Individuals with Chronic Primary Cardiovascular and Pulmonary Dysfunction
This chapter reviews the pathophysiology and medical management in relation to the comprehensive physical therapy management of individuals with chronic primary cardiovascular and pulmonary pathology. Exercise testing and training are major components of the comprehensive physical therapy management of individuals with chronic primary cardiovascular and pulmonary conditions, and this topic is presented in detail in Chapter 24.
Because the heart and lungs are interdependent and function as a single unit, primary lung or heart disease must be considered with respect to the other organ and in the context of oxygen transport overall.1,2 Despite a plethora of research and numerous official position statements and clinical practice guidelines, the definition and diagnoses of chronic heart disease and chronic lung disease and their management remain inconsistent in practice.3 Although there is consensus regarding the effectiveness of both cardiac and pulmonary rehabilitation,4 this inconsistent practice is associated with the underuse, overuse, and misuse of therapies regardless of their established effectiveness.
The principles of the physical therapy management of people with various chronic primary cardiovascular and pulmonary conditions are presented rather than treatment prescriptions, which cannot be discussed without consideration of a specific patient (see Case Study Guide to accompany the text on-line). In this context, the general goals of the long-term management of people with each condition are presented, followed by the essential monitoring required and the primary interventions for maximizing cardiovascular and pulmonary function and oxygen transport. The selection of interventions for any given patient is based on the physiological hierarchy. The most physiological interventions are exploited first, followed by less physiological interventions and those whose effectiveness is less well documented (see Chapter 17).
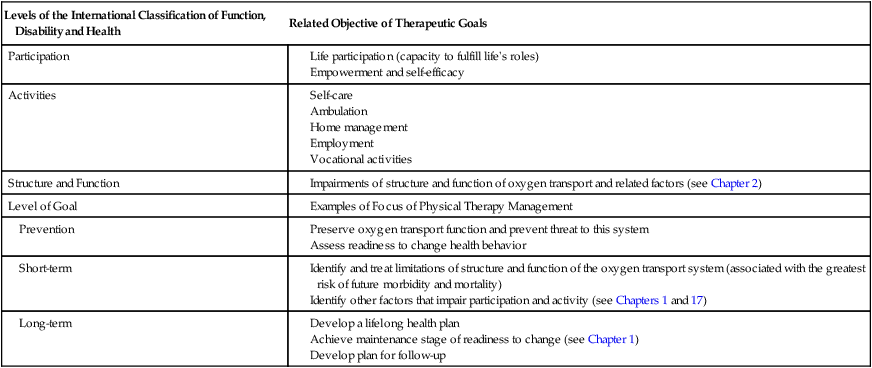
A template of care is shown in Table 31-1. Although there are many commonalities of physical therapy management across patients, only a detailed knowledge of each specific patient, in terms of his or her underlying pathologies and other factors, will lead to the optimal management plan and treatment prescriptions.
Table 31-1
| Levels of the International Classification of Function, Disability and Health | Related Objective of Therapeutic Goals |
| Participation | |
| Activities | |
| Structure and Function | |
| Level of Goal | |
| Prevention | |
| Short-term | |
| Long-term |
Individuals with Primary Cardiovascular Disease
Angina
Pathophysiology and Medical Management
Angina pectoris refers to pain resulting from reduced blood flow to the myocardium. Even though it is usually elicited during exercise, angina may be triggered by stress or in severe cases may occur at rest. Atherosclerosis of one or more of the coronary arteries is the principal cause. Coronary vasospasm is a less common cause of angina. The pathophysiology of angina is described in detail in Chapter 5. A history of angina necessitates further examination to establish the severity of the coronary artery occlusion. Individuals with manifestations of heart disease are categorized according to their limitation during physical activity based on the New York Heart Association (NYHA) Functional Classification (Table 31-2).
Table 31-2
New York Heart Association Functional Classification
| Classification | Characteristics |
| I | No symptoms and no limitation in ordinary physical activity. |
| II | Mild symptoms and slight limitation during ordinary physical activity. |
| III | Marked limitation in activity as a result of symptoms, even during less-than-ordinary activity. Comfortable only at rest. |
| IV | Severe limitations. Experiences symptoms even while at rest. |
If angina is severe and refractory to medical management, the patient is scheduled for coronary bypass surgery (Chapters 29 and 30) to restore normal coronary blood flow. The acute and long-term management of the surgical cardiac patient is presented in Chapter 30. In less severe cases, angina is managed conservatively with medications (e.g., sublingual nitroglycerin, nitroglycerin patch, education, and physical therapy). After the patient’s condition has stabilized, a graded exercise tolerance test may be conducted under supervision in a cardiac stress testing facility where 12-lead electrocardiogram (ECG) monitoring can be performed. The exercise intensity at which the patient exhibits angina (i.e., the anginal threshold) can be quantified and serve as the basis for the prescription of physical activity and exercise.
Principles of Physical Therapy Management
The goals of long-term management of the patient with angina include the following:
 Maximize the patient’s quality of life, general health, and well-being through maximizing physiological reserve capacity
Maximize the patient’s quality of life, general health, and well-being through maximizing physiological reserve capacity
 Educate regarding heart disease, self-management, nutrition, weight control, smoking reduction and cessation, anger and stress management, disease prevention, risk factors, medications and their use, physical activity, and exercise
Educate regarding heart disease, self-management, nutrition, weight control, smoking reduction and cessation, anger and stress management, disease prevention, risk factors, medications and their use, physical activity, and exercise
 Maximize aerobic capacity and efficiency of oxygen transport of all steps in the pathway
Maximize aerobic capacity and efficiency of oxygen transport of all steps in the pathway
 Optimize physical endurance and exercise capacity
Optimize physical endurance and exercise capacity
 Optimize general muscle strength and thereby peripheral oxygen extraction
Optimize general muscle strength and thereby peripheral oxygen extraction
 Design comprehensive lifelong health and rehabilitation programs with the patient
Design comprehensive lifelong health and rehabilitation programs with the patient
Patients with angina are at risk of having an infarction; therefore vigilance and stringent monitoring are necessary to detect angina or frank myocardial infarction. These patients are potentially hemodynamically unstable; thus their hemodynamic responses before, during, and after treatment, particularly aerobic and strengthening exercises, should be monitored and recorded. Minimally, heart rate, blood pressure, and rate-pressure product should be recorded, along with the patient’s subjective responses to treatment. Heavy lifting, static exercise, straining, the Valsalva maneuver, and heavy, repetitive upper-extremity work are avoided during physical activity and exercise. These activities are associated with a disproportionate hemodynamic response. Physical activity and aerobic exercise are prescribed at a target heart rate or perceived exertion ranges that are below the anginal threshold based on a graded exercise tolerance test (see Chapters 19 and 24). Peak exercise tests in patients with cardiac dysfunction that may elicit angina or ST-segment changes are performed in a cardiac stress testing laboratory, usually under the supervision of a cardiologist unless in a specialized facility where physical therapists perform such testing.
The body position in which aerobic exercise is performed is important in patients with heart disease. Positions of recumbency increase the volume of fluid shifted from the periphery to the central circulation. This increases venous return and the work of the heart. Therefore upright body positions have long been known to minimize cardiac work during exercise in these patients and during rest after exercise.5,6
Sexual dysfunction is common in individuals with systemic atherosclerosis owing in part to underlying pathology (dyslipidemia, vascular insufficiency, and diabetes), medication, and the psychological impact of heart disease.7 In terms of energy demands, those of sexual activity are comparable to those of other daily activities (e.g., walking 1 mile on the level). Optimizing health in general with diet and exercise can contribute to regression of atherosclerosis and improved peripheral circulation. Breathing control, body positioning, and energy conservation strategies such as exercising at a high energy time of day may also help minimize symptoms. Also, patients should be advised to avoid sexual activity within an hour of eating, and even then not to consume a heavy meal.
