In patients with subacute presentations, fever is typically low-grade and rarely exceeds 39.4°C (103°F); in contrast, temperatures of 39.4°–40°C (103°–104°F) are often noted in acute endocarditis. Fever may be blunted in patients who are elderly, are severely debilitated, or have renal failure.
Cardiac Manifestations Although heart murmurs are usually indicative of the predisposing cardiac pathology rather than of endocarditis, valvular damage and ruptured chordae may result in new regurgitant murmurs. In acute endocarditis involving a normal valve, murmurs may be absent initially but ultimately are detected in 85% of cases. Congestive heart failure (CHF) develops in 30–40% of patients as a consequence of valvular dysfunction. Occasionally, CHF is due to endocarditis-associated myocarditis or an intracardiac fistula. Heart failure due to aortic valve dysfunction progresses more rapidly than does that due to mitral valve dysfunction. Extension of infection beyond valve leaflets into adjacent annular or myocardial tissue results in perivalvular abscesses, which in turn may cause intracardiac fistulae with new murmurs. Abscesses may burrow from the aortic valve annulus through the epicardium, causing pericarditis, or into the upper ventricular septum, where they may interrupt the conduction system, leading to varying degrees of heart block. Mitral perivalvular abscesses, which are usually more distant from the conduction system, only rarely cause conduction abnormalities; if such abnormalities occur in this setting, the conduction pathway is most likely disrupted near the atrioventricular node or in the proximal bundle of His. Emboli to a coronary artery occur in 2% of patients and may result in myocardial infarction.
Noncardiac Manifestations The classic nonsuppurative peripheral manifestations of subacute endocarditis (e.g., Janeway lesions; Fig. 155-2A) are related to prolonged infection; with early diagnosis and treatment, these have become infrequent. In contrast, septic embolization mimicking some of these lesions (subungual hemorrhage, Osler’s nodes) is common in patients with acute S. aureus endocarditis (Fig. 155-2B). Musculoskeletal pain usually remits promptly with treatment but must be distinguished from focal metastatic infections (e.g., spondylodiscitis), which may complicate 10–15% of cases. Hematogenously seeded focal infection occurs most often in the skin, spleen, kidneys, skeletal system, and meninges. Arterial emboli, one-half of which precede the diagnosis, are clinically apparent in up to 50% of patients. Endocarditis caused by S. aureus, vegetations >10 mm in diameter (as measured by echocardiography), and infection involving the mitral valve, especially the anterior leaflet, are independently associated with an increased risk of embolization. Symptoms, pain, or ischemia-induced dysfunction relate to the organ or area suffering embolic arterial occlusion (e.g., kidney, spleen, bowel, extremity). Cerebrovascular emboli presenting as strokes or occasionally as encephalopathy complicate 15–35% of cases of endocarditis. Again, one-half of these events precede the diagnosis of endocarditis. The frequency of stroke is 8 per 1000 patient-days during the week prior to diagnosis; the figure falls to 4.8 and 1.7 per 1000 patient-days during the first and second weeks of effective antimicrobial therapy, respectively. This decline exceeds that which can be attributed to change in vegetation size. Only 3% of strokes occur after 1 week of effective therapy. Emboli occurring late during or after effective therapy do not in themselves constitute evidence of failed antimicrobial treatment.
FIGURE 155-2 A. Janeway lesions on toe (left) and plantar surface (right) of the foot in subacute Neisseria mucosa endocarditis. (Image courtesy of Rachel Baden, MD.) B. Septic emboli with hemorrhage and infarction due to acute Staphylococcus aureus endocarditis.
Other neurologic complications include aseptic or purulent meningitis, intracranial hemorrhage due to hemorrhagic infarcts or ruptured mycotic aneurysms, and seizures. (Mycotic aneurysms are focal dilations of arteries occurring at points in the artery wall that have been weakened by infection in the vasa vasorum or where septic emboli have lodged.) Microabscesses in brain and meninges occur commonly in S. aureus endocarditis; surgically drainable intracerebral abscesses are infrequent.
Immune complex deposition on the glomerular basement membrane causes diffuse hypocomplementemic glomerulonephritis and renal dysfunction, which typically improve with effective antimicrobial therapy. Embolic renal infarcts cause flank pain and hematuria but rarely cause renal dysfunction.
Manifestations of Specific Predisposing Conditions Almost 50% of endocarditis associated with injection drug use is limited to the tricuspid valve and presents with fever but with faint or no murmur and no peripheral manifestations. Septic pulmonary emboli, which are common with tricuspid endocarditis, cause cough, pleuritic chest pain, nodular pulmonary infiltrates, or occasionally pyopneumothorax. Infection of the aortic or mitral valves presents with the typical clinical features of endocarditis, including peripheral manifestations.
If not associated with a retained intracardiac device or masked by the symptoms of concurrent comorbid illness, health care–associated endocarditis has typical manifestations. CIED endocarditis may be associated with obvious or cryptic generator pocket infection and results in fever, minimal murmur, and pulmonary symptoms due to septic emboli. Late-onset PVE presents with typical clinical features. In cases arising within 60 days of valve surgery (early onset), typical symptoms may be obscured by comorbidity associated with recent surgery. In both early-onset and more delayed presentations, paravalvular infection is common and often results in partial valve dehiscence, regurgitant murmurs, CHF, or disruption of the conduction system.
DIAGNOSIS
In order to avoid delayed or missed diagnosis, careful clinical, microbiologic, and echocardiographic evaluation should be pursued when febrile patients have endocarditis predispositions, cardiac or noncardiac features of endocarditis, or microbiologic findings consistent with endocarditis (e.g., a stroke or splenic infarct, multiple positive blood cultures for an endocarditis-associated organism).
The Duke Criteria The diagnosis of infective endocarditis is established with certainty only when vegetations are examined histologically and microbiologically. Nevertheless, a highly sensitive and specific diagnostic schema—known as the modified Duke criteria—is based on clinical, laboratory, and echocardiographic findings commonly encountered in patients with endocarditis (Table 155-3). While developed as a research tool rather than for patient management, the criteria can be a helpful diagnostic tool. If the criteria are to be maximally helpful in evaluating patients, appropriate data must be collected. Furthermore, clinical judgment must be exercised in order to use the criteria effectively. Documentation of two major criteria, of one major criterion and three minor criteria, or of five minor criteria allows a clinical diagnosis of definite endocarditis. The diagnosis of endocarditis is rejected if an alternative diagnosis is established, if symptoms resolve and do not recur with ≤4 days of antibiotic therapy, or if surgery or autopsy after ≤4 days of antimicrobial therapy yields no histologic evidence of endocarditis. Illnesses not classified as definite endocarditis or rejected as such are considered cases of possible infective endocarditis when either one major and one minor criterion or three minor criteria are fulfilled. Requiring some clinical features of endocarditis for classification as possible infective endocarditis increases the specificity of the schema without significantly reducing its sensitivity. Unless there are extenuating circumstances, patients with definite or possible endocarditis are treated as such.
|
THE MODIFIED DUKE CRITERIA FOR THE CLINICAL DIAGNOSIS OF INFECTIVE ENDOCARDITISa |
aDefinite endocarditis is defined by documentation of two major criteria, of one major criterion and three minor criteria, or of five minor criteria. See text for further details. bTransesophageal echocardiography is required for optimal assessment of possible prosthetic valve endocarditis or complicated endocarditis. cValvular disease with stenosis or regurgitation, presence of a prosthetic valve, congenital heart disease including corrected or partially corrected conditions (except isolated atrial septal defect, repaired ventricular septal defect, or closed patent ductus arteriosus), prior endocarditis, or hypertrophic cardiomyopathy. dExcluding single positive cultures for coagulase-negative staphylococci and diphtheroids, which are common culture contaminants, or for organisms that do not cause endocarditis frequently, such as gram-negative bacilli.
Source: Adapted from JS Li et al: Clin Infect Dis 30:633, 2000. With permission from Oxford University Press.
The criteria emphasize bacteremia and echocardiographic findings typical of endocarditis. The requirement for multiple positive blood cultures over time is consistent with the continuous low-density bacteremia characteristic of endocarditis. Among patients with untreated endocarditis who ultimately have a positive blood culture, 95% of all blood cultures are positive. The diagnostic criteria attach significance to the species of organism isolated from blood cultures. To fulfill a major criterion, the isolation of an organism that causes both endocarditis and bacteremia in the absence of endocarditis (e.g., S. aureus, enterococci) must take place repeatedly (i.e., persistent bacteremia) and in the absence of a primary focus of infection. Organisms that rarely cause endocarditis but commonly contaminate blood cultures (e.g., diphtheroids, CoNS) must be isolated repeatedly if their isolation is to serve as a major criterion.
Blood Cultures Isolation of the causative microorganism from blood cultures is critical for diagnosis and for planning treatment. In patients with suspected NVE, PVE, or CIED endocarditis who have not received antibiotics during the prior 2 weeks, three 2-bottle blood culture sets, separated from one another by at least 2 h, should be obtained from different venipuncture sites over 24 h. If the cultures remain negative after 48–72 h, two or three additional blood culture sets should be obtained, and the laboratory should be consulted for advice regarding optimal culture techniques. Pending culture results, empirical antimicrobial therapy should be withheld initially from hemodynamically stable patients with suspected subacute endocarditis, especially those who have received antibiotics within the preceding 2 weeks. Thus, if necessary, additional blood culture sets can be obtained without the confounding effect of empirical treatment. Patients with acute endocarditis or with deteriorating hemodynamics who may require urgent surgery should receive empirical treatment immediately after three sets of blood cultures are obtained over several hours.
Non-Blood-Culture Tests Serologic tests can be used to implicate organisms that are difficult to recover by blood culture: Brucella, Bartonella, Legionella, Chlamydia psittaci, and C. burnetii. Pathogens can also be identified in vegetations by culture, microscopic examination with special stains (i.e., the periodic acid–Schiff stain for T. whipplei), or direct fluorescence antibody techniques and by the use of polymerase chain reaction to recover unique microbial DNA or DNA encoding the 16S or 28S ribosomal unit (16S rRNA or 28S rRNA); sequencing of these DNAs allows identification of bacteria and fungi, respectively.
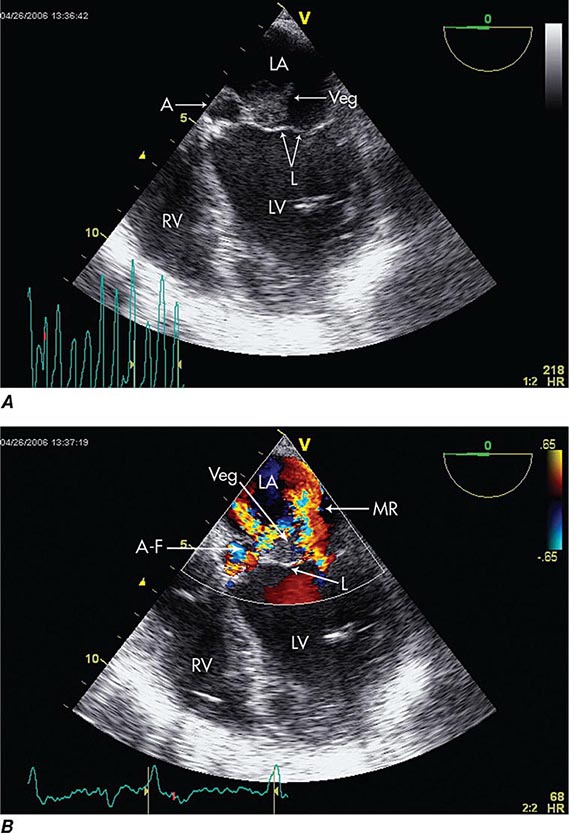
Echocardiography Echocardiography anatomically confirms and measures vegetations, detects intracardiac complications, and assesses cardiac function (Fig. 155-3). Transthoracic echocardiography (TTE) is noninvasive and exceptionally specific; however, it cannot image vegetations <2 mm in diameter, and in 20% of patients it is technically inadequate because of emphysema or body habitus. TTE detects vegetations in 65–80% of patients with definite clinical endocarditis but is not optimal for evaluating prosthetic valves or detecting intracardiac complications. TEE is safe and detects vegetations in >90% of patients with definite endocarditis; nevertheless, initial studies may yield false-negative results in 6–18% of endocarditis patients. When endocarditis is likely, a negative TEE result does not exclude the diagnosis but rather warrants repetition of the study once or twice in 7–10 days. TEE is the optimal method for the diagnosis of PVE, the detection of myocardial abscess, valve perforation, or intracardiac fistulae and for the detection of vegetations in patients with CIED. In patients with CIED and negative blood cultures, a mass adherent to the lead is likely to be a bland thrombosis rather than an infected vegetation.
FIGURE 155-3 Imaging of a mitral valve infected with Staphylococcus aureus by low-esophageal, four-chamber-view, transesophageal echocardiography (TEE). A. Two-dimensional echocardiogram showing a large vegetation with an adjacent echolucent abscess cavity. B. Color-flow Doppler image showing severe mitral regurgitation through both the abscess-fistula and the central valve orifice. A, abscess; A-F, abscess-fistula; L, valve leaflets; LA, left atrium; LV, left ventricle; MR, mitral central valve regurgitation; RV, right ventricle; veg, vegetation. (With permission of Andrew Burger, MD.)
Because S. aureus bacteremia is associated with a high prevalence of endocarditis, routine echocardiographic evaluation (TTE or preferably TEE) is recommended in these patients. Patients with nosocomial S. aureus bacteremia are at increased risk of endocarditis if one or more of the following are present: positive blood cultures for 2–4 days, hemodialysis dependency, a permanent intracardiac device, spine infection, nonvertebral osteomyelitis, or an endocarditis-predisposing valve abnormality. Ideally, these patients should be evaluated with TEE. In patients with none of these findings, the risk of endocarditis is low and evaluation with TTE may suffice.
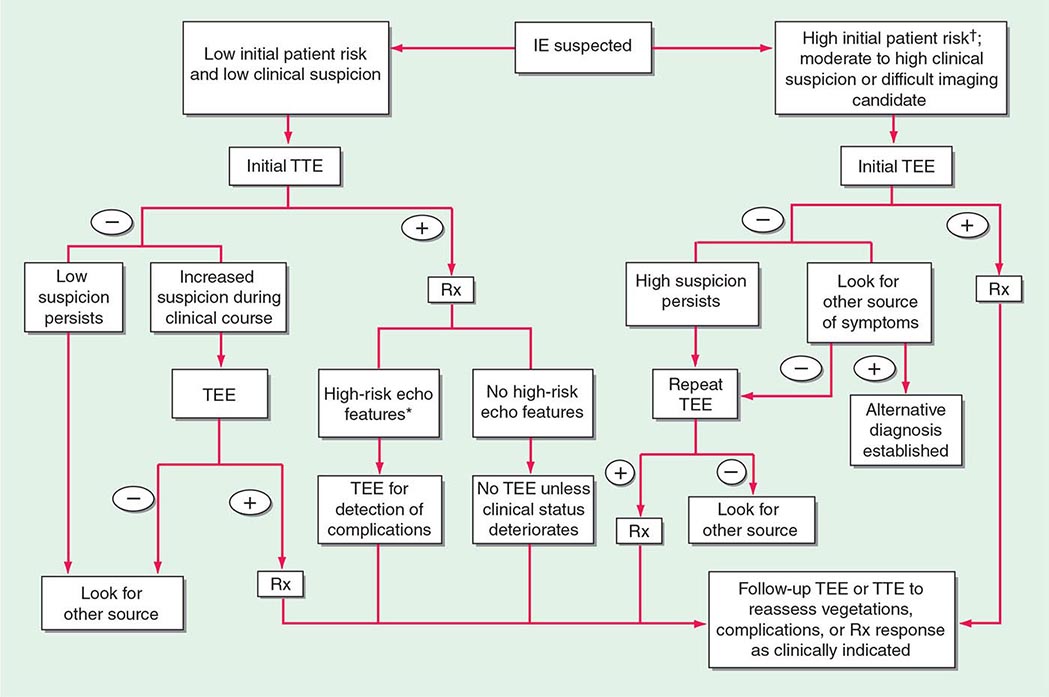
Experts favor echocardiographic evaluation of all patients with a clinical diagnosis of endocarditis; however, the test should not be used to screen patients with a low probability of endocarditis (e.g., patients with unexplained fever). An American Heart Association approach to the use of echocardiography for evaluation of patients with suspected endocarditis is illustrated in (Fig. 155-4).
FIGURE 155-4 The diagnostic use of transesophageal and transtracheal echocardiography (TEE and TTE, respectively). †High initial patient risk for infective endocarditis (IE), as listed in Table 155-8, or evidence of intracardiac complications (new regurgitant murmur, new electrocardiographic conduction changes, or congestive heart failure). *High-risk echocardiographic features include large vegetations, valve insufficiency, paravalvular infection, or ventricular dysfunction. Rx indicates initiation of antibiotic therapy. (Reproduced with permission from Diagnosis and Management of Infective Endocarditis and Its Complications. Circulation 98:2936, 1998. © 1998 American Heart Association.)
Other Studies Many studies that are not diagnostic—i.e., complete blood count, creatinine determination, liver function tests, chest radiography, and electrocardiography—are important in the management of patients with endocarditis. The erythrocyte sedimentation rate, C-reactive protein level, and circulating immune complex titer are commonly increased in endocarditis (Table 155-2). Cardiac catheterization is useful primarily to assess coronary artery patency in older individuals who are to undergo surgery for endocarditis.
|
TREATMENT |
INFECTIVE ENDOCARDITIS |
ANTIMICROBIAL THERAPY
To cure endocarditis, all bacteria in the vegetation must be killed. However, it is difficult to eradicate these bacteria because local host defenses are deficient and because the bacteria are largely nongrowing and metabolically inactive and thus are less easily killed by antibiotics. Accordingly, therapy must be bactericidal and prolonged. Antibiotics are generally given parenterally to achieve serum concentrations that, through passive diffusion, result in effective concentrations in the depths of the vegetation. To select effective therapy requires knowledge of the susceptibility of the causative microorganisms. The decision to initiate treatment empirically must balance the need to establish a microbiologic diagnosis against the potential progression of disease or the need for urgent surgery (see “Blood Cultures,” earlier). Simultaneous infection at other sites (such as the meninges), allergies, end-organ dysfunction, interactions with concomitantly administered medications, and risks of adverse events must be considered in the selection of therapy.
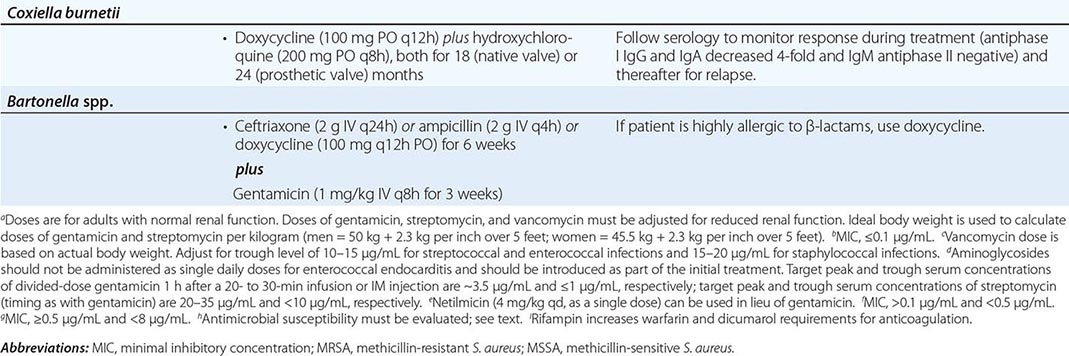
Although given for several weeks longer, the regimens recommended for the treatment of PVE (except that caused by staphylococci) are similar to those used to treat NVE (Table 155-4). Recommended doses and durations of therapy should be followed unless alterations are required by end-organ dysfunction or adverse events.
|
ANTIBIOTIC TREATMENT FOR INFECTIVE ENDOCARDITIS CAUSED BY COMMON ORGANISMSa |
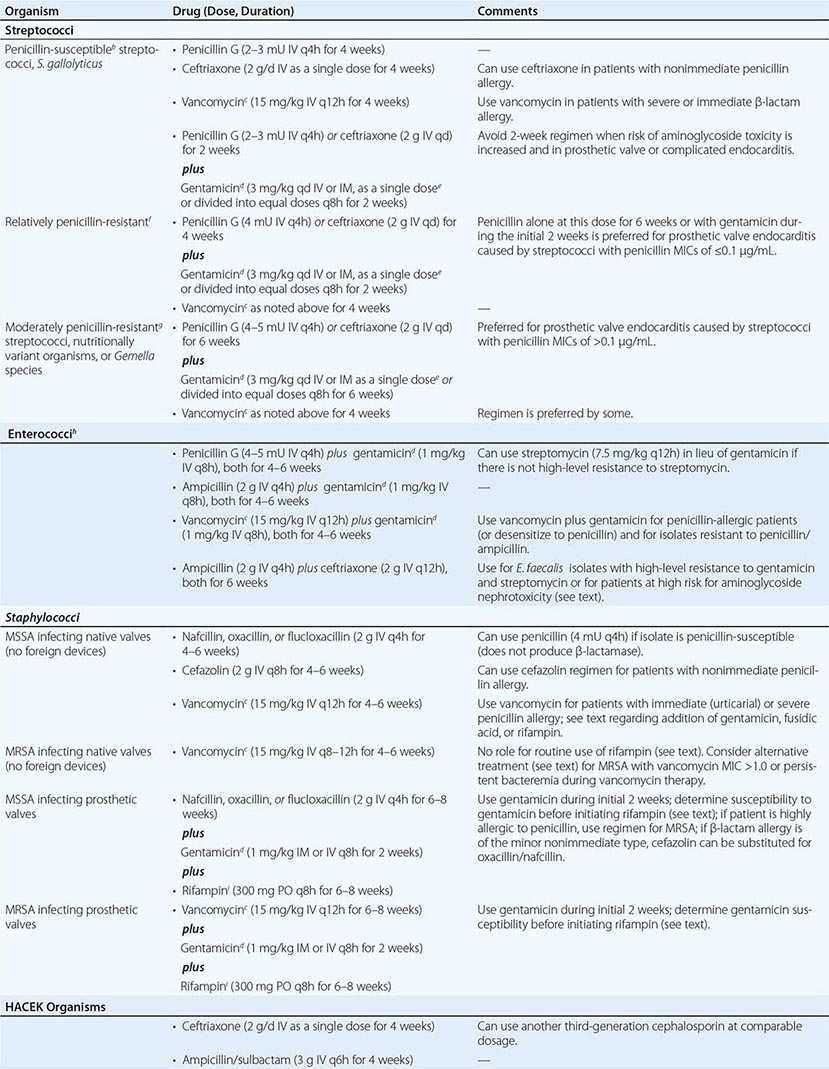
Organism-Specific Therapies • STREPTOCOCCI Optimal therapy for streptococcal endocarditis is based on the minimal inhibitory concentration (MIC) of penicillin for the causative isolate (Table 155-4). The 2-week penicillin/gentamicin or ceftriaxone/gentamicin regimens should not be used to treat PVE or complicated NVE. Caution should be exercised in considering aminoglycoside-containing regimens for the treatment of patients at increased risk for aminoglycoside toxicity. The regimens recommended for relatively penicillin-resistant streptococci are advocated for treatment of group B, C, or G streptococcal endocarditis. Nutritionally variant organisms (Granulicatella or Abiotrophia species) and Gemella species are treated with the regimens for moderately penicillin-resistant streptococci, as is PVE caused by these organisms or by streptococci with a penicillin MIC of >0.1 μg/mL (Table 155-4).
ENTEROCOCCI Enterococci are resistant to oxacillin, nafcillin, and the cephalosporins and are only inhibited—not killed—by penicillin, ampicillin, teicoplanin (not available in the United States), and vancomycin. To kill enterococci requires the synergistic interaction of a cell wall–active antibiotic that is effective at achievable serum concentrations (penicillin, ampicillin, vancomycin, or teicoplanin) and an aminoglycoside (gentamicin or streptomycin) to which the isolate does not exhibit high-level resistance. An isolate’s resistance to cell wall–active agents or its ability to replicate in the presence of gentamicin at ≥500 μg/mL or streptomycin at 1000–2000 μg/mL—a phenomenon called high-level aminoglycoside resistance—indicates that the ineffective antimicrobial agent cannot participate in the interaction to produce killing. High-level resistance to gentamicin predicts that tobramycin, netilmicin, amikacin, and kanamycin also will be ineffective. In fact, even when enterococci are not highly resistant to gentamicin, it is difficult to predict the ability of these other aminoglycosides to participate in synergistic killing; consequently, they should not, in general, be used to treat enterococcal endocarditis. High concentrations of ampicillin plus ceftriaxone or cefotaxime, by expanded binding of penicillin-binding proteins, also kill E. faecalis in vitro and in animal models of endocarditis.
Enterococci must be tested for high-level resistance to streptomycin and gentamicin, β-lactamase production, and susceptibility to penicillin and ampicillin (MIC, <8 μg/mL) and to vancomycin (MIC, ≤4 μg/mL) and teicoplanin (MIC ≤2 μg/ml). If the isolate produces β-lactamase, ampicillin/sulbactam or vancomycin can be used as the cell wall–active component; if the penicillin/ampicillin MIC is ≥8 μg/mL, vancomycin can be considered; and if the vancomycin MIC is ≥8 μg/mL, penicillin or ampicillin can be considered. In the absence of high-level resistance, gentamicin or streptomycin should be used as the aminoglycoside (Table 155-4). Although the dose of gentamicin used to achieve bactericidal synergy in treating enterococcal endocarditis is smaller than that used in standard therapy, nephrotoxicity (or vestibular toxicity with streptomycin) is not uncommon during treatment lasting 4–6 weeks. Regimens in which the aminoglycoside component is given for only 2–3 weeks have been curative and associated with less nephrotoxicity than those using longer courses of gentamicin. Thus regimens wherein gentamicin is administered for only 2–3 weeks are preferred by some.
If there is high-level resistance to both gentamicin and streptomycin, a synergistic bactericidal effect cannot be achieved by the addition of an aminoglycoside; thus no aminoglycoside should be given. Instead, an 8- to 12-week course of a single cell wall–active agent can be considered; for E. faecalis endocarditis, high doses of ampicillin combined with ceftriaxone or cefotaxime are suggested (Table 155-4). Nonrandomized comparative studies suggest that ampicillin-ceftriaxone may be as effective as (and less nephrotoxic than) penicillin or ampicillin plus an aminoglycoside in the treatment of E. faecalis endocarditis. Given the reduced risk of nephrotoxicity with ampicillin-ceftriaxone therapy, this regimen may also be preferred in patients who are at increased risk for aminoglycoside nephrotoxicity.
If the enterococcal isolate is resistant to all of the commonly used agents, suppression of bacteremia followed by surgical treatment should be considered. The role of newer agents potentially active against multidrug-resistant enterococci (quinupristin/dalfopristin [E. faecium only], linezolid, and daptomycin) in the treatment of endocarditis has not been established.
STAPHYLOCOCCI The regimens used to treat staphylococcal endocarditis (Table 155-4) are based not on coagulase production but rather on the presence or absence of a prosthetic valve or foreign device, the native valve(s) involved, and the susceptibility of the isolate to penicillin, methicillin, and vancomycin. All staphylococci are considered penicillin-resistant until shown not to produce penicillinase. Similarly, methicillin resistance has become so prevalent among staphylococci that empirical therapy should be initiated with a regimen that covers methicillin-resistant organisms and should later be revised if the isolate proves to be susceptible to methicillin. The addition of 3–5 days of gentamicin to a β-lactam antibiotic or vancomycin to enhance therapy for native mitral or aortic valve endocarditis has not improved survival rates and may be associated with nephrotoxicity. Neither this addition nor the addition of fusidic acid or rifampin is recommended.
