Individuals with Acute Surgical Conditions
 The patient’s complete return to full participation in life and the capacity to perform its requisite activities
The patient’s complete return to full participation in life and the capacity to perform its requisite activities
 Avoidance of recurrence of the problem for which the individual’s surgery was indicated
Avoidance of recurrence of the problem for which the individual’s surgery was indicated
 Reduced subsequent doctor- and hospital-based care and need for medication
Reduced subsequent doctor- and hospital-based care and need for medication
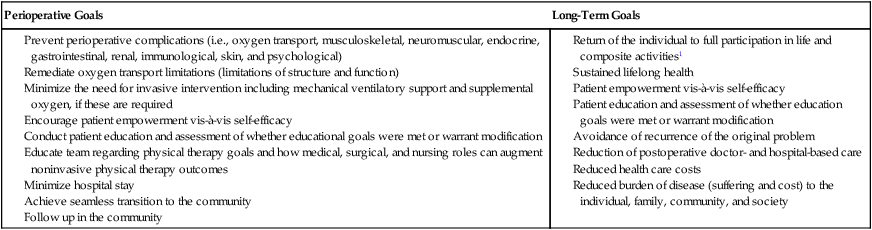
The decision as to whether and to what extent physical therapy is indicated is based on the individual’s need rather than strictly on his or her condition. The patient’s condition is one factor that can determine perioperative risk, operative course, and long-term outcomes. Factors other than the primary indication for surgery, however, can have a more important effect on perioperative course and outcomes. Because of this, the preoperative assessment determines who requires physical therapy management and who does not. Physical therapy prevents complications and addresses oxygen transport threats and deficits. In the long term, physical therapy helps ensure that the individual returns to the highest level of living and regains or surpasses premorbid presurgical functional status. In cases in which the underlying condition can recur, a prime physical therapy objective is to minimize this possibility. Surgical outcomes, based on the physical therapy perspective within the International Classification of Functioning, Disability and Health,1 are shown in Box 30-1.
The purpose of this chapter is to review the identification of surgical risk in a given individual and the management of patients with cardiovascular and pulmonary risk factors and dysfunction secondary to acute surgical conditions. Surgery today has become more extreme in two ways. First, minimally invasive surgery has shortened the operative period, hastened discharge, and reduced risk.2 Second, with advances in instrumentation, monitoring, and anesthesia, more invasive, prolonged, and risky surgery is being performed with improved chances of survival.
The cardiovascular and pulmonary effects of anesthesia and surgery are described. The two types of surgery that have the greatest impact on cardiovascular and pulmonary function, namely thoracic and cardiovascular surgery, are highlighted. These surgeries are particularly invasive and lengthy, often require heavy and prolonged anesthesia and sedation, are typically performed on older people whose health status may be poor, and are generally associated with increased risk. Thus they warrant intensive perioperative physical therapy. Patients are assessed with respect to their presurgical and surgical hemodynamic and oxygen transport status to establish oxygen transport capacity and the degree to which increased metabolic demands associated with the perisurgical conditions as well as interventions can be met. In particular, cardiac output and oxygen delivery (DO2) will increase to compensate for these increased metabolic demands. Increased metabolic demands, however, are dependent on age, severity of illness, type of surgery, comorbidity, and complications.3 Furthermore, people who are overweight or obese, a common lifestyle-related condition, are more likely to require surgery. Obesity can reduce arterial oxygen tensions and the compliance of the respiratory system irrespective of the tidal volume or respiratory rate.4 A detailed analysis of these factors can identify risks, expedite early intervention such as mobilization, and increase survival.
The four categories of factors that threaten or impair oxygen transport are described in Chapter 17. These factors include the underlying pathology, restricted mobility and recumbency, extrinsic factors related to the patient’s care, and intrinsic factors related to the patient. This chapter examines in detail the effects of surgery, including the effects of anesthesia and other medications on oxygen transport as well as the impact of the underlying condition, restricted mobility and recumbency, and factors associated with the patient on an individual’s status postoperatively. These are described in a format to facilitate assessment and ongoing evaluation.