Myocardial Infarction
Pathophysiology and Medical Management
The patient’s ECG will be important for determining the parameters of exercise, the level of monitoring required, and education. Dysrhythmias are described in Chapter 4, and basic ECG reading is presented in Chapter 12. Ventricular dysrhythmias can be lethal. Occasional premature ventricular contractions must be monitored to ensure that their frequency remains low and that coupling does not occur. Atrial fibrillation is considered a relatively serious dysrhythmia. It is associated with a high incidence of coronary disease, stroke, and overall mortality.8 Medication or a pacemaker may be necessary.
Central sleep-disordered breathing is highly prevalent in individuals with left ventricular dysfunction and is associated with abnormal cardiac autonomic control and increased dysrhythmias.9 Although sleep-disordered breathing may not be related to the severity of hemodynamic dysfunction, loss of recuperative sleep will affect functional capacity as well as capacity and motivation to participate in an exercise program and be physically active.
Health-related quality of life reported by individuals with chronic heart failure is associated with function and exercise capacity, not with ejection fraction.10 Health-related quality of life should be an outcome measure for all individuals managed for heart failure because it provides important supplemental information that is independent of physiological indices of cardiac function and the NYHA classification of function (see Table 31-2).
Nonpharmacological approaches to the management of individuals with heart failure are an essential component to the overall management of the condition.11 These measures are incorporated into an individualized program of health behavior change, and include the following:
 Promote adherence to the recommendations
Promote adherence to the recommendations
 Avoid added sodium (salt and preservatives)
Avoid added sodium (salt and preservatives)
 Maintain optimal blood cholesterol and triglyceride levels
Maintain optimal blood cholesterol and triglyceride levels
 Maintain normal blood pressure
Maintain normal blood pressure
 Restrict fluid in the presence of congestive heart failure
Restrict fluid in the presence of congestive heart failure
Risk factor modification is a major goal. A marker of inflammation such as C-reactive protein along with appropriate lipid testing findings may be a more discriminating risk factor than lipid profiling alone.12 Refining the risk factor definition on the basis of C-reactive protein level will help target management (e.g., indicate necessity for intensified exercise programs, weight loss, and smoking cessation).
Principles of Physical Therapy Management
After discharge from the hospital, many patients who have had a myocardial infarction see a physical therapist either privately or through a cardiac rehabilitation program. Patients may remain on a supervised rehabilitation program, including an exercise program, for 6 to 12 months in a specialized center (see Chapter 24).
Depression is a common symptom reported by individuals with coronary artery disease and is associated with increased morbidity and mortality. Individuals with depressive symptoms are more likely to exhibit myocardial ischemia during mental stress testing and during activities of daily living.13 Myocardial ischemia induced by mental stress may be a mechanism by which depression increases the risk of morbidity and mortality in individuals with coronary artery disease. Although aggressive type A individuals are thought to have an increased incidence of heart disease compared with passive type B personalities, anger and hostility have been identified as the toxic negative emotions most implicated in morbidity and mortality related to heart disease.14
A graded exercise tolerance test is conducted before the patient leaves the hospital or when he or she is enrolled in an exercise program. The time between the exercise test and the exercise prescription and implementation of the exercise program should be minimal. Peak (formerly referred to as maximal) exercise tests are conducted in the presence of a cardiologist (unless in a specialized facility where physical therapists may do such testing) and provide the optimal basis for an exercise prescription. Submaximal exercise tests can be conducted by the physical therapist and can provide the basis for an exercise program; however, the prescription should be conservative compared with the prescription based on the peak exercise test. The principles and practice of exercise testing are described in Chapters 19, 24, and 25. Such testing is both an art and an exacting science and should be carried out in a rigidly standardized manner to ensure the test results are maximally valid, reliable, and useful.
The goals of long-term management of the patient with myocardial infarction include the following:
 Maximize the patient’s quality of life, general health, capacity to return to work, and well-being through maximizing physiological reserve capacity
Maximize the patient’s quality of life, general health, capacity to return to work, and well-being through maximizing physiological reserve capacity
 Educate regarding myocardial infarction, self-management, nutrition, weight control, smoking reduction and cessation, relaxation and stress management, risk factors, disease prevention, medications, lifestyle, activities of daily living, and avoidance of static exercise, straining, and the Valsalva maneuver
Educate regarding myocardial infarction, self-management, nutrition, weight control, smoking reduction and cessation, relaxation and stress management, risk factors, disease prevention, medications, lifestyle, activities of daily living, and avoidance of static exercise, straining, and the Valsalva maneuver
 Maximize aerobic capacity and efficiency of oxygen transport
Maximize aerobic capacity and efficiency of oxygen transport
 Optimize physical endurance and exercise capacity
Optimize physical endurance and exercise capacity
 Optimize general muscle strength and thereby peripheral oxygen extraction
Optimize general muscle strength and thereby peripheral oxygen extraction
 Design comprehensive lifelong health and rehabilitation programs with the patient
Design comprehensive lifelong health and rehabilitation programs with the patient
Peak exercise tests in cardiac patients that may elicit angina or ST-segment changes are performed in a cardiac stress testing laboratory under the supervision of a cardiologist. The parameters of the exercise prescription are set based on a peak exercise test. Intensity is set within a heart rate, oxygen consumption, and exertion range (e.g., 70% to 85% of the anginal threshold) (see Chapter 19).
As with patients with angina, the body position in which aerobic exercise is performed by patients with myocardial infarction is important. Positions of recumbency increase the volume of fluid shifted from the periphery to the central circulation. This increases venous return and the work of the heart. Therefore upright body positions are selected for these patients to minimize cardiac work during exercise and during rest after exercise.5,6,15
Valve Disease
Pathophysiology and Medical Management
Clinically, patients with valve disease may demonstrate exertional dyspnea, excessive fatigue, palpitations, fluid retention, and orthopnea. These signs and symptoms are often relieved when exertion is discontinued. Aerobic exercise, however, has been shown to reduce the symptoms of prolapsed valve.16 Anxiety has been reported to decrease general well-being. If effectively managed, however, reduced anxiety can improve or reduce chest pain, fatigue, and dizziness.
Principles of Physical Therapy Management
The goals of long-term management of the patient with valvular heart disease include the following:
 Maximize the patient’s quality of life, general health, and well-being through maximizing physiological reserve capacity
Maximize the patient’s quality of life, general health, and well-being through maximizing physiological reserve capacity
 Educate regarding cardiac valvular disease, self-management, nutrition, weight control, smoking reduction and cessation, relaxation and stress management, cardiac risk factors, disease prevention, medications, lifestyle, activities of daily living, and avoidance of static exercise, straining, and the Valsalva maneuver
Educate regarding cardiac valvular disease, self-management, nutrition, weight control, smoking reduction and cessation, relaxation and stress management, cardiac risk factors, disease prevention, medications, lifestyle, activities of daily living, and avoidance of static exercise, straining, and the Valsalva maneuver
 Maximize aerobic capacity and efficiency of oxygen transport
Maximize aerobic capacity and efficiency of oxygen transport
 Optimize physical endurance and exercise capacity
Optimize physical endurance and exercise capacity
 Optimize general muscle strength and thereby peripheral oxygen extraction
Optimize general muscle strength and thereby peripheral oxygen extraction
 Design comprehensive lifelong health and rehabilitation programs with the patient
Design comprehensive lifelong health and rehabilitation programs with the patient
Physical therapists are involved in the management of patients with valve defects with regard to both the medical aspects, either as a primary or secondary problem, and surgical aspects. After surgery these patients progress well; the principles of their management are presented in Chapter 30. With respect to the medical management of valve defects, the goal is to optimize oxygen transport in the patient for whom surgery is not indicated either because the defect is not sufficiently severe or because the patient cannot or refuses to undergo surgery. Although the mechanical defect cannot be improved, oxygen transport may be improved in some patients with judicious exercise prescription. The parameters of the exercise prescription are usually moderate in that inappropriate exercise doses can further disrupt the inappropriate balance between oxygen demand and supply and thus further exacerbate symptoms. In addition, there is the potential for further valvular dysfunction if the myocardium is mechanically strained.