For treatment of endocarditis caused by methicillin-resistant S. aureus (MRSA), vancomycin, dosed to achieve trough concentrations of 15–20 μg/mL, is recommended, with the caveat that this regimen may be associated with nephrotoxicity. Although resistance to vancomycin among staphylococci is rare, reduced vancomycin susceptibility among MRSA strains is increasingly encountered. Isolates with a vancomycin MIC of 4–16 μg/mL have intermediate susceptibility and are referred to as vancomycin-intermediate S. aureus (VISA). Isolates with an MIC of 2 μg/mL may harbor subpopulations with higher MICs. These heteroresistant VISA (hVISA) isolates are not detectable by routine susceptibility testing. Because of the pharmacokinetics/pharmacodynamics of vancomycin, killing of MRSA with a vancomycin MIC of >1.0 μg/mL is unpredictable, even with aggressive vancomycin dosing. Although not approved by the U.S. Food and Drug Administration for this indication, daptomycin (6 mg/kg [or, as some experts prefer, 8–10 mg/kg] IV once daily) has been recommended as an alternative to vancomycin, particularly for left-sided endocarditis caused by VISA, hVISA, or isolates with a vancomycin MIC of >1.0 μg/mL. These isolates should be tested to document daptomycin susceptibility. Daptomycin activity against MRSA—even against some isolates with reduced daptomycin susceptibility—is enhanced by the addition of nafcillin or ceftaroline. Case reports suggest that either the latter combinations or ceftaroline alone (600 mg IV q8h) may be effective in recalcitrant MRSA endocarditis. Nevertheless, a discussion of treatment of endocarditis in which MRSA bacteremia persists despite therapy is beyond the scope of this chapter and requires consultation with an infectious disease specialist. The efficacy of linezolid for left-sided MRSA endocarditis has not been established. Although not widely adopted by other groups, the recommendation of the British Society for Antimicrobial Chemotherapy is that a second drug be added to vancomycin (rifampin) or to daptomycin (rifampin, gentamicin, or linezolid) for the treatment of NVE due to MRSA.
Methicillin-susceptible S. aureus endocarditis that is uncomplicated and limited to the tricuspid or pulmonic valve can often be treated with a 2-week course that combines oxacillin or nafcillin (but not vancomycin) with gentamicin. However, patients with prolonged fever (≥5 days) during therapy or multiple septic pulmonary emboli should receive standard-duration therapy. Vancomycin plus gentamicin for 2 weeks as treatment for right-sided endocarditis caused by MRSA yields suboptimal results; thus this entity is treated for 4 weeks with vancomycin or daptomycin (6 mg/kg as a single daily dose).
Staphylococcal PVE is treated for 6–8 weeks with a multidrug regimen. Rifampin is an essential component because it kills staphylococci that are adherent to foreign material in a biofilm. Two other agents (selected on the basis of susceptibility testing) are combined with rifampin to prevent in vivo emergence of resistance. Because many staphylococci (particularly MRSA and Staphylococcus epidermidis) are resistant to gentamicin, the isolate’s susceptibility to gentamicin or an alternative agent should be established before rifampin treatment is begun. If the isolate is resistant to gentamicin, then another aminoglycoside, a fluoroquinolone (chosen on the basis of susceptibility), or another active agent should be substituted for gentamicin.
OTHER ORGANISMS In the absence of meningitis, endocarditis caused by Streptococcus pneumoniae isolates with a penicillin MIC of ≤1 μg/mL can be treated with IV penicillin (4 million units every 4 h), ceftriaxone (2 g/d as a single dose), or cefotaxime (at a comparable dosage). Infection caused by pneumococcal strains with a penicillin MIC of ≥2 μg/mL should be treated with vancomycin. If meningitis is suspected or present, treatment with vancomycin plus ceftriaxone—at the doses advised for meningitis—should be initiated until susceptibility results are known. Definitive therapy should then be selected on the basis of meningitis breakpoints (penicillin MIC, 0.06 μg/mL; or ceftriaxone MIC, 0.5 μg/mL). P. aeruginosa endocarditis is treated with an antipseudomonal penicillin (ticarcillin or piperacillin) and high doses of tobramycin (8 mg/kg per day in three divided doses). Endocarditis caused by Enterobacteriaceae is treated with a potent β-lactam antibiotic plus an aminoglycoside. Corynebacterial endocarditis is treated with a penicillin plus an aminoglycoside (if the organism is susceptible to the aminoglycoside) or with vancomycin, which is highly bactericidal for most strains. Therapy for Candida endocarditis consists of amphotericin B plus flucytosine and early surgery; long-term (if not indefinite) suppression with an oral azole is advised. Echinocandin treatment of Candida endocarditis has been effective in sporadic cases; nevertheless, the role of echinocandins in this setting has not been established.
Empirical Therapy In designing therapy (largely with antimicrobials and doses from Table 155-4 to target putative microorganisms) to be administered before culture results are known or when cultures are negative, clinical clues (e.g., acute vs. subacute presentation, site of infection, patient’s predispositions) as well as epidemiologic clues to etiology must be considered. Thus empirical therapy for acute endocarditis in an injection drug user should cover MRSA and gram-negative bacilli. Treatment with vancomycin plus gentamicin, initiated immediately after blood samples are obtained for culture, covers these organisms as well as many other potential causes. Similarly, treatment of health care–associated endocarditis must cover MRSA. In the treatment of culture-negative episodes, marantic endocarditis must be excluded and fastidious organisms sought by serologic testing. In the absence of prior antibiotic therapy, it is unlikely that S. aureus, CoNS, or enterococcal infection will present with negative blood cultures; thus, in this situation, recommended empirical therapy targets not these organisms but rather nutritionally variant organisms, the HACEK group, and Bartonella species. Pending the availability of diagnostic data, blood culture–negative subacute NVE is treated with gentamicin plus ampicillin-sulbactam (12 g every 24 h) or ceftriaxone; doxycycline (100 mg twice daily) is added for enhanced Bartonella coverage. For culture-negative PVE, vancomycin, gentamicin, cefepime, and rifampin should be used if the prosthetic valve has been in place for ≤1 year. Empirical therapy for infected prosthetic valves in place for >1 year is similar to that for culture-negative NVE. If cultures may be negative because of confounding by prior antibiotic administration, broader empirical therapy may be indicated, with particular attention to pathogens that are likely to be inhibited by the specific prior therapy.
CIED Endocarditis Antimicrobial therapy for CIED endocarditis is adjunctive to complete device removal. The antimicrobial selected is based on the causative organism and should be used as recommended for NVE (Table 155-4). Bacteremic CIED infection may be complicated by coincident NVE or remote-site infection (e.g., osteomyelitis). A 4- to 6-week course of endocarditis-targeted therapy is recommended for patients with CIED endocarditis and for those with bacteremia that continues during ongoing antimicrobial therapy after device removal. Although S. aureus bacteremia (and persistent CoNS bacteremia) in patients who have a CIED in place is likely—in the absence of another source—to reflect endocarditis and should be managed accordingly, not all bloodstream infections in these patients indicate endocarditis. If evidence suggesting endocarditis is lacking, bloodstream infection due to gram-negative bacilli, streptococci, enterococci, and Candida species may not indicate device infection. However, in the absence of another source, relapse after antimicrobial therapy increases the likelihood of CIED endocarditis and warrants treatment as such.
Outpatient Antimicrobial Therapy Fully compliant, clinically stable patients who are no longer bacteremic, are not febrile, and have no clinical or echocardiographic findings that suggest an impending complication may complete therapy as outpatients. Careful follow-up and a stable home setting are necessary, as are predictable IV access and use of antimicrobial agents that are stable in solution. Recommended regimens should not be compromised to accommodate outpatient therapy.
Monitoring Antimicrobial Therapy Measurement of the serum bactericidal titer—the highest dilution of the patient’s serum during therapy that kills 99.9% of the standard inoculum of the infecting organism—is not recommended for assessment of standard regimens but may be useful for assessment of the treatment of endocarditis caused by unusual organisms. Serum concentrations of aminoglycosides and vancomycin should be monitored and doses adjusted to avoid or address toxicity.
Antibiotic toxicities, including allergic reactions, occur in 25–40% of patients and commonly arise after several weeks of therapy. Blood tests to detect renal, hepatic, and hematologic toxicity should be performed periodically.
Blood cultures should be repeated daily until sterile in patients with endocarditis due to S. aureus or difficult-to-treat organisms, rechecked if there is recrudescent fever, and performed again 4–6 weeks after therapy to document cure. Blood cultures become sterile within 2 days after the start of appropriate therapy when infection is caused by viridans streptococci, enterococci, or HACEK organisms. In S. aureus endocarditis, β-lactam therapy results in sterile cultures in 3–5 days, whereas in MRSA endocarditis, positive cultures may persist for 7–9 days with vancomycin or daptomycin treatment. MRSA bacteremia persisting despite an adequate dosage of vancomycin may indicate infection due to a strain with reduced vancomycin susceptibility and therefore may point to a need for alternative therapy. When fever persists for 7 days despite appropriate antibiotic therapy, patients should be evaluated for paravalvular abscess, extracardiac abscesses (spleen, kidney), or complications (embolic events). Recrudescent fever raises the possibility of these complications but also of drug reactions or complications of hospitalization. Vegetations become smaller with effective therapy; however, 3 months after cure, 50% are unchanged and 25% are slightly larger.
SURGICAL TREATMENT
Intracardiac and central nervous system complications are important causes of morbidity and death due to infective endocarditis. In some cases, effective treatment for these complications requires surgery. The indications for cardiac surgical treatment of endocarditis (Table 155-5) have been derived from observational studies and expert opinion. The strength of individual indications varies; thus the risks and benefits as well as the timing of surgery must be individualized (Table 155-6). From 25% to 40% of patients with left-sided endocarditis undergo cardiac surgery during active infection, with slightly higher surgery rates for PVE than NVE. Intracardiac complications (which are most reliably detected by TEE) and CHF are the most commonly cited indications for surgery. The benefit of surgery has been assessed primarily in studies comparing populations of medically and surgically treated patients matched for the necessity of surgery (indications assessed in studies as propensity), with adjustments for predictors of death (comorbidities) and timing of the surgical intervention. Although study results vary, surgery for currently advised indications appears to convey a significant survival benefit (27–55%) that becomes apparent only with follow-up for ≥6 months. During the initial weeks after surgery, mortality risk may appear increased (disease + surgery–related mortality).
|
INDICATIONS FOR CARDIAC SURGICAL INTERVENTION IN PATIENTS WITH ENDOCARDITIS |
aSurgery must be carefully considered; findings are often combined with other indications to prompt surgery.
|
TIMING OF CARDIAC SURGICAL INTERVENTION IN PATIENTS WITH ENDOCARDITIS |
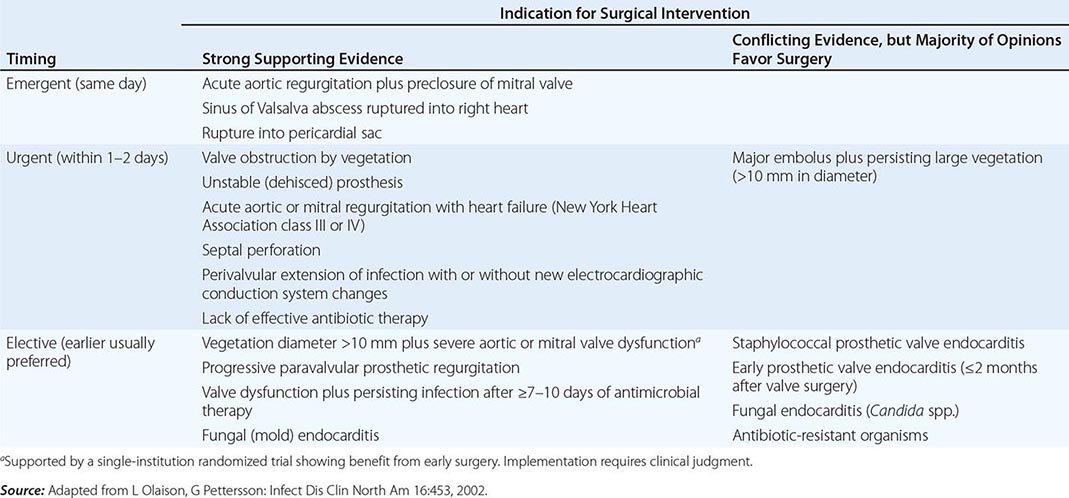
Indications • CONGESTIVE HEART FAILURE Moderate to severe refractory CHF caused by new or worsening valve dysfunction is the major indication for cardiac surgery. At 6 months of follow-up, patients with left-sided endocarditis and moderate to severe heart failure due to valve dysfunction who are treated medically have a 50% mortality rate, while among matched patients who undergo surgery the mortality rate is 15%. The survival benefit with surgery, which is most predictable among patients with the most weighty indications (propensity), is seen in both NVE and PVE. Surgery can relieve functional stenosis due to large vegetations or restore competence to damaged regurgitant valves by repair or replacement.
PERIVALVULAR INFECTION This complication, which is most common with aortic valve infection, occurs in 10–15% of native valve and 45–60% of prosthetic valve infections. It is suggested by persistent unexplained fever during appropriate therapy, new electrocardiographic conduction disturbances, or pericarditis. TEE with color Doppler is the test of choice to detect perivalvular abscesses (sensitivity, ≥85%). For optimal outcome, surgery is required, especially when fever persists, fistulae develop, prostheses are dehisced and unstable, or infection relapses after appropriate treatment. Cardiac rhythm must be monitored since high-grade heart block may require insertion of a pacemaker.
UNCONTROLLED INFECTION Continued positive blood cultures or otherwise-unexplained persistent fevers (in patients with either blood culture–positive or –negative endocarditis) despite optimal antibiotic therapy may reflect uncontrolled infection and may warrant surgery. Surgical treatment is also advised for endocarditis caused by organisms against which effective antimicrobial therapy is lacking (e.g., yeasts, fungi, P. aeruginosa, other highly resistant gram-negative bacilli, Brucella species).
S. AUREUS ENDOCARDITIS The mortality rate for S. aureus PVE exceeds 50% with medical treatment but is reduced to 25% with surgical treatment. In patients with intracardiac complications associated with S. aureus PVE, surgical treatment reduces the mortality rate twentyfold. Surgical treatment should be considered for patients with S. aureus native aortic or mitral valve infection who have TTE-demonstrable vegetations and remain septic during the initial week of therapy. Isolated tricuspid valve endocarditis, even with persistent fever, rarely requires surgery.
PREVENTION OF SYSTEMIC EMBOLI Death and persisting morbidity may result from cerebral or coronary artery emboli. Predicting a high risk of systemic embolization by echocardiographic determination of vegetation size and anatomy does not by itself identify those patients in whom surgery to prevent emboli will result in increased chances of survival. Net benefits from surgery to prevent emboli are most likely when other surgical benefits can be achieved simultaneously—e.g., repair of a moderately dysfunctional valve or debridement of a paravalvular abscess. Only 3.5% of patients undergo surgery solely to prevent systemic emboli. Valve repair, with the consequent avoidance of prosthesis insertion, improves the benefit-to-risk ratio of surgery performed to address vegetations.
CIED ENDOCARDITIS Removal of all hardware is recommended for patients with established CIED infection (pocket or intracardiac lead) or erosion of the device through the skin. Percutaneous lead extraction is preferred. With lead vegetations of >3 cm and the resulting risk of a pulmonary embolus or with retained hardware after attempted percutaneous extraction, surgical removal should be considered. Removal of the infected CIED during the initial hospitalization is associated with increased 30-day and 1-year survival rates over those attained with antibiotic therapy and device retention. If necessary, the CIED can be reimplanted percutaneously or surgically (epicardial leads) at a new site after at least 10–14 days of effective antimicrobial therapy. CIEDs should be removed and replaced subsequently when patients undergo valve surgery for endocarditis.
Timing of Cardiac Surgery With the more life-threatening indications for surgery (valve dysfunction and severe CHF, paravalvular abscess, major prosthesis dehiscence), early surgery—i.e., during the initial week of therapy—is associated with a greater chance of survival than later surgery. With less compelling indications, surgery may reasonably be delayed to allow further treatment as well as improvement in overall health (Table 155-6). After 14 days of recommended antibiotic therapy, excised valves are culture-negative in 99% and 50% of patients with streptococcal and S. aureus endocarditis, respectively. Recrudescent endocarditis on a new implanted prosthetic valve follows surgery for active NVE and PVE in 2% and 6–15% of patients, respectively. These frequencies do not justify the risk of an adverse outcome due to a delay in surgery, particularly in patients with severe heart failure, valve dysfunction, and uncontrolled staphylococcal infections. Delay is justified when infection is controlled and CHF is resolved with medical therapy.
Neurologic complications of endocarditis may be exacerbated as a consequence of cardiac surgery. The risk of neurologic deterioration is related to the type of neurologic complication and the interval between the complication and surgery. Whenever feasible, cardiac surgery should be delayed for 2–3 weeks after a nonhemorrhagic embolic infarction and for 4 weeks after a cerebral hemorrhage. A ruptured mycotic aneurysm should be treated before cardiac surgery.
Antibiotic Therapy after Cardiac Surgery Organisms have been detected on Gram’s stain—or their DNA has been detected by polymerase chain reaction—in excised valves from 45% of patients who have successfully completed the recommended therapy for endocarditis. In only 7% of these patients are the organisms, most of which are unusual and antibiotic resistant, cultured from the valve. Detection of organisms or their DNA does not necessarily indicate antibiotic failure; in fact, relapse of endocarditis after surgery is uncommon. Thus, when valve cultures are negative in uncomplicated NVE caused by susceptible organisms, the duration of preoperative plus postoperative treatment should equal the total duration of recommended therapy, with ~2 weeks of treatment administered after surgery. For endocarditis complicated by paravalvular abscess, partially treated PVE, or cases with culture-positive valves, a full course of therapy should be given postoperatively.
Extracardiac Complications Splenic abscess develops in 3–5% of patients with endocarditis. Effective therapy requires either image-guided percutaneous drainage or splenectomy. Mycotic aneurysms occur in 2–15% of endocarditis patients; one-half of these cases involve the cerebral arteries and present as headaches, focal neurologic symptoms, or hemorrhage. Cerebral aneurysms should be monitored by angiography. Some will resolve with effective antimicrobial therapy, but those that persist, enlarge, or leak should be treated surgically if possible. Extracerebral aneurysms present as local pain, a mass, local ischemia, or bleeding; these aneurysms are treated surgically.
OUTCOME
Factors that can adversely affect outcome include older age, severe comorbid conditions and diabetes, delayed diagnosis, involvement of prosthetic valves or the aortic valve, an invasive (S. aureus) or antibiotic-resistant (P. aeruginosa, yeast) pathogen, intracardiac and major neurologic complications, and an association with health care. Death and poor outcome often are related not to failure of antibiotic therapy but rather to the interactions of comorbidities and endocarditis-related end-organ complications. In developed countries, overall survival rates are 80–85%; however, rates vary considerably among subpopulations of endocarditis patients. Survival rates for patients with NVE caused by viridans streptococci, HACEK organisms, or enterococci (susceptible to synergistic therapy) are 85–90%. For S. aureus NVE in patients who do not inject drugs, survival rates are 55–70%, whereas 85–90% of injection drug users survive this infection. PVE beginning within 2 months of valve replacement results in mortality rates of 40–50%, whereas rates are only 10–20% in later-onset cases.
PREVENTION
To prevent endocarditis (long a goal in clinical practice), past expert committees have supported systemic antibiotic administration prior to many bacteremia-inducing procedures. A reappraisal of the evidence for antibiotic prophylaxis for endocarditis by the American Heart Association and the European Society of Cardiology culminated in guidelines advising its more restrictive use. At best, the benefit of antibiotic prophylaxis is minimal. Most endocarditis cases do not follow a procedure. Although dental treatments have been widely considered to predispose to endocarditis, such infection occurs no more frequently in patients who are undergoing dental treatment than in matched controls who are not. Furthermore, the frequency and magnitude of bacteremia associated with dental procedures and a routine day’s activities (e.g., tooth brushing and flossing) are similar; because dental procedures are infrequent events, exposure of cardiac structures to bacteremic oral-cavity organisms is notably greater from routine daily activities than from dental care. The relation of gastrointestinal and genitourinary procedures to subsequent endocarditis is even more tenuous than that of dental procedures. In addition, cost-effectiveness and cost-benefit estimates suggest that antibiotic prophylaxis represents a poor use of resources.
Nevertheless, studies in animal models suggest that antibiotic prophylaxis may be effective. Thus it is possible that rare cases of endocarditis are prevented. Weighing the potential benefits, potential adverse events, and costs associated with antibiotic prophylaxis, the American Heart Association and the European Society of Cardiology now recommend prophylactic antibiotics (Table 155-7) only for those patients at highest risk for severe morbidity or death from endocarditis (Table 155-8). Maintaining good dental hygiene is essential. Prophylaxis is recommended only when there is manipulation of gingival tissue or the periapical region of the teeth or perforation of the oral mucosa (including surgery on the respiratory tract). Prophylaxis is not advised for patients undergoing gastrointestinal or genitourinary tract procedures. High-risk patients should be treated before or when they undergo procedures on an infected genitourinary tract or on infected skin and soft tissue.
|
ANTIBIOTIC REGIMENS FOR PROPHYLAXIS OF ENDOCARDITIS IN ADULTS WITH HIGH-RISK CARDIAC LESIONSa,b |
aDosing for children: for amoxicillin, ampicillin, cephalexin, or cefadroxil, use 50 mg/kg PO; cefazolin, 25 mg/kg IV; clindamycin, 20 mg/kg PO or 25 mg/kg IV; clarithromycin, 15 mg/kg PO; and vancomycin, 20 mg/kg IV. bFor high-risk lesions, see Table 155-8. Prophylaxis is not advised for other lesions. cDo not use cephalosporins in patients with immediate hypersensitivity (urticaria, angioedema, anaphylaxis) to penicillin.
Source: Table created using the guidelines published by the American Heart Association and the European Society of Cardiology (W Wilson et al: Circulation 116:1736, 2007; and G Habib et al: Eur Heart J 30:2369, 2009).
|
HIGH-RISK CARDIAC LESIONS FOR WHICH ENDOCARDITIS PROPHYLAXIS IS ADVISED BEFORE DENTAL PROCEDURES |
aNot a target population for prophylaxis according to recommendations of the European Society for Cardiology.
Source: Table created using the guidelines published by the American Heart Association and the European Society of Cardiology (W Wilson et al: Circulation 116:1736, 2007; and G Habib et al: Eur Heart J 30:2369, 2009).
In patients with aortic or mitral valve regurgitation or a prosthetic valve, treatment of acute Q fever with doxycycline plus hydroxychloroquine (for doses, see Table 155-4) for 12 months is highly effective in preventing C. burnetii endocarditis.
The National Institute for Health and Clinical Excellence in the United Kingdom has advised discontinuation of all antibiotic prophylaxis for endocarditis. Limited surveillance studies have not detected increased viridans streptococcal endocarditis subsequent to the promulgation of guidelines that are more restrictive or advise no prophylaxis.
156 |
Infections of the Skin, Muscles, and Soft Tissues |
![]() Skin and soft tissue infections occur in all races, all ethnic groups, and all geographic locations, although some have unique geographic niches. In modern times, the frequency and severity of some skin and soft tissue infections have increased for several reasons. First, microbes are rapidly disseminated throughout the world via efficient air travel, acquiring genes for virulence factors and antibiotic resistance. Second, natural disasters, such as earthquakes, tsunamis, tornadoes, and hurricanes, appear to be increasing in frequency, and the injuries sustained during these events commonly cause major skin and soft-tissue damage that predisposes to infection. Third, trauma and casualties resulting from combat and terrorist activities can markedly damage or destroy tissues and provide both endogenous and exogenous pathogens with ready access to deeper structures. Unfortunately, because the marvels of modern medicine may not be available during human-instigated and natural disasters, primary treatment may be delayed and the likelihood of severe infection and death increased.
Skin and soft tissue infections occur in all races, all ethnic groups, and all geographic locations, although some have unique geographic niches. In modern times, the frequency and severity of some skin and soft tissue infections have increased for several reasons. First, microbes are rapidly disseminated throughout the world via efficient air travel, acquiring genes for virulence factors and antibiotic resistance. Second, natural disasters, such as earthquakes, tsunamis, tornadoes, and hurricanes, appear to be increasing in frequency, and the injuries sustained during these events commonly cause major skin and soft-tissue damage that predisposes to infection. Third, trauma and casualties resulting from combat and terrorist activities can markedly damage or destroy tissues and provide both endogenous and exogenous pathogens with ready access to deeper structures. Unfortunately, because the marvels of modern medicine may not be available during human-instigated and natural disasters, primary treatment may be delayed and the likelihood of severe infection and death increased.
ANATOMIC RELATIONSHIPS: CLUES TO THE DIAGNOSIS OF SOFT TISSUE INFECTIONS
Skin and soft tissue infections have been common human afflictions for centuries. However, between 2000 and 2004, hospital admissions for skin and soft tissue infections rose by 27%, a remarkable increase that was attributable largely to the emergence of the USA300 clone of methicillin-resistant Staphylococcus aureus (MRSA). This chapter provides an anatomic approach to understanding the types of soft tissue infections and the diverse microbes responsible.
Protection against infection of the epidermis depends on the mechanical barrier afforded by the stratum corneum, since the epidermis itself is devoid of blood vessels (Fig. 156-1). Disruption of this layer by burns or bites, abrasions, foreign bodies, primary dermatologic disorders (e.g., herpes simplex, varicella, ecthyma gangrenosum), surgery, or vascular or pressure ulcer allows penetration of bacteria to the deeper structures. Similarly, the hair follicle can serve as a portal either for components of the normal flora (e.g., Staphylococcus) or for extrinsic bacteria (e.g., Pseudomonas in hot-tub folliculitis). Intracellular infection of the squamous epithelium with vesicle formation may arise from cutaneous inoculation, as in infection with herpes simplex virus (HSV) type 1; from the dermal capillary plexus, as in varicella and infections due to other viruses associated with viremia; or from cutaneous nerve roots, as in herpes zoster. Bacteria infecting the epidermis, such as Streptococcus pyogenes, may be translocated laterally to deeper structures via lymphatics, an event that results in the rapid superficial spread of erysipelas. Later, engorgement or obstruction of lymphatics causes flaccid edema of the epidermis, another characteristic of erysipelas.
FIGURE 156-1 Structural components of the skin and soft tissue, superficial infections, and infections of the deeper structures. The rich capillary network beneath the dermal papillae plays a key role in the localization of infection and in the development of the acute inflammatory reaction.
The rich plexus of capillaries beneath the dermal papillae provides nutrition to the stratum germinativum, and physiologic responses of this plexus produce important clinical signs and symptoms. For example, infective vasculitis of the plexus results in petechiae, Osler’s nodes, Janeway lesions, and palpable purpura, which, if present, are important clues to the existence of endocarditis (Chap. 155). In addition, metastatic infection within this plexus can result in cutaneous manifestations of disseminated fungal infection (Chap. 240), gonococcal infection (Chap. 181), Salmonella infection (Chap. 190), Pseudomonas infection (i.e., ecthyma gangrenosum; Chap. 189), meningococcemia (Chap. 180), and staphylococcal infection (Chap. 172). The plexus also provides bacteria with access to the circulation, thereby facilitating local spread or bacteremia. The postcapillary venules of this plexus are a prominent site of polymorphonuclear leukocyte sequestration, diapedesis, and chemotaxis to the site of cutaneous infection.
Amplification of these physiologic mechanisms by excessive levels of cytokines or bacterial toxins causes leukostasis, venous occlusion, and pitting edema. Edema with purple bullae, ecchymosis, and cutaneous anesthesia suggests loss of vascular integrity and necessitates exploration of the deeper structures for evidence of necrotizing fasciitis or myonecrosis. An early diagnosis requires a high level of suspicion in instances of unexplained fever and of pain and tenderness in the soft tissue, even in the absence of acute cutaneous inflammation.
