series have been reported to our knowledge on the safety or efficacy of the technique.
In children, an extensive laminectomy is undesirable because of the risk of postoperative spinal deformity.159,249 Hulme and Dott249 suggested two limited procedures for children. They recommended first a laminoplasty type of en bloc removal of the lamina and ligaments with replacement after drainage. Alternatively, they advised exploration of the canal through a small fenestration made by removing ligamentum flavum and portions of adjacent lamina and insertion of thin rubber catheters. They thought that this technique was appropriate when gross purulence was encountered but recommended laminectomy if granulation tissue was found to be compressing the dura.249 Devilers reported on four children successfully managed by a modification of Hulme’s second technique. A single-level laminectomy was performed, catheters were passed cranially and caudally, and the epidural space was irrigated with antibiotic solution. None of the children required reoperation, and no sinus tract developed with this technique.243
A variation of Hulme’s technique was reported by Cardan and Nanulescu in 1987.272 A  -year-old boy with an extensive epidural abscess was treated by epidural lavage using Mancao needles. Three hundred milliliters of isotonic saline was flushed through the epidural space over a 30-minute period while the patient was under general anesthesia. A multiple-hole catheter was then inserted from the sacral hiatus to the midthoracic spine, and a gentamycin isotonic saline solution was administered. The patient improved clinically and, at 18 months postoperatively, was neurologically intact without any sequelae.
-year-old boy with an extensive epidural abscess was treated by epidural lavage using Mancao needles. Three hundred milliliters of isotonic saline was flushed through the epidural space over a 30-minute period while the patient was under general anesthesia. A multiple-hole catheter was then inserted from the sacral hiatus to the midthoracic spine, and a gentamycin isotonic saline solution was administered. The patient improved clinically and, at 18 months postoperatively, was neurologically intact without any sequelae.
A modification of this technique has been employed in adults with good initial outcome. Schultz and colleagues273 reported on two patients with extensive epidural abscesses. Both patients had abscesses extending from the cervical to the lumbar spine. Rather than performing full-length laminectomies, limited approaches above and below the levels of involvement were used to pass Fogarty catheters through the areas of the abscesses. Once the catheters reached to the opposite opening, the balloon was inflated and carefully pulled back through the canal, effectively “milking” the purulent material out of the canal. Usually, two passes were required. Both patients had resolution of the infection. One patient had near full recovery of motor function, and the other patient had moderate improvement of motor function. This technique is promising as an alternative to complete laminectomies, particularly when there is extensive involvement over many levels or when a minimally invasive approach is warranted due to a fragile medical condition of the patient.
Prognosis
The natural history of an untreated epidural abscess is relentless progression of symptoms and eventual paralysis and possibly death. Before the advent of antibiotics, the overall mortality rate was between 55% and 70%.234,241,274 Mixter and Smithwick274 reported on 10 cases; all 3 patients treated nonoperatively died. With surgery, the mortality rate decreased to between 30% and 57%241,274; 50% of the survivors were left with residual neurologic deficit.241 From the data on 168 patients reported in six early series since the introduction of antibiotics, 38% made a complete recovery, 29% had residual weakness, 21% were paralyzed, and 12% died.225,227,231,233,241,244,245 The data from five series published since 1990228,229,275–278 indicated that 78% of patients undergoing surgery recover fully or with minimal weakness. The prognosis is similar for patients with acute or with chronic disease as long as they are managed appropriately.227
The prognosis for neurologic recovery depends on the duration and severity of the neurologic deficit.225,232,233,244,245 Heusner found that most patients with paresis of less than 36 hours’ duration had a complete recovery. No patient with complete paralysis for more than 36 to 48 hours recovers significant neurologic function.232,244,279 Complete sensory loss is also a poor prognostic factor.244 Patients who have an acute progressive syndrome with complete paraplegia occurring within the first 12 hours have a poor prognosis; it is postulated that these patients have spinal cord infarction rather than mechanical compression as the pathogenesis of the neurologic deficit.35 Rigamonti and colleagues239 reported more recently on 75 patients with spinal epidural abscesses. In patients with severe neurologic deficit, treatment after 24 hours had a 47% poor outcome, whereas those treated before 24 hours had a 10% poor outcome. Thus they recommend early surgical intervention in patients with neurologic deficit.
Other associated conditions thought to be poor prognostic factors are diabetes, advanced age, female gender, HIV infection, and associated vertebral osteomyelitis.35,51,232 Furthermore, patients with thoracic level involvement and those with severe deficits preoperatively, also have significantly worse outcomes.280 The prognosis with subdural abscess is relatively similar—two thirds of the patients in reported cases made a complete or good recovery after surgical treatment in association with antibiotic therapy.263,281
Granulomatous Infections
Granulomatous infections may be caused by fungi, certain bacteria, and spirochetes. If a granuloma is identified on the frozen section, appropriate studies should be initiated to assist an accurate diagnosis.282 The most common granulomatous spine infection in the world is tuberculosis. TB spondylitis will be described in detail; the fungal and other granulomatous infections will be briefly reviewed by outlining the differences between them and TB infection. Bacteria in the order Actinomycetales cause chronic infections. This order includes the following families of pathogens: Mycobacteriaceae (genus: Mycobacterium), Actinomycetaceae (genera: Actinomyces, Arachnia), and Nocardiaceae (genus: Nocardia).283
Tuberculosis
The incidence of TB spondylitis varies considerably throughout the world and is usually proportional to the quality of public health services available. It is extremely common in underdeveloped countries where malnutrition and overcrowding are major problems. In affluent countries, the incidence has decreased dramatically in the past 30 years and it now is uncommon.15 Bone and joint involvement develops in approximately 10% of patients with tuberculosis, 284 and half of these affected patients have tuberculosis of the spine.285,286 A neurologic deficit will develop in 10% to 47% of those with TB spondylitis.5,188,286–295 In developing countries, the disease is still a significant source of morbidity and mortality and remains the most common cause of nontraumatic paraplegia.296
In North America, Europe, and Saudi Arabia, the disease primarily affects adults; in Asia and Africa, a large percentage of the patients are children.288,289,294,297–303 These patterns are changing, and a decrease in the incidence of infection in infants and young children has been noted in Hong Kong.300 The age incidence of paraplegia corresponds with the general age incidence of tuberculosis of the spine, except for the first decade in which the incidence of paraplegia is significantly less.291
