Chapter 10 Infection Control
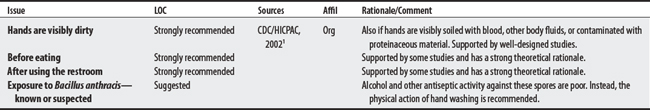
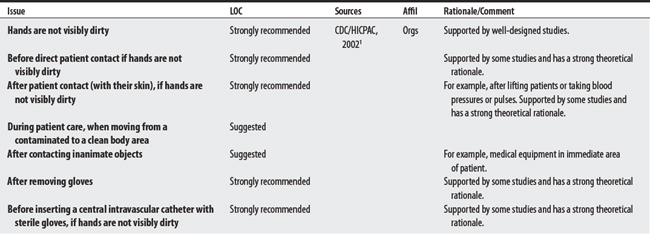
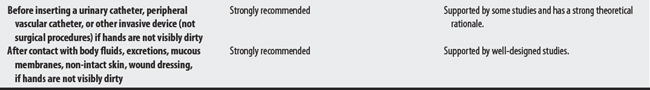
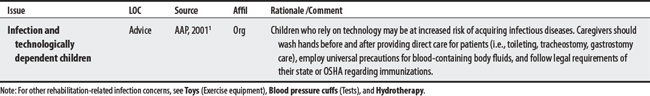
10.1 Guidelines for Hand Hygiene in Health-Care Settings
The Centers for Disease Control (CDC), Health Care Infection Control Practice Advisory Committee (HICPAC), Society for Healthcare Epidemiology of America (SHEA), Infectious Disease Society of America (DSA), and Association for Professionals in Infection Control (APIC) have made 2002 Hand Hygiene recommendations for the use of soap and water and alcohol-based rubs in the health care center.1 Proper hand hygiene can help prevent the spread of antimicrobial-resistant infections, whereas poor hand hygiene may be a contributing factor in patient mortality. Compliance for hand hygiene is noted to be problematic among health care workers.2
10.2 Universal Precautions
The Centers for Disease Control (CDC) made 1987 recommendations for the prevention of HIV, hepatitis B virus, and other pathogens (blood-borne) transmission when providing health care or first aid.1–3 These recommendations, known as Universal Precautions (or Universal Blood and Body Fluid Precautions), are briefly summarized below. For detailed guidelines of these and other precautions involving invasive procedures, dentistry, mortician services, dialysis, laboratories, and environmental considerations for HIV transmission (such as infection, housekeeping, decontamination of spills, and laundry) consult the CDC 19871 (and CDC 1988 supplement & clarification3) publications at www.cdc.gov/mmwr/preview/mmwrhtml/00023587.htm and www.cdc.gov/mmwr/preview/mmwrhtml/00000039.htm.
PROCEDURAL
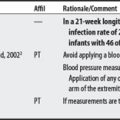
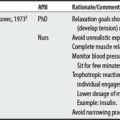
| Universal Precautions: Appropriate barrier precautions should be routinely used by all health care workers to prevent skin and mucous membrane exposure when contact with patient’s blood or other body fluids is anticipated. Blood and body fluid precautions should be consistently used for all patients. | CDC, 19871–3 | Medical history and examination cannot reliably identify all patients infected with blood-borne pathogens or HIV. |
| Use gloves for touching blood, body fluids, mucous membranes, or non-intact skin of all patients, or when performing procedures for vascular access. Change gloves after contact with each patient. | ||
| Use masks and protective eyewear or face shield if the procedure is likely to generate droplets of blood or fluids to prevent exposure of mucous membranes of mouth, nose, and eyes. | ||
| Use gowns or aprons if procedure generates splash of blood or other body fluids. | ||
| Wash skin surfaces (e.g., hands) immediately/thoroughly if contaminated with blood or other body fluids. | ||
| Wash hands immediately after glove removal. | ||
| Prevent injuries with sharp instruments (i.e., needles, scalpels). Do not recap needles or manipulate them with your hand. All sharp instruments and disposable syringes should be disposed of in puncture-resistant containers as close to the use area as practically possible. | ||
| Mouthpieces, resuscitation bags, and other ventilation devices should be available in areas anticipated. Even though saliva is not implicated in HIV transmission, minimize need for emergency mouth-to-mouth resuscitation. | ||
| Health care workers with exudative lesions or weeping dermatitis should refrain from all direct patient contact and equipment until condition is resolved. | ||
| Pregnant health care workers should be familiar with precautions to minimize risk of HIV transmission because of risk to the fetus from perinatal transmission. |
1 Centers for Disease Control and Prevention. CDC MMWR Supplements Recommendations for Prevention of HIV Transmission in Health-Care Settings. Aug 21, 1987/36(SU02). Available at: http://www.cdc.gov/epo/mmwr/preview/mmwrhtml/00023587.htm. Accessed May 17, 2005.
2 Centers for Disease Control and Prevention. Issues in Health Care Settings Universal Precautions for Prevention of Transmission of HIV and Other Bloodborne Infections. Available at: http://www.cdc.gov/ncidod/hip/Blood/universa.htm/. Accessed May 17, 2005.
3 Centers for Disease Control and Prevention. Perspectives in Disease Prevention and Health Promotion Update: Universal Precautions for Prevention of Transmission of Human Immunodeficiency Virus, Hepatitis B Virus, and Other Bloodborne Pathogens in Health-Care Settings. MMWR Weekly. 1988;37(24):1988. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/00000039.htm. Accessed May 17, 2005.