Table 156-1 indicates the chapters in which the infections described below are discussed in greater detail. Many of these infections are illustrated in the chapters cited or in Chap. 25e (Atlas of Rashes Associated with Fever).
|
SKIN AND SOFT TISSUE INFECTIONS |
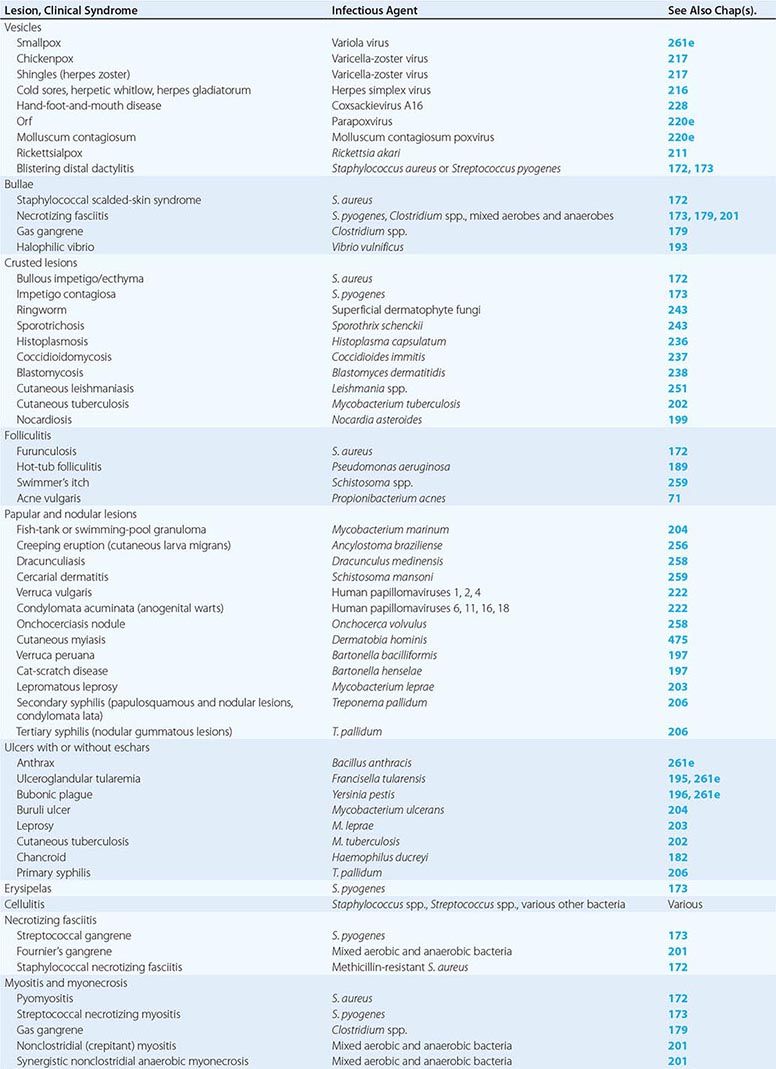
INFECTIONS ASSOCIATED WITH VESICLES
(Table 156-1) Vesicle formation due to infection is caused by viral proliferation within the epidermis. In varicella and variola, viremia precedes the onset of a diffuse centripetal rash that progresses from macules to vesicles, then to pustules, and finally to scabs over the course of 1–2 weeks. Vesicles of varicella have a “dewdrop” appearance and develop in crops randomly about the trunk, extremities, and face over 3–4 days. Herpes zoster occurs in a single dermatome; the appearance of vesicles is preceded by pain for several days. Zoster may occur in persons of any age but is most common among immunosuppressed individuals and elderly patients, whereas most cases of varicella occur in young children. Vesicles due to HSV are found on or around the lips (HSV-1) or genitals (HSV-2) but also may appear on the head and neck of young wrestlers (herpes gladiatorum) or on the digits of health care workers (herpetic whitlow). Recurrent herpes labialis (HSV-1) and herpes genitalis commonly follow primary infection. Coxsackievirus A16 characteristically causes vesicles on the hands, feet, and mouth of children. Orf is caused by a DNA virus related to smallpox virus and infects the fingers of individuals who work around goats and sheep. Molluscum contagiosum virus induces flaccid vesicles on the skin of healthy and immunocompromised individuals. Although variola (smallpox) in nature was eradicated as of 1977, postmillennial terrorist events have renewed interest in this devastating infection (Chap. 261e). Viremia beginning after an incubation period of 12 days is followed by a diffuse maculopapular rash, with rapid evolution to vesicles, pustules, and then scabs. Secondary cases can occur among close contacts.
Rickettsialpox begins after mite-bite inoculation of Rickettsia akari into the skin. A papule with a central vesicle evolves to form a 1- to 2.5-cm painless crusted black eschar with an erythematous halo and proximal adenopathy. While more common in the northeastern United States and the Ukraine in 1940–1950, rickettsialpox has recently been described in Ohio, Arizona, and Utah. Blistering dactylitis is a painful, vesicular, localized S. aureus or group A streptococcal infection of the pulps of the distal digits of the hands.
INFECTIONS ASSOCIATED WITH BULLAE
(Table 156-1) Staphylococcal scalded-skin syndrome (SSSS) in neonates is caused by a toxin (exfoliatin) from phage group II S. aureus. SSSS must be distinguished from toxic epidermal necrolysis (TEN), which occurs primarily in adults, is drug-induced, and is associated with a higher mortality rate. Punch biopsy with frozen section is useful in making this distinction since the cleavage plane is the stratum corneum in SSSS and the stratum germinativum in TEN (Fig. 156-1). Intravenous γ-globulin is a promising treatment for TEN. Necrotizing fasciitis and gas gangrene also induce bulla formation (see “Necrotizing Fasciitis,” below). Halophilic vibrio infection can be as aggressive and fulminant as necrotizing fasciitis; a helpful clue in its diagnosis is a history of exposure to waters of the Gulf of Mexico or the Atlantic seaboard or (in a patient with cirrhosis) the ingestion of raw seafood. The etiologic organism (Vibrio vulnificus) is highly susceptible to tetracycline.
INFECTIONS ASSOCIATED WITH CRUSTED LESIONS
(Table 156-1) Impetigo contagiosa is caused by S. pyogenes, and bullous impetigo is due to S. aureus. Both skin lesions may have an early bullous stage but then appear as thick crusts with a golden-brown color. Epidemics of impetigo caused by MRSA have been reported. Streptococcal lesions are most common among children 2–5 years of age, and epidemics may occur in settings of poor hygiene, particularly among children in lower socioeconomic settings in tropical climates. It is important to recognize impetigo contagiosa because of its relationship to poststreptococcal glomerulonephritis. Rheumatic fever is not a complication of skin infection caused by S. pyogenes. Superficial dermatophyte infection (ringworm) can occur on any skin surface, and skin scrapings with KOH staining are diagnostic. Primary infections with dimorphic fungi such as Blastomyces dermatitidis and Sporothrix schenckii can initially present as crusted skin lesions resembling ringworm. Disseminated infection with Coccidioides immitis can also involve the skin, and biopsy and culture should be performed on crusted lesions in patients from endemic areas. Crusted nodular lesions caused by Mycobacterium chelonei have been described in HIV-seropositive patients. Treatment with clarithromycin looks promising.
FOLLICULITIS
(Table 156-1) Hair follicles serve as portals for a number of bacteria, although S. aureus is the most common cause of localized folliculitis. Sebaceous glands empty into hair follicles and ducts and, if these portals are blocked, form sebaceous cysts that may resemble staphylococcal abscesses or may become secondarily infected. Infection of sweat glands (hidradenitis suppurativa) also can mimic infection of hair follicles, particularly in the axillae. Chronic folliculitis is uncommon except in acne vulgaris, where constituents of the normal flora (e.g., Propionibacterium acnes) may play a role.
Diffuse folliculitis occurs in two settings. Hot-tub folliculitis is caused by Pseudomonas aeruginosa in waters that are insufficiently chlorinated and maintained at temperatures of 37–40°C. Infection is usually self-limited, although bacteremia and shock have been reported. Swimmer’s itch occurs when a skin surface is exposed to water infested with freshwater avian schistosomes. Warm water temperatures and alkaline pH are suitable for mollusks that serve as intermediate hosts between birds and humans. Free-swimming schistosomal cercariae readily penetrate human hair follicles or pores but quickly die and elicit a brisk allergic reaction, causing intense itching and erythema.
PAPULAR AND NODULAR LESIONS
(Table 156-1) Raised lesions of the skin occur in many different forms. Mycobacterium marinum infections of the skin may present as cellulitis or as raised erythematous nodules. Similar lesions caused by Mycobacterium abscessus and M. chelonei have been described among patients undergoing cosmetic laser surgery and tattooing, respectively. Erythematous papules are early manifestations of cat-scratch disease (with lesions developing at the primary site of inoculation of Bartonella henselae) and bacillary angiomatosis (also caused by B. henselae). Raised serpiginous or linear eruptions are characteristic of cutaneous larva migrans, which is caused by burrowing larvae of dog or cat hookworms (Ancylostoma braziliense) and which humans acquire through contact with soil that has been contaminated with dog or cat feces. Similar burrowing raised lesions are present in dracunculiasis caused by migration of the adult female nematode Dracunculus medinensis. Nodules caused by Onchocerca volvulus measure 1–10 cm in diameter and occur mostly in persons bitten by Simulium flies in Africa. The nodules contain the adult worm encased in fibrous tissue. Migration of microfilariae into the eyes may result in blindness. Verruga peruana is caused by Bartonella bacilliformis, which is transmitted to humans by the sandfly Phlebotomus. This condition can take the form of single gigantic lesions (several centimeters in diameter) or multiple small lesions (several millimeters in diameter). Numerous subcutaneous nodules may also be present in cysticercosis caused by larvae of Taenia solium. Multiple erythematous papules develop in schistosomiasis; each represents a cercarial invasion site. Skin nodules as well as thickened subcutaneous tissue are prominent features of lepromatous leprosy. Large nodules or gummas are features of tertiary syphilis, whereas flat papulosquamous lesions are characteristic of secondary syphilis. Human papillomavirus may cause singular warts (verruca vulgaris) or multiple warts in the anogenital area (condylomata acuminata). The latter are major problems in HIV-infected individuals.
ULCERS WITH OR WITHOUT ESCHARS
(Table 156-1) Cutaneous anthrax begins as a pruritic papule, which develops within days into an ulcer with surrounding vesicles and edema and then into an enlarging ulcer with a black eschar. Cutaneous anthrax may cause chronic nonhealing ulcers with an overlying dirty-gray membrane, although lesions may also mimic psoriasis, eczema, or impetigo. Ulceroglandular tularemia may have associated ulcerated skin lesions with painful regional adenopathy. Although buboes are the major cutaneous manifestation of plague, ulcers with eschars, papules, or pustules are also present in 25% of cases.
Mycobacterium ulcerans typically causes chronic skin ulcers on the extremities of individuals living in the tropics. Mycobacterium leprae may be associated with cutaneous ulcerations in patients with lepromatous leprosy related to Lucio’s phenomenon, in which immune-mediated destruction of tissue bearing high concentrations of M. leprae bacilli occurs, usually several months after initiation of effective therapy. Mycobacterium tuberculosis also may cause ulcerations, papules, or erythematous macular lesions of the skin in both immunocompetent and immunocompromised patients.
Decubitus ulcers are due to tissue hypoxemia secondary to pressure-induced vascular insufficiency and may become secondarily infected with components of the skin and gastrointestinal flora, including anaerobes. Ulcerative lesions on the anterior shins may be due to pyoderma gangrenosum, which must be distinguished from similar lesions of infectious etiology by histologic evaluation of biopsy sites. Ulcerated lesions on the genitals may be either painful (chancroid) or painless (primary syphilis).
ERYSIPELAS
(Table 156-1) Erysipelas is due to S. pyogenes and is characterized by an abrupt onset of fiery-red swelling of the face or extremities. The distinctive features of erysipelas are well-defined indurated margins, particularly along the nasolabial fold; rapid progression; and intense pain. Flaccid bullae may develop during the second or third day of illness, but extension to deeper soft tissues is rare. Treatment with penicillin is effective; swelling may progress despite appropriate treatment, although fever, pain, and the intense red color diminish. Desquamation of the involved skin occurs 5–10 days into the illness. Infants and elderly adults are most commonly afflicted, and the severity of systemic toxicity varies.
CELLULITIS
(Table 156-1) Cellulitis is an acute inflammatory condition of the skin that is characterized by localized pain, erythema, swelling, and heat. It may be caused by indigenous flora colonizing the skin and appendages (e.g., S. aureus and S. pyogenes) or by a wide variety of exogenous bacteria. Because the exogenous bacteria involved in cellulitis occupy unique niches in nature, a thorough history (including epidemiologic data) provides important clues to etiology. When there is drainage, an open wound, or an obvious portal of entry, Gram’s stain and culture provide a definitive diagnosis. In the absence of these findings, the bacterial etiology of cellulitis is difficult to establish, and in some cases staphylococcal and streptococcal cellulitis may have similar features. Even with needle aspiration of the leading edge or a punch biopsy of the cellulitis tissue itself, cultures are positive in only 20% of cases. This observation suggests that relatively low numbers of bacteria may cause cellulitis and that the expanding area of erythema within the skin may be a direct effect of extracellular toxins or of the soluble mediators of inflammation elicited by the host.
Bacteria may gain access to the epidermis through cracks in the skin, abrasions, cuts, burns, insect bites, surgical incisions, and IV catheters. Cellulitis caused by S. aureus spreads from a central localized infection, such as an abscess, folliculitis, or an infected foreign body (e.g., a splinter, a prosthetic device, or an IV catheter). MRSA is rapidly replacing methicillin-sensitive S. aureus (MSSA) as a cause of cellulitis in both inpatient and outpatient settings. Cellulitis caused by MSSA or MRSA is usually associated with a focal infection, such as a furuncle, a carbuncle, a surgical wound, or an abscess; the U.S. Food and Drug Administration preferentially refers to these types of infection as purulent cellulitis. In contrast, cellulitis due to S. pyogenes is a more rapidly spreading, diffuse process that is frequently associated with lymphangitis and fever and should be referred to as nonpurulent cellulitis. Recurrent streptococcal cellulitis of the lower extremities may be caused by organisms of group A, C, or G in association with chronic venous stasis or with saphenous venectomy for coronary artery bypass surgery. Streptococci also cause recurrent cellulitis among patients with chronic lymphedema resulting from elephantiasis, lymph node dissection, or Milroy’s disease. Recurrent staphylococcal cutaneous infections are more common among individuals who have eosinophilia and elevated serum levels of IgE (Job’s syndrome) and among nasal carriers of staphylococci. Cellulitis caused by Streptococcus agalactiae (group B Streptococcus) occurs primarily in elderly patients and those with diabetes mellitus or peripheral vascular disease. Haemophilus influenzae typically causes periorbital cellulitis in children in association with sinusitis, otitis media, or epiglottitis. It is unclear whether this form of cellulitis will (like meningitis) become less common as a result of the impressive efficacy of the H. influenzae type b vaccine.
Many other bacteria also cause cellulitis. It is fortunate that these organisms occur in such characteristic settings that a good history provides useful clues to the diagnosis. Cellulitis associated with cat bites and, to a lesser degree, with dog bites is commonly caused by Pasteurella multocida, although in the latter case Staphylococcus intermedius and Capnocytophaga canimorsus also must be considered. Sites of cellulitis and abscesses associated with dog bites and human bites also contain a variety of anaerobic organisms, including Fusobacterium, Bacteroides, aerobic and anaerobic streptococci, and Eikenella corrodens. Pasteurella is notoriously resistant to dicloxacillin and nafcillin but is sensitive to all other β-lactam antimicrobial agents as well as to quinolones, tetracycline, and erythromycin. Ampicillin/clavulanate, ampicillin/sulbactam, and cefoxitin are good choices for the treatment of animal or human bite infections. Aeromonas hydrophila causes aggressive cellulitis in tissues surrounding lacerations sustained in freshwater (lakes, rivers, and streams). This organism remains sensitive to aminoglycosides, fluoroquinolones, chloramphenicol, trimethoprim-sulfamethoxazole, and third-generation cephalosporins; it is resistant to ampicillin, however.
P. aeruginosa causes three types of soft tissue infection: ecthyma gangrenosum in neutropenic patients, hot-tub folliculitis, and cellulitis following penetrating injury. Most commonly, P. aeruginosa is introduced into the deep tissues when a person steps on a nail. Treatment includes surgical inspection and drainage, particularly if the injury also involves bone or joint capsule. Choices for empirical treatment while antimicrobial susceptibility data are awaited include an aminoglycoside, a third-generation cephalosporin (ceftazidime, cefoperazone, or cefotaxime), a semisynthetic penicillin (ticarcillin, mezlocillin, or piperacillin), or a fluoroquinolone (although drugs of the last class are not indicated for the treatment of children <13 years old).
Gram-negative bacillary cellulitis, including that due to P. aeruginosa, is most common among hospitalized, immunocompromised hosts. Cultures and sensitivity tests are critically important in this setting because of multidrug resistance (Chap. 189).
The gram-positive aerobic rod Erysipelothrix rhusiopathiae is most often associated with fish and domestic swine and causes cellulitis primarily in bone renderers and fishmongers. E. rhusiopathiae remains susceptible to most β-lactam antibiotics (including penicillin), erythromycin, clindamycin, tetracycline, and cephalosporins but is resistant to sulfonamides, chloramphenicol, and vancomycin. Its resistance to vancomycin, which is unusual among gram-positive bacteria, is of potential clinical significance since this agent is sometimes used in empirical therapy for skin infection. Fish food containing the water flea Daphnia is sometimes contaminated with M. marinum, which can cause cellulitis or granulomas on skin surfaces exposed to the water in aquariums or injured in swimming pools. Rifampin plus ethambutol has been an effective therapeutic combination in some cases, although no comprehensive studies have been undertaken. In addition, some strains of M. marinum are susceptible to tetracycline or to trimethoprim-sulfamethoxazole.
NECROTIZING FASCIITIS
(Table 156-1) Necrotizing fasciitis, formerly called streptococcal gangrene, may be associated with group A Streptococcus or mixed aerobic–anaerobic bacteria or may occur as a component of gas gangrene caused by Clostridium perfringens. Strains of MRSA that produce the Panton-Valentine leukocidin (PVL) toxin have been reported to cause necrotizing fasciitis. Early diagnosis may be difficult when pain or unexplained fever is the only presenting manifestation. Swelling then develops and is followed by brawny edema and tenderness. With progression, dark-red induration of the epidermis appears, along with bullae filled with blue or purple fluid. Later the skin becomes friable and takes on a bluish, maroon, or black color. By this stage, thrombosis of blood vessels in the dermal papillae (Fig. 156-1) is extensive. Extension of infection to the level of the deep fascia causes this tissue to take on a brownish-gray appearance. Rapid spread occurs along fascial planes, through venous channels and lymphatics. Patients in the later stages are toxic and frequently manifest shock and multiorgan failure.
Necrotizing fasciitis caused by mixed aerobic-anaerobic bacteria begins with a breach in the integrity of a mucous membrane barrier, such as the mucosa of the gastrointestinal or genitourinary tract. The portal can be a malignancy, a diverticulum, a hemorrhoid, an anal fissure, or a urethral tear. Other predisposing factors include peripheral vascular disease, diabetes mellitus, surgery, and penetrating injury to the abdomen. Leakage into the perineal area results in a syndrome called Fournier’s gangrene, characterized by massive swelling of the scrotum and penis with extension into the perineum or the abdominal wall and the legs.
Necrotizing fasciitis caused by S. pyogenes has increased in frequency and severity since 1985. There are two distinct clinical presentations: those with no portal of entry and those with a defined portal of entry. Infections in the first category often begin deep at the site of a nonpenetrating minor trauma, such as a bruise or a muscle strain. Seeding of the site via transient bacteremia is likely, although most patients deny antecedent streptococcal infection. The affected patients present with only severe pain and fever. Late in the course, the classic signs of necrotizing fasciitis, such as purple (violaceous) bullae, skin sloughing, and progressive toxicity, develop. In infections of the second type, S. pyogenes may reach the deep fascia from a site of cutaneous infection or penetrating trauma. These patients have early signs of superficial skin infection with progression to necrotizing fasciitis. In either case, toxicity is severe, and renal impairment may precede the development of shock. In 20–40% of cases, myositis occurs concomitantly, and, as in gas gangrene (see below), serum creatine phosphokinase levels may be markedly elevated. Necrotizing fasciitis due to mixed aerobic-anaerobic bacteria may be associated with gas in deep tissue, but gas usually is not present when the cause is S. pyogenes or MRSA. Prompt surgical exploration down to the deep fascia and muscle is essential. Necrotic tissue must be surgically removed, and Gram’s staining and culture of excised tissue are useful in establishing whether group A streptococci, mixed aerobic-anaerobic bacteria, MRSA, or Clostridium species are present (see “Treatment,” below).
MYOSITIS AND MYONECROSIS
(Table 156-1) Muscle involvement can occur with viral infection (e.g., influenza, dengue, or coxsackievirus B infection) or parasitic invasion (e.g., trichinellosis, cysticercosis, or toxoplasmosis). Although myalgia develops in most of these infections, severe muscle pain is the hallmark of pleurodynia (coxsackievirus B), trichinellosis, and bacterial infection. Acute rhabdomyolysis predictably occurs with clostridial and streptococcal myositis but may also be associated with influenza virus, echovirus, coxsackievirus, Epstein-Barr virus, and Legionella infections.
Pyomyositis is usually due to S. aureus, is common in tropical areas, and generally has no known portal of entry. Cases of pyomyositis caused by MRSA producing the PVL toxin have been described among children in the United States. Muscle infection begins at the exact site of blunt trauma or muscle strain. Infection remains localized, and shock does not develop unless organisms produce toxic shock syndrome toxin 1 or certain enterotoxins and the patient lacks antibodies to the toxin produced by the infecting organisms. In contrast, S. pyogenes may induce primary myositis (referred to as streptococcal necrotizing myositis) in association with severe systemic toxicity. Myonecrosis occurs concomitantly with necrotizing fasciitis in ~50% of cases. Both are part of the streptococcal toxic shock syndrome.
Gas gangrene usually follows severe penetrating injuries that result in interruption of the blood supply and introduction of soil into wounds. Such cases of traumatic gangrene are usually caused by the clostridial species C. perfringens, C. septicum, and C. histolyticum. Rarely, latent or recurrent gangrene can occur years after penetrating trauma; dormant spores that reside at the site of previous injury are most likely responsible. Spontaneous nontraumatic gangrene among patients with neutropenia, gastrointestinal malignancy, diverticulosis, or recent radiation therapy to the abdomen is caused by several clostridial species, of which C. septicum is the most commonly involved. The tolerance of this anaerobe to oxygen probably explains why it can initiate infection spontaneously in normal tissue anywhere in the body.
Gas gangrene of the uterus, especially that due to Clostridium sordellii, historically occurred as a consequence of illegal or self-induced abortion and nowadays also follows spontaneous abortion, vaginal delivery, and cesarean section. C. sordellii has also been implicated in medically induced abortion. Postpartum C. sordellii infections in young, previously healthy women present as a unique clinical picture: little or no fever, lack of a purulent discharge, refractory hypotension, extensive peripheral edema and effusions, hemoconcentration, and a markedly elevated white blood cell count. The infection is almost uniformly fatal, with death ensuing rapidly. C. sordellii and C. novyi have also been associated with cutaneous injection of black tar heroin; mortality rates are lower among the affected individuals, probably because their aggressive injection-site infections are readily apparent and diagnosis is therefore prompt.
Synergistic nonclostridial anaerobic myonecrosis, also known as necrotizing cutaneous myositis and synergistic necrotizing cellulitis, is a variant of necrotizing fasciitis caused by mixed aerobic and anaerobic bacteria with the exclusion of clostridial organisms (see “Necrotizing Fasciitis,” above).
DIAGNOSIS
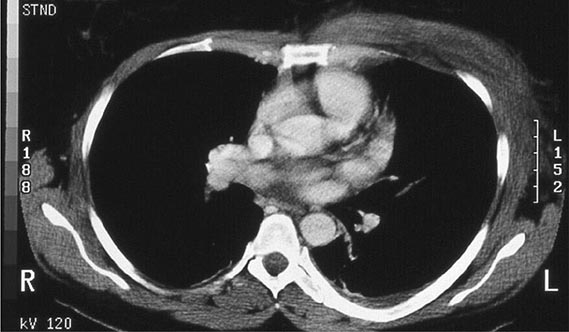
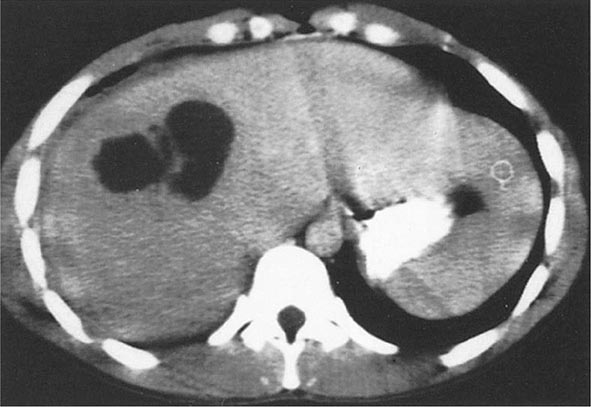
This chapter emphasizes the physical appearance and location of lesions within the soft tissues as important diagnostic clues. Other crucial considerations in narrowing the differential diagnosis are the temporal progression of the lesions as well as the patient’s travel history, animal exposure or bite history, age, underlying disease status, and lifestyle. However, even the astute clinician may find it challenging to diagnose all infections of the soft tissues by history and inspection alone. Soft tissue radiography, CT (Fig. 156-2), and MRI may be useful in determining the depth of infection and should be performed when the patient has rapidly progressing lesions or evidence of a systemic inflammatory response syndrome. These tests are particularly valuable for defining a localized abscess or detecting gas in tissue. Unfortunately, they may reveal only soft tissue swelling and thus are not specific for fulminant infections such as necrotizing fasciitis or myonecrosis caused by group A Streptococcus (Fig. 156-2), where gas is not found in lesions.
FIGURE 156-2 CT showing edema and inflammation of the left chest wall in a patient with necrotizing fasciitis and myonecrosis caused by group A Streptococcus.
Aspiration of the leading edge or punch biopsy with frozen section may be helpful if the results of imaging tests are positive, but false-negative results occur in ~80% of cases. There is some evidence that aspiration alone may be superior to injection and aspiration with normal saline. Frozen sections are especially useful in distinguishing SSSS from TEN and are quite valuable in cases of necrotizing fasciitis. Open surgical inspection, with debridement as indicated, is clearly the best way to determine the extent and severity of infection and to obtain material for Gram’s staining and culture. Such an aggressive approach is important and may be lifesaving if undertaken early in the course of fulminant infections where there is evidence of systemic toxicity.
|
INFECTIONS OF THE SKIN, MUSCLES, AND SOFT TISSUES |
A full description of the treatment of all the clinical entities described herein is beyond the scope of this chapter. As a guide to the clinician in selecting appropriate treatment, the antimicrobial agents useful in the most common and the most fulminant cutaneous infections are listed in Table 156-2.
|
TREATMENT OF COMMON INFECTIONS OF THE SKIN |
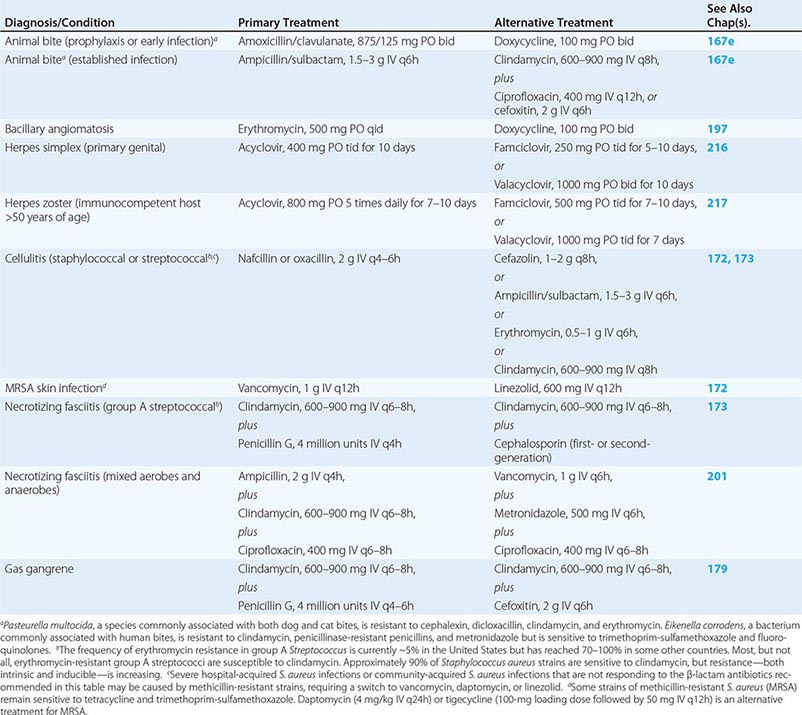
Furuncles, carbuncles, and abscesses caused by MRSA and MSSA are common, and their treatment depends upon the size of the lesion. Furuncles <2.5 cm in diameter are usually treated with moist heat. Those that are larger (4.5 cm of erythema and induration) require surgical drainage, and the occurrence of these larger lesions in association with fever, chills, or leukocytosis requires both drainage and antibiotic treatment. A study in children demonstrated that surgical drainage of abscesses (mean diameter, 3.8 cm) was as effective when used alone as when combined with trimethoprim-sulfamethoxazole treatment. However, the rate of recurrence of new lesions was lower in the group undergoing both drainage and antibiotic treatment.