1. Does the defect preclude treatment?
2. Does the defect require that treatment be modified? If so, how?
3. What special precautions should be taken?
4. What signs and symptoms would indicate the patient is distressed?
5. What parameters should be monitored?
6. Is the patient taking medications as prescribed? How might these medications alter the patient’s response to treatment?
7. Is there any evidence of heart failure? If so, what will the effects of exercise be?
8. If there is no evidence of heart failure at rest, what is the chance that insufficiency will develop with exercise?
The body position in which aerobic exercise is performed is important in patients with heart disease. Positions of recumbency increase the volume of fluid shifted from the periphery to the central circulation. This increases venous return and the work of the heart. Therefore upright body positions are selected for these patients to minimize cardiac work during exercise and during rest after exercise.5,6
Peripheral Vascular Disease
Pathophysiology and Medical Management
Peripheral vascular disease refers to diseases of the arteries and the veins. Peripheral arterial disease results primarily from atherosclerosis and occlusion of the peripheral arteries (e.g., thoracic aorta, femoral artery, and popliteal artery).17 The diagnosis may be overlooked until serious limb ischemia is evident.18 Diabetes mellitus, which can result in microangiopathy and autonomic polyneuropathy, is another important cause of PVD in the lower extremities. Venous disease results in phlebitis, venous stasis, and thromboembolus and leads to valvular incompetence of the veins of the legs.
Individuals with PVD secondary to diabetes mellitus have accelerated atherosclerosis compared with age-matched individuals without diabetes. Diabetes affects the macrocirculation and microcirculation; thus wounds must be prevented, particularly in the lower legs and feet, and managed aggressively should they occur. These individuals may be at risk for lower extremity lesions because of autonomic neuropathy and angiopathy. To restore insulin sensitivity and promote weight loss, activity levels must be significantly increased, and a formal exercise program instituted. Weight-bearing activities are safe for individuals with poor sensation in the feet and do not increase the risk of reulceration.19
Principles of Physical Therapy Management
It should be assumed that individuals with peripheral arterial disease have coronary and cerebral arterial disease necessitating aggressive risk factor management to reduce the risk of myocardial infarction, stroke, and death.20 Primary interventions include smoking cessation; treatment of hypertension, glucose intolerance, and diabetes; and management of low-density lipoprotein cholesterol.
 Maximize the patient’s quality of life, general health, and well-being through maximizing physiological reserve capacity
Maximize the patient’s quality of life, general health, and well-being through maximizing physiological reserve capacity
 Educate regarding atherosclerosis, heart disease, and other sequelae, self-management, nutrition, weight control, smoking reduction and cessation, risk factors, disease prevention, medications, lifestyle, activities of daily living, and avoidance of static exercise, straining, and the Valsalva maneuver
Educate regarding atherosclerosis, heart disease, and other sequelae, self-management, nutrition, weight control, smoking reduction and cessation, risk factors, disease prevention, medications, lifestyle, activities of daily living, and avoidance of static exercise, straining, and the Valsalva maneuver
 If impaired peripheral perfusion of the limbs is present, educate regarding self-assessment of the skin; sock type, care, and cleanliness; shoe fitting; and wound care if indicated
If impaired peripheral perfusion of the limbs is present, educate regarding self-assessment of the skin; sock type, care, and cleanliness; shoe fitting; and wound care if indicated
 Maximize aerobic capacity and efficiency of oxygen transport
Maximize aerobic capacity and efficiency of oxygen transport
 Optimize the work of the heart
Optimize the work of the heart
 Optimize physical endurance and exercise capacity
Optimize physical endurance and exercise capacity
 Optimize general muscle strength and thereby peripheral oxygen extraction
Optimize general muscle strength and thereby peripheral oxygen extraction
 Design comprehensive lifelong health and rehabilitation programs with the patient
Design comprehensive lifelong health and rehabilitation programs with the patient
The primary interventions for maximizing cardiovascular and pulmonary function and oxygen transport in patients with PVD secondary to atherosclerosis include some combination of education, aerobic exercises, strengthening exercises, relaxation, activity pacing, and energy conservation. Exercise, in particular walking, is an important component of management to ameliorate symptoms and improve functional capacity and quality of life.18,21 Pharmacotherapy may help relieve symptoms in the short term, whereas exercise benefits are likely to be long term in terms of addressing systemic atherosclerosis. An ergonomic assessment of both work and home environments may be indicated to minimize myocardial strain.
Individuals with PVD may underestimate their increased risk of cardiovascular disease22; thus education focuses on teaching the basic pathophysiology of atherosclerosis, its risk factors, prevention, and reversal. Health promotion practices are advocated (e.g., smoking reduction and cessation, nutrition, weight control, and regular physical activity and exercise). In addition, types of physical activity that impose undue myocardial strain, increase intrathoracic pressure, and restrict venous return and cardiac output, such as heavy lifting, straining, or the Valsalva maneuver, are avoided. The patient is taught to practice vigilance in monitoring for signs and symptoms of vascular insufficiency in the affected limb and intermittent claudication. Any sign of skin redness in the feet should be monitored closely. In the patient with diabetes, any threat of skin breakdown requires medical attention and discontinuation of exercise until medical clearance has been obtained. Patients with peripheral artery disease are taught to take special care of their feet before and after exercise. The feet and footwear should be kept clean. The inner surfaces of shoes and socks should be smooth.
The body position in which aerobic exercise is performed is important in patients with PVD. Positions of recumbency eliminate the vertical gravitational gradient. This gradient increases blood pressure in the lower extremities. Therefore the claudication threshold is lowered in recumbent positions. Recumbent positions also increase venous return and the work of the heart. Therefore upright body positions are selected for these patients to maximize blood pressure in the lower extremities and to minimize cardiac work during exercise and during rest after exercise.5
Hypertension
Pathophysiology and Medical Management
Systemic hypertension or high blood pressure is a serious condition. Most patients experience no symptoms; thus adherence to medication regimens is often poor. Approximately 90% of hypertension is termed essential hypertension (i.e., no known cause). Hypertension predisposes a patient to stroke, myocardial infarction, renal dysfunction and failure, hemorrhage, and infarction of other vital organs. Blood pressure tends to increase with age. With the aging of the population, the incidence of hypertension is increasing. Increased blood pressure results from increased peripheral vascular resistance; therefore medications are prescribed that reduce myocardial afterload and peripheral vascular resistance. Hypertension and antihypertensive medication are risk factors for type 2 diabetes mellitus.23 Therefore avoiding a patient’s need for medication or at least reducing it is a singularly important physical therapy outcome.
Pulmonary hypertension may occur in the absence of primary cardiac disease. So-called “primary pulmonary hypertension” is often associated with altered resting lung function. Abnormal lung mechanics and diffusing capacity are directly associated with disease severity and may contribute to the dyspnea and fatigue reported by individuals with primary pulmonary hypertension.24
Principles of Physical Therapy Management
Physical therapy contributes to increased metabolic demands and therefore imposes a hemodynamic load resulting in increased heart rate and blood pressure. The assessment should document the history of hypertension, its medical management, and the patient’s response. Regardless of the condition being treated, the hypertensive patient’s blood pressure must be monitored accurately and treatment modified accordingly.25 Blood pressure medications, however, are known to attenuate hemodynamic responses to exercise (Chapter 44); thus blood pressure as an index of hemodynamic status may be limited in some individuals.