In the United States, it is estimated that 10% of all tuberculosis cases occurred in HIV-positive patients.304 Although it can occur in patients with any range of CD4 count, disseminated and extrapulmonary disease is more common in patients with CD4 counts less than 200 cells/µL and is an acquired immunodeficiency syndrome (AIDS)-defining condition.304 Weinstein and Eismont51 showed that patients with HIV had a higher rate of osseous spinal tuberculosis than the general public. Their data indicated that HIV positive patients were 11 times more likely to be admitted for spinal tuberculosis than HIV-negative patients. HIV-positive patients represented 24% of the patients admitted with spinal tuberculosis. Among their patients with spinal tuberculosis, the average CD4 count was 75.7 cells/mm3.51
Etiology
Spinal tuberculosis may occur from hematogenous spread from well-established foci outside the spine. The pulmonary and genitourinary systems are the most frequent sources, but spinal tuberculosis may also arise from other skeletal lesions.76,288 At presentation, the primary focus of infection may be quiescent. Spinal involvement may develop from visceral lesions by direct extension.76
Bacteriology
Infection is most commonly caused by Mycobacterium tuberculosis, but any species of Mycobacterium may be responsible.305
Pathogenesis/Pathology
The pathogenesis of the early stages of spinal tuberculosis is similar to that of pyogenic infections of the spine and may result from hematogenous spread or from direct extension of disease.76 One study has suggested that the venous or lymphatic routes may be more important than the arterial system for dissemination of this disease. Blacklock was unable to produce spinal disease by injection of mycobacteria into a vertebra or into the left ventricle of experimental animals.306
There are three major types of spinal involvement: paradiscal, central, and anterior.307 In one series of 914 cases, the disease was paradiscal in 33%, central in 11.6%, and anterior in 2.1%; in 52.8%, the disease was too widespread at presentation for identification of the primary focus.290 Atypical forms of spinal tuberculosis include those with neural arch involvement only and rare cases in which granulomas occur in the spinal canal without bony involvement.290,308,309 A similar classification system along with specific MRI findings have recently been described by Moorthy and Prabhu.310 The actual incidence of tuberculosis primarily involving the posterior elements is unknown but is probably between 2% and 10%.308,309,311 MRI shows homogeneous hyperintense T2-weight signal in the posterior elements and associated paraspinal abscess.310
With paradiscal disease, the infection begins in the metaphyseal area and spreads under the anterior longitudinal ligament to involve the adjacent bodies. In contrast to pyogenic infections, the disc is relatively resistant to infection and may be preserved, even with extensive bone loss.76 Disc space narrowing has been postulated to occur either as a result of extension of disease or from dehydration of the disc secondary to the altered functional capacities of the endplate. MRI shows low signal on T1-weighted images and high signal on T2-weighted images in the endplate, with disc space narrowing, and large paraspinal and occasional epidural abscesses.310
In cases with primarily anterior involvement, the infection spreads beneath the anterior longitudinal ligament and may extend over several segments. The radiographic features include scalloped anterior erosion of several vertebral bodies. This pattern is said to result from aortic pulsations transmitted via a prevertebral abscess beneath the anterior longitudinal ligament.312 However, similar changes have been seen in the cervical spine, and another hypothesis is that the scalloping may be due to changes in local vertebral body blood supply.188 A combination of pressure and ischemia caused by this pus may produce anterior scalloping. MRI reveals subligamentous abscesses, preservation of disc space, and abnormal signal of multiple vertebral bodies.310
In cases classified as central involvement, the disease begins within the middle of the vertebral body and remains isolated to one vertebra. These lesions are frequently mistaken for a tumor. They tend to lead to vertebral collapse and therefore are the most likely type to produce significant spinal deformity.307 Such pathologic fractures may mimic the more common osteoporotic compression fracture.313 MRI in central lesions shows signal abnormality of the vertebral body with preservation of the disc space and may also mimic lymphoma or metastases.310 The pathologic features of TB spondylitis may be altered by secondary pyogenic infection, which may occur through sinus tracts or after débridement procedures.76
The pathologic findings in TB spondylitis differ in several ways from those in pyogenic infections. The disc is relatively resistant to TB infection. The pathologic changes generally take longer to develop and are frequently associated with greater deformity. Large paraspinal abscesses are more common with TB infections.23,28,76,295
There are numerous mechanisms by which a neurologic deficit may develop in a patient with TB spondylitis. The focus of disease may be within the bone or, occasionally, within the spinal canal without osseous involvement.298,308,309,314–317 Seddon recognized that neurologic deficits may occur either acutely or chronically.2 He classified acute disease as “paraplegia of active disease” and recognized that this was due to either external pressure or invasion of the dura. Pressure on the spinal cord may arise from an epidural granuloma or abscess, from sequestered bone and disc, or from pathologic subluxation or dislocation of the vertebra. The paraplegia in chronic cases is related to pressure on the cord from epidural granulomas or fibrosis or from a ridge of bone anteriorly caused by a progressive kyphotic deformity. Several other authors have confirmed these patho-genetic mechanisms at operation or postmortem examination.10,188,284,317–320
An epidural granuloma is analogous to a pyogenic epidural abscess. Most frequently, the granuloma arises by spread from the adjacent bone. Because the primary bony lesion is anterior in the majority of cases, spinal cord compression occurs anteriorly. With posterior arch involvement, however, the cord may be compressed from behind.309,311,321 Although isolated involvement of the neural arch is uncommon, posterior compression from arch involvement occurs in approximately 10% of cases associated with paralysis.12
Rarely, an epidural granuloma may occur directly by hematogenous seeding without any bony involvement.* Other lesions that may cause a neurologic deficit without bony involvement are intradural tuberculomas and TB arachnoiditis.298,314,316 Paraplegia from extraosseous disease occurs in no more than 5% of cases.298
Transdural extension of TB inflammation was first described by Michod in 1871.319 Since then, it has been described by other authors.188,295,316,317,319 Presumably, transdural extension can occur regardless of whether or not the process originates within the bone. Tuberculosis meningitis is characterized by a granulomatous reaction in the subarachnoid space.322 Intradural extramedullary mycobacterial disease is the least common presentation of spinal tuberculosis. In 2005 Roca reviewed 22 cases in the literature over the past 25 years. Only 3 (14%) were HIV positive and had CD4 counts of 137 to 228.322 Roca reported that the majority of patients (82%) with intradural extramedullary tuberculomas required operative intervention. At surgery, pathologic tissue revealed granulomatous reaction secondary to a persistent inflammatory reaction.322 Although organisms may be absent in the specimen, immunohistochemical staining reveals tuberculosis antigen (Fig. 86–15).