Early and aggressive surgical exploration is essential in cases of suspected necrotizing fasciitis, myositis, or gangrene in order to (1) visualize the deep structures, (2) remove necrotic tissue, (3) reduce compartment pressure, and (4) obtain suitable material for Gram’s staining and for aerobic and anaerobic cultures. Appropriate empirical antibiotic treatment for mixed aerobic–anaerobic infections could consist of ampicillin/sulbactam, cefoxitin, or the following combination: (1) clindamycin (600–900 mg IV every 8 h) or metronidazole (500 mg every 6 h) plus (2) ampicillin or ampicillin/sulbactam (1.5–3 g IV every 6 h) plus (3) gentamicin (1–1.5 mg/kg every 8 h). Group A streptococcal and clostridial infection of the fascia and/or muscle carries a mortality rate of 20–50% with penicillin treatment. In experimental models of streptococcal and clostridial necrotizing fasciitis/myositis, clindamycin has exhibited markedly superior efficacy, but no comparative clinical trials have been performed. A retrospective study of children with invasive group A streptococcal infection demonstrated higher survival rates with clindamycin treatment than with β-lactam antibiotic therapy. Hyperbaric oxygen treatment also may be useful in gas gangrene due to clostridial species. Antibiotic treatment should be continued until all signs of systemic toxicity have resolved, all devitalized tissue has been removed, and granulation tissue has developed (Chaps. 173, 179, and 201).
In summary, infections of the skin and soft tissues are diverse in presentation and severity and offer a great challenge to the clinician. This chapter provides an approach to diagnosis and understanding of the pathophysiologic mechanisms involved in these infections. More in-depth information is found in chapters on specific infections.
157 |
Infectious Arthritis |
Although Staphylococcus aureus, Neisseria gonorrhoeae, and other bacteria are the most common causes of infectious arthritis, various mycobacteria, spirochetes, fungi, and viruses also infect joints (Table 157-1). Since acute bacterial infection can destroy articular cartilage rapidly, all inflamed joints must be evaluated without delay to exclude noninfectious processes and determine appropriate antimicrobial therapy and drainage procedures. For more detailed information on infectious arthritis caused by specific organisms, the reader is referred to the chapters on those organisms.
|
DIFFERENTIAL DIAGNOSIS OF ARTHRITIS SYNDROMES |
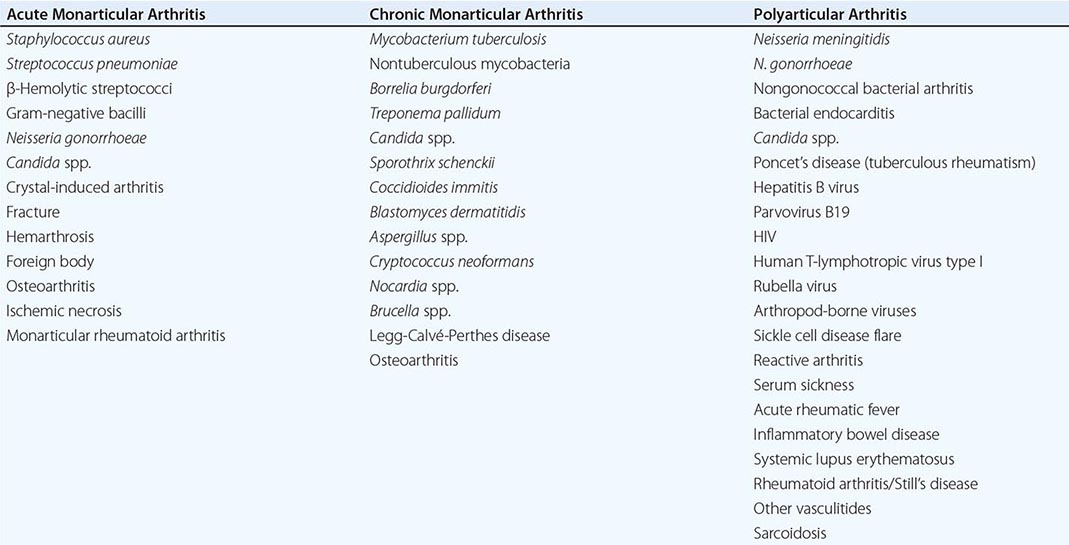
Acute bacterial infection typically involves a single joint or a few joints. Subacute or chronic monarthritis or oligoarthritis suggests mycobacterial or fungal infection; episodic inflammation is seen in syphilis, Lyme disease, and the reactive arthritis that follows enteric infections and chlamydial urethritis. Acute polyarticular inflammation occurs as an immunologic reaction during the course of endocarditis, rheumatic fever, disseminated neisserial infection, and acute hepatitis B. Bacteria and viruses occasionally infect multiple joints, the former most commonly in persons with rheumatoid arthritis.
ACUTE BACTERIAL ARTHRITIS
PATHOGENESIS
Bacteria enter the joint from the bloodstream; from a contiguous site of infection in bone or soft tissue; or by direct inoculation during surgery, injection, animal or human bite, or trauma. In hematogenous infection, bacteria escape from synovial capillaries, which have no limiting basement membrane, and within hours provoke neutrophilic infiltration of the synovium. Neutrophils and bacteria enter the joint space; later, bacteria adhere to articular cartilage. Degradation of cartilage begins within 48 h as a result of increased intraarticular pressure, release of proteases and cytokines from chondrocytes and synovial macrophages, and invasion of the cartilage by bacteria and inflammatory cells. Histologic studies reveal bacteria lining the synovium and cartilage as well as abscesses extending into the synovium, cartilage, and—in severe cases—subchondral bone. Synovial proliferation results in the formation of a pannus over the cartilage, and thrombosis of inflamed synovial vessels develops. Bacterial factors that appear important in the pathogenesis of infective arthritis include various surface-associated adhesins in S. aureus that permit adherence to cartilage and endotoxins that promote chondrocyte-mediated breakdown of cartilage.
MICROBIOLOGY
The hematogenous route of infection is the most common route in all age groups, and nearly every bacterial pathogen is capable of causing septic arthritis. In infants, group B streptococci, gram-negative enteric bacilli, and S. aureus are the most common pathogens. Since the advent of the Haemophilus influenzae vaccine, the predominant causes among children <5 years of age have been S. aureus, Streptococcus pyogenes (group A Streptococcus), and (in some centers) Kingella kingae. Among young adults and adolescents, N. gonorrhoeae is the most commonly implicated organism. S. aureus accounts for most nongonococcal isolates in adults of all ages; gram-negative bacilli, pneumococci, and β-hemolytic streptococci—particularly groups A and B but also groups C, G, and F—are involved in up to one-third of cases in older adults, especially those with underlying comorbid illnesses.
Infections after surgical procedures or penetrating injuries are due most often to S. aureus and occasionally to other gram-positive bacteria or gram-negative bacilli. Infections with coagulase-negative staphylococci are unusual except after the implantation of prosthetic joints or arthroscopy. Anaerobic organisms, often in association with aerobic or facultative bacteria, are found after human bites and when decubitus ulcers or intraabdominal abscesses spread into adjacent joints. Polymicrobial infections complicate traumatic injuries with extensive contamination. Bites and scratches from cats and other animals may introduce Pasteurella multocida or Bartonella henselae into joints either directly or hematogenously, and bites from humans may introduce Eikenella corrodens or other components of the oral flora. Penetration of a sharp object through a shoe is associated with Pseudomonas aeruginosa arthritis in the foot.
NONGONOCOCCAL BACTERIAL ARTHRITIS
Epidemiology Although hematogenous infections with virulent organisms such as S. aureus, H. influenzae, and pyogenic streptococci occur in healthy persons, there is an underlying host predisposition in many cases of septic arthritis. Patients with rheumatoid arthritis have the highest incidence of infective arthritis (most often secondary to S. aureus) because of chronically inflamed joints; glucocorticoid therapy; and frequent breakdown of rheumatoid nodules, vasculitic ulcers, and skin overlying deformed joints. Diabetes mellitus, glucocorticoid therapy, hemodialysis, and malignancy all carry an increased risk of infection with S. aureus and gram-negative bacilli. Tumor necrosis factor inhibitors (e.g., etanercept, infliximab), which increasingly are used for the treatment of rheumatoid arthritis, predispose to mycobacterial infections and possibly to other pyogenic bacterial infections and could be associated with septic arthritis in this population. Pneumococcal infections complicate alcoholism, deficiencies of humoral immunity, and hemoglobinopathies. Pneumococci, Salmonella species, and H. influenzae cause septic arthritis in persons infected with HIV. Persons with primary immunoglobulin deficiency are at risk for mycoplasmal arthritis, which results in permanent joint damage if tetracycline and replacement therapy with IV immunoglobulin are not administered promptly. IV drug users acquire staphylococcal and streptococcal infections from their own flora and acquire pseudomonal and other gram-negative infections from drugs and injection paraphernalia.
Clinical Manifestations Some 90% of patients present with involvement of a single joint—most commonly the knee; less frequently the hip; and still less often the shoulder, wrist, or elbow. Small joints of the hands and feet are more likely to be affected after direct inoculation or a bite. Among IV drug users, infections of the spine, sacroiliac joints, and sternoclavicular joints (Fig. 157-1) are more common than infections of the appendicular skeleton. Polyarticular infection is most common among patients with rheumatoid arthritis and may resemble a flare of the underlying disease.
FIGURE 157-1 Acute septic arthritis of the sternoclavicular joint. A man in his forties with a history of cirrhosis presented with a new onset of fever and lower neck pain. He had no history of IV drug use or previous catheter placement. Jaundice and a painful swollen area over his left sternoclavicular joint were evident on physical examination. Cultures of blood drawn at admission grew group B Streptococcus. The patient recovered after treatment with IV penicillin. (Courtesy of Francisco M. Marty, MD, Brigham and Women’s Hospital, Boston; with permission.)
The usual presentation consists of moderate to severe pain that is uniform around the joint, effusion, muscle spasm, and decreased range of motion. Fever in the range of 38.3–38.9°C (101–102°F) and sometimes higher is common but may not be present, especially in persons with rheumatoid arthritis, renal or hepatic insufficiency, or conditions requiring immunosuppressive therapy. The inflamed, swollen joint is usually evident on examination except in the case of a deeply situated joint such as the hip, shoulder, or sacroiliac joint. Cellulitis, bursitis, and acute osteomyelitis, which may produce a similar clinical picture, should be distinguished from septic arthritis by their greater range of motion and less-than-circumferential swelling. A focus of extraarticular infection, such as a boil or pneumonia, should be sought. Peripheral-blood leukocytosis with a left shift and elevation of the erythrocyte sedimentation rate or C-reactive protein level are common.
Plain radiographs show evidence of soft-tissue swelling, joint-space widening, and displacement of tissue planes by the distended capsule. Narrowing of the joint space and bony erosions indicate advanced infection and a poor prognosis. Ultrasound is useful for detecting effusions in the hip, and CT or MRI can demonstrate infections of the sacroiliac joint, the sternoclavicular joint, and the spine very well.
Laboratory Findings Specimens of peripheral blood and synovial fluid should be obtained before antibiotics are administered. Blood cultures are positive in up to 50–70% of S. aureus infections but are less frequently positive in infections due to other organisms. The synovial fluid is turbid, serosanguineous, or frankly purulent. Gram-stained smears confirm the presence of large numbers of neutrophils. Levels of total protein and lactate dehydrogenase in synovial fluid are elevated, and the glucose level is depressed; however, these findings are not specific for infection, and measurement of these levels is not necessary for diagnosis. The synovial fluid should be examined for crystals, because gout and pseudogout can resemble septic arthritis clinically, and infection and crystal-induced disease occasionally occur together. Organisms are seen on synovial fluid smears in nearly three-quarters of infections with S. aureus and streptococci and in 30–50% of infections due to gram-negative and other bacteria. Cultures of synovial fluid are positive in >90% of cases. Inoculation of synovial fluid into bottles containing liquid media for blood cultures increases the yield of a culture, especially if the pathogen is a fastidious organism or the patient is taking an antibiotic. NAA-based assays for bacterial DNA, when available, can be useful for the diagnosis of partially treated or culture-negative bacterial arthritis.
|
TREATMENT |
NONGONOCOCCAL BACTERIAL ARTHRITIS |
Prompt administration of systemic antibiotics and drainage of the involved joint can prevent destruction of cartilage, postinfectious degenerative arthritis, joint instability, or deformity. Once samples of blood and synovial fluid have been obtained for culture, empirical antibiotics should be given that are directed against the bacteria visualized on smears or the pathogens that are likely in light of the patient’s age and risk factors. Initial therapy should consist of IV administration of bactericidal agents; direct instillation of antibiotics into the joint is not necessary to achieve adequate levels in synovial fluid and tissue. An IV third-generation cephalosporin such as cefotaxime (1 g every 8 h) or ceftriaxone (1–2 g every 24 h) provides adequate empirical coverage for most community-acquired infections in adults when smears show no organisms. IV vancomycin (1 g every 12 h) is used if there are gram-positive cocci on the smear. If methicillin-resistant S. aureus is an unlikely pathogen (e.g., when it is not widespread in the community), either oxacillin or nafcillin (2 g every 4 h) should be given. In addition, an aminoglycoside or third-generation cephalosporin should be given to IV drug users and to other patients in whom P. aeruginosa may be the responsible agent.
Definitive therapy is based on the identity and antibiotic susceptibility of the bacteria isolated in culture. Infections due to staphylococci are treated with oxacillin, nafcillin, or vancomycin for 4 weeks. Pneumococcal and streptococcal infections due to penicillin-susceptible organisms respond to 2 weeks of therapy with penicillin G (2 million units IV every 4 h); infections caused by H. influenzae and by strains of Streptococcus pneumoniae that are resistant to penicillin are treated with cefotaxime or ceftriaxone for 2 weeks. Most enteric gram-negative infections can be cured in 3–4 weeks by a second- or third-generation cephalosporin given IV or by a fluoroquinolone such as levofloxacin (500 mg IV or PO every 24 h). P. aeruginosa infection should be treated for at least 2 weeks with a combination regimen composed of an aminoglycoside plus either an extended-spectrum penicillin such as mezlocillin (3 g IV every 4 h) or an antipseudomonal cephalosporin such as ceftazidime (1 g IV every 8 h). If tolerated, this regimen is continued for an additional 2 weeks; alternatively, a fluoroquinolone such as ciprofloxacin (750 mg PO twice daily) is given by itself or with the penicillin or cephalosporin in place of the aminoglycoside.
Timely drainage of pus and necrotic debris from the infected joint is required for a favorable outcome. Needle aspiration of readily accessible joints such as the knee may be adequate if loculations or particulate matter in the joint does not prevent its thorough decompression. Arthroscopic drainage and lavage may be employed initially or within several days if repeated needle aspiration fails to relieve symptoms, decrease the volume of the effusion and the synovial white cell count, and clear bacteria from smears and cultures. In some cases, arthrotomy is necessary to remove loculations and debride infected synovium, cartilage, or bone. Septic arthritis of the hip is best managed with arthrotomy, particularly in young children, in whom infection threatens the viability of the femoral head. Septic joints do not require immobilization except for pain control before symptoms are alleviated by treatment. Weight bearing should be avoided until signs of inflammation have subsided, but frequent passive motion of the joint is indicated to maintain full mobility. Although addition of glucocorticoids to antibiotic treatment improves the outcome of S. aureus arthritis in experimental animals, no clinical trials have evaluated this approach in humans.
GONOCOCCAL ARTHRITIS
Epidemiology Although its incidence has declined in recent years, gonococcal arthritis (Chap. 181) has accounted for up to 70% of episodes of infectious arthritis in persons <40 years of age in the United States. Arthritis due to N. gonorrhoeae is a consequence of bacteremia arising from gonococcal infection or, more frequently, from asymptomatic gonococcal mucosal colonization of the urethra, cervix, or pharynx. Women are at greatest risk during menses and during pregnancy and overall are two to three times more likely than men to develop disseminated gonococcal infection (DGI) and arthritis. Persons with complement deficiencies, especially of the terminal components, are prone to recurrent episodes of gonococcemia. Strains of gonococci that are most likely to cause DGI include those which produce transparent colonies in culture, have the type IA outer-membrane protein, or are of the AUH-auxotroph type.
Clinical Manifestations and Laboratory Findings The most common manifestation of DGI is a syndrome of fever, chills, rash, and articular symptoms. Small numbers of papules that progress to hemorrhagic pustules develop on the trunk and the extensor surfaces of the distal extremities. Migratory arthritis and tenosynovitis of the knees, hands, wrists, feet, and ankles are prominent. The cutaneous lesions and articular findings are believed to be the consequence of an immune reaction to circulating gonococci and immune-complex deposition in tissues. Thus, cultures of synovial fluid are consistently negative, and blood cultures are positive in fewer than 45% of patients. Synovial fluid may be difficult to obtain from inflamed joints and usually contains only 10,000–20,000 leukocytes/μL.
True gonococcal septic arthritis is less common than the DGI syndrome and always follows DGI, which is unrecognized in one-third of patients. A single joint such as the hip, knee, ankle, or wrist is usually involved. Synovial fluid, which contains >50,000 leukocytes/μL, can be obtained with ease; the gonococcus is evident only occasionally in Gram-stained smears, and cultures of synovial fluid are positive in fewer than 40% of cases. Blood cultures are almost always negative.
Because it is difficult to isolate gonococci from synovial fluid and blood, specimens for culture should be obtained from potentially infected mucosal sites. NAA-based urine tests also may be positive. Cultures and Gram-stained smears of skin lesions are occasionally positive. All specimens for culture should be plated onto Thayer-Martin agar directly or in special transport media at the bedside and transferred promptly to the microbiology laboratory in an atmosphere of 5% CO2, as generated in a candle jar. NAA-based assays are extremely sensitive in detecting gonococcal DNA in synovial fluid. A dramatic alleviation of symptoms within 12–24 h after the initiation of appropriate antibiotic therapy supports a clinical diagnosis of the DGI syndrome if cultures are negative.
|
TREATMENT |
GONOCOCCAL ARTHRITIS |
Initial treatment consists of ceftriaxone (1 g IV or IM every 24 h) to cover possible penicillin-resistant organisms. Once local and systemic signs are clearly resolving, the 7-day course of therapy can be completed with an oral fluoroquinolone such as ciprofloxacin (500 mg twice daily) if the organism is known to be susceptible. If penicillin-susceptible organisms are isolated, amoxicillin (500 mg three times daily) may be used. Suppurative arthritis usually responds to needle aspiration of involved joints and 7–14 days of antibiotic treatment. Arthroscopic lavage or arthrotomy is rarely required. Patients with DGI should be treated for Chlamydia trachomatis infection unless this infection is ruled out by appropriate testing.
It is noteworthy that arthritis symptoms similar to those seen in DGI occur in meningococcemia. A dermatitis-arthritis syndrome, purulent monarthritis, and reactive polyarthritis have been described. All respond to treatment with IV penicillin.
SPIROCHETAL ARTHRITIS
LYME DISEASE
Lyme disease (Chap. 210) due to infection with the spirochete Borrelia burgdorferi causes arthritis in up to 60% of persons who are not treated. Intermittent arthralgias and myalgias—but not arthritis—occur within days or weeks of inoculation of the spirochete by the Ixodes tick. Later, there are three patterns of joint disease: (1) Fifty percent of untreated persons experience intermittent episodes of monarthritis or oligoarthritis involving the knee and/or other large joints. The symptoms wax and wane without treatment over months, and each year 10–20% of patients report loss of joint symptoms. (2) Twenty percent of untreated persons develop a pattern of waxing and waning arthralgias. (3) Ten percent of untreated patients develop chronic inflammatory synovitis that results in erosive lesions and destruction of the joint. Serologic tests for IgG antibodies to B. burgdorferi are positive in more than 90% of persons with Lyme arthritis, and an NAA-based assay detects Borrelia DNA in 85%.
|
TREATMENT |
LYME ARTHRITIS |
Lyme arthritis generally responds well to therapy. A regimen of oral doxycycline (100 mg twice daily for 30 days), oral amoxicillin (500 mg four times daily for 30 days), or parenteral ceftriaxone (2 g/d for 2–4 weeks) is recommended. Patients who do not respond to a total of 2 months of oral therapy or 1 month of parenteral therapy are unlikely to benefit from additional antibiotic therapy and are treated with anti-inflammatory agents or synovectomy. Failure of therapy is associated with host features such as the human leukocyte antigen DR4 (HLA-DR4) genotype, persistent reactivity to OspA (outer-surface protein A), and the presence of hLFA-1 (human leukocyte function–associated antigen 1), which cross-reacts with OspA.
SYPHILITIC ARTHRITIS
Articular manifestations occur in different stages of syphilis (Chap. 206). In early congenital syphilis, periarticular swelling and immobilization of the involved limbs (Parrot’s pseudoparalysis) complicate osteochondritis of long bones. Clutton’s joint, a late manifestation of congenital syphilis that typically develops between ages 8 and 15 years, is caused by chronic painless synovitis with effusions of large joints, particularly the knees and elbows. Secondary syphilis may be associated with arthralgias, with symmetric arthritis of the knees and ankles and occasionally of the shoulders and wrists, and with sacroiliitis. The arthritis follows a subacute to chronic course with a mixed mononuclear and neutrophilic synovial-fluid pleocytosis (typical cell counts, 5000–15,000/μL). Immunologic mechanisms may contribute to the arthritis, and symptoms usually improve rapidly with penicillin therapy. In tertiary syphilis, Charcot’s joint results from sensory loss due to tabes dorsalis. Penicillin is not helpful in this setting.
MYCOBACTERIAL ARTHRITIS
Tuberculous arthritis (Chap. 202) accounts for ~1% of all cases of tuberculosis and 10% of extrapulmonary cases. The most common presentation is chronic granulomatous monarthritis. An unusual syndrome, Poncet’s disease, is a reactive symmetric form of polyarthritis that affects persons with visceral or disseminated tuberculosis. No mycobacteria are found in the joints, and symptoms resolve with antituberculous therapy.
Unlike tuberculous osteomyelitis (Chap. 158), which typically involves the thoracic and lumbar spine (50% of cases), tuberculous arthritis primarily involves the large weight-bearing joints, in particular the hips, knees, and ankles, and only occasionally involves smaller non-weight-bearing joints. Progressive monarticular swelling and pain develop over months or years, and systemic symptoms are seen in only half of all cases. Tuberculous arthritis occurs as part of a disseminated primary infection or through late reactivation, often in persons with HIV infection or other immunocompromised hosts. Coexistent active pulmonary tuberculosis is unusual.
Aspiration of the involved joint yields fluid with an average cell count of 20,000/μL, with ~50% neutrophils. Acid-fast staining of the fluid yields positive results in fewer than one-third of cases, and cultures are positive in 80%. Culture of synovial tissue taken at biopsy is positive in ~90% of cases and shows granulomatous inflammation in most. NAA methods can shorten the time to diagnosis to 1 or 2 days. Radiographs reveal peripheral erosions at the points of synovial attachment, periarticular osteopenia, and eventually joint-space narrowing. Therapy for tuberculous arthritis is the same as that for tuberculous pulmonary disease, requiring the administration of multiple agents for 6–9 months. Therapy is more prolonged in immunosuppressed individuals such as those infected with HIV.
Various atypical mycobacteria (Chap. 204) found in water and soil may cause chronic indolent arthritis. Such disease results from trauma and direct inoculation associated with farming, gardening, or aquatic activities. Smaller joints, such as the digits, wrists, and knees, are usually involved. Involvement of tendon sheaths and bursae is typical. The mycobacterial species involved include Mycobacterium marinum, M. avium-intracellulare, M. terrae, M. kansasii, M. fortuitum, and M. chelonae. In persons who have HIV infection or are receiving immunosuppressive therapy, hematogenous spread to the joints has been reported for M. kansasii, M. avium complex, and M. haemophilum. Diagnosis usually requires biopsy and culture, and therapy is based on antimicrobial susceptibility patterns.
FUNGAL ARTHRITIS
Fungi are an unusual cause of chronic monarticular arthritis. Granulomatous articular infection with the endemic dimorphic fungi Coccidioides immitis, Blastomyces dermatitidis, and (less commonly) Histoplasma capsulatum (Fig. 157-2) results from hematogenous seeding or direct extension from bony lesions in persons with disseminated disease. Joint involvement is an unusual complication of sporotrichosis (infection with Sporothrix schenckii) among gardeners and other persons who work with soil or sphagnum moss. Articular sporotrichosis is six times more common among men than among women, and alcoholics and other debilitated hosts are at risk for polyarticular infection.
FIGURE 157-2 Chronic arthritis caused by Histoplasma capsulatum in the left knee. A. A man in his sixties from El Salvador presented with a history of progressive knee pain and difficulty walking for several years. He had undergone arthroscopy for a meniscal tear 7 years before presentation (without relief) and had received several intraarticular glucocorticoid injections. The patient developed significant deformity of the knee over time, including a large effusion in the lateral aspect. B. An x-ray of the knee showed multiple abnormalities, including severe medial femorotibial joint-space narrowing, several large subchondral cysts within the tibia and the patellofemoral compartment, a large suprapatellar joint effusion, and a large soft tissue mass projecting laterally over the knee. C. MRI further defined these abnormalities and demonstrated the cystic nature of the lateral knee abnormality. Synovial biopsies demonstrated chronic inflammation with giant cells, and cultures grew H. capsulatum after 3 weeks of incubation. All clinical cystic lesions and the effusion resolved after 1 year of treatment with itraconazole. The patient underwent a left total knee replacement for definitive treatment. (Courtesy of Francisco M. Marty, MD, Brigham and Women’s Hospital, Boston; with permission.)
Candida infection involving a single joint—usually the knee, hip, or shoulder—results from surgical procedures, intraarticular injections, or (among critically ill patients with debilitating illnesses such as diabetes mellitus or hepatic or renal insufficiency and patients receiving immunosuppressive therapy) hematogenous spread. Candida infections in IV drug users typically involve the spine, sacroiliac joints, or other fibrocartilaginous joints. Unusual cases of arthritis due to Aspergillus species, Cryptococcus neoformans, Pseudallescheria boydii, and the dematiaceous fungi also have resulted from direct inoculation or disseminated hematogenous infection in immunocompromised persons. In the United States, a 2012 national outbreak of fungal arthritis (and meningitis) caused by Exserohilum rostratum was linked to intraspinal and intraarticular injection of a contaminated preparation of methylprednisolone acetate.
The synovial fluid in fungal arthritis usually contains 10,000–40,000 cells/μL, with ~70% neutrophils. Stained specimens and cultures of synovial tissue often confirm the diagnosis of fungal arthritis when studies of synovial fluid give negative results. Treatment consists of drainage and lavage of the joint and systemic administration of an antifungal agent directed at a specific pathogen. The doses and duration of therapy are the same as for disseminated disease (see Part 8, Section 16). Intraarticular instillation of amphotericin B has been used in addition to IV therapy.
VIRAL ARTHRITIS
Viruses produce arthritis by infecting synovial tissue during systemic infection or by provoking an immunologic reaction that involves joints. As many as 50% of women report persistent arthralgias, and 10% report frank arthritis within 3 days of the rash that follows natural infection with rubella virus and within 2–6 weeks after receipt of live-virus vaccine. Episodes of symmetric inflammation of fingers, wrists, and knees uncommonly recur for >1 year, but a syndrome of chronic fatigue, low-grade fever, headaches, and myalgias can persist for months or years. IV immunoglobulin has been helpful in selected cases. Self-limited monarticular or migratory polyarthritis may develop within 2 weeks of the parotitis of mumps; this sequela is more common among men than among women. Approximately 10% of children and 60% of women develop arthritis after infection with parvovirus B19. In adults, arthropathy sometimes occurs without fever or rash. Pain and stiffness, with less prominent swelling (primarily of the hands but also of the knees, wrists, and ankles), usually resolve within weeks, although a small proportion of patients develop chronic arthropathy.
About 2 weeks before the onset of jaundice, up to 10% of persons with acute hepatitis B develop an immune complex–mediated, serum sickness–like reaction with maculopapular rash, urticaria, fever, and arthralgias. Less common developments include symmetric arthritis involving the hands, wrists, elbows, or ankles and morning stiffness that resembles a flare of rheumatoid arthritis. Symptoms resolve at the time jaundice develops. Many persons with chronic hepatitis C infection report persistent arthralgia or arthritis, both in the presence and in the absence of cryoglobulinemia.
![]() Painful arthritis involving larger joints often accompanies the fever and rash of several arthropod-borne viral infections, including those caused by chikungunya, O’nyong-nyong, Ross River, Mayaro, and Barmah Forest viruses (Chap. 233). Symmetric arthritis involving the hands and wrists may occur during the convalescent phase of infection with lymphocytic choriomeningitis virus. Patients infected with an enterovirus frequently report arthralgias, and echovirus has been isolated from patients with acute polyarthritis.
Painful arthritis involving larger joints often accompanies the fever and rash of several arthropod-borne viral infections, including those caused by chikungunya, O’nyong-nyong, Ross River, Mayaro, and Barmah Forest viruses (Chap. 233). Symmetric arthritis involving the hands and wrists may occur during the convalescent phase of infection with lymphocytic choriomeningitis virus. Patients infected with an enterovirus frequently report arthralgias, and echovirus has been isolated from patients with acute polyarthritis.