Interventions for the physical therapy management of hypertension are cause specific. Lifestyle factors are exploited to help reduce blood pressure and optimize long-term health. A program of aerobic exercise can effectively reduce high blood pressure in some patients. The parameters of the exercise prescription necessary to control hypertension include an aerobic type of exercise that is rhythmic and involves large muscle groups, an intensity of 60% to 75% of the patient’s age-predicted maximal heart rate, 60 to 90 minutes’ duration, and performance of the exercise five to seven times weekly for 3 months to achieve an optimal effect. The exercise intensity should be equivalent to a perceived exertion rating of 3 to 5 on the Borg scale (the patient is able to speak while exercising without gasping), provided that blood pressure does not increase excessively. Only modest exercise intensities are prescribed if the patient has extremely high resting blood pressure to ensure that blood pressure does not rise excessively and is not maintained at a high level for a prolonged period. If the patient’s hypertension responds to the exercise regimen, exercise must be included in the patient’s lifestyle in order for the effects to be maintained. In addition to exercise, many patients lose weight, adopt healthier lifestyle habits, and learn stress management and coping skills concurrently. When exercise is combined with a weight loss program, both resting and stress-induced blood pressures are reduced. The resulting hemodynamic profile resembles that of successful control with pharmacotherapy.26
Elderly individuals with hypertension may exhibit hypotension for almost 24 hours after exercise, along with lower cardiac output, stroke volume, and left ventricular end diastolic volume.27 Thus such individuals should be examined for this effect, and exercise should be modified accordingly.
The goals of long-term management of the patient with hypertension include the following:
 Maximize the patient’s quality of life, general health, and well-being through maximizing physiological reserve capacity
Maximize the patient’s quality of life, general health, and well-being through maximizing physiological reserve capacity
 Educate regarding hypertension, self-management, nutrition, weight control, smoking reduction and cessation, relaxation and stress management, risk factors, lifestyle factors, disease prevention, and medications and their applications and side effects
Educate regarding hypertension, self-management, nutrition, weight control, smoking reduction and cessation, relaxation and stress management, risk factors, lifestyle factors, disease prevention, and medications and their applications and side effects
 Maximize aerobic capacity and efficiency of oxygen transport
Maximize aerobic capacity and efficiency of oxygen transport
 Optimize physical endurance and exercise capacity
Optimize physical endurance and exercise capacity
 Optimize general muscle strength and thereby peripheral oxygen extraction
Optimize general muscle strength and thereby peripheral oxygen extraction
 With the effects of lifestyle changes (physical activity, weight loss, nutrition, smoking cessation, and potentially stress management), medication must be weaned correspondingly
With the effects of lifestyle changes (physical activity, weight loss, nutrition, smoking cessation, and potentially stress management), medication must be weaned correspondingly
 Design comprehensive, lifelong health and rehabilitation programs with the patient
Design comprehensive, lifelong health and rehabilitation programs with the patient
Systemic blood pressure responses to dynamic exercise are greater for upper-extremity than lower-extremity work.28 Thus exercise prescription includes aerobic exercise of the large muscle groups. Avoiding small muscle group work avoids increases in peripheral vascular resistance and hence hemodynamic work, as well as the increased exertion, strain, and work of the heart experienced with upper-extremity work. Exercise is also performed in erect and upright positions rather than recumbent positions to minimize the increased work of the heart secondary to central fluid shifts that occur when the patient is lying in recumbent positions.
Self-monitoring is an important responsibility of the individual with hypertension, given the need to establish valid measures on which interventions are based and modified.25 The most valid blood pressures are recorded by a well-trained individual with a reliable and accurate automatic blood pressure measurement system. The physical therapist can calibrate the home unit against a sphygmomanometer in the clinic or hospital. The individual is advised to measure his or her blood pressure first thing in the morning and record it.
Type 2 Diabetes Mellitus and Metabolic Syndrome
Pathophysiology and Medical Management
Type 2 diabetes mellitus is a condition associated with impaired insulin metabolism that can result in serious long-term multisystem consequences.29 The disease is classified as either insulin-dependent or non–insulin-dependent diabetes mellitus. Insulin is the carrier responsible for transporting glucose into the cells to undergo oxidation. Juvenile-onset diabetes is frequently the insulin-dependent type, whereas adult-onset diabetes often is the non–insulin-dependent type. The underlying pathophysiology of juvenile- and adult-onset diabetes, however, is distinct. Juvenile-onset (type 1) diabetes results from an inadequate number of islets of Langerhans in the pancreas, which are responsible for insulin production. Adult-onset (type 2) diabetes, on the other hand, results from reduced insulin sensitivity. In Western industrialized countries, adult-onset diabetes is associated with obesity, inactivity, poor diet, and stress. In addition, medications can contribute to blood sugar disturbances. The sequelae of type 2 diabetes mellitus that frequently result from poor regulation and management of the disease include angiopathy, peripheral neuropathy, autonomic neuropathy, gastrointestinal paresis, visual disturbance, and renal dysfunction.30
Individuals with type 2 diabetes mellitus have an accelerated rate of atherosclerotic changes in the vasculature compared with age- and sex-matched individuals without diabetes. These individuals are also prone to PVD secondary to microangiopathy, macroangiopathy, and autonomic neuropathy. People with type 2 diabetes mellitus constitute a significant proportion of patients with PVD who require surgical amputation of affected limbs as a consequence of peripheral ischemia. Muscle infarction is a less common but clinically important complication of longstanding diabetes.31 Muscle infarction manifests with pain and swelling over the affected area and at times a palpable mass and elevated creatine kinase levels. The symptoms resolve with conservative management including analgesics and relative immobility of the affected muscle.
Abnormalities of blood sugar metabolism can also be observed in individuals without diabetes. Diabetogenic factors, such as restricted mobility and stress, lead to glucose intolerance and insulin oversecretion.32,33 In the individual without diabetes, these effects can be tolerated over the short term. These factors, however, may result in a critical situation for the individual with diabetes.
Metabolic syndrome is increasingly common and includes central obesity, low high-density-lipoprotein cholesterol, hypertension, and often insulin resistance and hypertriglyceridemia.34
Principles of Physical Therapy Management
Patients with type 2 diabetes mellitus are treated cautiously. Exercise increases metabolic demand commensurate with intensity and hence cellular demand for glucose.35 Usually insulin administration is increased in preparation for exercise. Many active individuals who have type 2 diabetes mellitus are closely attuned to their dietary and insulin needs, which permits them to be as physically active as people without diabetes. Individuals with type 2 diabetes mellitus seen by physical therapists, however, are often labile and less well managed. Thus a readily available sugar source must be nearby for insulin regulation when a person with diabetes exercises or when the physical therapist exercises a patient with type 2 diabetes mellitus on an ergometer after anterior cruciate ligament repair.
In addition, people with type 2 diabetes mellitus may have hemodynamic disturbances because of an autonomic neuropathy and may exhibit impaired fluid-volume regulation during exercise.30 Patients may experience postural hypotension and become dizzy and lightheaded. In addition, diabetic patients may require a longer cool-down period to adjust hemodynamically after exercise.