Clinical Presentation
The clinical presentation of TB spondylitis is variable and depends on many factors. In the classic presentation, the patient complains of spine pain and exhibits manifestations of chronic illness such as weight loss, malaise, and intermittent fever. The physical findings include local tenderness, muscle spasm, and restricted motion. The patient may also have a spinal deformity and neurologic deficit. The duration of symptoms before a definitive diagnosis is made varies from months to years; most cases are diagnosed in less than 2 years.188 In affluent countries, presentation is generally early, whereas in underdeveloped countries the complications of neglected disease such as paraplegia, kyphosis, and draining sinuses may be the presenting complaints.295,302,323
The location of the pain corresponds to the site of the disease, which is most frequent in the thoracic region, less common in the lumbar region, and rare in the cervical spine and sacrum.188,290,293 Patients may present with an abscess in any one of many locations including the groin and buttocks.307 In 10% to 47% of patients, neurologic deficits develop during the course of their disease.5,188,286–288,290–295 The incidence of paraplegia is higher with spondylitis in the thoracic and the cervical spine.290,324
The manifestations of cervical spine involvement vary with the age of the patient. Children younger than age 10 years usually have extensive disease, with large abscesses and a relatively low (17%) incidence of paralysis. In patients older than this, the disease is more localized with less pus, but the incidence of paraplegia is 81%.324 A distinct syndrome has been reported in heroin addicts with TB spondylitis. All five patients in one series had an acute toxic reaction with fever, back pain, weight loss, night sweats, and rapidly evolving neurologic deficits. All patients had disseminated tuberculosis with involvement of extravertebral sites.325
Diagnostic Evaluation
The sedimentation rate is generally increased with TB spondylitis, but this is nonspecific. The tuberculin purified protein derivative (PPD) skin test is usually positive and indicates either past or present exposure to Mycobacterium.298 Cultures of early morning urine samples may be helpful in cases of renal involvement, and sputum specimens and gastric washings may be positive with active pulmonary disease. These laboratory findings are helpful in the diagnosis, but an absolute diagnosis can be made only by biopsy of the spine lesion.176 Aspiration of a subcutaneous abscess on occasion may reveal the organism and obviate the need for spine biopsy.
Isolation of Mycobacterium from clinical specimens takes 6 to 8 weeks, and the sensitivity of culture may be as low as 50%.326 In the past, the most rapid method of detecting mycobacteria was the staining and smear microscopy of acid-fast bacilli (AFB). However, the AFB smear technique requires 5000 to 10,000 bacilli per milliliter of sputum for detection with only 50% to 80% of specimens testing positive.327 Polymerase chain reaction (PCR) has been used to rapidly identify the presence of mycobacterium in formaldehyde solution–fixed, paraffin-embedded tissue specimens.328 Over the past several years, a number of commercially available molecular detection systems have been introduced. All of these systems use detection of mycobacterium DNA or RNA, using the publication of the M. tuberculosis genome.327 These extremely sensitive detection systems require great care in minimizing contaminants in the sample specimens and thus are relatively expensive. Molecular detection systems are also able to test for genes known to be associated with drug resistance including rifampin, isoniazid, pyrazinamide, ethambutol, and streptomycin. The specificity of molecular detection techniques is approximately 98%, the sensitivity 85%, the positive predictive value 95%, and the negative predictive value 93%.329
The findings on plain radiographs of the spine will vary depending on the pathologic type and chronicity of the infection. The earliest finding may be bone rarefaction, regardless of type. With peridiscal involvement, disc space narrowing is followed by bone destruction, similar to pyogenic infections. With anterior multilevel spine involvement, the anterior aspect of several adjacent vertebrae may be eroded in a scalloped fashion. Central body involvement resembles a tumor, with central rarefaction and bone destruction followed by collapse. The initial radiographs often show far advanced bony changes, in contrast to pyogenic infections in which radiographs may be normal on first presentation. The central type is more common in the thoracic area, and the peridiscal variant is more common in the lumbar region. The central type causes greater and earlier bone collapse than the peridiscal type.307 Although these radiographic changes are characteristic, a diagnosis based on radiologic changes alone is inadequate in 10% of cases.330
Chest radiographs are helpful in demonstrating pulmonary involvement and may show a paraspinal abscess. It is not possible to differentiate fibrosis and paravertebral edema from abscess formation on the basis of plain radiographs.188 Occasionally, lumbar spine radiographs will demonstrate calcification in the psoas muscle in cases with a long-standing abscess.188 Sclerotic reactive bone formation occurs with healing of TB infection but is seen much later and is less marked than with pyogenic infection.86 Heroin addicts with Pott disease may have atypical radiographs. In one study, four of five patients had atypical radiographs including two with an ivory vertebra.325 Radionuclide scanning with technetium or gallium may help to define the extent of disease.331 Gallium scanning has been recommended for diagnosing extrapulmonary tuberculosis and also to monitor the response to treatment.331 Unfortunately, radionuclide scans are not sensitive for TB infection; technetium bone scans are negative in 35% of cases, and gallium scans are negative in 70%.298 CT is useful to delineate soft tissue changes around the spine and in the canal but is not capable of differentiating an abscess from granulation tissue.
MRI is the imaging modality of choice because it demonstrates both bony and soft tissue involvement. The MRI findings in TB spondylitis may be indistinguishable from pyogenic infections, but there are some differences that are characteristic of tuberculosis and reflect the different pathologic types described earlier.332 The intervertebral disc may have normal height and a normal signal on MRI, reflecting the resistance of the disc to TB infection (Fig. 86–16). Involvement of the anterior aspect of several contiguous vertebral bodies or involvement of posterior elements suggests a diagnosis of TB spondylitis. Paraspinal masses tend to be longer in TB spondylitis than in pyogenic infections and can be imaged well with plain or gadolinium-enhanced MRIs. Enhanced scans can distinguish abscesses from granulation tissue (Fig. 86–17). A mass with near-total enhancement is generally granulation tissue, whereas a mass with enhancement only at the periphery is generally an abscess.333 As the infection resolves, the T1-weighted images of the vertebral body characteristically have progressively greater signal intensity.105 Even the MRI findings are not completely characteristic, and a biopsy is necessary in all cases. Central body tuberculosis closely resembles a neoplasm332,334; an epidural TB granuloma without osseous involvement cannot be differentiated from an epidural neoplastic metastatic lesion. The distinction between these conditions can be made only at operation.308
The differential diagnosis should include other bacterial and fungal infections, as well as sarcoidosis and neuropathic spine disease. Sarcoidosis rarely involves the spine but may produce paraspinal masses and circumscribed lytic spine lesions with or without a sclerotic rim. Purely sclerotic lesions occur less frequently.77 Neuropathic disease of the spine is usually limited to one to three contiguous vertebrae and is characterized by marked reactive sclerosis or destruction. Sclerosis associated with neuropathic disease of the spine parallels the base of the vertebral body and commonly involves the posterior arch. It is associated with paraspinal debris but not masses.77
Management