Several arthritis syndromes are associated with HIV infection. Reactive arthritis with painful lower-extremity oligoarthritis often follows an episode of urethritis in HIV-infected persons. HIV-associated reactive arthritis appears to be extremely common among persons with the HLA-B27 haplotype, but sacroiliac joint disease is unusual and is seen mostly in the absence of HLA-B27. Up to one-third of HIV-infected persons with psoriasis develop psoriatic arthritis. Painless monarthropathy and persistent symmetric polyarthropathy occasionally complicate HIV infection. Chronic persistent oligoarthritis of the shoulders, wrists, hands, and knees occurs in women infected with human T-lymphotropic virus type I. Synovial thickening, destruction of articular cartilage, and leukemic-appearing atypical lymphocytes in synovial fluid are characteristic, but progression to T cell leukemia is unusual.
PARASITIC ARTHRITIS
Arthritis due to parasitic infection is rare. The guinea worm Dracunculus medinensis may cause destructive joint lesions in the lower extremities as migrating gravid female worms invade joints or cause ulcers in adjacent soft tissues that become secondarily infected. Hydatid cysts infect bones in 1–2% of cases of infection with Echinococcus granulosus. The expanding destructive cystic lesions may spread to and destroy adjacent joints, particularly the hip and pelvis. In rare cases, chronic synovitis has been associated with the presence of schistosomal eggs in synovial biopsies. Monarticular arthritis in children with lymphatic filariasis appears to respond to therapy with diethylcarbamazine even in the absence of microfilariae in synovial fluid. Reactive arthritis has been attributed to hookworm, Strongyloides, Cryptosporidium, and Giardia infection in case reports, but confirmation is required.
POSTINFECTIOUS OR REACTIVE ARTHRITIS
Reactive polyarthritis develops several weeks after ~1% of cases of nongonococcal urethritis and 2% of enteric infections, particularly those due to Yersinia enterocolitica, Shigella flexneri, Campylobacter jejuni, and Salmonella species. Only a minority of these patients have the other findings of classic reactive arthritis, including urethritis, conjunctivitis, uveitis, oral ulcers, and rash. Studies have identified microbial DNA or antigen in synovial fluid or blood, but the pathogenesis of this condition is poorly understood.
Reactive arthritis is most common among young men (except after Yersinia infection) and has been linked to the HLA-B27 locus as a potential genetic predisposing factor. Patients report painful, asymmetric oligoarthritis that affects mainly the knees, ankles, and feet. Low-back pain is common, and radiographic evidence of sacroiliitis is found in patients with long-standing disease. Most patients recover within 6 months, but prolonged recurrent disease is more common in cases that follow chlamydial urethritis. Anti-inflammatory agents help relieve symptoms, but the role of prolonged antibiotic therapy in eliminating microbial antigen from the synovium is controversial.
Migratory polyarthritis and fever constitute the usual presentation of acute rheumatic fever in adults (Chap. 381). This presentation is distinct from that of poststreptococcal reactive arthritis, which also follows infections with group A Streptococcus but is not migratory, lasts beyond the typical 3-week maximum of acute rheumatic fever, and responds poorly to aspirin.
INFECTIONS IN PROSTHETIC JOINTS
Infection complicates 1–4% of total joint replacements. The majority of infections are acquired intraoperatively or immediately postoperatively as a result of wound breakdown or infection; less commonly, these joint infections develop later after joint replacement and are the result of hematogenous spread or direct inoculation. The presentation may be acute, with fever, pain, and local signs of inflammation, especially in infections due to S. aureus, pyogenic streptococci, and enteric bacilli. Alternatively, infection may persist for months or years without causing constitutional symptoms when less virulent organisms, such as coagulase-negative staphylococci or diphtheroids, are involved. Such indolent infections usually are acquired during joint implantation and are discovered during evaluation of chronic unexplained pain or after a radiograph shows loosening of the prosthesis; the erythrocyte sedimentation rate and C-reactive protein level are usually elevated in such cases.
The diagnosis is best made by needle aspiration of the joint; accidental introduction of organisms during aspiration must be avoided meticulously. Synovial fluid pleocytosis with a predominance of polymorphonuclear leukocytes is highly suggestive of infection, since other inflammatory processes uncommonly affect prosthetic joints. Culture and Gram’s stain usually yield the responsible pathogen. Sonication of explanted prosthetic material can improve the yield of culture, presumably by breaking up bacterial biofilms on the surfaces of prostheses. Use of special media for unusual pathogens such as fungi, atypical mycobacteria, and Mycoplasma may be necessary if routine and anaerobic cultures are negative.
|
TREATMENT |
PROSTHETIC JOINT INFECTIONS |
Treatment includes surgery and high doses of parenteral antibiotics, which are given for 4–6 weeks because bone is usually involved. In most cases, the prosthesis must be replaced to cure the infection. Implantation of a new prosthesis is best delayed for several weeks or months because relapses of infection occur most commonly within this time frame. In some cases, reimplantation is not possible, and the patient must manage without a joint, with a fused joint, or even with amputation. Cure of infection without removal of the prosthesis is occasionally possible in cases that are due to streptococci or pneumococci and that lack radiologic evidence of loosening of the prosthesis. In these cases, antibiotic therapy must be initiated within several days of the onset of infection, and the joint should be drained vigorously by open arthrotomy or arthroscopically. In selected patients who prefer to avoid the high morbidity rate associated with joint removal and reimplantation, suppression of the infection with antibiotics may be a reasonable goal. A high cure rate with retention of the prosthesis has been reported when the combination of oral rifampin and ciprofloxacin is given for 3–6 months to persons with staphylococcal prosthetic joint infection of short duration. This approach, which is based on the ability of rifampin to kill organisms adherent to foreign material and in the stationary growth phase, requires confirmation in prospective trials.
PREVENTION
To avoid the disastrous consequences of infection, candidates for joint replacement should be selected with care. Rates of infection are particularly high among patients with rheumatoid arthritis, persons who have undergone previous surgery on the joint, and persons with medical conditions requiring immunosuppressive therapy. Perioperative antibiotic prophylaxis, usually with cefazolin, and measures to decrease intraoperative contamination, such as laminar flow, have lowered the rates of perioperative infection to <1% in many centers. After implantation, measures should be taken to prevent or rapidly treat extraarticular infections that might give rise to hematogenous spread to the prosthesis. The effectiveness of prophylactic antibiotics for the prevention of hematogenous infection after dental procedures has not been demonstrated; in fact, viridans streptococci and other components of the oral flora are extremely unusual causes of prosthetic joint infection. Accordingly, the American Dental Association and the American Academy of Orthopaedic Surgeons do not recommend antibiotic prophylaxis for most dental patients with total joint replacements and have stated that there is no convincing evidence to support its use. Similarly, guidelines issued by the American Urological Association and the American Academy of Orthopaedic Surgeons do not recommend the use of prophylactic antibiotics for most patients with prosthetic joints who are undergoing urologic procedures but state that prophylaxis should be considered in certain situations—e.g., for patients (especially immunocompromised patients) who are undergoing a procedure posing a relatively high risk of bacteremia (such as lithotripsy or surgery involving bowel segments).
ACKNOWLEDGMENTS
The contributions of James H. Maguire and the late Scott J. Thaler to this chapter in earlier editions are gratefully acknowledged.
158 |
Osteomyelitis |
Osteomyelitis, an infection of bone, can be caused by various microorganisms that arrive at bone through different routes. Spontaneous hematogenous osteomyelitis may occur in otherwise healthy individuals, whereas local microbial spread mainly affects either individuals who have underlying disease (e.g., vascular insufficiency) or patients who have compromised skin or other tissue barriers, with consequent exposure of bone. The latter situation typically follows surgery involving bone, such as sternotomy or orthopedic repair.
The manifestations of osteomyelitis are different in children and adults. In children circulating microorganisms seed mainly long bones, whereas in adults the vertebral column is the most commonly affected site.
Management of osteomyelitis differs greatly depending on whether an implant is involved. The most important aim of the management of either type of osteomyelitis is to prevent progression to chronic osteomyelitis by rapid diagnosis and prompt treatment. Device-related bone and joint infection necessitates a multidisciplinary approach requiring antibiotic therapy and, in many cases, surgical removal of the device. The optimal duration of antibiotic treatment has not been established for any type of osteomyelitis in clinical trials. Therefore, the recommendations for therapy in this chapter reflect only expert opinions.
CLASSIFICATION
There is no generally accepted, comprehensive system for classification of osteomyelitis, primarily because of the multifaceted presentation of this infection. Different specialists are confronted with different facets of bone disease. Most often, however, general practitioners or internists are the first to encounter patients with the initial signs and symptoms of osteomyelitis. These primary care physicians should be able to recognize this disease in any of its forms. Osteomyelitis cases can be classified by various criteria, including pathogenesis, duration of infection, location of infection, and presence or absence of foreign material. The widely used Cierny-Mader staging system classifies osteomyelitis according to anatomic site, comorbidity, and radiographic findings, with stratification of long-bone osteomyelitis to optimize surgical management; this system encompasses both systemic and local factors affecting immune status, metabolism, and local vascularity.
Any of three mechanisms can underlie osteomyelitis: (1) hematogenous spread; (2) spread from a contiguous site following surgery; and (3) secondary infection in the setting of vascular insufficiency or concomitant neuropathy. Hematogenous osteomyelitis in adults typically involves the vertebral column. In only about half of patients can a primary focus be detected. The most common primary foci of infection are the urinary tract, skin/soft tissue, intravascular catheterization sites, and the endocardium. Spread from a contiguous source follows either bone trauma or surgical intervention. Wound infection leading to osteomyelitis typically occurs after cardiovascular intervention involving the sternum, orthopedic repair, or prosthetic joint insertion. Osteomyelitis secondary to vascular insufficiency or peripheral neuropathy most often follows chronic, progressively deep skin and soft tissue infection of the foot. The most common underlying condition is diabetes. In diabetes that is poorly controlled, the diabetic foot syndrome is caused by skin, soft tissue, and bone ischemia combined with motor, sensory, and autonomic neuropathy.
Classification of osteomyelitis according to the duration of infection, although ill defined (because there is no clear time limit for the transition from acute to chronic osteomyelitis), is useful because the management of acute and chronic osteomyelitis differs. Whereas acute osteomyelitis can generally be treated with antibiotics alone, antibiotic treatment for chronic osteomyelitis should be combined with debridement surgery. Acute hematogenous or contiguous osteomyelitis evolves over a short period—i.e., a few days or weeks. In contrast, subacute or chronic osteomyelitis lasts for weeks or months before treatment is started. Typical examples of a subacute course are vertebral osteomyelitis due to tuberculosis or brucellosis and delayed implant-associated infections caused mainly by low-virulence microorganisms (coagulase-negative staphylococci, Propionibacterium acnes). Chronic osteomyelitis develops when insufficient therapy leads to persistence or recurrence, most often after sternal, mandibular, or foot infection.
Classification by location distinguishes among cases in the long bones, the vertebral column, and the periarticular bones. Long bones are generally involved after hematogenous seeding in children or contiguous spread following trauma or surgery. The risk of vertebral osteomyelitis in adults increases with age. Periarticular osteomyelitis, which complicates septic arthritis that has not been adequately treated, is especially common in periprosthetic joint infection.
Osteomyelitis involving a foreign device requires surgical management for cure. Even acute implant-associated infection calls for prolonged antimicrobial therapy. Therefore, identification of this type of disease is of practical importance.
VERTEBRAL OSTEOMYELITIS
PATHOGENESIS
Vertebral osteomyelitis, also referred to as disk-space infection, septic diskitis, spondylodiskitis, or spinal osteomyelitis, is the most common manifestation of hematogenous bone infection in adults. This designation reflects a pathogenic process leading to involvement of the adjacent vertebrae and the corresponding intervertebral disk. In adults, the disk is avascular. Microorganisms invade via the segmental arterial circulation in adjacent endplates and then spread into the disk. Alternative routes of infection are retrograde seeding through the prevertebral venous plexus and direct inoculation during spinal surgery, epidural infiltration, or trauma. In the setting of implant surgery, microorganisms are inoculated either during the procedure or, if wound healing is impaired, in the early postoperative period.
EPIDEMIOLOGY
Vertebral osteomyelitis occurs more often in male than in female patients (ratio, 1.5:1). The overall incidence is 2.4 cases/100,000 population. There is a clear age-dependent increase from 0.3 cases/100,000 at ages <20 years to 6.5 cases/100,000 at ages >70 years. The observed increase in reported cases during the past two decades may reflect improvements in diagnosis resulting from the broad availability of MRI technology. In addition, the fraction of cases of vertebral osteomyelitis acquired in association with health care is certainly increasing as a consequence of the rising number of spinal interventions and local infiltrations.
MICROBIOLOGY
Vertebral osteomyelitis is typically classified as pyogenic or nonpyogenic. However, this distinction is arbitrary because, in “nonpyogenic” cases (tuberculous, brucellar), macroscopic pus formation (caseous necrosis, abscess) is quite common. A more accurate scheme is to classify cases as acute or subacute/chronic. Whereas the microbiologic spectrum of acute cases is similar in different parts of the world, the spectrum of subacute/chronic cases varies according to the geographic region. The great majority of cases are monomicrobial in etiology. Of episodes of acute vertebral osteomyelitis, 40–50% are caused by Staphylococcus aureus, 12% by streptococci, and 20% by gram-negative bacilli—mainly Escherichia coli (9%) and Pseudomonas aeruginosa (6%). Subacute vertebral osteomyelitis is typically caused by Mycobacterium tuberculosis or Brucella species in regions where these microorganisms are endemic. Osteomyelitis due to viridans streptococci also has a subacute presentation; these infections most often occur as secondary foci in patients with endocarditis. In vertebral osteomyelitis due to Candida species, the diagnosis is often delayed by several weeks; this etiology should be suspected in IV drug users who do not use sterile paraphernalia. In implant-associated spinal osteomyelitis, coagulase-negative staphylococci and P. acnes—which, in the absence of an implant, are generally considered contaminants—typically cause low-grade (chronic) infections. As an exception, coagulase-negative staphylococci can cause native spinal osteomyelitis in cases of prolonged bacteremia (e.g., in patients with infected pacemaker electrodes or implanted vascular catheters that are not promptly removed).
CLINICAL MANIFESTATIONS
The signs and symptoms of vertebral osteomyelitis are nonspecific. Only about half of patients develop fever >38°C (100.4°F), perhaps because analgesic drugs are frequently used by these patients. Back pain is the leading initial symptom (>85% of cases). The location of the pain corresponds to the site of infection: the cervical spine in ~10% of cases, the thoracic spine in 30%, and the lumbar spine in 60%. One exception is involvement at the thoracic level in two-thirds of cases of tuberculous osteomyelitis and at the lumbar level in only one-third. This difference is due to direct mycobacterial spread via pleural or mediastinal lymph nodes in pulmonary tuberculosis.
Neurologic deficits, such as radiculopathy, weakness, or sensory loss, are observed in about one-third of cases of vertebral osteomyelitis. In brucellar vertebral osteomyelitis, neurologic impairment is less frequent; in tuberculous osteomyelitis, it is about twice as frequent as in cases of other etiologies. Neurologic signs and symptoms are caused mostly by spinal epidural abscess. This complication starts with severe localized back pain and progresses to radicular pain, reflex changes, sensory abnormalities, motor weakness, bowel and bladder dysfunction, and paralysis.
A primary focus should always be sought but is found in only half of cases. Overall, endocarditis is identified in ~10% of patients. In osteomyelitis caused by viridans streptococci, endocarditis is the source in about half of patients.
Implant-associated spinal osteomyelitis can present as either early- or late-onset infection. Early-onset infection is diagnosed within 30 days after implant placement. S. aureus is the most common pathogen. Wound healing impairment and fever are the leading findings. Late-onset infection is diagnosed beyond 30 days after surgery, with low-virulence organisms such as coagulase-negative staphylococci or P. acnes as typical infecting agents. Fever is rare. One-quarter of patients have a sinus tract. Because of the delayed course and the lack of classic signs of infection, rapid diagnosis requires a high degree of suspicion.
DIAGNOSIS
Leukocytosis and neutrophilia have low levels of diagnostic sensitivity (only 65% and 40%, respectively). In contrast, an increased erythrocyte sedimentation rate or C-reactive protein (CRP) level has been reported in 98% and 100% of cases, respectively; thus, these tests are helpful in excluding vertebral osteomyelitis. The fraction of blood cultures that yield positive results depends heavily on whether the patient has been pretreated with antibiotics; across studies, the range is from 30% to 78%. In view of this low rate of positive blood culture after antibiotic treatment, such therapy should be withheld until microbial growth is proven unless the patient has sepsis syndrome. In patients with negative blood cultures, CT-guided or open biopsy is needed. Whether a CT-guided biopsy with a negative result is repeated or followed by open biopsy depends on the experience of personnel at the specific center. Bone samples should be cultured for aerobic, anaerobic, and fungal agents, with a portion of the sample sent for histopathologic study. In cases with a subacute/chronic presentation, a suggestive history, or a granuloma detected during histopathologic analysis, mycobacteria and brucellae also should be sought. When blood and tissue cultures are negative despite suggestive histopathology, broad-range polymerase chain reaction analysis of biopsy specimens or aspirated pus should be considered. This technique allows detection of unusual pathogens such as Tropheryma whipplei.
Given that signs and symptoms of osteomyelitis are nonspecific, the clinical differential diagnosis of febrile back pain is broad, including pyelonephritis, pancreatitis, and viral syndromes. In addition, multiple noninfectious pathologies of the vertebral column, such as osteoporotic fracture, seronegative spondylitis (ankylosing spondylitis, psoriasis, reactive arthritis, enteropathic arthritis), and spinal stenosis must be considered.
Imaging procedures are the most important tools not only for the diagnosis of vertebral osteomyelitis but also for the detection of pyogenic complications and alternative conditions (e.g., bone metastases or osteoporotic fractures). Plain radiography is a reasonable first step in evaluating patients without neurologic symptoms and may reveal an alternative diagnosis. Because of its low sensitivity, plain radiography generally is not helpful in acute osteomyelitis, but it can be useful in subacute or chronic cases. The gold standard is MRI, which should be performed expeditiously in patients with neurologic impairment in order to rule out a herniated disk or to detect pyogenic complications in a timely manner. Even if the pathologic findings on MRI suggest vertebral osteomyelitis, alternative diagnoses should be considered, especially when blood cultures are negative. The most common alternative diagnosis is erosive osteochondrosis. Septic bone necrosis, gouty spondylodiskitis, and erosive diskovertebral lesions (Andersson lesions) in ankylosing spondylitis may likewise mimic vertebral osteomyelitis. CT is less sensitive than MRI but may be helpful in guiding a percutaneous biopsy. In the future, positron-emission tomography (PET) with 18F-fluorodeoxyglucose, which has a high degree of diagnostic accuracy, may be an alternative imaging procedure when MRI is contraindicated. 18F-fluorodeoxyglucose PET should be considered for patients with implants and patients in whom several foci are suspected.
|
TREATMENT |
VERTEBRAL OSTEOMYELITIS |
The aims of therapy for vertebral osteomyelitis are (1) elimination of the pathogen(s), (2) protection from further bone loss, (3) relief of back pain, (4) prevention of complications, and (5) stabilization, if needed.
ANTIMICROBIAL THERAPY
Table 158-1 summarizes suggested antimicrobial regimens for infections attributable to the most common etiologic agents. For optimal antimicrobial therapy, identification of the infecting agent is required. Therefore, in patients without sepsis syndrome, antibiotics should not be administered until the pathogen is identified in a blood culture, a bone biopsy, or an aspirated pus collection. Traditionally, bone infections are at least initially treated by the IV route. Unfortunately, relevant controlled trials are lacking, and the preference for the IV route is not evidence based. There are no good arguments for the assumption that IV therapy is superior to oral administration if the following requirements are met: (1) optimal antibiotic spectrum, (2) excellent bioavailability of the oral drug, (3) clinical studies confirming efficacy of the oral drug, (4) normal intestinal function, and (5) no vomiting. However, a short initial course of parenteral therapy with a β-lactam antibiotic may lower the risk of emergence of fluoroquinolone resistance, especially if P. aeruginosa infection is treated with ciprofloxacin or staphylococcal infection with the combination of a fluoroquinolone plus rifampin. These suggestions are based on observational studies and expert opinion. There are no data from controlled trials on the optimal duration of therapy. Most experts suggest 6 weeks for patients who have acute osteomyelitis without an implant. According to an observational study, prolonging antibiotic therapy beyond 6 weeks does not improve the rate of recovery or lower the risk of recurrence. However, prolonged antibiotic therapy is recommended for patients with abscesses that have not been drained and patients with spinal implants. Treatment efficacy should be regularly monitored through inquiries about signs and symptoms (fever, pain) and assessment for signs of inflammation (elevated CRP concentrations). Follow-up MRI is appropriate only for patients with pyogenic complications, since the correlation between clinical healing and improvement on MRI is very poor.
|
ANTIBIOTIC THERAPY FOR OSTEOMYELITIS IN ADULTS WITHOUT IMPLANTSa |
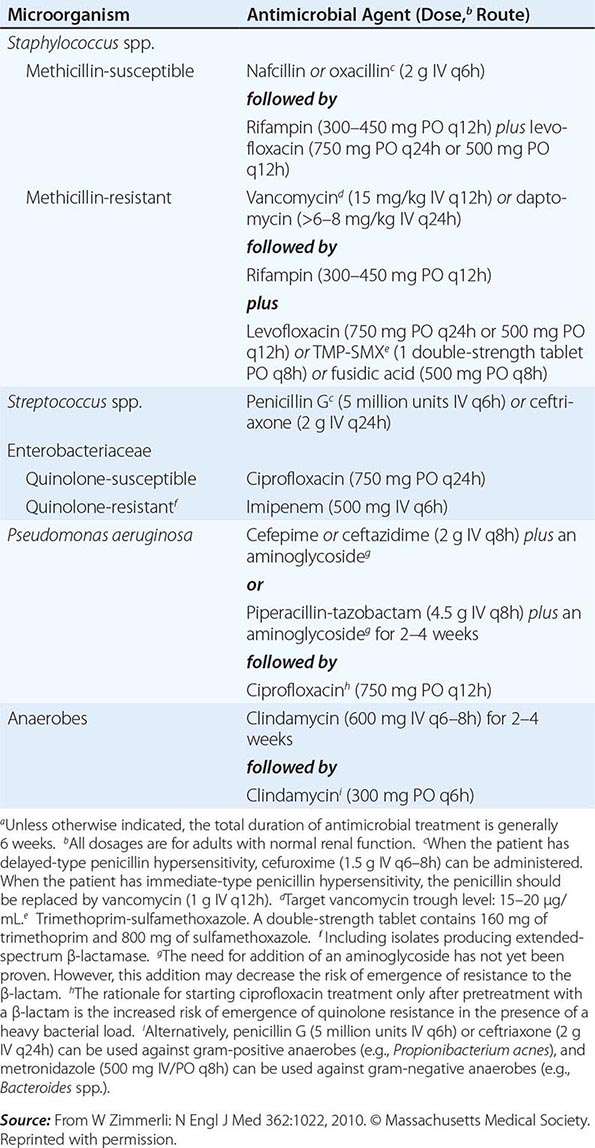
Surgical treatment generally is not needed in acute hematogenous vertebral osteomyelitis. However, it is always necessary in implant-associated spinal infection. Early infections (those occurring up to 30 days after internal stabilization) can be cured with debridement, implant retention, and a 3-month course of antibiotics (Table 158-2). In contrast, in late infection with a duration of >30 days, implant removal and a 6-week-course of antibiotics (Table 158-1) are required for complete elimination of the infection. If implants cannot be removed, oral suppressive long-term treatment should follow the initial course of IV antibiotics. The optimal duration of suppressive therapy is unknown. However, if antibiotic therapy is discontinued after, for example, 1 year, close clinical and laboratory (CRP) follow-up is needed.
|
ANTIBIOTIC THERAPY FOR OSTEOMYELITIS ASSOCIATED WITH ORTHOPEDIC DEVICES |
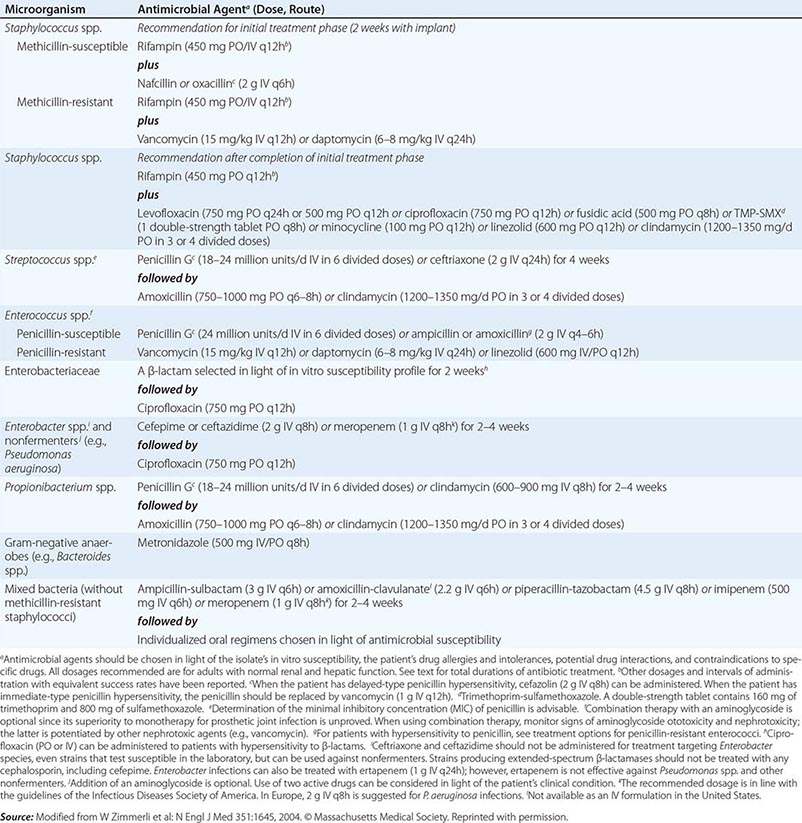
COMPLICATIONS
Complications include persistent pain, persistently increased CRP levels, and new-onset or persistent neurologic impairment. In cases of persistent pain with or without signs of inflammation, paravertebral, epidural, or psoas abscesses (Fig. 158-1) must be sought. Epidural abscesses occur in 15–20% of cases. This complication is more common in the cervical column (30%) than in the lumbar spine (12%). Persistent pain despite normalization of CRP values indicates mechanical complications such as severe osteonecrosis or spinal instability. These patients require a consult with an experienced orthopedic surgeon.
FIGURE 158-1 CT scan of acute vertebral osteomyelitis (L1/L2) due to Staphylococcus aureus in a 64-year-old man. Low-grade fever persisted despite appropriate IV antibiotic therapy. The scan revealed a psoas abscess on the right side.
OSTEOMYELITIS IN LONG BONES
PATHOGENESIS
Osteomyelitis in long bones is a consequence of hematogenous seeding, exogenous contamination during trauma (open fracture), or perioperative contamination during orthopedic repairs. Its presentation is either acute (with a duration of days to a few weeks) or chronic. Hematogenous infection in long bones typically occurs in children. Ineffectively treated hematogenous osteomyelitis during childhood can progress to chronic disease. In adults, the leading pathogenic source is exogenous infection, mainly associated with internal fixation devices. Chronic osteomyelitis can recur after a symptom-free interval of >50 years. Such recurrences are most common among elderly patients who developed osteomyelitis in the preantibiotic era.
EPIDEMIOLOGY
In adults, most cases of long-bone osteomyelitis are posttraumatic or postsurgical; less frequently, late recurrence arises from hematogenous infections during childhood. The risk of infection depends on the type of fracture. After closed fracture, implant-associated infection occurs in fewer than 1% of patients. In contrast, after open fracture, the risk of osteomyelitis ranges from ~2% up to 16%, with the precise figure depending on the degree of tissue damage during trauma.
MICROBIOLOGY
The spectrum of microorganisms causing hematogenous long-bone osteomyelitis does not differ from that in vertebral osteomyelitis. S. aureus is most commonly isolated from adult patients. In rare cases, mycobacteria or fungal agents such as Cryptococcus species, Sporothrix schenckii, Blastomyces dermatitidis, or Coccidioides species are found in patients who live or have traveled in endemic regions. Impaired cellular immunity (e.g., in HIV infection or after transplantation) predisposes to these etiologies. Coagulase-negative staphylococci are the second most common etiologic agents (after S. aureus) in implant-associated osteomyelitis. After open fracture, contiguous long-bone osteomyelitis is typically caused by gram-negative bacilli or a polymicrobial mixture of organisms.