Treatment principles are presented. These are not intended, however, to be a treatment prescription for a particular patient. The effects of anesthesia and surgery must be considered in addition to the underlying pathology and the effects of restricted mobility, body position, and intrinsic and extrinsic factors (see Chapter 17). All these factors must be considered and integrated in prescribing treatment and defining the specific parameters of the prescription. Such integration is essential for treatment to be targeted to the underlying problems and to be maximally effective.
Perioperative Course
Surgery and Its Cardiovascular and Pulmonary Consequences
Factors that place a patient at risk can contribute to perioperative cardiovascular and pulmonary dysfunction if preventive strategies fail (Box 30-2). Cardiovascular and pulmonary complications are the major cause of perioperative morbidity and mortality, particularly in patients undergoing thoracic or cardiovascular surgery.5 The physical therapist must establish the risk factors based on premorbid health assessment including age, smoking habits, nutrition, weight, regular physical activity and fitness, sleep, and stress, as well as cardiac dysfunction, lung dysfunction, musculoskeletal dysfunction, neuromuscular dysfunction, and endocrine dysfunction—in particular, type 2 diabetes mellitus.6
Physical therapy has a role in preparing patients for surgery some weeks in advance—a service that is not being fully exploited in health care. Maximizing a patient’s health will lead to fewer complications, will shorten hospital stay, and will hasten recovery and return to full participation in daily life. Interventions can include health education, including initiating or supporting smoking cessation. Smoking cessation or smoking reduction by at least 50% has been shown to improve the outcomes after hip and knee replacements.7 Comparable benefits could be expected for other types of surgery, particularly cardiovascular and thoracic procedures. Optimizing nutrition and prescribing an exercise program, even if modified because of the patient’s underlying condition, can augment oxygen transport. Thus, when oxygen transport is unavoidably compromised by anesthesia and surgery, the patient has greater reserve capacity.
People who are overweight and obese have direct, serious weight-related morbidity including hypertension, type 2 diabetes mellitus, lipid-related heart conditions, and sleep apnea. In addition, people who require joint replacement surgery because of arthropathy secondary to irreversible joint damage are more likely to be overweight.8 Thus, overweight and obesity constitute major complications during surgery and recovery. Given their prevalence, overweight and obesity warrant being addressed by physical therapists in every patient, whether surgical or medical (see Chapters 1 and 6). Furthermore, body mass index as well as weight-to-hip ratio and age have been reported to be significant predictors for type 2 diabetes mellitus and hypertension, which further complicates the clinical presentation and management of surgical patients who are overweight or obese.9
Early surgery for hip fracture in older adults has not been shown unequivocally to result in improved outcomes—that is, reduced complications (pneumonia and bed sores), earlier recovery, and reduced mortality.10 It is likely that clinically some patients may benefit whereas others may benefit from some delay. Irrespective, the outcomes of physical therapy will be enhanced in either situation if instituted in a timely manner. Studies are needed to establish the degree to which physical therapy including lifestyle behavior change (weight loss in particular) may avert surgery all together, or appropriately delay it. In some patients, early surgery may be preferable. In this case, some finite period of time in which a course of physical therapy could be instituted prior to surgery, could augment surgical outcomes.
Anesthesia and Supplemental Oxygen
Anesthesia results in depression of breathing. Thoracic respiratory excursion is reduced. The tone and pattern of contraction of the respiratory muscles, particularly the diaphragm and the intercostal muscles, change, which contributes to many secondary cardiovascular and pulmonary effects observed after surgery. The loss of end-expiratory diaphragmatic tone causes the diaphragm to ascend into the chest by 2 cm during anesthesia with or without paralysis.11 Reductions in functional residual capacity (FRC) are correlated with this change and with altered chest wall configuration and increased thoracic blood volume.12,13 One of the most pervasive and predictable clinical effects observed in the postoperative period is alveolar collapse. Total lung capacity, FRC, and residual volume are decreased. The FRC is reduced in the supine position compared with the erect sitting position14,15 and is further reduced with the induction of anesthesia. Anesthesia, however, fails to reduce FRC in the sitting position.