The goals of management are to eradicate the infection and to prevent or treat neurologic deficits and spinal deformity. The modern era in the treatment of spinal tuberculosis began in 1943 with the discovery of streptomycin by Waxmin, and the first major description on the use of streptomycin in TB bone and joint lesions was published by Bosworth and colleagues335 in 1950. The drug had a tremendous influence on the mortality rate from tuberculosis. Between the 5 years before streptomycin was used and the 5 years after its introduction, the mortality rate at Sea View Hospital in New York decreased by 72.5%.258 Kondo and Yamada336 reported a decrease in the mortality rate from 42.9% to 9.3% with the addition of streptomycin to the regimen for patients treated nonoperatively. In patients undergoing Albee’s fusion, the mortality rate was 32% without streptomycin and none with streptomycin. In patients undergoing focal débridement, the mortality rate decreased from 71.4% without streptomycin to 2.1% with streptomycin.336
In 1952 Bosworth and associates published a preliminary report showing encouraging results with the use of isoniazid.337 These drugs and others eliminated the risk of dissemination of disease and the development of chronic sinuses after surgical débridement and allowed radical procedures to be performed in relative safety.338,339 Both drugs were found to be effective without surgery when the patients were kept immobilized in the hospital for long periods.340
In Nigeria, a shortage of medical beds and poor medical facilities forced Konstam and Konstam10,11 to use chemotherapy on an ambulatory basis. Although many patients in their study were lost to follow-up, 96% of those returning were thought to be healed and free of disease. Spinal deformity was found to be a problem with this form of treatment; only 75% developed a bony fusion, 49% had between 0 and 10 degrees of increased kyphosis, and 18% had 30 degrees or more of kyphosis.10 Other authors found reasonably good results with chemotherapy alone.9,288,341
Hodgson and Stock338,342 had excellent results with their procedure of radical débridement and anterior strut graft fusion in association with chemotherapy (the Hong Kong operation). In 1963 the Medical Research Council Committee for Research on Tuberculosis in the Tropics began to investigate these widely divergent forms of treatment. A subcommittee was established that later became known as the Working Party on Tuberculosis of the Spine. This group initiated a number of large-scale controlled prospective trials of treatment methods. The design of each study was based on the available resources in areas where tuberculosis was endemic. The first studies, carried out in Korea and Rhodesia, established that chemotherapy is highly effective in ambulatory patients.301,323,343 These investigations showed that there was no advantage to an initial period of bed rest in the hospital,301 application of a plaster of Paris jacket,343 or addition of streptomycin to the chemotherapy regimen.301,323,343 These results were maintained after 5 years344 and 10 years345 of follow-up. Other studies comparing the effectiveness of débridement with that of more radical resection and bone grafting were carried out at three different centers. In Hong Kong, where the radical procedure was popularized, resection and fusion were found to have advantages in terms of less deformity and earlier bony fusion.346 Patients with extensive disease and neurologic deficit were excluded from that study. In two concurrent studies in Africa in which patients with more severe disease were included, there was no significant difference between the two surgical approaches.302 Most of the patients in the three centers were doing well by the 3-year follow-up, and these results were maintained with up to 5 years of follow-up.303 No changes were found at 10 years in the Hong Kong series.347 The Medical Research Council then set out to determine whether short courses of chemotherapy would be as effective as the standard 18-month regimen (used in all previous studies). In Hong Kong, patients underwent the radical operation and either a 6-month or 9-month chemotherapy regimen of isoniazid and rifampin supplemented with streptomycin for 6 months. The 6-month and 9-month courses were equally effective and at least as successful as the standard 18-month regimen when assessed at 3 years.348 In South India, ambulatory chemotherapy alone with 6- or 9-month regimens was compared with radical surgery plus 6 months of chemotherapy.349 Ninety-seven percent of the patients treated by the 9-month regimen achieved a favorable status at 3 years compared with 93% for the patients in the 6-month ambulatory group. Surprisingly, only 85% of the patients in the surgical series achieved a favorable status. The conclusion of the Research Council was that the treatment of choice for spinal tuberculosis in developing countries is ambulatory chemotherapy with 6- or 9-month regimens of isoniazid and rifampin. Surgery should be considered only for biopsy or the management of myelopathy, abscesses, and sinuses. Even in technically advanced countries they advised against surgery in all cases. When surgery is felt to be necessary, the Hong Kong operation was recommended.347,348 Although the results of the studies in Hong Kong and Africa on radical débridement and fusion versus débridement alone were at variance, the overall conclusion was that the Hong Kong operation allows anterior bony fusion to occur earlier and in a higher percentage of patients. Kyphotic deformity was less common and not progressive in those patients undergoing the more radical procedure.347 Other independent studies have demonstrated the effectiveness of débridement and fusion and support the recommendation of the Medical Research Council.172,176,350–353 The group in Hong Kong has written extensively on this approach and is responsible for its popularity.* Another advantage of anterior decompression and fusion compared with nonoperative treatment that has been demonstrated by a number of authors is the higher recovery rate in patients with neurologic deficit.188,292,294,298
Refinements in antituberculosis chemotherapy have permitted a more selective approach to the surgical management of spinal tuberculosis. Rather than operate in every case, Tuli described a “middle-path” regimen of operating only when medical management failed.12,285 The first line of treatment was drug therapy; operation was considered for the following: decompression in patients with neurologic deficit who failed to respond to conservative therapy, posterior spinal lesions, failure of response after 3 to 6 months of nonoperative treatment, doubtful diagnosis, instability after healing, or recurrence of disease or of neurologic complications. In cases without neurologic involvement, healing occurred in 94% with antibiotics alone. In 200 cases with neurologic involvement, 38% of the patients recovered with drugs alone; of those patients requiring operation, 69% recovered completely. The overall success rate in patients with neurologic complications treated by this regimen was 78.5%.12
The indications for operation outlined by Tuli are similar to our current recommendations, except that patients with a neurologic deficit would be operated on urgently rather than after a delay to see if drug therapy alone would be effective. In general, the indications for operation are the same as with pyogenic infection. Lifeso and colleagues298 think that patients with mild neurologic deficits should not undergo operation because medical therapy alone with close observation is safe. Two of their 23 patients became worse with conservative treatment; both recovered completely after anterior decompression and fusion. They also thought that patients with slight kyphosis could be treated with medical therapy alone because the increase in kyphosis and in the number of affected vertebral bodies reported in children was not found in adults treated medically.298
When an operation is indicated, it is easier to do it early because abscesses tend to dissect along tissue planes. If operation is delayed, fibrosis makes the procedure technically much more difficult. Hodgson and Stock175 found a direct correlation between the duration of neurologic symptoms before the operation and the time for recovery from paraplegia. Others have confirmed this finding.292 Operation also is advised in late-onset paralysis associated with cord compression by a hard bony ridge in association with kyphosis. Hsu and colleagues318 think that, in patients with mild or moderate paraplegia, stabilization alone may be indicated, with decompression reserved for those patients with severe paralysis.
