CHAPTER 6 Infection and surgery
Principles of wound management
Factors affecting wound healing
PREVENTION OF SURGICAL SITE INFECTION (Incorporating NICE guidelines 2008)
Antibiotics in surgery
Principles of antibiotic therapy
Selection of antibiotic
2. Based on signs, symptoms and clinical experience, a guess is made at the likely infecting organism.
3. The appropriate specimens are taken for microbiological examination, i.e. culture and sensitivity testing.
4. The most effective drug against the suspected organism is given in line with individual hospital guidelines. If doubt exists this is discussed with a microbiologist.
Prophylactic antibiotics
Indications for prophylactic antibiotics
• Implantation of foreign bodies, e.g. cardiac prosthetic valves, artificial joints, prosthetic vascular grafts
• Patients with pre-existing cardiac disease who are undergoing surgical procedures including dental procedures, e.g. patients with mitral valve disease as prophylaxis against infective endocarditis
• Amputations, especially for ischaemia or crush injuries, where there is dead muscle; risk of gas gangrene is high especially in contaminated wounds; penicillin is the antibiotic of choice
Specific antibiotics (→ Table 6.1)
Surgical infections
Sepsis
• In the region of injury there is local production of inflammatory mediators and cytokines. These lead to vasodilatation, increased vascular permeability and the recruitment of cells that fight infection.
• In more severe injury the cytokine release has a systemic effect; this includes the production of acute phase proteins, pyrexia and an increase in peripheral leukocytes. This response is regulated by a group of counter-regulatory cytokines.
• In patients with SIRS there is an exaggerated response and the production of cytokines exceeds the counter-regulatory mechanisms. Cytokines such as IL-1 and TNF-α produce vasodilatation leading to hypotension, increased vascular permeability leading to oedema and third space fluid loss. There is also widespread activation of leukocytes that can cause damage in organs distant from the site of injury, e.g. lungs.
Management of SIRS
• Identify source of sepsis. Likely possible sources include: the wound; intravascular access (arterial, central venous, cannulas); urinary catheters/urinary tract infection; prosthetic implants; chest infection
Tetanus
Treatment
Prophylactic
• Active immunization with tetanus toxoid. All children should be immunized and this is repeated at 6 weeks and 6 months after the initial dose. Booster doses should be given at 5-yearly intervals. All patients attending an A&E department with new trauma, however mild, should have a booster, unless one has been given within the previous 5 years.
Therapeutic
2. Isolate the patient in a quiet darkened room. Give diazepam or chlorpromazine. In severe cases, the patient will need to be paralysed and ventilated. Feeding should be given via a fine-bore nasogastric tube. Ventilation may need to be continued for up to 4 weeks. A trial period of weaning off relaxants without recurrence of spasm will indicate when ventilation is no longer required. Tracheostomy may be required.
Methicillin-resistant Staphylococcus aureus (MRSA)
Infection and the surgeon
HIV
Precautions for the care of known and suspected hiv, hbv and hcv carriers
Special precautions
• Any patient considered as a risk should be indicated as belonging to a high-risk category on the operating list (under no circumstances should the actual disease causing the risk be placed on the operating list for reasons of patient confidentiality).
• Arrangements should be made for contaminated fluid, dressings, etc. to be handled and disposed of correctly.
Management of sharps injuries
Procedure at Occupational Health or Emergency Department
• Take detailed information – details of injury; how long ago it occurred; was the skin penetrated; did it bleed; was the sharp visibly contaminated with blood; was the source patient known to be infected and with what; any first aid measures used.
Post-exposure prophylaxis
Hepatitis B
• If the source patient tests positive for HBV, the healthcare worker should have been vaccinated and serum antibody positive.
• If antibody levels are low, a dose of hyperimmune anti-hepatitis B IgG plus one dose of vaccine should be given.

 It is best to avoid the intramuscular route if possible as it is uncomfortable for the patient and in shocked patients absorption would be inadequate.
It is best to avoid the intramuscular route if possible as it is uncomfortable for the patient and in shocked patients absorption would be inadequate.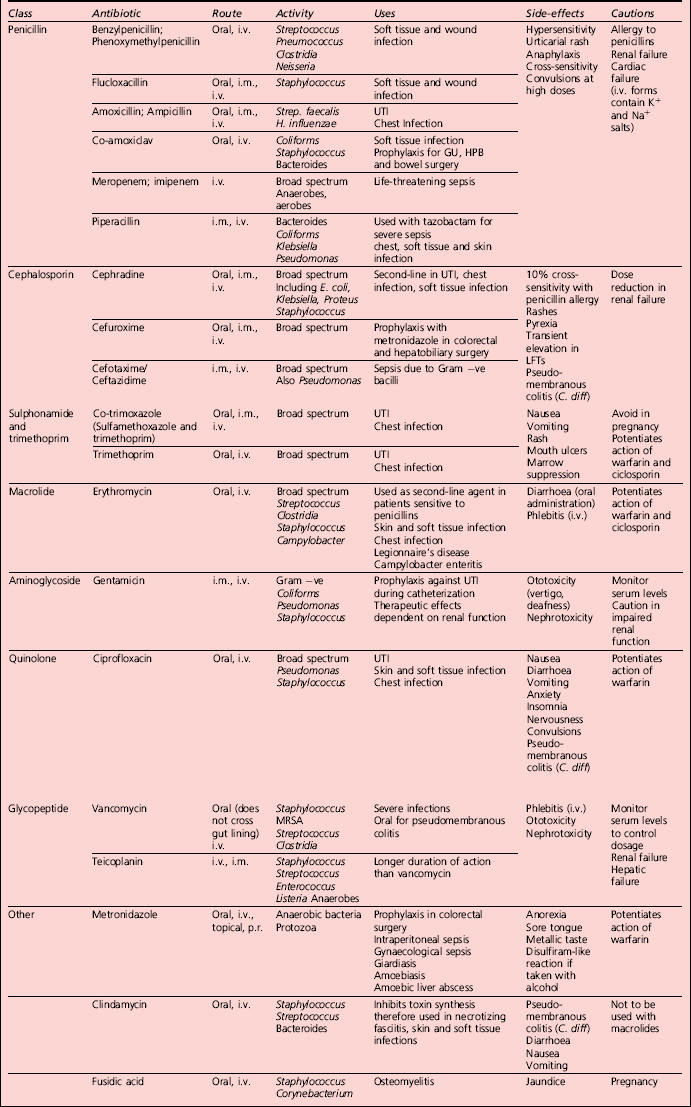
 Erysipelas is an uncommon skin infection caused by a Streptococcus (Group A). The condition is usually encountered on the scalp, face and neck. Pain and redness of the skin are apparent, the margin being well demarcated and raised above the normal skin. Pyrexia and malaise usually accompany the local signs. Treatment is with penicillin.
Erysipelas is an uncommon skin infection caused by a Streptococcus (Group A). The condition is usually encountered on the scalp, face and neck. Pain and redness of the skin are apparent, the margin being well demarcated and raised above the normal skin. Pyrexia and malaise usually accompany the local signs. Treatment is with penicillin.