 Maximize the patient’s quality of life, general health, and well-being through maximizing physiological reserve capacity
Maximize the patient’s quality of life, general health, and well-being through maximizing physiological reserve capacity
 Educate regarding type 2 diabetes mellitus or metabolic syndrome, self-management, nutrition (good nutrition with optimal lipid and triglyceride dietary control), weight control, blood sugar regulation and its management (i.e., the balance among nutrition, diet, exercise, stress, and insulin requirements), medications, smoking reduction or cessation, relaxation, stress management, and foot care, if necessary, in conjunction with hygiene and infection control
Educate regarding type 2 diabetes mellitus or metabolic syndrome, self-management, nutrition (good nutrition with optimal lipid and triglyceride dietary control), weight control, blood sugar regulation and its management (i.e., the balance among nutrition, diet, exercise, stress, and insulin requirements), medications, smoking reduction or cessation, relaxation, stress management, and foot care, if necessary, in conjunction with hygiene and infection control
 Maximize aerobic capacity and efficiency of oxygen transport
Maximize aerobic capacity and efficiency of oxygen transport
 Optimize physical endurance and exercise capacity
Optimize physical endurance and exercise capacity
 Optimize general muscle strength and thus peripheral oxygen extraction
Optimize general muscle strength and thus peripheral oxygen extraction
 With the effects of lifestyle changes (physical activity, weight loss, nutrition, smoking cessation, and, potentially, stress management), medication must be weaned correspondingly
With the effects of lifestyle changes (physical activity, weight loss, nutrition, smoking cessation, and, potentially, stress management), medication must be weaned correspondingly
 Design comprehensive lifelong health and rehabilitation programs with the patient
Design comprehensive lifelong health and rehabilitation programs with the patient
The primary interventions in the long-term management of type 2 diabetes mellitus include education, maintenance of a log of diet and insulin regimens, activity and exercise, aerobic exercise, strengthening exercises, relaxation, stress management, activity pacing, and energy conservation.36 It may be necessary to consult a nutritionist to assist with promoting lifelong change.
Generally there are no contraindications to patients with type 2 diabetes mellitus being physically active and participating in an exercise program. Daily exercise is advocated for insulin-dependent and non–insulin-dependent diabetic patients to optimize glucose control. The exercise prescription parameters are set at 40% to 85% of peak functional work capacity.35 If the patient is exercising daily, the exercise parameters are set at the lower end of this range. If the exercise sessions are less frequent (e.g., in the case of an individual with non–insulin-dependent diabetes whose blood glucose is well maintained and whose weight is acceptable), exercise intensity is set at the higher end of this range.
The risk of hypoglycemia can be reduced by observing the following precautions: frequently monitor blood glucose, decrease the insulin dose (in consultation with the physician) or increase carbohydrate intake before exercise, avoid injecting insulin into areas that are active during exercise, avoid exercise during peak insulin activity, consume carbohydrates before, during, and after prolonged aerobic activity, and be knowledgeable about the signs and symptoms of hypoglycemia.35
Individuals with Primary Pulmonary Disease: Obstructive Patterns
Chronic Airflow Limitation
Chronic airflow limitation is a descriptive term that refers to those disorders that previously were termed chronic obstructive pulmonary disease (COPD) (e.g., chronic bronchitis, emphysema, bronchiectasis, and cystic fibrosis). Although there may be a reversible component, airflow obstruction associated with these disorders is largely irreversible. The pathophysiology of these conditions is reviewed in Chapter 5, and special considerations with respect to exercise testing and training are detailed in Chapter 24.
Bates37 described the syndrome of chronic airflow limitation as being caused by four external factors, mediated by four primary tissue responses, and modified by four physiological responses. The principal external causative factors include inhaled irritants, allergens, infections, and climate. The four principal tissue responses include large and small airway changes, airway hyperreactivity, bronchiolar damage, and alveolar destruction. The principal physiological responses include a reversible increased airway reactivity component, pulmonary vascular response to alveolar hypoventilation, control of breathing response to ventilation-perfusion imbalance and hypoxemia, and tissue defenses against elastase. Decline in pulmonary function and rate of development of the syndrome depend on the combination of causative factors and individual responses.
Management of chronic lung disease should be an integrated and comprehensive program that depends on teamwork, good communication, an approach focused on the individual, and his or her adherence to health recommendations.3 Because of the primary contribution of lifestyle to most cases of heart and lung conditions, there is a long but variable latency before clinical signs and symptoms manifest.38 Therefore advocating healthy lifestyles and working with each individual to embrace such a lifestyle as health insurance will ultimately reduce the burden of the diseases of civilization.
Chronic Bronchitis
Pathophysiology and Medical Management
Chronic bronchitis is usually associated with a history of smoking and is defined as mucous hypersecretion and cough producing sputum for 3 months or more over a 2-year period.39 Over the first few years of smoking, reversible airway changes occur. Over 10 to 15 years of smoking, mucous hypersecretion and chronic bronchitis become apparent. After 25 to 35 years of smoking, irreversible airway damage and chronic disability occur. Smoking is the major cause of emphysema and lung cancer.
The natural history of chronic bronchitis related to smoking includes mucous hypersecretion, reduction in forced expiratory volume in 1 second (FEV1), and increased heterogeneity of the distributions of ventilation, perfusion, ventilation-perfusion matching, and diffusion.40,41 General debility and deconditioning ensue.
Smoking contributes to increased mucus production in the small airways, increased mucus in the large airways, respiratory bronchiolitis, reduced elastic recoil, increased airway reactivity, and vascular changes.37 These changes lead to nonuniformity of time constants in the lung, with consequent inhomogeneous distribution of inspired gas and premature small airway closure, and to nonuniformity of ventilation, perfusion, and diffusion distributions. Although variable among smokers, pulmonary function changes generally correspond to the amount smoked and duration of smoking history. Over time the pulmonary function profile becomes increasingly consistent with chronic airflow limitation (i.e., reduced FEV1 and reduced FEV1/forced vital capacity); however, these are late indicators of pulmonary changes. Signs of uneven distribution of ventilation and increased closing volumes, indicative of small airway involvement, are early pulmonary function changes in smokers. Exercise diffusing capacity is reduced, which explains in part the reduced maximal volume of oxygen use of smokers. Dynamic compliance with breathing frequency is also reduced. Residual volume is increased as a percent of total lung capacity (TLC). Tracheal mucous velocity is reduced, and secretion clearance is impaired. Any patient with a smoking history, regardless of a diagnosis, has some degree of chronic airflow limitation, which must be considered when these patients receive medical or surgical care, as well as physical therapy.
Principles of Physical Therapy Management
 Maximize the patient’s quality of life, general health, and well-being through maximizing his or her physiological reserve capacity
Maximize the patient’s quality of life, general health, and well-being through maximizing his or her physiological reserve capacity
 Assess lifestyle-related health risk factors
Assess lifestyle-related health risk factors
 As indicated, address multisystem conditions that affect presenting signs and symptoms (regarding comorbidity, see Chapters 6, 13, 25, and 32)
As indicated, address multisystem conditions that affect presenting signs and symptoms (regarding comorbidity, see Chapters 6, 13, 25, and 32)
 Educate the patient about chronic bronchitis; self-management; effects of smoking, nutrition, weight control, smoking reduction or cessation, stress management, and other lifestyle factors; medications; infection control, and role of a long-term rehabilitation program
Educate the patient about chronic bronchitis; self-management; effects of smoking, nutrition, weight control, smoking reduction or cessation, stress management, and other lifestyle factors; medications; infection control, and role of a long-term rehabilitation program
 Facilitate mucociliary transport
Facilitate mucociliary transport
 Optimize lung volumes and capacities and flow rates
Optimize lung volumes and capacities and flow rates
 Optimize ventilation and perfusion matching and gas exchange
Optimize ventilation and perfusion matching and gas exchange
 Maximize aerobic capacity and efficiency of oxygen transport
Maximize aerobic capacity and efficiency of oxygen transport
 Optimize physical endurance and exercise capacity
Optimize physical endurance and exercise capacity
 Optimize general muscle strength and thereby peripheral oxygen extraction
Optimize general muscle strength and thereby peripheral oxygen extraction
 Design comprehensive lifelong health and rehabilitation programs with the patient
Design comprehensive lifelong health and rehabilitation programs with the patient
Aerobic exercise is a well-established essential component of the long-term management of the patient with chronic bronchitis to optimize the efficiency of oxygen transport overall including mobilization and removal of secretions.42 The goal is to increase the exercise threshold intensity at which incapacitating dyspnea, perceived exertion, and desaturation occur.