Regardless of whether an operation is performed or not, chemotherapy is an integral part of the management of spinal tuberculosis. The only cases in which chemotherapy is not indicated are those in which late-onset paraplegia from progressive deformity has occurred in a patient with healed inactive disease. Drug therapy is usually started preoperatively but may be started after operation if a biopsy is necessary. The first line of drugs currently in use include isoniazid (INH), rifampin (RMP), pyrazinamide (PZA), streptomycin (STM), and ethambutol (EMB). A number of second-line agents that occasionally are used in special circumstances include ethionamide, cycloserine, kanamycin, capreomycin, prothionamide, and para-aminosalicylic (PAS).355 The choice of agents, dosages, and duration of therapy should be directed by an infectious disease expert.
Multiple drugs are used because of the potential for resistance to a single agent. Selection of rational combinations of drugs is based on the mechanism of action and toxicity of the agents.355 The organisms may be in several different environments and therefore not accessible to all agents. They may reside in the extracellular space, either in the hyperoxic neutral environment of the pulmonary cavity or in the hypoxic acidic environment of caseous material in the spine. They also may exist in the highly suppressive acidic environment inside the activated macrophage. INH and RMP are bactericidal against both intracellular and extracellular organisms.356 RMP may have an advantage against bacilli with low metabolic activity, as are present in caseous material. PZA is bactericidal only in an acidic environment and therefore is effective against intracellular organisms or within caseous lesions. Conversely, STM is active only in the extracellular space and therefore is often used to complement PZA. EMB is bacteriostatic against both intracellular and extracellular organisms and often is used in multiple-drug regimens in place of the once-popular PAS. All the above agents have the potential for significant toxicity. Hepatitis may be caused by both INH and RMP and is four times more common in patients receiving both agents than in those receiving INH alone. INH can also cause dose-dependent peripheral neuritis. The major toxicity of STM is nerve VIII damage; that of EMB is optic neuritis.
Antimicrobial resistance may occur from the multiplication of resistant mutants under the selective pressure of single-drug therapy. Resistance developing during the course of treatment in a patient with an initially drug-sensitive infection is termed “secondary resistance.” “Primary resistance,” defined as infection with drug-resistant organisms in a previously untreated patient, may be transmitted to other patients. The prevalence of primary resistance rose from less than 3% in the United States during the 1970s to approximately 9% by 1986.357 Resistance is much more common in certain urban areas and in patients who are homeless, drug abusers, or infected with HIV. The patterns of drug resistance are variable throughout the world, reemphasizing the need for close follow-up during treatment.10,175,298,348 Resistance is generally not a problem with multiple-drug regimens as long as the patient is in compliance.
A 6-month three-drug regimen including INH, RMP, and PZA is used for most cases of drug-sensitive infection in Western nations. Atypical mycobacterial species are often resistant to standard drug regimens.305 Because spinal tuberculosis carries a significant risk, maximal chemotherapy should be used. In a study of lumbar and lumbosacral spine involvement, triple antibiotic therapy with INH, EMB, and RMP yielded excellent results.358 All patients healed the original site of infection with little change in spinal alignment. At 36 months’ follow-up, kyphosis angle improved slightly by 2.2 degrees and the Cobb angle increased slightly by 5.4 degrees.358 Spontaneous bony union occurred in 87.5% of patients. Purtuiset and colleagues359 reported on their experience of 103 cases of spinal TB occurring in a developed country. Most of their patients (74%) were treated with medical therapy alone and the remainder with surgery. Overall, there were two TB-related deaths. Their mean duration of medical treatment was 14 months. These results are similar to those observed in less developed countries such as India.360
Surgical Treatment
An operation may be performed to drain abscesses, to débride sequestered bone and disc, to decompress the spinal cord, or to stabilize the spine for the prevention or correction of deformity. In 1779 Pott described the drainage of a TB abscess: “The remedy for this most dreadful disease consists merely in procuring a large discharge of matter, by suppuration from underneath the membrana adiposa on each side of the curvature, and in maintaining such discharge until the patient shall have perfectly recovered the use of his legs.”1 His statement was rather optimistic—many patients did not recover neurologic function after this procedure, and many others died of secondary pyogenic infection. In general, abscess drainage is indicated only if the patient is septic from the abscess or has a neurologic deficit from an epidural abscess or when the abscess is extremely extensive. After drainage of an abscess, the tissues may be closed in layers or the wound may be packed open. Paravertebral abscesses in the thoracic spine can be drained effectively by a costotransversectomy.202 Large psoas abscesses may be drained by a retroperitoneal approach.361
Simple débridement of the spine without fusion is advocated by some surgeons.302,336 However, most authors agree with the conclusions of the Medical Research Council that the Hong Kong procedure of anterior radical débridement and strut graft fusion is superior.* Surgery performed when the disease is active is safer, and the response is faster and better than that performed in patients with healed disease.318
In the Hong Kong procedure, the spine is approached anteriorly so that the affected area may be dealt with most directly. The sequestered bone and caseous material must be débrided back to bleeding bone above and below and back to the posterior longitudinal ligament. The decompression should go back to the dura in cases of neurologic deficit when spinal cord decompression is necessary.303 The angular deformity is corrected by insertion of a strut graft. Autogenous bone grafting at the time of the primary débridement is reliable in both adults and children.† The incidence of fusion with a bone graft is 97% at 10 years, compared with 90% with débridement alone. Medical management with chemotherapy alone may yield a solid fusion in 65% to 79% of cases.9,10,103
†References 172, 175, 176, 181, 188, 292, 295, 299, 342, 347, 351, 353, 363–365.