CLINICAL MANIFESTATIONS
The leading symptoms in adults with primary or recurrent hematogenous long-bone osteomyelitis are pain and low-grade fever. Infection occasionally manifests as clinical sepsis and local signs of inflammation (erythema and swelling). After internal fixation, osteomyelitis can be classified as acute (≤3 weeks) or chronic. Acute long-bone osteomyelitis manifests as signs of surgical site infection, such as erythema and impaired wound healing. Acute implant-associated infection may also follow hematogenous seeding at any time after implantation of a device. Typical symptoms are new-onset pain and signs of sepsis. Chronic infections are usually caused by low-virulence microorganisms or occur after ineffective treatment of early-onset infection. Patients may present with persisting pain, subtle local signs of inflammation, intermittent discharge of pus, or fluctuating erythema over the scar (Fig. 158-2).
FIGURE 158-2 A 42-year-old man who had had a malleolar fracture 6 weeks previously had persistent pain and slight inflammation after orthopedic repair. His infection was treated with oral antibiotics without debridement surgery. This insufficient management of an implant-associated Staphylococcus aureus infection was complicated by a sinus tract.
DIAGNOSIS
The diagnostic workup for acute hematogenous long-bone osteomyelitis is similar to that for vertebral osteomyelitis. Bone remodeling and thus marker uptake are increased for at least 1 year after surgery. Therefore, the three-phase bone scan is not useful during this interval. However, in late recurrences it allows rapid diagnosis at low cost. If the results are positive, CT is required in order to estimate the extent of inflamed tissue and to detect bone necrosis (sequesters). Implant-associated infection should be suspected if CRP values do not return to the normal range or rise after an initial decrease. Clinical and laboratory suspicion should prompt surgical exploration and sampling.
In chronic osteomyelitis of >1 year’s duration, single-photon emission CT plus conventional CT (SPECT/CT) is a good option, either with 99mTc methylene diphosphonate (99mTc-MDP)–labeled leukocytes or with labeled monoclonal antibodies to granulocytes. Surgical debridement is needed for diagnostic (biopsy culture, histology) and therapeutic reasons.
|
TREATMENT |
OSTEOMYELITIS IN LONG BONES |
Treatment for acute hematogenous infection in long bones is identical to that for acute vertebral osteomyelitis (Table 158-1). The suggested duration of antibiotic therapy is 4–6 weeks. In contrast to chronic or implant-associated osteomyelitis, acute hematogenous infection does not require surgical intervention. Initial IV administration of antimicrobial agents is followed by long-term oral treatment. The duration of the initial IV phase of therapy has not been defined. The IV course can be as short as a couple of days if a drug with excellent bioavailability is available. In case of recurrence of chronic osteomyelitis as well as in each type of exogenous osteomyelitis (acute, chronic, with or without an implant), a combination of surgical debridement, obliteration of dead space, and long-term antibiotic therapy is needed.
The therapeutic aims in patients whose infections are associated with internal fixation devices are consolidation of the fracture and prevention of chronic osteomyelitis. Stable implants can be maintained except in patients with uncontrolled sepsis. Appropriate antimicrobial therapies are listed in Table 158-2. The cure rate for early staphylococcal implant-associated infections treated with a fluoroquinolone plus rifampin is >90%. Rifampin is efficacious against staphylococcal biofilms of ≤3 weeks’ duration. Similarly, fluoroquinolones are active against biofilms formed by gram-negative bacilli. In these cases, an initial 2-week course of IV therapy with a β-lactam is suggested in order to minimize the risk of emergence of resistance to the oral drugs. The total duration of treatment is 3 months, and the device can be retained even after antibiotics have been discontinued. In contrast, in cases caused by rifampin-resistant staphylococci or fluoroquinolone-resistant gram-negative bacilli, the hardware should be removed after consolidation of the fracture and before discontinuation of antibiotics. These patients are treated with an oral antibiotic (suppressive therapy) as long as retention of the hardware is necessary.
COMPLICATIONS
The main complication of long-bone osteomyelitis is the persistence of infection with progression to chronic osteomyelitis. This risk is especially high after internal fixation of an open fracture and among patients with implant-associated osteomyelitis that is treated without surgical debridement. In chronic osteomyelitis, recurrent sinus tracts result in severe damage to skin and soft tissue (Fig. 158-2). Patients who have chronic open wounds need a therapeutic approach combining orthopedic repair and plastic reconstructive surgery.
PERIPROSTHETIC JOINT INFECTION
PATHOGENESIS
Implanted foreign material is highly susceptible to local infection due to local immunodeficiency around the device. Infection occurs by either the exogenous or the hematogenous route. More rarely, contiguous spread from adjacent sites of osteomyelitis or deep soft-tissue infection may cause periprosthetic joint infection (PJI). The fact that foreign devices are covered with host proteins such as fibronectin favors the adherence of staphylococci and the formation of a biofilm that resists phagocytosis.
EPIDEMIOLOGY
The risk of infection manifesting during the first 2 postoperative years varies according to the joint. It is lowest after hip and knee arthroplasty (0.3–1.5%) and highest after ankle and elbow replacement (4–10%). The risk of hematogenous PJI is highest in the early postoperative period. However, hematogenous seeding occurs throughout life, and most cases therefore develop >2 years after implantation.
MICROBIOLOGY
About 70% of cases of PJI are caused by staphylococci (S. aureus and coagulase-negative staphylococci), 10% by streptococci, 10% by gram-negative bacilli, and the rest by various other microorganisms. All microorganisms can cause PJI, including fungi and mycobacteria. P. acnes causes up to one-third of episodes of periprosthetic shoulder infection.
CLASSIFICATION AND CLINICAL MANIFESTATIONS
PJI is traditionally classified as early (<3 months after implantation), delayed (3–24 months after surgery), or late (>2 years after implantation). For therapeutic decision-making (see below), it is more useful to classify PJI as (1) acute hematogenous PJI with <3 weeks of symptoms, (2) early postinterventional PJI manifesting within 1 month after surgery, and (3) chronic PJI with symptom duration of >3 weeks.
Acute exogenous PJI typically presents with local signs of infection (Fig. 158-3). In contrast, acute hematogenous PJI, most often caused by S. aureus, is characterized by new-onset pain that initially is not accompanied by prominent local inflammatory signs. In most cases, an ongoing sepsis syndrome dominates the clinical picture. Key findings in chronic PJI are joint effusion, local pain, implant loosening, and occasionally a sinus tract. Chronic PJI is most commonly caused by low-virulence microorganisms such as coagulase-negative staphylococci or P. acnes. These infections are characterized by nonspecific symptoms, such as chronic pain caused by low-grade inflammation or early loosening.
FIGURE 158-3 Early periprosthetic joint infection of the left hip caused by group B streptococci in a 68-year-old woman.
DIAGNOSIS
Blood tests such as the measurement of CRP (elevated levels, ≥10 mg/L) and erythrocyte sedimentation rate (elevated rates, ≥30 mm/h) are sensitive (91–97%) but not specific (70–78%). Synovial fluid cell counts are ~90% sensitive and specific, with threshold values of 1700 leukocytes/μL in periprosthetic knee infection and 4200 leukocytes/μL in periprosthetic hip infection. During debridement surgery, at least three but optimally six tissue samples should be obtained for culture and histopathology. If implant material (modular parts, screws, or the prosthesis) is removed, sonication of this material followed by culture and/or use of molecular methods to examine the sonicate fluid allows the detection of microorganisms in biofilms.
The three-phase bone scan is very sensitive for detecting PJI but is not specific. As mentioned above, this test does not differentiate bone remodeling from infection and therefore is not useful during at least the first year after implantation. CT and MRI detect soft tissue infection, prosthetic loosening, and bone erosion, but imaging artifacts caused by metal implants limit their use. 18F-fluorodeoxyglucose PET is an alternative method with fair sensitivity and specificity for the detection of PJI. However, this technique is not yet an established procedure for this purpose.
|
TREATMENT |
PERIPROSTHETIC JOINT INFECTION |
Treatment of PJI requires a multidisciplinary approach involving an experienced orthopedic surgeon, an infectious disease specialist, a plastic reconstructive surgeon, and a microbiologist. Therefore, most patients are referred to a specialized center. In general, the goal of treatment is cure—i.e., a pain-free functional joint with complete eradication of the infecting pathogen(s). However, for patients with severe comorbidity, lifelong suppressive antimicrobial therapy may be preferred. As a rule, antimicrobial therapy without surgical intervention is not curative but merely suppressive. There are four curative surgical options: debridement and implant retention, one-stage implant exchange, two-stage implant exchange, and implant removal without replacement. Implant retention offers a good chance of infection-free survival (>80%) only if the following conditions are fulfilled: (1) acute infection, (2) stable implant, (3) pathogen susceptible to a biofilm-active antimicrobial agent (see below), and (4) skin and soft tissue in good condition.
Table 158-2 summarizes pathogen-specific antimicrobial therapy for PJI. Initial IV therapy is followed by long-term oral antibiotics. Efficacious treatment is best defined in staphylococcal implant-associated infections. Rifampin exhibits excellent activity against biofilms composed of susceptible staphylococci. Because of the risk of rapid emergence of resistance, rifampin must always be combined with another effective antibiotic. If gram-negative infections are treated with implant retention, fluoroquinolones should be used because of their activity against gram-negative biofilms.
PREVENTION OF HEMATOGENOUS INFECTION
As mentioned above, hematogenous seeding may occur throughout life. This risk is highest during S. aureus bacteremia from a distant focus. Therefore, documented bacterial infections should be promptly treated in patients with prosthetic joints. However, according to a large, prospective, case-control study, the risk of prosthetic hip or knee infection is not increased following dental procedures. Therefore, antibiotic prophylaxis is not needed during dental work.
STERNAL OSTEOMYELITIS
PATHOGENESIS
Sternal osteomyelitis occurs primarily after sternal surgery (with the entry of exogenous organisms) and more rarely by hematogenous seeding or contiguous extension from adjacent sites of sternocostal arthritis. Exogenous sternal osteomyelitis after open sternal surgery is also called deep sternal wound infection. Exogenous infection may also follow minor sternal trauma, sternal fracture, and manubriosternal septic arthritis. Tuberculous sternal osteomyelitis typically manifests during hematogenous seeding in children or as reactivated infection in adults. Reactivation is sometimes preceded by blunt trauma. In rare cases, tuberculous sternal osteomyelitis is caused by continuous infection from an infected internal mammary lymph node.
EPIDEMIOLOGY
The incidence of poststernotomy wound infection varies from 0.5% to 5%, but figures are even higher among patients with risk factors such as diabetes, obesity, chronic renal failure, emergency surgery, use of bilateral internal mammary arteries, and reexploration for bleeding. Rapid diagnosis and correct management of superficial sternal wound infection prevent its progression to sternal osteomyelitis. Primary (hematogenous) sternal osteomyelitis accounts for only 0.3% of all cases of osteomyelitis. Risk factors are IV drug use, HIV infection, radiotherapy, blunt trauma, cardiopulmonary resuscitation, alcohol abuse, liver cirrhosis, and hemoglobinopathy.
MICROBIOLOGY
Poststernotomy osteomyelitis is generally caused by S. aureus (40–50% of cases), coagulase-negative staphylococci (15–30%), enterococci (5–12%), or gram-negative bacilli (15–25%). Fungal infections caused by Candida species also play a role. The fact that ~20% of cases are polymicrobial is indicative of exogenous superinfection during therapy. Hematogenous sternal osteomyelitis is caused most commonly by S. aureus. Other microorganisms play a role in special populations—e.g., P. aeruginosa in IV drug users, Salmonella species in individuals with sickle cell anemia, and M. tuberculosis in patients from endemic areas who have previously had tuberculosis.
CLINICAL MANIFESTATIONS
Exogenous sternal osteomyelitis manifests as fever, increased local pain, erythema, wound discharge, and sternal instability (Fig. 158-4). Contiguous mediastinitis is a feared complication, occurring in ~10–30% of patients with sternal osteomyelitis. Hematogenous sternal osteomyelitis is characterized by sternal pain, swelling, and erythema. In addition, most patients have systemic signs and symptoms of sepsis.
FIGURE 158-4 Sternal osteomyelitis caused by Staphylococcus epidermidis 5 weeks after sternotomy for aortocoronary bypass in a 72-year-old man.
The differential diagnosis of hematogenous sternal osteomyelitis includes immunologic processes typically presenting as systemic or multifocal inflammation of the sternum or the sternoclavicular or sternocostal joints (e.g., SAPHO [synovitis, acne, pustulosis, hyperostosis, osteitis], vasculitis, and chronic multifocal relapsing osteomyelitis).
DIAGNOSIS
In primary sternal osteomyelitis, the diagnostic workup does not differ from that in other types of hematogenous osteomyelitis (see above). When a patient has grown up in regions where tuberculosis is endemic, a specific workup for mycobacterial infection should be performed, especially if osteomyelitis had its onset after a blunt sternal trauma. In secondary sternal osteomyelitis, leukocyte counts may be normal, but the CRP level is >100 mg/L in most cases. Tissue sampling for microbiologic studies is crucial. In osteomyelitis associated with sternal wires, low-virulence microorganisms, such as coagulase-negative staphylococci, play an important role. In order to differentiate between colonization and infection, samples from at least three deep biopsies should be subjected to microbiologic examination. Superficial swab cultures are not diagnostic and may be misleading. No studies have compared the value of the various imaging modalities in suspected primary sternal osteomyelitis. However, MRI is the current gold standard for detection of each type of osteomyelitis.
|
TREATMENT |
STERNAL OSTEOMYELITIS |
In cases of deep sternal wound infection, antibiotic therapy should be started immediately after samples have been obtained for microbiologic analyses in order to control clinical sepsis. To protect a newly inserted heart valve, initial treatment should be directed against staphylococci, with consideration of the local susceptibility pattern. In centers with a high prevalence of methicillin-resistant S. aureus, vancomycin or daptomycin should be added to a broad-spectrum β-lactam drug. As soon as cultures of blood and/or deep wound biopsies have confirmed the pathogen’s identity and susceptibility pattern, treatment should be optimized and narrowed accordingly. Tables 158-1 and 158-2 show appropriate therapeutic choices for the most frequently identified microorganisms causing sternal osteomyelitis in the absence and presence, respectively, of an implanted device. In a recent observational study of patients with staphylococcal deep sternal wound infection, the use of a rifampin-containing regimen was predictive of success. The optimal duration of antibiotic therapy has not been established. In acute sternal osteomyelitis without hardware, a 6-week course is the rule. In patients with remaining sternal wires, treatment duration is generally prolonged to 3 months (Table 158-2). Like other types of tuberculous bone infection, tuberculous sternal osteomyelitis is treated for 6–12 months.
Primary sternal osteomyelitis can generally be treated without surgery. In contrast, in secondary sternal osteomyelitis, debridement is always required. This procedure should be performed by a team of experienced surgeons, since mediastinitis, bone infection, and skin and soft tissue damage may need to be treated during the same intervention.
PROGNOSIS
Primary sternal osteomyelitis poses a minimal mortality risk. In contrast, the in-hospital mortality rates from secondary sternal osteomyelitis are 15–30% after sternal surgery.
FOOT OSTEOMYELITIS
PATHOGENESIS
Osteomyelitis of the foot usually occurs in patients with diabetes, peripheral arterial insufficiency, or peripheral neuropathy and after foot surgery. These entities are often linked to each other, especially in diabetic patients with late complications. However, foot osteomyelitis is also seen in patients with isolated peripheral neuropathy and can manifest as implant-associated osteomyelitis in patients without comorbidity due to a deep wound infection after foot surgery (hallux valgus surgery, arthrodesis, total ankle arthroplasty). Foot osteomyelitis is acquired almost exclusively by the exogenous route. It is a complication of deep pressure ulcers and of impaired wound healing after surgery.
EPIDEMIOLOGY
The incidence of diabetic foot infection is 30–40 cases/1000 persons with diabetes per year. The condition starts with skin and soft tissue lesions and progresses to osteomyelitis, especially in patients with risk factors. About 60–80% of patients with diabetic foot infection have confirmed osteomyelitis. Diabetic foot osteomyelitis increases the risk of amputation. With adequate management of the early stage of diabetic foot infections, the rate of amputation can be lowered.
RISK FACTORS
Risk factors for diabetic foot infection are (1) peripheral motor, sensory, and autonomic neuropathy; (2) neuro-osteoarthropathic deformities (Charcot foot; Fig. 158-5); (3) arterial insufficiency; (4) uncontrolled hyperglycemia; (5) disabilities such as reduced vision; and (6) maladaptive behavior.
FIGURE 158-5 Neuropathic joint disease (Charcot foot) complicated by chronic foot osteomyelitis in a 78-year old woman with diabetes mellitus complicated by severe neuropathy.
MICROBIOLOGY
The correlation between cultures from bone biopsy and those from wound swabs or even deep soft tissue punctures is poor. Consistent results have been found in only 13–43% of cases in various studies. The correlation is better when S. aureus is isolated (40–50%) than when anaerobes (20–35%), gram-negative bacilli (20–30%), or coagulase-negative staphylococci (0–20%) are identified. When only bone biopsy samples are considered, the leading pathogens are S. aureus (30–40%), anaerobes (10–20%), and various gram-negative bacilli (30–40%). The precise distribution depends on whether the patient already has been treated with antibiotics. Anaerobes are especially prevalent in chronic wounds. Pretreatment typically selects for P. aeruginosa or enterococci.
DIAGNOSIS
In many cases, foot osteomyelitis can be diagnosed clinically, without imaging procedures. Most clinicians rely on the “probe-to-bone” test, which has a positive predictive value of ~90% in populations with a high pretest probability. Thus, in a patient with diabetes who is hospitalized for a chronic deep foot ulcer, the diagnosis of foot osteomyelitis is highly probable if bone can be directly touched with a metal instrument. In a patient with a lower pretest probability, MRI should be performed because of its high degree of sensitivity (80–100%) and specificity (80–90%). Plain radiography has a sensitivity of only 30–90% and a specificity of only 50–90%; it may be considered for follow-up of patients with confirmed diabetic foot osteomyelitis.
|
TREATMENT |
FOOT OSTEOMYELITIS |
As mentioned above, correlation between cultures of bone and those of wound swabs or wound punctures is poor. Antibiotic treatment should be based on bone culture. If no bone biopsy is performed, empirical therapy chosen in light of the most common infecting agents and the type of clinical syndrome should be given. Wound debridement combined with a 4- to 6-week course of antibiotics has been shown to render amputation unnecessary in about two-thirds of patients. According to the 2012 Infectious Diseases Society of America Clinical Practice Guideline for the Diagnosis and Treatment of Diabetic Foot Infections, the following management strategies should be considered. If a foot ulcer is clinically infected, prompt empirical antimicrobial therapy may prevent progression to osteomyelitis. When the risk of methicillin-resistant S. aureus is considered high, an agent active against these strains (e.g., vancomycin) should be chosen. If the patient has not recently received antibiotics, the spectrum of the selected antibiotic must include gram-positive cocci (e.g., clindamycin, ampicillin-sulbactam). If the patient has received antibiotics within the past month, the spectrum of empirical antibiotics should include gram-negative bacilli (e.g., clindamycin plus a fluoroquinolone). If the patient has risk factors for Pseudomonas infection (previous colonization, residence in a warm climate, frequent exposure of the foot to water), an empirical antipseudomonal agent (e.g., piperacillin-tazobactam, cefepime) is indicated. If osteomyelitis is suspected either on clinical grounds (probe to bone) or on the basis of imaging procedures (MRI), bone biopsy should be performed. If not all infected bone is surgically removed, the patient should be treated for 4–6 weeks in line with the identified pathogen(s) and their susceptibility. Treatment should initially be given by the IV route. Whether therapy can later be administered by the oral route depends on the bioavailability of oral drugs that cover the infecting agents. If dead bone cannot be removed, long-term therapy (at least 3 months) should be considered. In such cases, cure of osteomyelitis is usually the exception, and repetitive suppressive treatment may be needed.
159 |
Intraabdominal Infections and Abscesses |
Intraperitoneal infections generally arise because a normal anatomic barrier is disrupted. This disruption may occur when the appendix, a diverticulum, or an ulcer ruptures; when the bowel wall is weakened by ischemia, tumor, or inflammation (e.g., in inflammatory bowel disease); or with adjacent inflammatory processes, such as pancreatitis or pelvic inflammatory disease, in which enzymes (in the former case) or organisms (in the latter) may leak into the peritoneal cavity. Whatever the inciting event, once inflammation develops and organisms usually contained within the bowel or another organ enter the normally sterile peritoneal space, a predictable series of events takes place. Intraabdominal infections occur in two stages: peritonitis and—if the patient survives this stage and goes untreated—abscess formation. The types of microorganisms predominating in each stage of infection are responsible for the pathogenesis of disease.
PERITONITIS
Peritonitis is a life-threatening event that is often accompanied by bacteremia and sepsis syndrome (Chap. 325). The peritoneal cavity is large but is divided into compartments. The upper and lower peritoneal cavities are divided by the transverse mesocolon; the greater omentum extends from the transverse mesocolon and from the lower pole of the stomach to line the lower peritoneal cavity. The pancreas, duodenum, and ascending and descending colon are located in the anterior retroperitoneal space; the kidneys, ureters, and adrenals are found in the posterior retroperitoneal space. The other organs, including liver, stomach, gallbladder, spleen, jejunum, ileum, transverse and sigmoid colon, cecum, and appendix, are within the peritoneal cavity. The cavity is lined with a serous membrane that can serve as a conduit for fluids—a property exploited in peritoneal dialysis (Fig. 159-1). A small amount of serous fluid is normally present in the peritoneal space, with a protein content (consisting mainly of albumin) of <30 g/L and <300 white blood cells (WBCs, generally mononuclear cells) per microliter. In bacterial infections, leukocyte recruitment into the infected peritoneal cavity consists of an early influx of polymorphonuclear leukocytes (PMNs) and a prolonged subsequent phase of mononuclear cell migration. The phenotype of the infiltrating leukocytes during the course of inflammation is regulated primarily by resident-cell chemokine synthesis.
FIGURE 159-1 Diagram of the intraperitoneal spaces, showing the circulation of fluid and potential areas for abscess formation. Some compartments collect fluid or pus more often than others. These compartments include the pelvis (the lowest portion), the subphrenic spaces on the right and left sides, and Morrison’s pouch, which is a posterosuperior extension of the subhepatic spaces and is the lowest part of the paravertebral groove when a patient is recumbent. The falciform ligament separating the right and left subphrenic spaces appears to act as a barrier to the spread of infection; consequently, it is unusual to find bilateral subphrenic collections. (Reprinted with permission from B Lorber [ed]: Atlas of Infectious Diseases, vol VII: Intra-abdominal Infections, Hepatitis, and Gastroenteritis. Philadelphia, Current Medicine, 1996, p 1.13.)
PRIMARY (SPONTANEOUS) BACTERIAL PERITONITIS
Peritonitis is either primary (without an apparent source of contamination) or secondary. The types of organisms found and the clinical presentations of these two processes are different. In adults, primary bacterial peritonitis (PBP) occurs most commonly in conjunction with cirrhosis of the liver (frequently the result of alcoholism). However, the disease has been reported in adults with metastatic malignant disease, postnecrotic cirrhosis, chronic active hepatitis, acute viral hepatitis, congestive heart failure, systemic lupus erythematosus, and lymphedema as well as in patients with no underlying disease. Although PBP virtually always develops in patients with preexisting ascites, it is, in general, an uncommon event, occurring in ≤10% of cirrhotic patients. The cause of PBP has not been established definitively but is believed to involve hematogenous spread of organisms in a patient in whom a diseased liver and altered portal circulation result in a defect in the usual filtration function. Organisms multiply in ascites, a good medium for growth. The proteins of the complement cascade have been found in peritoneal fluid, with lower levels in cirrhotic patients than in patients with ascites of other etiologies. The opsonic and phagocytic properties of PMNs are diminished in patients with advanced liver disease. Cirrhosis is associated with alterations in the gut microbiota, including an increased prevalence of potentially pathogenic bacteria such as Enterobacteriaceae. Small-intestinal bacterial overgrowth is frequently present in advanced stages of liver cirrhosis and has been linked with pathologic bacterial translocation and PBP. Factors promoting these changes in cirrhosis may include deficiencies in Paneth cell defensins, reduced intestinal motility, decreased pancreatobiliary secretions, and portal-hypertensive enteropathy.
The presentation of PBP differs from that of secondary peritonitis. The most common manifestation is fever, which is reported in up to 80% of patients. Ascites is found but virtually always predates infection. Abdominal pain, an acute onset of symptoms, and peritoneal irritation during physical examination can be helpful diagnostically, but the absence of any of these findings does not exclude this often-subtle diagnosis. Nonlocalizing symptoms (such as malaise, fatigue, or encephalopathy) without another clear etiology should also prompt consideration of PBP in a susceptible patient. It is vital to sample the peritoneal fluid of any cirrhotic patient with ascites and fever. The finding of >250 PMNs/μL is diagnostic for PBP, according to Conn (http://jac.oxfordjournals.org/cgi/content/full/47/3/369). This criterion does not apply to secondary peritonitis (see below). The microbiology of PBP is also distinctive. While enteric gram-negative bacilli such as Escherichia coli are most commonly encountered, gram-positive organisms such as streptococci, enterococci, or even pneumococci are sometimes found. In an important development, widespread use of quinolones to prevent PBP in high-risk subgroups of patients, frequent hospitalizations, and exposure to broad-spectrum antibiotics have led to a change in flora of infections in patients with cirrhosis, with more gram-positive bacteria and extended-spectrum β-lactamase–producing Enterobacteriaceae in recent years. Risk factors for multiresistant infections include nosocomial origin of infection, long-term norfloxacin prophylaxis, recent infection with multiresistant bacteria, and recent use of β-lactam antibiotics. In PBP, a single organism is typically isolated; anaerobes are found less frequently in PBP than in secondary peritonitis, in which a mixed flora including anaerobes is the rule. In fact, if PBP is suspected and multiple organisms including anaerobes are recovered from the peritoneal fluid, the diagnosis must be reconsidered and a source of secondary peritonitis sought.
The diagnosis of PBP is not easy. It depends on the exclusion of a primary intraabdominal source of infection. Contrast-enhanced CT is useful in identifying an intraabdominal source for infection. It may be difficult to recover organisms from cultures of peritoneal fluid, presumably because the burden of organisms is low. However, the yield can be improved if 10 mL of peritoneal fluid is placed directly into a blood culture bottle. Because bacteremia frequently accompanies PBP, blood should be cultured simultaneously. To maximize the yield, culture samples should be collected prior to administration of antibiotics. No specific radiographic studies are helpful in the diagnosis of PBP. A plain film of the abdomen would be expected to show ascites. Chest and abdominal radiography should be performed in patients with abdominal pain to exclude free air, which signals a perforation (Fig. 159-2).
FIGURE 159-2 Pneumoperitoneum. Free air under the diaphragm on an upright chest film suggests the presence of a bowel perforation and associated peritonitis. (Image courtesy of Dr. John Braver; with permission.)
|
TREATMENT |
PRIMARY BACTERIAL PERITONITIS |
Treatment for PBP is directed at the isolate from blood or peritoneal fluid. Gram’s staining of peritoneal fluid often gives negative results in PBP. Therefore, until culture results become available, therapy should cover gram-negative aerobic bacilli and gram-positive cocci. Third-generation cephalosporins such as cefotaxime (2 g q8h, administered IV) provide reasonable initial coverage in moderately ill patients. Broad-spectrum antibiotics, such as penicillin/β-lactamase inhibitor combinations (e.g., piperacillin/tazobactam, 3.375 g q6h IV for adults with normal renal function) or ceftriaxone (2 g q24h IV), are also options. Broader empirical coverage aimed at resistant hospital-acquired gram-negative bacteria (e.g., treatment with carbapenem) may be appropriate for nosocomially acquired PBP until culture results become available. Empirical coverage for anaerobes is not necessary. A mortality benefit from albumin (1.5 g/kg of body weight within 6 h of detection and 1.0 g/kg on day 3) has been demonstrated for patients who present with serum creatinine levels ≥1 mg/dL, blood urea nitrogen levels ≥30 mg/dL, or total bilirubin levels ≥4 mg/dL but not for patients who do not meet these criteria. After the infecting organism is identified, therapy should be narrowed to target the specific pathogen. Patients with PBP usually respond within 72 h to appropriate antibiotic therapy. Antimicrobial treatment can be administered for as little as 5 days if rapid improvement occurs and blood cultures are negative, but a course of up to 2 weeks may be required for patients with bacteremia and for those whose improvement is slow. Persistence of WBCs in the ascitic fluid after therapy should prompt a search for additional diagnoses.