Emphysema
Pathophysiology and Medical Management
Emphysema is associated with a prolonged history of smoking and chronic bronchitis and indicates significant irreversible lung damage. A less common type of emphysema not associated with smoking is alpha1-antitrypsin deficiency. Antitrypsin is essential in balancing elastin production and degradation and in preserving optimal lung compliance. A deficiency of antitrypsin reduces lung elasticity and contributes to the characteristic increase in lung compliance that is the hallmark of emphysema. The pathophysiology of emphysema is detailed in Chapter 5. The principal pathophysiological deficits include irreversible alveolar damage resulting from loss of elastic recoil and the normal tethering of the alveoli, which renders the lung parenchyma excessively compliant and floppy. Excessive distension and dilatation of the terminal bronchioles and destruction of alveoli reduce the surface area for gas exchange. Hence diffusing capacity is correspondingly reduced. The dead space in the lungs and TLC increase significantly. Breathing at normal tidal volume, the patient’s airways close beyond the degree normally occurring with aging, and this contributes to ventilation and perfusion mismatch and hypoxemia. Time constants are altered such that alveolar units are not evenly ventilated. In the nonacute, chronic stages the primary problems include inadequate and inefficient gas exchange resulting from the structural damage to the lungs and altered respiratory mechanics of the lungs and chest wall and their interaction. The lungs are hyperinflated, the chest wall becomes rigidly fixed in a hyperinflated position, the normal bucket handle and pump handle motions of the chest wall are impaired, the hemidiaphragms are flattened, the mediastinal structures are shifted, and the heart is displaced and rotated, making it mechanically inefficient.40 The normal mucociliary transport system is ineffective because years of smoking destroy the cilia, reduce their number, and alter their configuration and orientation; thus their function is correspondingly obliterated or impaired. In addition, these patients are unable to generate high transpulmonary pressures and forced expiratory flow rates because of altered respiratory mechanics. Consequently, coughing is weak and ineffective. The administration of supplemental oxygen is limited because these patients rely on their hypoxic drive to breathe. This life-preserving drive can be attenuated with even moderate levels of oxygen. Thus oxygen administration is limited to low flows. The respiratory muscles are often weak, if not fatigued from being in a flattened position, and hence suboptimal on the length-tension curve.43 The clinical consequences of hyperinflation include abnormal chest wall movement, impaired inspiratory muscle function, increased oxygen cost of breathing, impaired exercise capacity, hypoxemia and hypercapnia, and breathlessness. Overall, patients with emphysema, particularly severe emphysema, tend to be inactive and deconditioned, which further compromises the efficiency of the oxygen transport system and the capacity of other steps in the pathway to compensate.
Noninvasive positive pressure mechanical ventilation (NPPV) has been an important advance in the management of individuals with chronic lung disease.44 Those with daytime hypercapnia with nocturnal hypoventilation may benefit most.45 The efficacy of NPPV, however, is jeopardized by poor adherence to its use. Predictors of successful use include ability to protect the airway, acuteness of illness, and a good initial response within the first couple of hours. Barriers include discomfort of the nose piece or face mask, patient-ventilator asynchrony, excess sternocleidomastoid activity, unstable vital signs, prolonged hours of ventilator use, problems with adaptation, symptoms, and poor gas exchange. In addition to immediate clinical benefits, NPPV may help avoid or postpone respiratory failure and invasive mechanical ventilation and weaning in this population. Other benefits that may be associated with NPPV include improved sleep and quality of life and reduced hospitalization. The physical therapist needs to identify potential barriers and address these to maximize adaptation and adherence to NPPV. Patient subgroups of those who will benefit from NPPV must be identified. Technology research must improve comfort and adherence to NPPV.
Long-term outcome of lung volume reduction surgery for people with severe emphysema has been positive. Six months after surgery, right ventricular performance increases, particularly during exercise.46
Principles of Physical Therapy Management
The goals for long-term management of the patient with emphysema include the following:
 Maximize the patient’s quality of life, general health, and well-being through maximizing his or her physiological reserve capacity
Maximize the patient’s quality of life, general health, and well-being through maximizing his or her physiological reserve capacity
 Educate regarding emphysema, self-management, smoking reduction and cessation, medications, nutrition, weight control, stress management, infection control, and the role of a long-term rehabilitation program
Educate regarding emphysema, self-management, smoking reduction and cessation, medications, nutrition, weight control, stress management, infection control, and the role of a long-term rehabilitation program
 Optimize lung volumes and capacities and flow rates
Optimize lung volumes and capacities and flow rates
 Optimize ventilation and perfusion matching
Optimize ventilation and perfusion matching
 Maximize aerobic capacity and efficiency of oxygen transport
Maximize aerobic capacity and efficiency of oxygen transport
 Optimize physical endurance and exercise capacity
Optimize physical endurance and exercise capacity
 Optimize general muscle strength and thereby peripheral oxygen extraction
Optimize general muscle strength and thereby peripheral oxygen extraction
 Optimize respiratory muscle strength and endurance and overall respiratory muscle efficiency
Optimize respiratory muscle strength and endurance and overall respiratory muscle efficiency
 Ensure that sleep and rest are optimal
Ensure that sleep and rest are optimal
 Design comprehensive lifelong health and rehabilitation programs with the patient
Design comprehensive lifelong health and rehabilitation programs with the patient
Comparable to the patient with chronic bronchitis, sleep disturbances are common in the patient with emphysema. Activity and sleep patterns are assessed to ensure sleep is maximally restorative. If obstructive sleep apnea is disturbing the patient’s sleep, recommendations can be made regarding optimal body positioning during sleep. Back elevation improves airway instability, and in some instances side-lying positions may reduce symptoms.47 If noninvasive mechanical ventilation (e.g., nasal continuous positive airway pressure) is necessary, these body positions may help reduce the amount of ventilatory support required.
The benefits of aerobic and strengthening exercise in the long-term management of airflow limitation to optimize oxygen transport in patients with compromised oxygen delivery are well established.48–50 Patients with severe limitations are often unable to exercise at a sufficient intensity to effect aerobic adaptations to the exercise stimulus. Benefits of exercise in these patients may be explained by desensitization of dyspnea, improved movement efficiency and hence movement economy, improved anaerobic capacity, improved ventilatory muscle strength and endurance, and increased motivation.51,52 Exercise intensity is prescribed based on rating of breathlessness (modified Borg scale) (Chapters 18 and 19), in conjunction with objective and other subjective responses from the exercise test. Objective and subjective responses to exercise in patient populations, however, reflect many factors in addition to pathophysiology (see Chapter 19 for guidelines to maximize test validity).
Patients with chronic airflow limitation alter their breathing patterns so that they breathe on the most metabolically efficient portion of the pressure relaxation curve (see Chapters 5 and 31). These patients tend to breathe with prolonged expiratory phases to maximize gas transfer and mixing in the lungs in order to minimize the effects of altered ventilatory time constants. To facilitate such a breathing pattern, the patient tends to breathe through pursed lips, which may create back pressure to maintain the patency of the airways. The metabolic efficiency of the patient’s breathing pattern may be improved further by altering breathing mechanics rather than imposing a different breathing pattern that may be suboptimal.53 Altering breathing mechanics involves manipulating the patient’s body position to promote alveolar ventilation, perfusion, and ventilation and perfusion matching, thereby reducing the work of the heart.