The choice of graft material is based on considerations of graft incorporation and structural support. The grafts used most frequently are iliac crest and ribs. Fibular grafts provide good structural support, but the large amount of cortical bone is undesirable in cases of infection. In addition, long segments of fibula are likely to fracture. In a study of 4-cm-long canine fibular grafts, the grafts were markedly weakened between 6 weeks and 6 months after implantation. The total incorporation may take several years; at 48 weeks, approximately 60% of the necrotic matrix had been remodeled. Despite that, the strength of the graft is nearly normal at 1 year.184 Bradford and Daher185 described the use of vascularized rib grafts for stabilization of kyphosis. Incorporation of the grafts occurred between 4 and 16 weeks (mean, 8.5 weeks). They described three patients in whom the graft was placed 4 cm or more anterior to the apical vertebra for mechanical advantage, and none of these grafts fractured.185 High fusion rates have been reported when vascularized rib grafts are used in the treatment of TB kyphosis.186
Kemp and colleagues172 found that rib grafting was inadequate in adults. They reported a 32% incidence of graft fracture and a mean increase in kyphosis of 20 degrees. Partial collapse occurred in some cases because the ribs penetrated the endplate. The overall fusion rate was 62% with rib grafts and 94.5% when autogenous, full-thickness iliac crest grafts were inserted, as long as they crossed the coronal diameter of the vertebra.172 Iliac crest may be preferable to rib, especially in patients with large defects.172,175,183
McCuen described the first case of TB spondylitis treated by laminectomy in 1882. In the early part of this century it had become a common procedure for patients with Pott paraplegia. In 1935 Seddon condemned the procedure, claiming that “laminectomy is futile” because it removes the integrity of the posterior arch and may lead to instability and further neurologic damage.177 The opinion that laminectomy is contraindicated is shared by many authors.173,291,292,295,317,339,351,366 Patients actually may improve considerably immediately after laminectomy, but, as Bosworth and colleagues335 noted, paraplegia inevitably recurs unless fusion is performed both anteriorly and posteriorly. They described 14 patients who had had laminectomies: all died except 4 who had “circumduction” fusions.335 Currently, the only indication for laminectomy in the treatment of Pott paraplegia is atypical disease involving the neural arch and causing posterior spinal cord compression.145,173,177,309,317 It is also reasonable in rare circumstances with posterior epidural tuberculoma without bony involvement.308
Débridement, decompression, and fusion in the thoracic spine may be performed through a transthoracic approach, through a costotransversectomy, or by an extrapleural anterolateral approach. The last has the theoretic benefit of avoiding the TB empyema.351 However, no studies have demonstrated any actual advantage of an extrapleural approach over a standard thoracotomy. Kirkaldy-Willis and Thomas176 demonstrated that the transthoracic approach is more successful than lateral rachiotomy (modified costotransversectomy). The fusion rate was 95% in the former and 78% in the latter; the mortality was 3% and 8%, respectively.176 They recommended thoracotomy in cases of early tuberculosis, with lateral rachiotomy reserved for late-onset paraplegia associated with a large kyphotic deformity requiring lateral exposure of the dura.176 Kemp and colleagues172 support this concept.
With tuberculosis, the periosteum is generally thicker and frequently adherent to the pleura. Therefore it is often necessary to dissect in a subperiosteal plane for exposure. If a lung abscess is found at the time of thoracotomy, the abscess may be débrided by scooping out the necrotic material. Yau and Hodgson367 rarely found an air leak in this situation and had good success by insufflating the cavity with streptomycin and suturing the visceral pleura. Because of the potential for wound dehiscence in these patients, who are frequently immunocompromised and have poor wound-healing potential, the wounds should be closed in layers with interrupted nonabsorbable sutures. In patients with lesions involving more than two vertebral bodies, a period of bed rest followed by external support in a TLSO is recommended until the fusion becomes consolidated if instrumentation is not used.183
Posterior fusion alone, without instrumentation, does not control progressive kyphosis,368 but it may be performed in addition to anterior strut grafting for added stability (Fig. 86–18).183,188 (If a laminectomy is performed for posterior neural compression, a fusion should also be performed if any of the facets are removed.173 Progressive kyphosis may occur in the immature spine in spite of a solid anterior fusion. Some authors recommend that a posterior fusion should be performed in addition to an anterior fusion in order to eliminate the risk of increasing deformity.173,341 Fountain and colleagues362 found that progressive kyphosis developed in only 3 of 31 children with solid anterior fusions. They recommended performing a supplementary posterior fusion only if progressive deformity is noted.
Anterior grafts may not provide stable fixation, especially in cases in which the graft spans more than two disc spaces.183 To prevent loss of correction, some authors recommend a two-stage procedure with an instrumented posterior fusion followed by anterior débridement and fusion.333,369,370 Moon and colleagues369 reported on 39 adults undergoing the two-stage procedure in the same operative setting or in a delayed fashion. The infection was cured in all cases, and they achieved excellent deformity correction without a prior anterior release. The loss of correction did not exceed 3 degrees. Similarly good results have been reported by other groups from various countries such as Taiwan, South Africa, India, Kuwait, and Turkey.371–375
Güven and colleagues376 recommend a single-stage posterior approach without any anterior procedure in cases without paralysis, multisegmental involvement, or large abscesses. They reported on 10 patients who underwent the procedure. All patients had resolution of the infection and the mean loss of correction was only 3.4 degrees. Mehta and Bhojraj377 have proposed a reasonable classification system for surgical treatment of patients with thoracic spine infection. They propose four treatment groups on the basis of the location of the infection. Group A patients, who had paradiscal or central involvement with no deformity, were treated with transthoracic débridement and strut fusion with no further instrumentation. Group B patients, who had paradiscal or central involvement along with deformity, were treated with transthoracic débridement and strut fusion with posterior instrumentation. Group C patients were similar to group A patients but were too ill to tolerate a transthoracic approach. These patients were treated via a posterior transpedicular decompression and posterior instrumentation. Group D patients, who had only posterior element involvement but no deformity were treated with posterior decompression alone with no fusion or instrumentation. With these treatment guidelines, all their patients did well.377
Oga and colleagues378 studied the risk of using spinal instrumentation despite active TB infection. All 11 of their patients had resolution of the infection and none developed a kyphotic deformity after operation. They also evaluated the adherence properties of Mycobacterium tuberculosis and S. epidermidis to stainless steel. The Staphylococcus heavily colonized the rods and was covered with a thick biofilm, whereas only a few biofilm covered colonies of Mycobacterium tuberculosis were seen. These findings have prompted the use of anterior instrumentation at the time of initial anterior débridement. Three recent reports reveal that this single-stage technique is efficacious. Benli and colleagues379 reported on 63 patients from Turkey with involvement of the thoracic and lumbar spines. All patients underwent anterior débridement and decompression with autogenous iliac crest strut grafting. In the same setting, a lateral plate was applied. Kyphosis was corrected by 89% and maintained at an average follow-up of 51 months. Of the patients who had neurologic deficit, 80% had full recovery and 16% with partial recovery. No recurrence of infection was found. Govender reported on 41 patients from South Africa.380 In these patients the anterior strut was fresh frozen allograft. Compared with autogenous rib graft, the fusion rate was slower with allograft. Fusion and remodeling was seen in 33 of 41 patients and partial remodeling with fusion in 8 patients at a mean follow-up of 6.4 years. There were no cases of fracture or late sepsis. Yilmaz and colleagues381 reported on 22 patients from Turkey with similar results.