The consequences of reduced FRC with anesthesia and surgery have major implications for postoperative complications and the course of recovery. Airway closure occurs with anesthesia, and this likely contributes to intrapulmonary shunting. Compression atelectasis of the dependent (lowermost) lung fields occurs during surgery.16 In addition, compression atelectasis occurs when lung tissue and surrounding structures are being physically manipulated by the surgeon. Although reduced airway caliber in areas of low lung volume can be offset by the airway-dilating effect of many inhaled anesthetics, airway resistance is increased by obstruction of the breathing circuits, valves, and tracheal tubes. The airways may also be obstructed with foreign matter such as blood and secretions, or from bronchospasm caused by irritation. Because of the decrease in FRC, lung compliance is decreased and the work of breathing is increased. Hypoxemia secondary to transpulmonary shunting is usually maximal within 72 hours after surgery and may not be completely resolved for several days. Persistent reduction in FRC after surgery delays the restoration of the normal alveolar-arterial oxygen gradient.
Anesthesia and tissue dissection contribute to major changes in lung volume, mechanics, and gas exchange. The extent and duration of these changes increase with the magnitude of the operative procedure and degree of anesthesia required. Tissue oxygenation can be threatened during the intraoperative period, and the relationship between oxygen consumption (VO2) and delivery (DO2) compromised.17 Mismatch between VO2 and DO2 is associated with a complicated clinical course and prolonged intensive care unit stay in the absence of conventional indicators such as low ejection fraction and longer cardiovascular and pulmonary bypass time.18 Oxygen extraction increases to compensate for reduced DO2. Early optimization of the ratio of VO2 and DO2 is indicated to reduce perioperative morbidity and mortality.
After surgery the normal pattern of breathing is disrupted. Shallow, monotonous tidal ventilation without normal occasional, spontaneous deep breaths causes alveolar collapse within an hour.15 Unless resolved within a few hours, atelectasis becomes increasingly resistant to reinflation. This complication is exacerbated in patients receiving narcotics.
Immediate Postoperative Period
After surgery the patient is detained in the recovery room until vital signs have stabilized, there is no apparent internal or external bleeding, and the patient is responding to his or her name. Patients recovering from minor surgery are usually transferred to a ward once discharged from the recovery room. A patient is transferred to the intensive care unit after surgery if complications arose during surgery, if the patient cannot be readily stabilized and requires close monitoring, or if the patient had more serious surgery such as cranial, cardiovascular thoracic, or emergency surgery such as that resulting from multiple trauma (see Chapter 35).
Pharmacological Considerations
Common pharmacological agents prescribed for patients perioperatively are described in Chapter 45. Physical therapists need a thorough knowledge of these when managing the surgical patient so management can be optimized.
Several factors are particularly important in managing surgical patients because these factors can affect the patients’ sensitivity to narcotic analgesics such as morphine.19,20 There is considerable intersubject response variability to these agents. Older patients, for example, can be expected to be more sensitive to narcotics. Diverse multisystem pathology has a marked effect on the degradation, absorption, biotransformation, and excretion of morphine. Exaggerated effects of morphine have been reported when administered in conjunction with other agents such as other narcotic analgesics, phenothiazines, tranquilizers, or sedative-hypnotics; in addition, such exaggerated effects have been reported in patients with respiratory depression, hypotension, and sedation and in patients who are unconscious. Situations in which exaggerated drug effects have been reported are commonly encountered in the intensive care setting and can result in unpredictable responses. Finally, the physical dependence and abuse potential of these agents cannot be ignored.
 Have nonpharmacological means of analgesia been exploited?
Have nonpharmacological means of analgesia been exploited?
 If pharmacological analgesia is indicated, could analgesics other than narcotics be used?
If pharmacological analgesia is indicated, could analgesics other than narcotics be used?
 Can the dose of narcotic be reduced so that satisfactory pain control can be achieved in combination with nonpharmacological interventions?
Can the dose of narcotic be reduced so that satisfactory pain control can be achieved in combination with nonpharmacological interventions?