Breathing control maneuvers (breathing exercises) warrant special mention. Breathing control has been thought to reduce the work of breathing. Inadvertent use of breathing exercises, however, can increase the work of breathing. Diaphragmatic breathing can reduce ventilatory efficiency in people with COPD.54 Furthermore, these exercises are associated with greater oxygen cost than spontaneous breathing in stable patients with COPD.53 The fact that patients do not breathe with the most energetically economic breathing pattern is of considerable clinical interest and suggests that biomechanical efficiency overrides economic efficiency. These findings support that an altered breathing pattern is the consequence of the underlying problem rather than the problem itself. Thus management should be focused on the factors that determine biomechanical efficiency and breathing pattern. Other than pursed-lip breathing, evidence for retraining breathing patterns in people with stable COPD is not well supported.55
Body positioning is a primary determinant of pulmonary function. Thus patients should be encouraged to perform coughing and other forced expiratory maneuvers in upright positions.56 Leaning forward can increase intraabdominal and intrathoracic pressures, elevate the diaphragm, and increase expiratory flow rate.
Obstructive sleep apnea is often associated with COPD. This is complicated further by obesity in some patients. Upright positioning and weight loss can improve respiratory mechanics and oxygenation.57 A more upright sleeping posture could improve nighttime oxygenation in this patient group.
Asthma
Pathophysiology and Medical Management
Asthma is a common respiratory condition that is characterized by hypersensitivity of the airways to various triggers resulting in reversible airway obstruction (i.e., bronchospasm and bronchial edema) (see Chapter 5).39 In mild cases, no treatment other than prophylaxis may be needed. In severe cases, asthma can be life-threatening. Once affected by the trigger, the airways narrow, increasing the resistance to airflow and reducing oxygen delivery. Breathing through narrowed airways contributes to wheezing, reduced alveolar ventilation, rapid shallow breathing, shortness of breath, increased work of breathing, desaturation, and cyanosis. Increased inhomogeneity of the distribution of ventilation is present in some patients with nonacute asthma.58 Expiratory flow-volume loops remain the cornerstone of monitoring asthma.59 Although some triggers may produce mucous hypersecretion, even normal amounts of pulmonary secretions can obstruct narrowed airways and lead to atelectasis. Asthma that has well-defined triggers is easier to manage than cases in which the triggers are less specific.
Principles of Physical Therapy Management
The goals of long-term management of the patient with asthma include the following:
 Maximize the patient’s quality of life, general health, and well-being through maximizing his or her physiological reserve capacity
Maximize the patient’s quality of life, general health, and well-being through maximizing his or her physiological reserve capacity
 Educate regarding asthma, self-management, nutrition, weight control, air quality including smoking reduction and cessation, stress management, medications and their uses, prevention of asthmatic attacks, and infection control
Educate regarding asthma, self-management, nutrition, weight control, air quality including smoking reduction and cessation, stress management, medications and their uses, prevention of asthmatic attacks, and infection control
 Maximize aerobic capacity and efficiency of oxygen transport
Maximize aerobic capacity and efficiency of oxygen transport
 Optimize physical endurance and exercise capacity
Optimize physical endurance and exercise capacity
 Optimize general muscle strength and thereby peripheral oxygen extraction
Optimize general muscle strength and thereby peripheral oxygen extraction
 Design comprehensive lifelong health and rehabilitation programs with the patient
Design comprehensive lifelong health and rehabilitation programs with the patient
The exercise prescription parameters are set below the bronchospasm threshold, which is established based on an exercise test (see Chapters 19 and 24). Specialized challenge tests are performed in a pulmonary function laboratory. Exercise training enables the patient to determine the balance between optimal aerobic capacity and medication and the optimal physical environment for exercise. Temperature and humidity can have significant effects on work output in patients with asthma.
Bronchiectasis
Pathophysiology and Medical Management
Bronchiectasis is characterized by dilatation and anatomical distortion of the airways and obliteration of the peripheral bronchial tree.41 Bronchiectasis is often the sequela of prolonged chronic lung infection. The associated inflammation leads to occlusion of the airways, which results in atelectasis of the parenchyma and consequent dilatation of central airways by increased traction on the peribronchial sheath. In addition, chronic inflammation weakens the walls of the airways, leading to further dilatation. Fibrotic connective tissue changes in the wall contribute further to dilatation and airway distortion. These anatomical changes adversely affect normal respiratory mechanics and hence pressure volume characteristics of the lung. The chest wall becomes hyperinflated and assumes the barrel shape associated with chronic airflow limitation. The overall severity of bronchiectasis depends on the number of lung segments involved. There is often some reversible airflow limitation associated with bronchiectasis.
Principles of Physical Therapy Management
The goals of long-term management of the patient with bronchiectasis include the following:
 Maximize the patient’s quality of life, general health, and well-being through maximizing his or her physiological reserve capacity and function
Maximize the patient’s quality of life, general health, and well-being through maximizing his or her physiological reserve capacity and function
 Educate regarding bronchiectasis, self-management, nutrition, weight control, smoking reduction and cessation, stress management, medications and their use, and infection control
Educate regarding bronchiectasis, self-management, nutrition, weight control, smoking reduction and cessation, stress management, medications and their use, and infection control
 Facilitate mucociliary transport
Facilitate mucociliary transport
 Optimize lung volumes and capacities and flow rates
Optimize lung volumes and capacities and flow rates
 Optimize ventilation and perfusion matching
Optimize ventilation and perfusion matching
 Maximize aerobic capacity and efficiency of oxygen transport
Maximize aerobic capacity and efficiency of oxygen transport
 Optimize physical endurance and exercise capacity
Optimize physical endurance and exercise capacity
 Optimize general muscle strength and thus peripheral oxygen extraction
Optimize general muscle strength and thus peripheral oxygen extraction
 Design comprehensive lifelong health and rehabilitation programs with the patient
Design comprehensive lifelong health and rehabilitation programs with the patient
Cystic Fibrosis
Pathophysiology and Medical Management
Cystic fibrosis is a complex exocrine disease that has significant systemic effects.39 The disease is congenital and is hallmarked by nutritional deficits contributing to impaired growth and development. Pulmonary function shows progressive decline with commensurate reductions in homogeneity of ventilation and inspiratory pressures.58 Cardiovascular and pulmonary involvement can be classified into three groups: no physical signs in the chest; occasional cough and sputum; and constant cough, sputum, and other signs. Patients in each classification can benefit from physical therapy with respect to enhancing oxygen transport. Moderate and severe disease is characterized by significant airflow obstruction secondary to copious, tenacious secretions. In addition, pulmonary hypertension and right heart insufficiency may be manifested and eventual failure may ensue. Left ventricular diastolic failure may also be a feature of advanced disease.60
Principles of Physical Therapy Management
The goals of long-term management of the patient with cystic fibrosis include the following:
 Maximize the patient’s quality of life, general health, well-being, and growth and development through maximizing his or her physiological reserve capacity
Maximize the patient’s quality of life, general health, well-being, and growth and development through maximizing his or her physiological reserve capacity
 Educate the patient and family regarding cystic fibrosis, self-management, nutrition, avoidance of smokers, stress management and relaxation, prevention of acute exacerbations of the disease, infection control, and medication uses, modes of administration, pharmacokinetics, and times to peak efficacies
Educate the patient and family regarding cystic fibrosis, self-management, nutrition, avoidance of smokers, stress management and relaxation, prevention of acute exacerbations of the disease, infection control, and medication uses, modes of administration, pharmacokinetics, and times to peak efficacies
 Facilitate mucociliary transport
Facilitate mucociliary transport
 Optimize lung volumes and capacities and flow rates
Optimize lung volumes and capacities and flow rates
 Optimize ventilation and perfusion matching
Optimize ventilation and perfusion matching
 Reduce the work of and strain on the heart
Reduce the work of and strain on the heart
 Maximize aerobic capacity and efficiency of oxygen transport
Maximize aerobic capacity and efficiency of oxygen transport
 Optimize physical endurance and exercise capacity
Optimize physical endurance and exercise capacity
 Optimize general muscle strength and thereby peripheral oxygen extraction
Optimize general muscle strength and thereby peripheral oxygen extraction
 Design comprehensive lifelong health and rehabilitation programs with the individual (and the family if the patient is a child)
Design comprehensive lifelong health and rehabilitation programs with the individual (and the family if the patient is a child)
Physical activity and aerobic exercise must be integrated early into the lifestyle of the child with cystic fibrosis.61 As much as possible, the child is integrated into activities of his or her peer group. A prescribed aerobic exercise program is designed to optimize the efficiency of oxygen transport at all steps in the pathway and thereby enhance functional capacity overall. Physical activity and aerobic exercise enhance mucociliary transport and mucociliary clearance, maximize alveolar ventilation and ventilation and perfusion matching, increase ventilatory muscle strength and endurance and airway diameter, and stimulate a productive effective cough. Furthermore, physical activity and exercise have been associated with improved immunity and reduced risks of infection.62,63 These are significant outcomes for patients with cystic fibrosis, who have thick, copious secretions.