The incidence of cord compression with cervical TB spondylitis is more than 40% overall and much higher in adults324; therefore an infection in this region requires aggressive treatment. Hsu and Leong324 reported excellent results from using the Hong Kong procedure via a Southwick-Robinson approach in conjunction with medical management. With C1-C2 involvement, drainage may be performed by the transoral route with or without a supplementary posterior occiput-to-C2 fusion.261 Isolated involvement of the arch of the atlas has been treated successfully in one case by chemotherapy, needle aspiration of an abscess, and halo-brace immobilization.382 Lesions at the craniocervical junction are rare, occurring in only 0.3% to 1% of patients with TB spondylitis.383 Behari and colleagues383 reported on 25 patients treated variably for craniocervical infection. They classified patients as grade I, defined by neck pain only and no pyramidal signs; grade II, defined by a neurologic status of independent but with minor disability; grade III, defined by partial disability requiring assistance with activities of daily living; and grade IV, defined by severe disability including respiratory compromise. Grade I and II patients were treated with brace immobilization and medical therapy. Grade III and IV patients underwent anterior decompression followed by posterior fusion. Significant improvements in all grades were seen with this strategy.
Lesions between C3 and C7 may be approached through either the anterior triangle174 or the posterior triangle. The latter may be preferable in some cases because pus often tracks and points in the posterior triangle, making dissection easier.384 When cervical disease is complicated by kyphosis, staged procedures may be necessary. Strut grafting may be performed at the time of débridement if the deformity can be reduced. If the deformity is too great, traction may be necessary before final anterior grafting. Anterior reconstruction should be followed by posterior stabilization and fusion.354 Laminectomies are contraindicated in the cervical spine because subluxation and further neurologic deficits may occur.324
Complications of surgical treatment are frequent. The operative risk is greatest in elderly patients with extensive disease. In one series, the operative mortality was 2.9% and an additional 1% of the patients died of the disease later.342 Early complications include wound sepsis, pleural effusion, pulmonary embolism, CSF fistula into the pleural cavity, ileus, progressive neurologic deficit, damage to the ureter, loss of graft fixation or graft fracture, atelectasis, pneumonia, air leak, Horner syndrome, and injury to one of the great vessels.181 When streptomycin is placed directly on exposed dura, convulsions may occur.181 Late complications include graft resorption, graft fracture, nonunion, and progressive kyphosis.172,183,385 Adrenal insufficiency may occur secondary to TB involvement of the adrenal glands. Adrenal suppression should be suspected, especially if calcification is noted on radiographic studies.292
Prognosis
Mortality
Before the advent of chemotherapy, the morality rate in patients treated nonoperatively was 12% to 43%.5,290,293,336 The rate in patients with a neurologic deficit was close to 60%.291 In one study, the mortality rate was found to be linked directly to associated pulmonary involvement: 9.4% of the patients with spine infections and inactive pulmonary tuberculosis died, in contrast to 51.3% of those who had active pulmonary disease or metastatic spread to other organs.286 Attempted débridement of the spine without antibiotic coverage was associated with a mortality rate as high as 71%.336 With the chemotherapeutic regimens now available, the mortality rate should be less than 5% if the disease is diagnosed early, the patients comply with the regimen, and follow-up is close.297,298 The mortality rate in patients treated with the Hong Kong procedure in addition to antibiotics is directly proportional to the severity of the neurologic deficit. In one study, among patients undergoing operation, the mortality rate was 2% in those with mild to moderate neurologic deficit, 6% in those with moderate neurologic deficit and 11% in those with a severe deficit.297
Relapse
The relapse rate in patients treated with the antibiotics available between 1952 and 1962 was 21%.288 With current medical regimens and close follow-up, the rate should approach zero.298
Kyphosis
Progressive kyphosis is a significant cosmetic deformity, but more important is the fact that it may cause a neurologic deficit or respiratory and cardiac failure due to restriction of pulmonary function (Fig. 86–19). Rajasekaran and Soundarapandian reported the results of a prospective controlled study performed in collaboration with the Medical Research Council.183 The treatment groups included chemotherapy alone for either 6 or 9 months or radical surgery in combination with 6 months of chemotherapy. Ninety patients (98% of the study group) were followed for a minimum of 6 years. Those who underwent nonoperative treatment had a statistically significant higher rate of kyphotic deformity than those treated surgically. There was a direct correlation between the final angle of the deformity and the amount of initial loss of vertebral body. The angle increased severely in 10% of the surgical group and in 32% of the nonsurgical group. Severe deformity in the surgical group was related to graft failure.
To predict the angle of deformity expected, the researchers devised a formula385; Y = a + bX in which Y is the final angle of the deformity, X is the amount of initial loss of vertebral body, and a and b are constants (5.5 and 30.5, respectively). With their formula, the final angle of the gibbus was predictable, with 90% accuracy in the patients treated nonsurgically.385 If the predicted angle is excessive, early operation should be considered.
Rajasekaran and Soundarapandian183 provided additional information on 81 patients treated by the Hong Kong operation and followed for a minimum of 8 years; 19% of these patients had an increase in the gibbous angle of up to 20 degrees, and in 22% it was more than 20 degrees. The major risk factor for increasing deformity was extensive involvement of the vertebral bodies, which resulted in a large defect after débridement and necessitated a graft spanning more than two disc spaces. Patients with lesions of the thoracic vertebrae and those with marked kyphosis preoperatively were also more likely to have progression. These authors concluded that when the length of the graft exceeds two disc spaces, surgical treatment should be augmented by prolonged bed rest, bracing, or posterior arthrodesis. Rib strut grafts were used in many of the patients with progressive deformities, and it was proposed that iliac crest graft may be preferable in patients with large defects.183 Iliac crest grafts were used exclusively by Hodgson and Stock175 and may explain the low incidence of progressive kyphosis in their series. Others also have recommended the use of iliac crest grafts rather than rib struts.172 In patients with small defects, however, the availability of rib graft and avoidance of additional donor site problems make rib grafts a more attractive alternative.