The administration of narcotics has important implications for physical therapy. These powerful analgesics are often the medications of choice for major pain relief and comfort. Their secondary effects, however, which include reduced arousal and monotonous tidal ventilation, are primary physical therapy concerns. Narcotics interfere with a patient’s ability to cooperate with treatment. If narcotics impair the patient’s ability to participate in treatment, analgesia with a less systemic effect is indicated. Patient-controlled analgesia (PCA) is an effective means of having the patient regulate the amount of analgesia he or she is receiving.21 Patients have been reported to administer less medication to themselves than nurses assessing their analgesia needs. Intravenous administration prolongs the peak-effect time of analgesics and therefore helps the patient tolerate longer, more intense treatments. Oversedation must be avoided if the patient is to derive maximal benefit from cardiovascular and pulmonary physical therapy treatments.
Factors Determining Surgical Response and Outcomes
A patient’s response to and outcome after surgery as well as potential complications depend on multiple factors (see Box 30-2). The type of surgery determines the degree of invasiveness, type or types of anesthetics and sedatives, type and level of respiratory support, static body position assumed during surgery, approximate duration of the surgery and period of anesthesia, incisions, dressings, lines, leads, catheters, monitoring devices, chest tubes, type and degree of pain that can be expected, and necessity for and type of pain control after surgery.
Preoperative Assessment And Preparation For Surgery
Preoperative physical therapy management includes the preoperative assessment and education; the primary components are shown in Box 30-3. During this time the physical therapist has an opportunity to develop rapport with the patient. The assessment establishes the risk of complications and prolonged hospital stay and the type and extent of perioperative physical therapy required. Postoperative neurological syndromes are common. Ongoing assessment helps ensure that these are identified and addressed early.22 The assessment establishes what the postoperative priorities will be; however, these are modified based on the postoperative assessment. The surgical procedures are described and the effects of surgery and anesthesia and sedation on gas exchange are reviewed so that the patient understands the importance of being actively involved in physical therapy, both during and between treatments after surgery.
The importance of a thorough preoperative assessment and teaching by the physical therapist cannot be overstated. The components of preoperative assessment and teaching are summarized in Box 30-3. In cases of elective surgery, preoperative teaching includes a general description of the surgery to be performed, the effect of anesthesia and surgery on cardiovascular and pulmonary function, and the systemic effects of restricted mobility and recumbency. The lines, leads, and catheters usually associated with the surgery are explained. The patient is instructed in breathing control maneuvers, supported coughing, chest wall mobility exercises, mobility exercises for the limbs (e.g., hip and knee and foot and ankle exercises), turning in bed, sitting up, transferring, chair sitting, and walking erect postoperatively. In addition, the patient is taught methods of maximizing comfort with body positioning and supporting the surgical incision. If the bed has controls the patient can manipulate, he or she is taught how to make bed adjustments as required. The postoperative course is explained in general terms so the patient can anticipate this period. If the patient is well informed preoperatively, he or she will be better oriented and capable of cooperating when he or she wakes from the anesthesia.
The physical therapist may be consulted by the surgeon to help make a poor-risk patient into a better-risk patient. Patients with upper–respiratory tract infections before surgery may have their surgeries postponed, depending on the type and extent of surgery to be performed, level of anesthesia indicated, and other medical conditions including cardiovascular and pulmonary disease, age, and smoking history. Patients with preoperative lower–respiratory tract infections constitute a greater operative risk; hence these patients often have their surgeries postponed until the infection has resolved. Patients with chronic cardiovascular and pulmonary diseases require a prolonged period of preoperative physical therapy in preparation for surgery. Elective surgery is not usually considered during an exacerbation of chronic lung disease. Even minor surgery may be potentially hazardous for the patient with previous lung disease. The adverse effects of total anesthesia on these patients are magnified because of their reduced pulmonary reserve capacity. Smoking should be discontinued for as long as possible before surgery. The patient is placed on an exercise conditioning program, a regimen of bronchial hygiene, oxygen if necessary, and prophylactic antibiotics. Even patients with extremely low functional work capacity can enhance the efficiency of the steps in the oxygen transport pathway (see Chapters 18 and 19) with a modified aerobic exercise conditioning program. This preoperative preparation may take one to several weeks, depending on the patient and the indications for surgery. Patients who are overweight can reduce their risk of perioperative complications by losing weight. Body mass is a major determinant of lung function, respiratory mechanics, and oxygenation during anesthesia,23 and adverse effects on these can lead to major surgical complications and problems during recovery.