Ventilatory devices such as the positive expiratory pressure (PEP) mask and the flutter valve have shown benefit in some patients with cystic fibrosis with respect to reducing airway closure, clearing secretions, and enhancing gas exchange.64,65 Such aids may be useful adjuncts in some patients; however, they do not replace the multiple benefits (including mobilizing and removing secretions) of physical activity and exercise on optimizing oxygen transport.
Individuals with Primary Pulmonary Disease: Restrictive Patterns
Interstitial Lung Disease
Pathophysiology and Medical Management
The pathophysiology of restrictive lung disorders and interstitial lung disease (ILD) in particular is described in Chapter 5. This classification of lung disease is associated with various occupations and the inhalation of inorganic and organic dust. As the disease progresses, TLC and vital capacity are reduced. Residual volume often remains the same. Maximal flow rates tend to be increased as compliance is reduced. The drive to breathe, breathing frequency, and the ratio of tidal volume to TLC are increased. Glandular hyperplasia may be present, leading to mucous hypersecretion in some patients. Diffusing capacity may be reduced, but this may be apparent only during exercise (i.e., arterial desaturation and dyspnea). Exercise-induced desaturation and reduction in partial pressure of arterial oxygen may also reflect shunt and ventilation and perfusion mismatch.
Principles of Physical Therapy Management
The goals of long-term management of the patient with ILD include the following:
 Maximize the patient’s quality of life, general health, and well-being through maximizing his or her physiological reserve capacity
Maximize the patient’s quality of life, general health, and well-being through maximizing his or her physiological reserve capacity
 Educate regarding ILD, self-management, nutrition, weight control, smoking reduction and cessation, relaxation and stress management, medications and their uses, prevention, health promotion, and infection control
Educate regarding ILD, self-management, nutrition, weight control, smoking reduction and cessation, relaxation and stress management, medications and their uses, prevention, health promotion, and infection control
 Optimize lung volumes and capacities
Optimize lung volumes and capacities
 Optimize ventilation and perfusion matching
Optimize ventilation and perfusion matching
 Optimize mucociliary transport
Optimize mucociliary transport
 Maximize aerobic capacity and efficiency of oxygen transport
Maximize aerobic capacity and efficiency of oxygen transport
 Optimize physical endurance and exercise capacity
Optimize physical endurance and exercise capacity
 Optimize general muscle strength and thereby peripheral oxygen extraction
Optimize general muscle strength and thereby peripheral oxygen extraction
 Design comprehensive lifelong health and rehabilitation programs with the patient
Design comprehensive lifelong health and rehabilitation programs with the patient
During aerobic exercise, patients with ILD are prone to arterial desaturation.66 Patients who desaturate during sleep require supplemental oxygen during exercise. The intensity of the exercise prescribed is based on arterial saturation, breathlessness, and work of the heart, in conjunction with other objective responses.
Lung Cancer
Pathophysiology and Medical Management
Lung cancer is a leading cause of death for men and the incidence is increasing for women. Once diagnosed, 80% of patients survive 1 year. Lung cancer is highly correlated with a history of smoking and exposure to coal tars, asbestos, and radioactive dusts. The majority of primary malignant tumors are bronchogenic carcinomas. They are centrally located and thus contribute to bronchial obstruction, atelectasis, and pneumonia. Pathophysiologically, lung cancer has features of both obstructive and restrictive lung disease. Presenting signs include airway obstruction, dyspnea, cough, and hemoptysis.39 Treatment is limited to surgery, if metastasis has been ruled out, or conservative management with radiation and chemotherapy.
If detected early, thoracic surgery may be performed to excise the cancerous tumor (see Chapter 29). If inoperable, or in the case of metastases, a patient may be managed at home or in a hospice. Patients are debilitated, often undernourished, fatigued, short of breath, lethargic, depressed, and in pain. Although these patients are often extremely ill, there is a growing trend to manage these patients in the community whenever possible. As the disease progresses, maintaining function and reducing the rate of deterioration become primary goals.
Principles of Physical Therapy Management
The goals of long-term management of the medical patient with lung cancer include the following:
 Maximize the patient’s quality of life, general health, and well-being through maximizing his or her physiological reserve capacity
Maximize the patient’s quality of life, general health, and well-being through maximizing his or her physiological reserve capacity
 Educate the patient and family about the benefits of a palliative program
Educate the patient and family about the benefits of a palliative program
 Promote self-determination and pay particular attention to being an active listener
Promote self-determination and pay particular attention to being an active listener
 Facilitate mucociliary transport
Facilitate mucociliary transport
 Optimize secretion clearance and protect the airways
Optimize secretion clearance and protect the airways
 Optimize lung volumes and capacities and flow rates
Optimize lung volumes and capacities and flow rates
 Optimize ventilation and perfusion matching
Optimize ventilation and perfusion matching
 Maximize aerobic capacity and efficiency of oxygen transport
Maximize aerobic capacity and efficiency of oxygen transport
 Optimize physical endurance and exercise capacity
Optimize physical endurance and exercise capacity
 Optimize general muscle strength and thereby peripheral oxygen extraction
Optimize general muscle strength and thereby peripheral oxygen extraction
 Optimize the benefits of sleep and rest
Optimize the benefits of sleep and rest
 Minimize the effects of restricted mobility and recumbency
Minimize the effects of restricted mobility and recumbency
 Design a rehabilitation program with the patient that is suited to his or her fluctuating needs
Design a rehabilitation program with the patient that is suited to his or her fluctuating needs
Summary
This chapter reviews the pathophysiology, medical management, and comprehensive physical therapy management of individuals with chronic primary cardiovascular and pulmonary pathology. Exercise testing and training are major components of the comprehensive management of these conditions, and this topic is presented separately in Chapter 24. Given that the heart and lungs are interdependent and function as a single unit, primary lung or heart disease is considered with respect to the other organ and in the context of oxygen transport overall.



