In addition to graft failure, children are at risk of progressive deformity after anterior débridement and fusion because of persistent growth posteriorly and growth retardation anteriorly. Close follow-up is necessary and a supplementary posterior fusion should be performed if progressive kyphosis occurs.188,362 A study comparing the radiographs of 117 children operated on for spinal tuberculosis at the age of 2 to 6 years showed that anterior fusion alone leads to greater kyphotic angulation than a posterior fusion, a combined anterior and posterior fusion, or anterior débridement alone.386
Neurologic Deficit
Patients with neurologic deficit may improve spontaneously without surgery or chemotherapy293,317 or with chemotherapy alone,10,12,288 but in general the prognosis is improved with early surgery.188,267,298 In one study, 94% of neurologically impaired patients recovered normal function after anterior decompression; only 79% totally recovered after nonoperative management.298 When patients with a neurologic deficit were operated on only if they failed to respond to an initial course of antibiotics, the overall success rate was 78.5%.12 As expected, patients with less severe neurologic deficit and those who were treated early after the development of neurologic signs had a better outcome.12,284,287,295,297,387 In one study of 64 patients, only 48% of those with severe neurologic deficits recovered, whereas 83% of patients with moderate deficits recovered; only 4 of 10 patients with late-onset paraplegia had a satisfactory recovery.297
Patients with paraplegia of long duration should be treated aggressively. Hodgson and colleagues295 found that the chances of complete recovery are good after surgical treatment, although it may take longer for them to recover. They documented recovery in a patient who had had a neurologic deficit for 5 years.295 In patients with late-onset paraplegia, the response to operation is faster, better, and safer in patients who have active disease than in those with healed disease and a hard, bony ridge compressing the cord.318 Overall, most patients with a neurologic deficit recover within 6 months, but those who have direct involvement of the meninges (pachymeningitis) may recover more slowly.295 Govender and colleagues284 found that patients who have an atrophic cord as seen on CT myelography preoperatively usually do poorly after decompression. Patients with cervical spine involvement are at high risk of neurologic deficit but do well after anterior débridement and fusion.324
The only indication for laminectomy is posterior cord involvement. In 19 patients with posterior element disease undergoing laminectomy, 16 had good results and 3 had fair results in one series. Six of 10 patients undergoing laminectomy for epidural tuberculomas without bony involvement had good results, 3 patients had fair results, and 1 had a poor result.308 The overall prognosis with posterior spinal tuberculosis is better in those patients who have less severe neurologic deformity of shorter duration, slower progression, and are younger and in good general health.311 In general, children have a better prognosis than adults.172,188,294,295
Fusion
Bosworth and colleagues291 thought that a solid fusion was essential for permanent recovery from TB spondylitis. They described five patients who initially recovered but became paralyzed again with the development of pseudarthrosis. These patients recovered once again after repair of the pseudarthrosis.291
Spontaneous bony fusion occurred in 27% of patients treated with bed rest in a plaster shell, without surgery or chemotherapy.290 With chemotherapy alone, spontaneous fusion occurred in 24% at 18 months and in 36% at 36 months.341 In the prospective study by the Medical Research Council, the fusion rate in patients treated by the Hong Kong procedure was 28% by 6 months, 70% by 12 months, 85% by 18 months, and 92% at 5 years. The corresponding values for the patients undergoing débridement without fusion were 3%, 23%, 52%, and 84%, and the fusion rates in patients treated by ambulatory chemotherapy alone were 9%, 26%, 50%, and 85%, respectively.
Actinomycosis
Actinomyces israelii is an anaerobic, slowly growing, filamentous, gram-positive bacteria. Actinomyces was originally discovered in 1877 as a genus containing the causative agent of actinomycosis in cattle. Thereafter, in 1891, A. israelii was first isolated from a lung abscess by Wolff and Israel.388 Since then, other Actinomyces spp. and related bacteria have been isolated and are believed to be involved in a wide variety of human infections, most commonly linked to A. israelii. A number of other species have also been involved in human infections. These include Actinomyces meyeri, Actinomyces graevenitzii, Actinomyces turicensis, Actinomyces gerencseriae, Actinomyces odontolyticus, Actinomyces cardiffensis, Actinomyces radingae, Actinomyces naeslundii, other Actinomyces species, and a closely related species, Varibaculum cambriensis.388 It is postulated that the coexistence of other organisms may assist anaerobic growth by reducing the oxygen tension in the local environment.
The diseases it causes mimic those produced by fungi. The organism, an endogenous, oral saprophyte, requires trauma, surgery, or other infection to penetrate the mucosa. Once Actinomyces invades the tissue of a disrupted mucus membrane, it slowly expands and develops into an abscess. It is noted for causing chronic suppurative infections with external sinuses that discharge distinctive aggregates of organisms (“sulfur granules”).282,389 Infections involving Actinomyces frequently are polymicrobic including Fusobacterium, Bacteriodes, Capnocytophaga, Eikenella, Staphylococcus, Streptococcus, and Enterococcus species.389
The lesions are characterized by hard, fibrotic walls with granulation tissue surrounding loculations of pus. Sinus tracts extending to the skin or into other organs are commonly seen in more chronic infections.389 Classic actinomycosis presents as an oral-cervicofacial lesion, known as “lumpy jaw” lesion, which occurs in approximately 55% of actinomycosis cases.390 Infection occurs at other sites and is manifest as thoracic (15%), abdominal and pelvic (20%), musculoskeletal (rare), and central nervous system (rare) disease.77,391
Several risk factors for the development of actinomycosis exist. It occurs more commonly in males, but there is no clear explanation for this. Other risk factors may include poor oral hygiene and the use of intrauterine devices. In addition, immunocompromise and other conditions such as diabetes, alcoholism, infections with immunosuppressive agents (e.g., human immunodeficiency virus), and steroid use are thought to predispose individuals to the development of actinomycosis.388,392
Before 1950, vertebral actinomycosis was the most common form of osseous involvement. Vertebral involvement is usually secondary to an infection at an adjacent tissue. Hematogenous spread is less common for actinomycosis. Vertebral infection occurs by extension from retropharyngeal, mediastinal, or retroperitoneal soft tissue abscesses. Unlike M. tuberculosis, the organism has a predilection for the cervical and thoracic spine from retropharyngeal or pulmonary spread.393,394
Actinomycosis may be difficult to differentiate from mycobacterial and nocardial infections. Accurate diagnosis is essential because the treatment regimens differ markedly from these other organisms. The organism must be isolated from an anaerobic culture, which may take up to 21 days for positive culture growth. As in tuberculosis, the radiographs may demonstrate prominent paraspinal abscesses and involvement of several vertebral bodies. Distinctive features include simultaneous vertebral body and posterior element involvement, spread to adjacent ribs, periosteal new bone formation outlining the vertebra, and a mixture of lytic and sclerotic changes that may produce a honeycomb appearance of the bone.77 The vertebral body collapse and disc space narrowing that are common in tuberculosis are uncommon in actinomycosis.77
Epidural abscesses may occur by extension from a vertebral source or through an intervertebral foramen from a cervical, pulmonary, or abdominal focus.389 The dura generally resists penetration, but neurologic deficit may occur by epidural compression.389 Before the introduction of penicillin, most cases of actinomycosis were fatal. The current treatment is still penicillin in large doses given over extended periods in association with abscess drainage and excision of sinus tracts when necessary.389 Other first-line antibiotics that are effective are tetracycline, erythromycin, clindamycin, and the cephalosporins.395,396 Long-term treatment for up to 6 months is common.394 When response to penicillin is poor, the possible reasons include an undrained abscess, polymicrobial infection, and perhaps bacterial resistance. Overall, the treatment of actinomycosis infection results in good outcomes, even when there is extensive involvement. In a recent case report of a patient with severe mediastinal, paraspinal, and thoracic epidural involvement, limited débridement and laminectomy combined with antibiotics yielded excellent results.397