Preoperative inspiratory muscle training has gained renewed interest as a means of preserving respiratory muscle function postoperatively and reducing postoperative pulmonary complications. Although maximal inspiratory pressure can be preserved,24,25 studies are needed to show that this intervention augments outcomes over and above the benefits of an exercise program before surgery. Furthermore, a narrowly focused intervention such as inspiratory muscle training may overlook the benefits of a more holistic preoperative preparation program. Such training needs to be prescribed judiciously.
Postoperative Management
Goals
The goals of postoperative physical therapy management related to oxygen transport appear in Box 30-4. The patient is mobilized in a systematic sequence that progresses from supine to turning in bed to sitting over the bed to standing to sitting in a chair to walking (Table 30-1). Some patients progress through these steps quickly, whereas others take longer. The rate at which patients are progressed depends on their responses. Pain medications are coordinated as needed with treatments to maximize treatment effectiveness. This progressive sequence is comparable to that of phase I of cardiac rehabilitation, the inpatient phase for surgical as well as medical patients, and includes education, counseling, and treatment as indicated. These goals are addressed between as well as during treatments. The patient is instructed in mobilization and body positioning coordinated with deep breathing and supported coughing maneuvers between treatment sessions, and these interventions should be performed hourly during waking hours.26,27 Such a regimen has been reported to result in favorable outcomes for invasive abdominal surgery.28
Table 30-1
Template for Progressing Mobilization in Surgical Patients
| Level | Date | Activity | Bathroom | Bathing |
| 1 | Confined to bed Assessment Body positioning |
Portable toilet when possible | Personal care by nurse May wash hands and feet |
|
| 2 | Sit up in chair for 20 minutes, three times per day | Use portable toilet | May wash in bed (not legs, back, or feet) | |
| 3 | Sit up in chair as much as possible | Bathe at bedside | ||
| 4 | Walk to bathroom | Bathe at sink (sitting) | ||
| 5 | Walk around room as able | Bathe at sink | ||
| 6 | Short walks in hall two or three times per day | |||
| 7 | Walk in halls as able | Take shower (sitting) or tub bath | ||
| 8 | Walk one flight of stairs with assistance | |||
| 9 | Discharge |
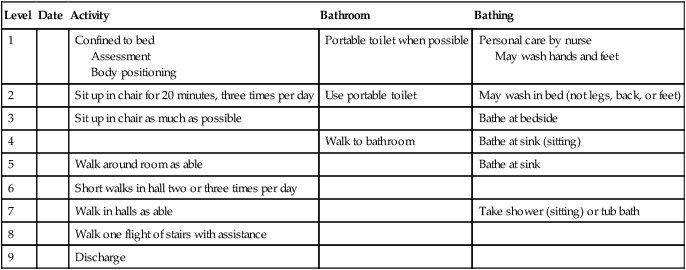
Adapted from Makrides L: Cardiac rehabilitation manual, Halifax, Nova Scotia, Canada, 1997, Cardiac Prevention Research Centre, Dalhousie University.
1. Maximize the patient’s ability to perform activities of daily living.
2. Maintain or increase general muscle strength and endurance.
3. Maximize muscle and soft tissue length and ligament integrity.
4. Maintain normal arousal and neurological function.
7. Maintain normal cognitive function to avoid disorientation and hospital-related psychoses.
Finally, there are important preventive goals (e.g., minimizing the effects of restricted mobility and recumbency on all organ systems) (see Chapters 19 and 20). Of particular concern in the surgical patient is the risk of thromboemboli and pulmonary emboli and the risk of pressure points and skin breakdown. Thus mobilization and regular activation of the muscle pumps to minimize circulatory stasis and frequent body-position changes are essential to reduce risks, which can have serious consequences for the patient’s recovery. Compression stockings are often put on the patient after surgery. These are not removed, except for cleaning and redistributing pressure, until the patient is consistently up and about. These stockings facilitate venous return and increase blood flow and velocity, thereby minimizing the risk of thrombus formation. Should thrombus formation be suspected, it may be necessary to attach an intermittent compression device to the legs to simulate muscle pump action.