Prevention • PRIMARY PREVENTION Several observational studies and a meta-analysis raise the concern that proton pump inhibitor therapy may increase the risk of PBP. No prospective studies have yet addressed whether avoidance of such therapy may prevent PBP. Nonselective beta blockers may prevent secondary bacterial peritonitis. A 2012 guideline from the American Association for the Study of Liver Diseases recommends chronic antibiotic prophylaxis with a regimen described in the next section for patients who are at highest risk for PBP—that is, those with an ascitic-fluid total protein level <1.5 g/dL along with impaired renal function (creatinine, ≥1.2 mg/dL; blood urea nitrogen, ≥25 mg/dL; or serum sodium, ≤130 mg/dL) and/or liver failure (Child-Pugh score, ≥9; and bilirubin, ≥3 mg/dL). A 7-day course of antibiotic prophylaxis is recommended for patients with cirrhosis and gastrointestinal bleeding.
SECONDARY PREVENTION PBP has a high rate of recurrence. Up to 70% of patients experience a recurrence within 1 year. Antibiotic prophylaxis is recommended for patients with a history of PBP to reduce this rate to <20% and improve short-term survival rates. Prophylactic regimens for adults with normal renal function include fluoroquinolones (ciprofloxacin, 750 mg weekly; norfloxacin, 400 mg/d) or trimethoprim-sulfamethoxazole (one double-strength tablet daily). However, long-term administration of broad-spectrum antibiotics in this setting has been shown to increase the risk of severe staphylococcal infections.
SECONDARY PERITONITIS
Secondary peritonitis develops when bacteria contaminate the peritoneum as a result of spillage from an intraabdominal viscus. The organisms found almost always constitute a mixed flora in which facultative gram-negative bacilli and anaerobes predominate, especially when the contaminating source is colonic. Early in the course of infection, when the host response is directed toward containment, exudate containing fibrin and PMNs is found. Early death in this setting is attributable to gram-negative bacillary sepsis and to potent endotoxins circulating in the bloodstream (Chap. 325). Gram-negative bacilli, particularly E. coli, are common bloodstream isolates, but Bacteroides fragilis bacteremia also occurs. The severity of abdominal pain and the clinical course depend on the inciting process. The organisms isolated from the peritoneum also vary with the source of the initial process and the normal flora at that site. Secondary peritonitis can result primarily from chemical irritation and/or bacterial contamination. For example, as long as the patient is not achlorhydric, a ruptured gastric ulcer will release low-pH gastric contents that will serve as a chemical irritant. The normal flora of the stomach comprises the same organisms found in the oropharynx but in lower numbers. Thus, the bacterial burden in a ruptured ulcer is negligible compared with that in a ruptured appendix. The normal flora of the colon below the ligament of Treitz contains ~1011 anaerobic organisms/g of feces but only 108 aerobes/g; therefore, anaerobic species account for 99.9% of the bacteria. Leakage of colonic contents (pH 7–8) does not cause significant chemical peritonitis, but infection is intense because of the heavy bacterial load.
Depending on the inciting event, local symptoms may occur in secondary peritonitis—for example, epigastric pain from a ruptured gastric ulcer. In appendicitis (Chap. 356), the initial presenting symptoms are often vague, with periumbilical discomfort and nausea followed in a number of hours by pain more localized to the right lower quadrant. Unusual locations of the appendix (including a retrocecal position) can complicate this presentation further. Once infection has spread to the peritoneal cavity, pain increases, particularly with infection involving the parietal peritoneum, which is innervated extensively. Patients usually lie motionless, often with knees drawn up to avoid stretching the nerve fibers of the peritoneal cavity. Coughing and sneezing, which increase pressure within the peritoneal cavity, are associated with sharp pain. There may or may not be pain localized to the infected or diseased organ from which secondary peritonitis has arisen. Patients with secondary peritonitis generally have abnormal findings on abdominal examination, with marked voluntary and involuntary guarding of the anterior abdominal musculature. Later findings include tenderness, especially rebound tenderness. In addition, there may be localized findings in the area of the inciting event. In general, patients are febrile, with marked leukocytosis and a left shift of the WBCs to band forms.
While recovery of organisms from peritoneal fluid is easier in secondary than in primary peritonitis, a tap of the abdomen is rarely the procedure of choice in secondary peritonitis. An exception is in cases involving trauma, where the possibility of a hemoperitoneum may need to be excluded early. Emergent studies (such as abdominal CT) to find the source of peritoneal contamination should be undertaken if the patient is hemodynamically stable; unstable patients may require surgical intervention without prior imaging.
|
TREATMENT |
SECONDARY PERITONITIS |
Treatment for secondary peritonitis includes early administration of antibiotics aimed particularly at aerobic gram-negative bacilli and anaerobes (see below). Mild to moderate disease can be treated with many drugs covering these organisms, including broad-spectrum penicillin/β-lactamase inhibitor combinations (e.g., ticarcillin/clavulanate, 3.1 g q4–6h IV), cefoxitin (2 g q4–6h IV), or a combination of either a fluoroquinolone (e.g., levofloxacin, 750 mg q24h IV) or a third-generation cephalosporin (e.g., ceftriaxone, 2 g q24h IV) plus metronidazole (500 mg q8h IV). Patients in intensive care units should receive imipenem (500 mg q6h IV), meropenem (1 g q8h IV), or combinations of drugs, such as ampicillin plus metronidazole plus ciprofloxacin. The role of enterococci and Candida species in mixed infections is controversial. Secondary peritonitis usually requires both surgical intervention to address the inciting process and antibiotics to treat early bacteremia, to decrease the incidence of abscess formation and wound infection, and to prevent distant spread of infection. Although surgery is rarely indicated in PBP in adults, it may be life-saving in secondary peritonitis. Recombinant human activated protein C (APC) was considered at one time for treatment of severe sepsis from causes including secondary peritonitis but was withdrawn from the market in 2011 after it was determined that the drug was associated with an increased risk of bleeding and that evidence for its beneficial effects was inadequate. Thus APC should not be used for sepsis or septic shock outside randomized clinical trials.
Peritonitis may develop as a complication of abdominal surgeries. These infections may be accompanied by localizing pain and/or nonlocalizing signs or symptoms such as fever, malaise, anorexia, and toxicity. As a nosocomial infection, postoperative peritonitis may be associated with organisms such as staphylococci, components of the gram-negative hospital microflora, and the microbes that cause PBP and secondary peritonitis, as described above.
PERITONITIS IN PATIENTS UNDERGOING CONTINUOUS AMBULATORY PERITONEAL DIALYSIS
A third type of peritonitis arises in patients who are undergoing continuous ambulatory peritoneal dialysis (CAPD). Unlike PBP and secondary peritonitis, which are caused by endogenous bacteria, CAPD-associated peritonitis usually involves skin organisms. The pathogenesis of infection is similar to that of intravascular device–related infection, in which skin organisms migrate along the catheter, which both serves as an entry point and exerts the effects of a foreign body. Exit-site or tunnel infection may or may not accompany CAPD-associated peritonitis. Like PBP, CAPD-associated peritonitis is usually caused by a single organism. Peritonitis is, in fact, the most common reason for discontinuation of CAPD. Improvements in equipment design, especially the Y-set connector, have resulted in a decrease from one case of peritonitis per 9 months of CAPD to one case per 24 months.
The clinical presentation of CAPD peritonitis resembles that of secondary peritonitis in that diffuse pain and peritoneal signs are common. The dialysate is usually cloudy and contains >100 WBCs/μL, >50% of which are neutrophils. However, the number of cells depends in part on dwell time. According to a guideline from the International Society for Peritoneal Dialysis (2010), for patients undergoing automated peritoneal dialysis who present during their nighttime treatment and whose dwell time is much shorter than with CAPD, the clinician should use the percentage of PMNs rather than the absolute number of WBCs to diagnose peritonitis. As the normal peritoneum has very few PMNs, a proportion above 50% is strong evidence of peritonitis even if the absolute WBC count does not reach 100/μL. Meanwhile, patients undergoing automated peritoneal dialysis without a daytime exchange who present with abdominal pain may have no fluid to withdraw, in which case 1 L of dialysate should be infused and permitted to dwell a minimum of 1–2 h, then drained, examined for turbidity, and sent for cell count with differential and culture. The differential (with a shortened dwell time) may be more useful than the absolute WBC count. In equivocal cases or in patients with systemic or abdominal symptoms in whom the effluent appears clear, a second exchange is performed, with a dwell time of at least 2 h. Clinical judgment should guide initiation of therapy.
The most common organisms are Staphylococcus species, which accounted for ~45% of cases in one series. Historically, coagulase-negative staphylococcal species were identified most commonly in these infections, but these isolates have more recently been decreasing in frequency. Staphylococcus aureus is more often involved among patients who are nasal carriers of the organism than among those who are not, and this organism is the most common pathogen in overt exit-site infections. Gram-negative bacilli and fungi such as Candida species are also found. Vancomycin-resistant enterococci and vancomycin-intermediate S. aureus have been reported to produce peritonitis in CAPD patients. The finding of more than one organism in dialysate culture should prompt evaluation for secondary peritonitis. As with PBP, culture of dialysate fluid in blood culture bottles improves the yield. To facilitate diagnosis, several hundred milliliters of removed dialysis fluid should be concentrated by centrifugation before culture.
|
TREATMENT |
CAPD PERITONITIS |
Empirical therapy for CAPD peritonitis should be directed at S. aureus, coagulase-negative Staphylococcus, and gram-negative bacilli until the results of cultures become available. Guidelines suggest that agents should be chosen on the basis of local experience with resistant organisms. In some centers, a first-generation cephalosporin such as cefazolin (for gram-positive bacteria) and a fluoroquinolone or a third-generation cephalosporin such as ceftazidime (for gram-negative bacteria) may be reasonable; in areas with high rates of infection with methicillin-resistant S. aureus, vancomycin should be used instead of cefazolin, and gram-negative coverage may need to be broadened—e.g., with an aminoglycoside, ceftazidime, cefepime, or carbapenem. Broad coverage including vancomycin should be particularly considered for toxic patients and for those with exit-site infections. Vancomycin should also be included in the regimen if the patient has a history of colonization or infection with methicillin-resistant S. aureus or has a history of severe allergy to penicillins and cephalosporins. Loading doses are administered intraperitoneally; doses depend on the dialysis method and the patient’s renal function. Antibiotics are given either continuously (i.e., with each exchange) or intermittently (i.e., once daily, with the dose allowed to remain in the peritoneal cavity for at least 6 h). If the patient is severely ill, IV antibiotics should be added at doses appropriate for the patient’s degree of renal failure. The clinical response to an empirical treatment regimen should be rapid; if the patient has not responded after 48–96 h of treatment, new samples should be collected for cell counts and cultures, and catheter removal should be considered. For patients who lack exit-site or tunnel infection, the typical duration of antibiotic treatment is 14 days. For patients with exit-site or tunnel infection, catheter removal should be considered, and a longer duration of antibiotic therapy (up to 21 days) may be appropriate. In fungal infections, the catheter should be removed immediately.
TUBERCULOUS PERITONITIS
See Chap. 202.
INTRAABDOMINAL ABSCESSES
INTRAPERITONEAL ABSCESSES
Abscess formation is common in untreated peritonitis if overt gram-negative sepsis either does not develop or develops but is not fatal. In experimental models of abscess formation, mixed aerobic and anaerobic organisms have been implanted intraperitoneally. Without therapy directed at anaerobes, animals develop intraabdominal abscesses. As in humans, these experimental abscesses may stud the peritoneal cavity, lie within the omentum or mesentery, or even develop on the surface of or within viscera such as the liver.
Pathogenesis and Immunity There is often disagreement about whether an abscess represents a disease state or a host response. In a sense, it represents both: while an abscess is an infection in which viable infecting organisms and PMNs are contained in a fibrous capsule, it is also a process by which the host confines microbes to a limited space, thereby preventing further spread of infection. In any event, abscesses do cause significant symptoms, and patients with abscesses can be quite ill. Experimental work has helped to define both the host cells and the bacterial virulence factors responsible—most notably in the case of B. fragilis. This organism, although accounting for only 0.5% of the normal colonic flora, is the anaerobe most frequently isolated from intraabdominal infections, is especially prominent in abscesses, and is the most common anaerobic bloodstream isolate. On clinical grounds, therefore, B. fragilis appears to be uniquely virulent. Moreover, B. fragilis acts alone to cause abscesses in animal models of intraabdominal infection, whereas most other Bacteroides species must act synergistically with a facultative organism to induce abscess formation.
Of the several virulence factors identified in B. fragilis, one is critical: the capsular polysaccharide complex found on the bacterial surface. This complex comprises at least eight distinct surface polysaccharides. Structural analysis of these polysaccharides has shown an unusual motif of oppositely charged sugars. Polysaccharides having these zwitterionic characteristics, such as polysaccharide A, evoke a host response in the peritoneal cavity that localizes bacteria into abscesses. B. fragilis and polysaccharide A have been found to adhere to primary mesothelial cells in vitro; this adherence, in turn, stimulates the production of tumor necrosis factor α and intercellular adhesion molecule 1 by peritoneal macrophages. Although abscesses characteristically contain PMNs, the process of abscess induction depends on the stimulation of T lymphocytes by these unique zwitterionic polysaccharides. The stimulated CD4+ T lymphocytes secrete leukoattractant cytokines and chemokines. The alternative pathway of complement and fibrinogen also participate in abscess formation.
While antibodies to the capsular polysaccharide complex enhance bloodstream clearance of B. fragilis, CD4+ T cells are critical in immunity to abscesses. When administered subcutaneously, B. fragilis polysaccharide A has immunomodulatory characteristics and stimulates CD4+ T regulatory cells via an interleukin 2–dependent mechanism to produce interleukin 10. Interleukin 10 downregulates the inflammatory response, thereby preventing abscess formation.
Clinical Presentation Of all intraabdominal abscesses, 74% are intraperitoneal or retroperitoneal and are not visceral. Most intraperitoneal abscesses result from fecal spillage from a colonic source, such as an inflamed appendix. Abscesses can also arise from other processes. They usually form within weeks of the development of peritonitis and may be found in a variety of locations from omentum to mesentery, pelvis to psoas muscles, and subphrenic space to a visceral organ such as the liver, where they may develop either on the surface of the organ or within it. Periappendiceal and diverticular abscesses occur commonly. Diverticular abscesses are least likely to rupture. Infections of the female genital tract and pancreatitis are also among the more common causative events. When abscesses occur in the female genital tract—either as a primary infection (e.g., tuboovarian abscess) or as an infection extending into the pelvic cavity or peritoneum—B. fragilis figures prominently among the organisms isolated. B. fragilis is not found in large numbers in the normal vaginal flora. For example, it is encountered less commonly in pelvic inflammatory disease and endometritis without an associated abscess. In pancreatitis with leakage of damaging pancreatic enzymes, inflammation is prominent. Therefore, clinical findings such as fever, leukocytosis, and even abdominal pain do not distinguish pancreatitis itself from complications such as pancreatic pseudocyst, pancreatic abscess (Chap. 371), or intraabdominal collections of pus. Especially in cases of necrotizing pancreatitis, in which the incidence of local pancreatic infection may be as high as 30%, needle aspiration under CT guidance is performed to sample fluid for culture. Many centers prescribe preemptive antibiotics for patients with necrotizing pancreatitis. Imipenem is frequently used for this purpose because it reaches high tissue levels in the pancreas (although it is not unique in this regard). Recent randomized controlled studies have not demonstrated a benefit from this practice, and some guidelines no longer recommend preemptive antibiotics for patients with acute pancreatitis. If needle aspiration yields infected fluid in the setting of acute necrotizing pancreatitis, antibiotic treatment is appropriate in conjunction with surgical and/or percutaneous drainage of infected material. Infected pseudocysts that occur remotely from acute pancreatitis are unlikely to be associated with significant amounts of necrotic tissue and may be treated with either surgical or percutaneous catheter drainage in conjunction with appropriate antibiotic therapy.
Diagnosis Scanning procedures have considerably facilitated the diagnosis of intraabdominal abscesses. Abdominal CT probably has the highest yield, although ultrasonography is particularly useful for the right upper quadrant, kidneys, and pelvis. Both indium-labeled WBCs and gallium tend to localize in abscesses and may be useful in finding a collection. Because gallium is taken up in the bowel, indium-labeled WBCs may have a slightly greater yield for abscesses near the bowel. Neither indium-labeled WBC nor gallium scans serve as a basis for a definitive diagnosis, however; both need to be followed by other, more specific studies, such as CT, if an area of possible abnormality is identified. Abscesses contiguous with or contained within diverticula are particularly difficult to diagnose with scanning procedures. Although barium should not be injected if a perforation is suspected, a barium enema occasionally may detect a diverticular abscess not diagnosed by other procedures. If one study is negative, a second study sometimes reveals a collection. Although exploratory laparotomy has been less commonly used since the advent of CT, this procedure still must be undertaken on occasion if an abscess is strongly suspected on clinical grounds.
|
TREATMENT |
INTRAPERITONEAL ABSCESSES |
An algorithm for the management of patients with intraabdominal (including intraperitoneal) abscesses by percutaneous drainage is presented in Fig. 159-3. The treatment of intraabdominal infections involves the determination of the initial focus of infection, the administration of broad-spectrum antibiotics targeting the organisms involved, and the performance of a drainage procedure if one or more definitive abscesses have formed. Antimicrobial therapy, in general, is adjunctive to drainage and/or surgical correction of an underlying lesion or process in intraabdominal abscesses. Unlike the intraabdominal abscesses resulting from most causes, for which drainage of some kind is generally required, abscesses associated with diverticulitis usually wall off locally after rupture of a diverticulum, so that surgical intervention is not routinely required.
FIGURE 159-3 Algorithm for the management of patients with intraabdominal abscesses using percutaneous drainage. Antimicrobial therapy should be administered concomitantly. (Reprinted with permission from B Lorber [ed]: Atlas of Infectious Diseases, vol VII: Intra-abdominal Infections, Hepatitis, and Gastroenteritis. Philadelphia, Current Medicine, 1996, p 1.30, as adapted from OD Rotstein, RL Simmons, in SL Gorbach et al [eds]: Infectious Diseases. Philadelphia, Saunders, 1992, p 668.)
A number of agents exhibit excellent activity against aerobic gram-negative bacilli. Because death in intraabdominal sepsis is linked to gram-negative bacteremia, empirical therapy for intraabdominal infection always needs to include adequate coverage of gram-negative aerobic, facultative, and anaerobic organisms. Even if anaerobes are not cultured from clinical specimens, they still must be covered by the therapeutic regimen. Empirical antibiotic therapy should be the same as that discussed above for secondary peritonitis.
VISCERAL ABSCESSES
Liver Abscesses The liver is the organ most subject to the development of abscesses. In one study of 540 intraabdominal abscesses, 26% were visceral. Liver abscesses made up 13% of the total number, or 48% of all visceral abscesses. Liver abscesses may be solitary or multiple; they may arise from hematogenous spread of bacteria or from local spread from contiguous sites of infection within the peritoneal cavity. In the past, appendicitis with rupture and subsequent spread of infection was the most common source for a liver abscess. Currently, associated disease of the biliary tract is most common. Pylephlebitis (suppurative thrombosis of the portal vein), usually arising from infection in the pelvis but sometimes from infection elsewhere in the peritoneal cavity, is another common source for bacterial seeding of the liver.
Fever is the most common presenting sign of liver abscess. Some patients, particularly those with associated disease of the biliary tract, have symptoms and signs localized to the right upper quadrant, including pain, guarding, punch tenderness, and even rebound tenderness. Nonspecific symptoms, such as chills, anorexia, weight loss, nausea, and vomiting, may also develop. Only 50% of patients with liver abscesses, however, have hepatomegaly, right-upper-quadrant tenderness, or jaundice; thus, one-half of patients have no symptoms or signs to direct attention to the liver. Fever of unknown origin may be the only manifestation of liver abscess, especially in the elderly. Diagnostic studies of the abdomen, especially the right upper quadrant, should be a part of any workup for fever of unknown origin. The single most reliable laboratory finding is an elevated serum concentration of alkaline phosphatase, which is documented in 70% of patients with liver abscesses. Other tests of liver function may yield normal results, but 50% of patients have elevated serum levels of bilirubin, and 48% have elevated concentrations of aspartate aminotransferase. Other laboratory findings include leukocytosis in 77% of patients, anemia (usually normochromic, normocytic) in 50%, and hypoalbuminemia in 33%. Concomitant bacteremia is found in one-third to one-half of patients. A liver abscess is sometimes suggested by chest radiography, especially if a new elevation of the right hemidiaphragm is seen; other suggestive findings include a right basilar infiltrate and a right pleural effusion.
Imaging studies are the most reliable methods for diagnosing liver abscesses. These studies include ultrasonography, CT (Fig. 159-4), indium-labeled WBC or gallium scan, and MRI. More than one such study may be required.
FIGURE 159-4 Multilocular liver abscess on CT scan. Multiple or multilocular abscesses are more common than solitary abscesses. (Reprinted with permission from B Lorber [ed]: Atlas of Infectious Diseases, vol VII: Intra-abdominal Infections, Hepatitis, and Gastroenteritis. Philadelphia, Current Medicine, 1996, Fig. 1.22.)
![]() Organisms recovered from liver abscesses vary with the source. In liver infection arising from the biliary tree, enteric gram-negative aerobic bacilli and enterococci are common isolates. Klebsiella pneumoniae liver abscess has been well described in Southeast Asia for more than 20 years and has become an emerging syndrome in North America and elsewhere. These community-acquired infections have been linked to a virulent hypermucoviscous K. pneumoniae phenotype and to a specific genotype. The typical syndrome includes liver abscess, bacteremia, and metastatic infection. Ampicillin/amoxicillin therapy started within the previous 30 days has been associated with increased risk for this syndrome, presumably because of selection for the causative strain. Unless previous surgery has been performed, anaerobes are not generally involved in liver abscesses arising from biliary infections. In contrast, in liver abscesses arising from pelvic and other intraperitoneal sources, a mixed flora including both aerobic and anaerobic species is common; B. fragilis is the species most frequently isolated. With hematogenous spread of infection, usually only a single organism is encountered; this species may be S. aureus or a streptococcal species such as one in the Streptococcus milleri group. Results of cultures obtained from drain sites are not reliable for defining the etiology of infections. Liver abscesses may also be caused by Candida species; such abscesses usually follow fungemia in patients receiving chemotherapy for cancer and often present when PMNs return after a period of neutropenia. Amebic liver abscesses are not an uncommon problem (Chap. 247). Amebic serologic testing gives positive results in >95% of cases. In addition, polymerase chain reaction (PCR) testing has been used in recent years. Negative results from these studies help to exclude this diagnosis.
Organisms recovered from liver abscesses vary with the source. In liver infection arising from the biliary tree, enteric gram-negative aerobic bacilli and enterococci are common isolates. Klebsiella pneumoniae liver abscess has been well described in Southeast Asia for more than 20 years and has become an emerging syndrome in North America and elsewhere. These community-acquired infections have been linked to a virulent hypermucoviscous K. pneumoniae phenotype and to a specific genotype. The typical syndrome includes liver abscess, bacteremia, and metastatic infection. Ampicillin/amoxicillin therapy started within the previous 30 days has been associated with increased risk for this syndrome, presumably because of selection for the causative strain. Unless previous surgery has been performed, anaerobes are not generally involved in liver abscesses arising from biliary infections. In contrast, in liver abscesses arising from pelvic and other intraperitoneal sources, a mixed flora including both aerobic and anaerobic species is common; B. fragilis is the species most frequently isolated. With hematogenous spread of infection, usually only a single organism is encountered; this species may be S. aureus or a streptococcal species such as one in the Streptococcus milleri group. Results of cultures obtained from drain sites are not reliable for defining the etiology of infections. Liver abscesses may also be caused by Candida species; such abscesses usually follow fungemia in patients receiving chemotherapy for cancer and often present when PMNs return after a period of neutropenia. Amebic liver abscesses are not an uncommon problem (Chap. 247). Amebic serologic testing gives positive results in >95% of cases. In addition, polymerase chain reaction (PCR) testing has been used in recent years. Negative results from these studies help to exclude this diagnosis.
|
TREATMENT |
LIVER ABSCESSES |
(Fig. 159-3) Drainage is the mainstay of therapy for intraabdominal abscesses, including liver abscesses; the approach can be either percutaneous (with a pigtail catheter kept in place or possibly with a device that can perform pulse lavage to fragment and evacuate the semisolid contents of a liver abscess) or surgical. However, there is growing interest in medical management alone for pyogenic liver abscesses. The drugs used for empirical therapy include the same ones used in intraabdominal sepsis and secondary bacterial peritonitis. Usually, blood cultures and a diagnostic aspirate of abscess contents should be obtained before the initiation of empirical therapy, with antibiotic choices adjusted when the results of Gram’s staining and culture become available. Cases treated without definitive drainage generally require longer courses of antibiotic therapy. When percutaneous drainage was compared with open surgical drainage, the average length of hospital stay for the former was almost twice that for the latter, although both the time required for fever to resolve and the mortality rate were the same for the two procedures. The mortality rate was appreciable despite treatment, averaging 15%. Several factors predict the failure of percutaneous drainage and therefore may favor primary surgical intervention. These factors include the presence of multiple, sizable abscesses; viscous abscess contents that tend to plug the catheter; associated disease (e.g., disease of the biliary tract) requiring surgery; the presence of yeast; communication with an untreated obstructed biliary tree; or the lack of a clinical response to percutaneous drainage in 4–7 days.
Treatment of candidal liver abscesses often entails initial administration of amphotericin B or liposomal amphotericin, with subsequent fluconazole therapy (Chap. 240). In some cases, therapy with fluconazole alone (6 mg/kg daily) may be used—e.g., in clinically stable patients whose infecting isolate is susceptible to this drug.
Splenic Abscesses Splenic abscesses are much less common than liver abscesses. The incidence of splenic abscesses has ranged from 0.14% to 0.7% in various autopsy series. The clinical setting and the organisms isolated usually differ from those for liver abscesses. The degree of clinical suspicion for splenic abscess needs to be high because this condition is frequently fatal if left untreated. Even in the most recently published series, diagnosis was made only at autopsy in 37% of cases. Although splenic abscesses may arise occasionally from contiguous spread of infection or from direct trauma to the spleen, hematogenous spread of infection is more common. Bacterial endocarditis is the most common associated infection (Chap. 155). Splenic abscesses can develop in patients who have received extensive immunosuppressive therapy (particularly those with malignancy involving the spleen) and in patients with hemoglobinopathies or other hematologic disorders (especially sickle cell anemia).
Although ~50% of patients with splenic abscesses have abdominal pain, the pain is localized to the left upper quadrant in only one-half of these cases. Splenomegaly is found in ~50% of cases. Fever and leukocytosis are generally present; the development of fever preceded diagnosis by an average of 20 days in one series. Left-sided chest findings may include abnormalities to auscultation, and chest radiographic findings may include an infiltrate or a left-sided pleural effusion. CT scan of the abdomen has been the most sensitive diagnostic tool. Ultrasonography can yield the diagnosis but is less sensitive. Liver-spleen scan or gallium scan may also be useful. Streptococcal species are the most common bacterial isolates from splenic abscesses, followed by S. aureus—presumably reflecting the associated endocarditis. An increase in the prevalence of gram-negative aerobic isolates from splenic abscesses has been reported; these organisms often derive from a urinary tract focus, with associated bacteremia, or from another intraabdominal source. Salmonella species are seen fairly commonly, especially in patients with sickle cell hemoglobinopathy. Anaerobic species accounted for only 5% of isolates in the largest collected series, but the reporting of a number of “sterile abscesses” may indicate that optimal techniques for the isolation of anaerobes were not used.
|
TREATMENT |
SPLENIC ABSCESSES |
Because of the high mortality figures reported for splenic abscesses, splenectomy with adjunctive antibiotics has traditionally been considered standard treatment and remains the best approach for complex, multilocular abscesses or multiple abscesses. However, percutaneous drainage has worked well for single, small (<3-cm) abscesses in some studies and may also be useful for patients with high surgical risk. Patients undergoing splenectomy should be vaccinated against encapsulated organisms (Streptococcus pneumoniae, Haemophilus influenzae, Neisseria meningitidis). The most important factor in successful treatment of splenic abscesses is early diagnosis.