Alternatively, some patients are restless and agitated after the effects of anesthesia have worn off. Hypoxemia can lead to restlessness and agitation. Thus it is important that these patients not be inappropriately sedated. This compounds their need for treatment while making them less able to cooperate with treatment simultaneously.29,30
Early Postoperative Physical Therapy
Rationale
To sustain alveolar inflation and normal FRC postoperatively, mobilization and body positioning coordinated with breathing control and supported coughing must be carried out frequently (i.e., every 1 to 2 hours) to maintain optimal alveolar volume and distribution of ventilation. Maximal inspiratory maneuvers are coordinated with mobilization and body positioning at least every hour as tolerated. Maximal inspiratory maneuvers alone, however, are unlikely to be effective because the inspiratory pressure may be insufficient to inflate atelectatic alveoli. Rather, patent alveoli will tend to be overexpanded. Mobilization and body positioning will directly alter the intrapleural pressure gradient and thereby optimize alveolar expansion. In patients who are obese and anesthetized and paralyzed, the prone position increases FRC, lung compliance, and oxygenation.23,31 Being prone may have some postoperative role in some patients who are obese, but the hazards of recumbent positions must be weighed against the benefits of being upright.
Normal passive expiratory efforts to end tidal volume are encouraged, and maximal or forced expiratory efforts are usually avoided to prevent airway closure and potential increase of atelectasis. Huffing (glottis open) rather than coughing (glottis closed) also minimizes airway closure. With huffing there is less risk of bronchospasm than with coughing, in which the glottis is closed, transpulmonary pressure is increased, and a compressive phase is involved. If indicated, coughing maneuvers are most effective in the sitting or slightly leaned-forward position, in which lung volumes and forced expiratory flow are maximized and the respiratory muscles are at a mechanical advantage with respect to the length-tension characteristics of the muscle fibers. Airway closure is position-dependent (see Chapter 20); therefore the degree of expiration encouraged by the physical therapist should be based on the patient’s body position. Airway closure is potentiated in patients who are older, smoke, or are obese and in patients who are in horizontal as opposed to upright body positions.
Mobilization and body positioning coordinated with breathing control and supported coughing maneuvers offer the greatest benefit to oxygen transport in the postoperative patient. Specific benefits are described in Chapters 18, 19 and 20. They include maximizing FRC, reducing closing volume, maximizing expiratory flow rates, promoting mucociliary transport, promoting airway clearance, optimizing lymphatic drainage, minimizing the effects of increased thoracic blood volume, maintaining fluid-volume regulating mechanisms, and minimizing the work of breathing and of the heart. Sustained maximal inspiration is one intervention that promotes alveolar expansion. Each deep breath is performed to maximal inspiration (i.e., to total lung capacity) with a 3- to 5-second breath hold. This maneuver may reduce pulmonary complications by promoting alveolar inflation and gas exchange. The patient is encouraged to repeat this maneuver several times hourly; frequently during mobilization; and before, during, and after body-position changes.
Although the benefits of incentive spirometry (Figure 30-1) postoperatively are equivocal at least after thoracic surgery,32 it may be useful in patients who are resistant or unable to cooperate fully with maximal inspiratory efforts or be adequately mobilized. Postoperative hypoxemia may be reduced with this technique, which uses the principle of sustained inspiration using a feedback device (either flow or volume feedback) to achieve maximal inflating pressure in the alveoli and maximal inhaled volume. Spirometers with a volume-controlled device, however, may improve diaphragmatic excursion more than flow-dependent devices.33 With proper instruction, the incentive spirometer can be used independently by the patient, which can be an advantage. This technique ensures that each inspiration is physiologically optimal and is reproduced precisely from one inspiration to the next. Patients who are surgical risks may benefit from being taught how to use the incentive spirometer preoperatively by the physical therapist in order to promote better inflation of the lungs with incentive spirometry postoperatively. However, use of a spirometer does not replace being upright and moving as much as possible. The patient continues with a regimen of breathing control and coughing maneuvers in conjunction with being upright and moving until full mobility and activities of daily living are resumed.
The application of intermittent positive pressure breathing (IPPB) appears to be less effective for the postoperative patient than previously believed. The details of this modality are described in Chapter 43.
Exercise testing echocardiography performed early after coronary bypass surgery can identify individuals who are high risk and would benefit from intensive secondary prevention as a particular focus in a cardiac rehabilitation program.34 Early exercise training improves autonomic nervous system function in addition to aerobic and functional capacity.35
Getting the Surgical Patient “Upright and Moving”
Mobilization in the upright position coordinated with breathing control and supported coughing maneuvers is encouraged immediately after the patient is first aroused after surgery, unless contraindicated, to help reverse and mitigate reduced arousal, atelectasis, FRC, and impaired mucociliary transport associated with surgery. Mobilization augments cardiovascular and pulmonary function (see Chapters 18 and 20), particularly when the patient is upright.36,37 These beneficial effects are enhanced by improved three-dimensional chest wall motion, improved gut motility, and reduced intraabdominal pressure. Extremity movement during ambulation increases alveolar ventilation, enhances ventilation and perfusion matching by increasing zone two of the lungs, and optimizes diffusing capacity through stimulating dilatation and recruitment of alveolar capillaries. The upright position ensures that the spine is erect, upper body musculature is relaxed, and the chest wall is symmetrical. Slouching and leaning, particularly to the affected side, reduce alveolar ventilation and contribute to uneven distribution of ventilation and areas of atelectasis.38,39 In addition, if this abnormal posture is maintained, mucociliary transport of the area is impaired and mucus collects and stagnates, increasing the risk of bacterial colonization and infection. Symmetrical posture is monitored at all times (i.e., during ambulation, sitting at bedside, bed mobility exercises, sitting up in bed, and lying in bed). Slouching and favoring the affected side will lead to cardiovascular and pulmonary complications and possibly musculoskeletal complications in the short and long term.
Prescription of body positioning is essential in the management of the patient postsurgically for two reasons. First, without direction, the patient will tend to assume a deleterious body position (i.e., maintaining a restricted number of body positions that favor the affected side for prolonged periods of time with minimal movement and “stirring up”). Therefore once the effects of mobilization have been exploited in a given treatment session, body positions that continue to enhance oxygen transport for a given patient and discourage excessive time in deleterious body positions are prescribed for “between-treatment” times. When not ambulating, patients are encouraged to assume a wide range of body positions (e.g., semiprone) between treatments, as frequently as possible (i.e., at least every 1 to 2 hours).40–43
Thoracic and Cardiovascular Surgery
Thoracic Surgery
At the conclusion of the surgery, chest tubes are placed to evacuate air and fluid from the pleural space by means of an underwater chest tube drainage system. The chest tube and drainage system resolve the pneumothorax created by reestablishing negative pressure in the pleural space and help to reinflate the remaining atelectatic lung tissue. After thoracic surgery, two chest tubes are usually inserted, one at the apex of the lung to evacuate air and one at the base of the lung to drain serosanguineous fluid. The therapist should become familiar with the various drainage systems, how drainage can be facilitated with mobilization and body positioning coordinated with breathing control and supported coughing maneuvers, and certain precautions that must be observed to avoid impairing drainage or disconnecting the tubing. Physical therapy for patients undergoing thoracic surgery has been reported to be cost-effective when a primary component of an interprofessional patient care management strategy44 as well as when administered prophylactically.45
Patients may appear to splint themselves, thereby restricting chest wall motion, to avoid pain when moving and deep breathing. They also may resist maximal inspiratory efforts when coughing. Although pain likely contributes to breathing at low lung volumes and ineffective coughing, phrenic nerve inhibition in patients with thoracic and upper abdominal surgeries is likely a more important factor restricting lung expansion. Being upright and moving is associated with increased FRC and tidal volume. Although modalities such as incentive spirometry may have a role in improving lung function in some high risk patients, generally it does not enhance recovery after thoracic surgery.32
Cardiovascular Surgery
Cardiovascular surgery is specialized thoracic surgery involving the heart and great vessels, most commonly for lifestyle-related ischemic heart disease. Even for individuals over 90 years of age, outcomes can be favorable.46
Because the flow of blood through the cardiovascular and pulmonary system is interrupted, the patient is placed on a cardiovascular and pulmonary bypass machine or on a machine called an extracorporeal membrane oxygenator. Cardiovascular surgery is most commonly performed for coronary artery bypass grafting, valve replacements, and aneurysm repairs. Because patients acquire an oxygen debt during the bypass procedure, high oxygen demands are present postsurgically.47
After bypass surgery, patients in whom the saphenous vein is excised for graft material have the added complication of surgery and wound healing in one leg. Mobility exercises on that leg are often restricted until there is no risk of bleeding or interference with healing. Comparable with the thoracic surgical patient, a cardiovascular patient leaves the operating room with various monitoring lines and leads, intravenous fluid infusion apparatus, possible blood or plasma infusion devices, a Swan-Ganz catheter (see Chapter 16), a central venous pressure line, an arterial line, a Foley catheter, and oxygen cannulas.