Perinephric and Renal Abscesses Perinephric and renal abscesses are not common. The former accounted for only ~0.02% of hospital admissions and the latter for ~0.2% in Altemeier’s series of 540 intraabdominal abscesses. Before antibiotics became available, most renal and perinephric abscesses were hematogenous in origin, usually complicating prolonged bacteremia, with S. aureus most commonly recovered. Now, in contrast, >75% of perinephric and renal abscesses arise from a urinary tract infection. Infection ascends from the bladder to the kidney, with pyelonephritis preceding abscess development. Bacteria may directly invade the renal parenchyma from medulla to cortex. Local vascular channels within the kidney may also facilitate the transport of organisms. Areas of abscess developing within the parenchyma may rupture into the perinephric space. The kidneys and adrenal glands are surrounded by a layer of perirenal fat that, in turn, is surrounded by Gerota’s fascia, which extends superiorly to the diaphragm and inferiorly to the pelvic fat. Abscesses extending into the perinephric space may track through Gerota’s fascia into the psoas or transversalis muscles, into the anterior peritoneal cavity, superiorly to the subdiaphragmatic space, or inferiorly to the pelvis. Of the risk factors that have been associated with the development of perinephric abscesses, the most important is concomitant nephrolithiasis obstructing urinary flow. Of patients with perinephric abscess, 20–60% have renal stones. Other structural abnormalities of the urinary tract, prior urologic surgery, trauma, and diabetes mellitus have also been identified as risk factors.
The organisms most frequently encountered in perinephric and renal abscesses are E. coli, Proteus species, and Klebsiella species. E. coli, the aerobic species most commonly found in the colonic flora, seems to have unique virulence properties in the urinary tract, including factors promoting adherence to uroepithelial cells. The urease of Proteus species splits urea, thereby creating a more alkaline and more hospitable environment for bacterial proliferation. Proteus species are frequently found in association with large struvite stones caused by the precipitation of magnesium ammonium sulfate in an alkaline environment. These stones serve as a nidus for recurrent urinary tract infection. Although a single bacterial species is usually recovered from a perinephric or renal abscess, multiple species may also be found. If a urine culture is not contaminated with periurethral flora and is found to contain more than one organism, a perinephric abscess or renal abscess should be considered in the differential diagnosis. Urine cultures may also be polymicrobial in cases of bladder diverticulum.
Candida species can cause renal abscesses. This fungus may spread to the kidney hematogenously or by ascension from the bladder. The hallmark of the latter route of infection is ureteral obstruction with large fungal balls.
The presentation of perinephric and renal abscesses is quite nonspecific. Flank pain and abdominal pain are common. At least 50% of patients are febrile. Pain may be referred to the groin or leg, particularly with extension of infection. The diagnosis of perinephric abscess, like that of splenic abscess, is frequently delayed, and the mortality rate in some series is appreciable, although lower than in the past. Perinephric or renal abscess should be most seriously considered when a patient presents with symptoms and signs of pyelonephritis and remains febrile after 4 or 5 days of treatment. Moreover, when a urine culture yields a polymicrobial flora, when a patient is known to have renal stones, or when fever and pyuria coexist with a sterile urine culture, these diagnoses should be entertained.
Renal ultrasonography and abdominal CT are the most useful diagnostic modalities. If a renal or perinephric abscess is diagnosed, nephrolithiasis should be excluded, especially when a high urinary pH suggests the presence of a urea-splitting organism.
|
TREATMENT |
PERINEPHRIC AND RENAL ABSCESSES |
Treatment for perinephric and renal abscesses, like that for other intraabdominal abscesses, includes drainage of pus and antibiotic therapy directed at the organism(s) recovered. For perinephric abscesses, percutaneous drainage is usually successful.
Psoas Abscesses The psoas muscle is another location in which abscesses are encountered. Psoas abscesses may arise from a hematogenous source, by contiguous spread from an intraabdominal or pelvic process, or by contiguous spread from nearby bony structures (e.g., vertebral bodies). Associated osteomyelitis due to spread from bone to muscle or from muscle to bone is common in psoas abscesses. When Pott’s disease was common, Mycobacterium tuberculosis was a frequent cause of psoas abscess. Currently, either S. aureus or a mixture of enteric organisms including aerobic and anaerobic gram-negative bacilli is usually isolated from psoas abscesses in the United States. S. aureus is most likely to be isolated when a psoas abscess arises from hematogenous spread or a contiguous focus of osteomyelitis; a mixed enteric flora is the most likely etiology when the abscess has an intraabdominal or pelvic source. Patients with psoas abscesses frequently present with fever, lower abdominal or back pain, or pain referred to the hip or knee. CT is the most useful diagnostic technique.
|
TREATMENT |
PSOAS ABSCESSES |
Treatment includes surgical drainage and the administration of an antibiotic regimen directed at the inciting organism(s).
Pancreatic Abscesses See Chap. 371.
ACKNOWLEDGMENT
The substantial contributions of Dori F. Zaleznik, MD, to this chapter in previous editions are gratefully acknowledged.
160 |
Acute Infectious Diarrheal Diseases and Bacterial Food Poisoning |
![]() Acute diarrheal disease is a leading cause of illness globally and is associated with an estimated 1.4 million deaths per year. Among children <5 years of age, diarrheal disease is second only to lower respiratory infection as the most common infectious cause of death. The incidence rate of diarrheal disease among children in low- and middle-income countries is estimated to be 2.9 episodes per child per year, for a total of 1.7 billion episodes annually. The morbidity from diarrhea is also significant. Recurrent intestinal infections are associated with physical and mental stunting, wasting, micronutrient deficiencies, and malnutrition. In short, diarrheal disease is a driving factor in global morbidity and mortality.
Acute diarrheal disease is a leading cause of illness globally and is associated with an estimated 1.4 million deaths per year. Among children <5 years of age, diarrheal disease is second only to lower respiratory infection as the most common infectious cause of death. The incidence rate of diarrheal disease among children in low- and middle-income countries is estimated to be 2.9 episodes per child per year, for a total of 1.7 billion episodes annually. The morbidity from diarrhea is also significant. Recurrent intestinal infections are associated with physical and mental stunting, wasting, micronutrient deficiencies, and malnutrition. In short, diarrheal disease is a driving factor in global morbidity and mortality.
The wide range of clinical manifestations of acute gastrointestinal illnesses is matched by the wide variety of infectious agents involved, including viruses, bacteria, and parasites (Table 160-1). This chapter discusses factors that enable gastrointestinal pathogens to cause disease, reviews host defense mechanisms, and delineates an approach to the evaluation and treatment of patients presenting with acute diarrhea. Individual organisms causing acute gastrointestinal illnesses are discussed in detail in subsequent chapters.
|
GASTROINTESTINAL PATHOGENS CAUSING ACUTE DIARRHEA |
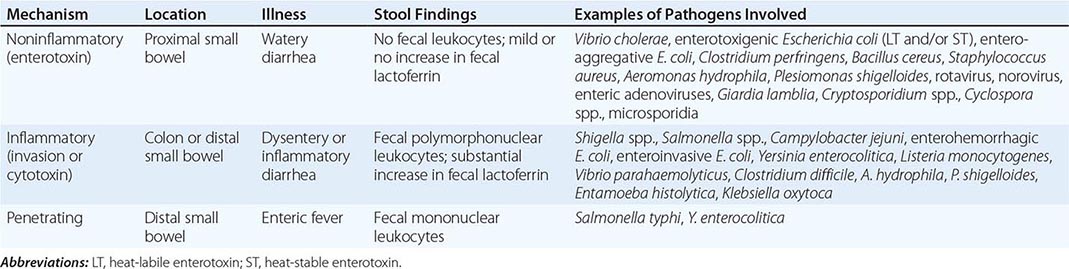
PATHOGENIC MECHANISMS
Enteric pathogens have developed a variety of tactics to overcome host defenses. Understanding the virulence factors employed by these organisms is important in the diagnosis and treatment of clinical disease.
INOCULUM SIZE
The number of microorganisms that must be ingested to cause disease varies considerably from species to species. For Shigella, enterohemorrhagic Escherichia coli, Giardia lamblia, or Entamoeba, as few as 10–100 bacteria or cysts can produce infection, while 105–108 Vibrio cholerae organisms must be ingested to cause disease. The infective dose of Salmonella varies widely, depending on the species, host, and food vehicle. The ability of organisms to overcome host defenses has important implications for transmission; Shigella, enterohemorrhagic E. coli, Entamoeba, and Giardia can spread by person-to-person contact, whereas under some circumstances Salmonella may have to grow in food for several hours before reaching an effective infectious dose.
ADHERENCE
Many organisms must adhere to the gastrointestinal mucosa as an initial step in the pathogenic process; thus, organisms that can compete with the normal bowel flora and colonize the mucosa have an important advantage in causing disease. Specific cell-surface proteins involved in attachment of bacteria to intestinal cells are important virulence determinants. V. cholerae, for example, adheres to the brush border of small-intestinal enterocytes via specific surface adhesins, including the toxin-coregulated pilus and other accessory colonization factors. Enterotoxigenic E. coli, which causes watery diarrhea, produces an adherence protein called colonization factor antigen that is necessary for colonization of the upper small intestine by the organism prior to the production of enterotoxin. Enteropathogenic E. coli, an agent of diarrhea in young children, and enterohemorrhagic E. coli, which causes hemorrhagic colitis and the hemolytic-uremic syndrome, produce virulence determinants that allow these organisms to attach to and efface the brush border of the intestinal epithelium.
TOXIN PRODUCTION
The production of one or more exotoxins is important in the pathogenesis of numerous enteric organisms. Such toxins include enterotoxins, which cause watery diarrhea by acting directly on secretory mechanisms in the intestinal mucosa; cytotoxins, which cause destruction of mucosal cells and associated inflammatory diarrhea; and neurotoxins, which act directly on the central or peripheral nervous system.
The prototypical enterotoxin is cholera toxin, a heterodimeric protein composed of one A and five B subunits. The A subunit contains the enzymatic activity of the toxin, while the B subunit pentamer binds holotoxin to the enterocyte surface receptor, the ganglioside GM1. After the binding of holotoxin, a fragment of the A subunit is translocated across the eukaryotic cell membrane into the cytoplasm, where it catalyzes the adenosine diphosphate ribosylation of a guanosine triphosphate–binding protein and causes persistent activation of adenylate cyclase. The end result is an increase of cyclic adenosine monophosphate in the intestinal mucosa, which increases Cl– secretion and decreases Na+ absorption, leading to a loss of fluid and the production of diarrhea.
Enterotoxigenic strains of E. coli may produce a protein called heat-labile enterotoxin (LT) that is similar to cholera toxin and causes secretory diarrhea by the same mechanism. Alternatively, enterotoxigenic strains of E. coli may produce heat-stable enterotoxin (ST), one form of which causes diarrhea by activation of guanylate cyclase and elevation of intracellular cyclic guanosine monophosphate. Some enterotoxigenic strains of E. coli produce both LT and ST.
Bacterial cytotoxins, in contrast, destroy intestinal mucosal cells and produce the syndrome of dysentery, with bloody stools containing inflammatory cells. Enteric pathogens that produce such cytotoxins include Shigella dysenteriae type 1, Vibrio parahaemolyticus, and Clostridium difficile. S. dysenteriae type 1 and Shiga toxin–producing strains of E. coli produce potent cytotoxins and have been associated with outbreaks of hemorrhagic colitis and hemolytic-uremic syndrome.
Neurotoxins are usually produced by bacteria outside the host and therefore cause symptoms soon after ingestion. Included are the staphylococcal and Bacillus cereus toxins, which act on the central nervous system to produce vomiting.
INVASION
Dysentery may result not only from the production of cytotoxins but also from bacterial invasion and destruction of intestinal mucosal cells. Infections due to Shigella and enteroinvasive E. coli are characterized by the organisms’ invasion of mucosal epithelial cells, intraepithelial multiplication, and subsequent spread to adjacent cells. Salmonella causes inflammatory diarrhea by invasion of the bowel mucosa but generally is not associated with the destruction of enterocytes or the full clinical syndrome of dysentery. Salmonella typhi and Yersinia enterocolitica can penetrate intact intestinal mucosa, multiply intracellularly in Peyer’s patches and intestinal lymph nodes, and then disseminate through the bloodstream to cause enteric fever, a syndrome characterized by fever, headache, relative bradycardia, abdominal pain, splenomegaly, and leukopenia.
HOST DEFENSES
Given the enormous number of microorganisms ingested with every meal, the normal host must combat a constant influx of potential enteric pathogens. Studies of infections in patients with alterations in defense mechanisms have led to a greater understanding of the variety of ways in which the normal host can protect itself against disease.
INTESTINAL MICROBIOTA
The large numbers of bacteria that normally inhabit the intestine (the intestinal microbiota) act as an important host defense mechanism, preventing colonization by potential enteric pathogens. Persons with fewer intestinal bacteria, such as infants who have not yet developed normal enteric colonization or patients receiving antibiotics, are at significantly greater risk of developing infections with enteric pathogens. The composition of the intestinal microbiota is as important as the number of organisms present. More than 99% of the normal colonic microbiota is made up of anaerobic bacteria, and the acidic pH and volatile fatty acids produced by these organisms appear to be critical elements in resistance to colonization.
GASTRIC ACID
The acidic pH of the stomach is an important barrier to enteric pathogens, and an increased frequency of infections due to Salmonella, G. lamblia, and a variety of helminths has been reported among patients who have undergone gastric surgery or are achlorhydric for some other reason. Neutralization of gastric acid with antacids, proton pump inhibitors, or H2 blockers—a common practice in the management of hospitalized patients—similarly increases the risk of enteric colonization. In addition, some microorganisms can survive the extreme acidity of the gastric environment; rotavirus, for example, is highly stable to acidity.
INTESTINAL MOTILITY
Normal peristalsis is the major mechanism for clearance of bacteria from the proximal small intestine. When intestinal motility is impaired (e.g., by treatment with opiates or other antimotility drugs, anatomic abnormalities, or hypomotility states), the frequency of bacterial overgrowth and infection of the small bowel with enteric pathogens is increased. Some patients whose treatment for Shigella infection consists of diphenoxylate hydrochloride with atropine (Lomotil) experience prolonged fever and shedding of organisms, while patients treated with opiates for mild Salmonella gastroenteritis have a higher frequency of bacteremia than those not treated with opiates.
IMMUNITY
Both cellular immune responses and antibody production play important roles in protection from enteric infections. Humoral immunity to enteric pathogens consists of systemic IgG and IgM as well as secretory IgA. The mucosal immune system may be the first line of defense against many gastrointestinal pathogens. The binding of bacterial antigens to the luminal surface of M cells in the distal small bowel and the subsequent presentation of antigens to subepithelial lymphoid tissue lead to the proliferation of sensitized lymphocytes. These lymphocytes circulate and populate all of the mucosal tissues of the body as IgA-secreting plasma cells.
GENETIC DETERMINANTS
![]() Host genetic variation influences susceptibility to diarrheal diseases. People with blood group O show increased susceptibility to disease due to V. cholerae, Shigella, E. coli O157, and norovirus. Polymorphisms in genes encoding inflammatory mediators have been associated with the outcome of infection with enteroaggregative E. coli, enterotoxin-producing E. coli, Salmonella, C. difficile, and V. cholerae.
Host genetic variation influences susceptibility to diarrheal diseases. People with blood group O show increased susceptibility to disease due to V. cholerae, Shigella, E. coli O157, and norovirus. Polymorphisms in genes encoding inflammatory mediators have been associated with the outcome of infection with enteroaggregative E. coli, enterotoxin-producing E. coli, Salmonella, C. difficile, and V. cholerae.
FIGURE 160-1 Clinical algorithm for the approach to patients with community-acquired infectious diarrhea or bacterial food poisoning. Key to superscripts: 1. Diarrhea lasting >2 weeks is generally defined as chronic; in such cases, many of the causes of acute diarrhea are much less likely, and a new spectrum of causes needs to be considered. 2. Fever often implies invasive disease, although fever and diarrhea may also result from infection outside the gastrointestinal tract, as in malaria. 3. Stools that contain blood or mucus indicate ulceration of the large bowel. Bloody stools without fecal leukocytes should alert the laboratory to the possibility of infection with Shiga toxin–producing enterohemorrhagic Escherichia coli. Bulky white stools suggest a small-intestinal process that is causing malabsorption. Profuse “rice-water” stools suggest cholera or a similar toxigenic process. 4. Frequent stools over a given period can provide the first warning of impending dehydration. 5. Abdominal pain may be most severe in inflammatory processes like those due to Shigella, Campylobacter, and necrotizing toxins. Painful abdominal muscle cramps, caused by electrolyte loss, can develop in severe cases of cholera. Bloating is common in giardiasis. An appendicitis-like syndrome should prompt a culture for Yersinia enterocolitica with cold enrichment. 6. Tenesmus (painful rectal spasms with a strong urge to defecate but little passage of stool) may be a feature of cases with proctitis, as in shigellosis or amebiasis. 7. Vomiting implies an acute infection (e.g., a toxin-mediated illness or food poisoning) but can also be prominent in a variety of systemic illnesses (e.g., malaria) and in intestinal obstruction. 8. Asking patients whether anyone else they know is sick is a more efficient means of identifying a common source than is constructing a list of recently eaten foods. If a common source seems likely, specific foods can be investigated. See text for a discussion of bacterial food poisoning. 9. Current antibiotic therapy or a recent history of treatment suggests Clostridium difficile diarrhea (Chap. 161). Stop antibiotic treatment if possible and consider tests for C. difficile toxins. Antibiotic use may increase the risk of chronic intestinal carriage following salmonellosis. 10. See text (and Chap. 149) for a discussion of traveler’s diarrhea. (After TS Steiner, RL Guerrant: Principles and syndromes of enteric infection, in Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, 7th ed, GL Mandell et al [eds]. Philadelphia, Churchill Livingstone, 2010, pp 1335–1351; RL Guerrant, DA Bobak: N Engl J Med 325:327, 1991; with permission.)
|
POST-DIARRHEA COMPLICATIONS OF ACUTE INFECTIOUS DIARRHEAL ILLNESS |
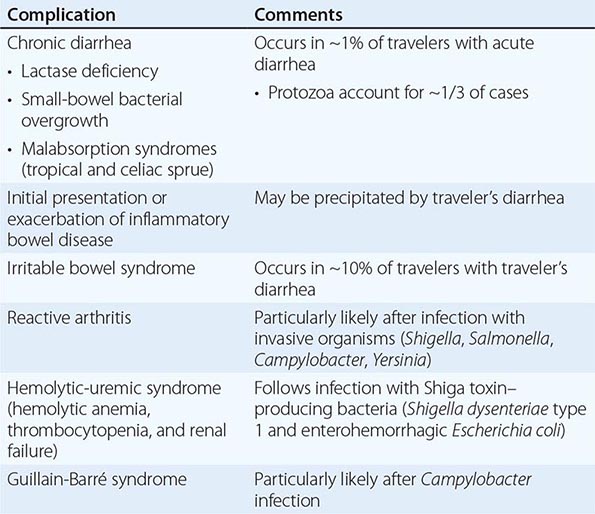
EPIDEMIOLOGY
TRAVEL HISTORY
![]() Of the several million people who travel from temperate industrialized countries to tropical regions of Asia, Africa, and Central and South America each year, 20–50% experience a sudden onset of abdominal cramps, anorexia, and watery diarrhea; thus traveler’s diarrhea is the most common travel-related infectious illness (Chap. 149). The time of onset is usually 3 days to 2 weeks after the traveler’s arrival in a resource-poor area; most cases begin within the first 3–5 days. The illness is generally self-limited, lasting 1–5 days. The high rate of diarrhea among travelers to underdeveloped areas is related to the ingestion of contaminated food or water.
Of the several million people who travel from temperate industrialized countries to tropical regions of Asia, Africa, and Central and South America each year, 20–50% experience a sudden onset of abdominal cramps, anorexia, and watery diarrhea; thus traveler’s diarrhea is the most common travel-related infectious illness (Chap. 149). The time of onset is usually 3 days to 2 weeks after the traveler’s arrival in a resource-poor area; most cases begin within the first 3–5 days. The illness is generally self-limited, lasting 1–5 days. The high rate of diarrhea among travelers to underdeveloped areas is related to the ingestion of contaminated food or water.
The organisms that cause traveler’s diarrhea vary considerably with location (Table 160-3), as does the pattern of antimicrobial resistance. In all areas, enterotoxigenic and enteroaggregative strains of E. coli are the most common isolates from persons with the classic secretory traveler’s diarrhea syndrome. Infection with Campylobacter jejuni is especially common in areas of Asia.
|
CAUSES OF TRAVELER’S DIARRHEA |
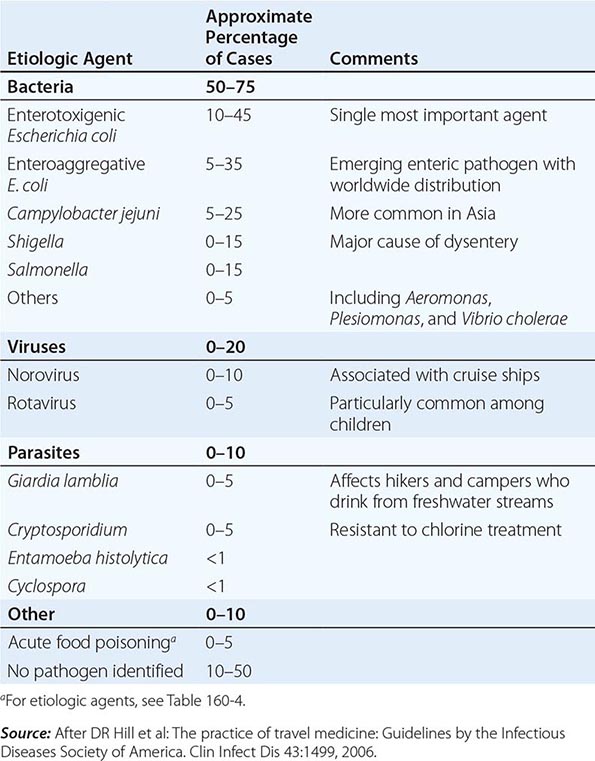
LOCATION
Closed and semi-closed communities, including day-care centers, schools, residential facilities, and cruise ships, are important settings for outbreaks of enteric infections. Norovirus, which is highly contagious and robust in surviving on surfaces, is the most common etiologic agent associated with outbreaks of acute gastroenteritis. Other common organisms, often spread by fecal-oral contact in such communities, are Shigella, C. jejuni, and Cryptosporidium. Rotavirus is rarely a cause of pediatric diarrheal outbreaks in the United States since rotavirus vaccination was broadly recommended in 2006. Similarly, hospitals are sites in which enteric infections are concentrated. Diarrhea is one of the most common manifestations of nosocomial infections. C. difficile is the predominant cause of nosocomial diarrhea among adults in the United States, and outbreaks of norovirus infection are common in health care settings. Klebsiella oxytoca has been identified as a cause of antibiotic-associated hemorrhagic colitis. Enteropathogenic E. coli has been associated with outbreaks of diarrhea in nurseries for newborns. One-third of elderly patients in chronic-care institutions develop a significant diarrheal illness each year; more than one-half of these cases are caused by cytotoxin-producing C. difficile. Antimicrobial therapy can predispose to pseudomembranous colitis by altering the normal colonic flora and allowing the multiplication of C. difficile (Chap. 161).
AGE
Globally, most morbidity and mortality from enteric pathogens involves children <5 years of age. Breast-fed infants are protected from contaminated food and water and derive some protection from maternal antibodies, but their risk of infection rises dramatically when they begin to eat solid foods. Exposure to rotavirus is universal, with most children experiencing their first infection in the first or second year of life if not vaccinated. Older children and adults are more commonly infected with norovirus. Other organisms with higher attack rates among children than among adults include enterotoxigenic, enteropathogenic, and enterohemorrhagic E. coli; Shigella; C. jejuni; and G. lamblia.
HOST IMMUNE STATUS
Immunocompromised hosts are at elevated risk of acute and chronic infectious diarrhea. Individuals with defects in cell-mediated immunity (including those with AIDS) are at particularly high risk of invasive enteropathies, including salmonellosis, listeriosis, and cryptosporidiosis. Individuals with hypogammaglobulinemia are at particular risk of C. difficile colitis and giardiasis. Patients with cancer are more likely to develop C. difficile infection as a result of chemotherapy and frequent hospitalizations. Infectious diarrhea can be life-threatening in immunocompromised hosts, with complications including bacteremia and metastatic seeding of infection. Furthermore, dehydration may compromise renal function and increase the toxicity of immunosuppressive drugs.
BACTERIAL FOOD POISONING
If the history and the stool examination indicate a noninflammatory etiology of diarrhea and there is evidence of a common-source outbreak, questions concerning the ingestion of specific foods and the time of onset of the diarrhea after a meal can provide clues to the bacterial cause of the illness. Potential causes of bacterial food poisoning are shown in Table 160-4.
|
BACTERIAL FOOD POISONING |
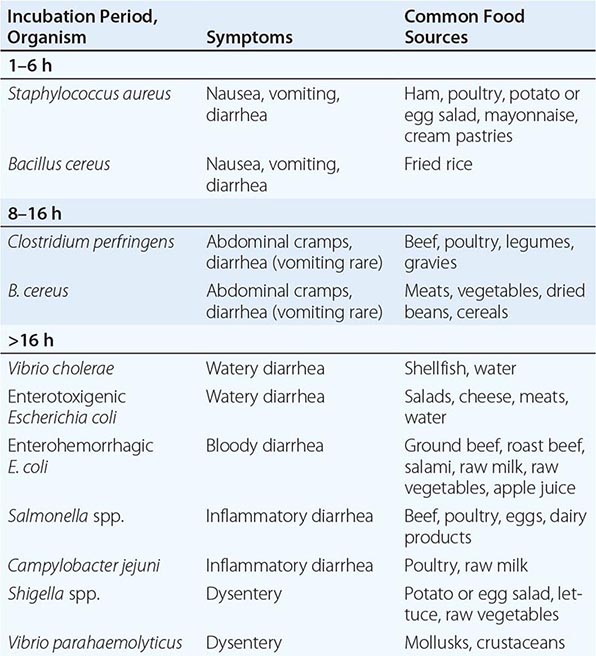
Bacterial disease caused by an enterotoxin elaborated outside the host, such as that due to Staphylococcus aureus or B. cereus, has the shortest incubation period (1–6 h) and generally lasts <12 h. Most cases of staphylococcal food poisoning are caused by contamination from infected human carriers. Staphylococci can multiply at a wide range of temperatures; thus, if food is left to cool slowly and remains at room temperature after cooking, the organisms will have the opportunity to form enterotoxin. Outbreaks following picnics where potato salad, mayonnaise, and cream pastries have been served offer classic examples of staphylococcal food poisoning. Diarrhea, nausea, vomiting, and abdominal cramping are common, while fever is less so.
B. cereus can produce either a syndrome with a short incubation period—the emetic form, mediated by a staphylococcal type of enterotoxin—or one with a longer incubation period (8–16 h)—the diarrheal form, caused by an enterotoxin resembling E. coli LT, in which diarrhea and abdominal cramps are characteristic but vomiting is uncommon. The emetic form of B. cereus food poisoning is associated with contaminated fried rice; the organism is common in uncooked rice, and its heat-resistant spores survive boiling. If cooked rice is not refrigerated, the spores can germinate and produce toxin. Frying before serving may not destroy the preformed, heat-stable toxin.
Food poisoning due to Clostridium perfringens also has a slightly longer incubation period (8–14 h) and results from the survival of heat-resistant spores in inadequately cooked meat, poultry, or legumes. After ingestion, toxin is produced in the intestinal tract, causing moderately severe abdominal cramps and diarrhea; vomiting is rare, as is fever. The illness is self-limited, rarely lasting >24 h.
Not all food poisoning has a bacterial cause. Nonbacterial agents of short-incubation food poisoning include capsaicin, which is found in hot peppers, and a variety of toxins found in fish and shellfish (Chap. 474).
LABORATORY EVALUATION
Many cases of noninflammatory diarrhea are self-limited or can be treated empirically, and in these instances the clinician may not need to determine a specific etiology. Potentially pathogenic E. coli cannot be distinguished from normal fecal flora by routine culture, and tests to detect enterotoxins are not available in most clinical laboratories. In situations in which cholera is a concern, stool should be cultured on selective media such as thiosulfate–citrate–bile salts–sucrose (TCBS) or tellurite-taurocholate-gelatin (TTG) agar. A latex agglutination test has made the rapid detection of rotavirus in stool practical for many laboratories, while reverse-transcriptase polymerase chain reaction (PCR) and specific antigen enzyme immunoassays have been developed for the identification of norovirus. Stool specimens should be examined by immunofluorescence-based rapid assays or (less sensitive) standard microscopy for Giardia cysts or Cryptosporidium if the level of clinical suspicion regarding the involvement of these organisms is high.