The preoperative preparation and teaching and the postoperative physical therapy management are intensive. Because of the invasiveness of cardiovascular surgery, patients are usually treated postoperatively in a specialized intensive care unit (see Chapter 33). The preoperative and postoperative physical therapy management of patients in the intensive care unit is a specialized area and is described in Chapters 34, 35 and 36.
Providing the patient with information about what to expect during the perioperative course relieves fear and anxiety. In addition, relaxation procedures can be useful. Patients must be reassured that their incisions and suture lines will not be disrupted with movement and physical therapy and that supported coughing and supporting themselves when moving will maximize comfort. Until the patient’s condition has stabilized, the patient’s mobility is restricted to low-intensity mobilization to promote its benefits on gas exchange and reduce metabolic demands and body positioning to optimize alveolar ventilation coordinated with deep breathing and supported coughing maneuvers. Although breathing exercises have been shown not to augment the benefits of body positioning and mobilization in patients after cardiac surgery,48 synchronizing breathing control with these interventions will ensure that the secretions stimulated with changing body position and moving are removed. Conventional airway clearance interventions (e.g., postural drainage and manual techniques) may be prescribed in the presence of excessive secretions or difficulty in mobilizing secretions and in the event of productive hydrostatic pneumonia. One systematic review concluded that so-called “prophylactic respiratory physiotherapy” after cardiac surgery was unsubstantiated.49 Critical components of contemporary physical therapy in the management of patients after cardiac surgery, however, include body positioning and early mobilization, which were not included as key words. The systematic review limited physical therapy simply to breathing exercises and nonspecific chest physiotherapy, which is not consistent with contemporary practice.
Patients undergoing cardiovascular surgery are transferred from the cardiovascular intensive care unit to the ward as quickly as possible. From the ward, these patients should be referred to a physical therapist and a cardiac rehabilitation program in the community for continuity of care and to maximize the functional gains resulting from the surgery. Established performance measures can be useful to streamline care and to help the patient sustain healthy living and medication adherence as needed.50
Finally, comparable to high-risk patients undergoing thoracic surgery, preoperative inspiratory muscle training has been examined in the management of high-risk patients undergoing cardiovascular surgery, in whom it has been shown to improve surgical outcomes.51 Gven the benefits of an exercise program before surgery as well as early mobilization, inspiratory muscle training needs to be shown to augment the benefits of these established interventions. Given the multisystem benefits of exercise before and after surgery, inspiratory muscle training is not an alternative.
Summary
The four categories of factors contributing to or threatening oxygen transport were described in Chapter 17 and are evaluated in the preoperative and postoperative assessments. These factors include pathology, restricted mobility and recumbency, extrinsic factors related to the patient’s care, and intrinsic factors related to the patient. This chapter examines in detail those factors related to surgery and anesthesia in particular, and the impact of underlying disease, restricted mobility, recumbency, and intrinsic factors on the effects of surgery and anesthesia. The role of the physical therapist, an integral member of the surgical team, is to ensure optimal long-term outcomes well beyond the technical success of the surgery, particularly in individuals who have undergone cardiovascular and thoracic surgery. A prime physical therapy outcome in patients who have undergone thoracic or cardiovascular surgery is prevention of both recurrence of the patient’s problem and repeated surgery.




































































