17 Incision and Drainage
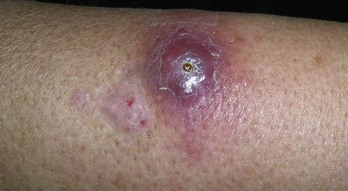
Incision and drainage (I&D) is a simple in-office procedure that in most cases is curative for superficial abscesses and related infections including uncomplicated methicillin-resistant Staphylococcus aureus (MRSA) abscesses. Commonly, patients will present with the acute onset of localized pain, swelling, and erythema indicating abscess formation (Figure 17-1). These can be the result of trauma, injection drug use, insect stings or bites, a secondary infection or inflammation of an epidermoid cyst, or paronychia from nail biting or manipulation, or they may arise without a clear inciting event.
The most common pathogens are Staphylococcus aureus and Streptococcus bacteria. Systemic antibiotics should usually only be given if there is surrounding cellulitis (Figure 17-2) or other signs or symptoms of further infection. There is no clear need for antibiotics even if localized MRSA is present, and there is also no clear indication for antibiotics in a patient with diabetes or an immune-compromised patient as long as the infection is a localized one that can be drained.1,2 Some patients may be colonized with MRSA and develop recurrent abscesses. In this situation, treatment with systemic antibiotics such as trimethoprim/sulfamethoxazole, doxycycline, or clindamycin based on local sensitivity patterns may help. Mupirocin is applied inside the nares twice daily for 5 days and topical chlorhexidine skin washing is commonly used to try to clear the carrier state, although the literature does not clearly support these practices.3,4
Contraindications and Cautions
Advantages of Incision and Drainage
Equipment
Incision and Drainage: Steps and Principles
Aftercare
There are no RCTs to inform us on how often and for how long a healing abscess should be packed.8 A small abscess can often be packed only once at the time of the I&D and then the patient can be directed to remove the packing at home in 2 days. A very large abscess may need repacking every other day for 1 to 2 weeks. Consider that each time an abscess is unpacked and repacked, it causes pain to the patient. Also the packing will delay the ultimate healing but may be needed when there is a risk that premature closure will allow a new abscess to form. Therefore, the decision on how often and how long an abscess is packed is based on physician experience, patient preferences as well as size and location.
Paronychia
Paronychia is a local bacterial infection of the nail fold. These infections are often caused by nail biting or manipulating the nail or nail margins (Figure 17-10). Prior to opening the abscess the paronychia can be locally anesthetized with ethyl chloride spray. It is important to be ready to make the cut in the paronychia quickly because the anesthetic effect is very brief. A No. 11 scalpel can be used to incise the abscess at the nail margin (Figure 17-11). These lesions are usually too small to allow packing. In more severe cases, a digital block or lidocaine injected locally may be needed. Counsel the patient to use warm soaks three times a day and to open the abscess manually if it closes and express any purulence until it heals.
Complications
Treating Specific Lesions
Special Populations
Immune-compromised patients may be particularly susceptible to localized or systemic infections that present as abscesses or skin infections. Evaluation should take into account the patient’s history, current symptoms, and physical findings. Laboratory testing, imaging studies, and systemic antibiotics may be needed and should be determined based on the overall clinical picture.9 In contrast to routine superficial abscesses, in which culture of the abscess fluid or cavity is not usually required, cultures may be helpful in these patients to guide antibiotic therapy of atypical organisms that may be present.
Coding and Billing Pearls
The CPT codes for I&D are shown in Box 17-1. Note that some specific locations have their own CPT codes. Those specific codes should be used rather than the generic ones since they often reimburse more. These areas include such cutaneous sites as the vulva, eyelid, and pinna. See Table 38-8 in Chapter 38, Surviving Financially, for a full listing of these sites and their reimbursement.
1. Lee MC, Rios AM, Aten MF, et al. Management and outcome of children with skin and soft tissue abscesses caused by community-acquired methicillin-resistant Staphylococcus aureus. Pediatr Infect Dis J. 2004;23(2):123-127.
2. Rajendran PM, Young D, Maurer T, et al. Randomized, double-blind, placebo-controlled trial of cephalexin for treatment of uncomplicated skin abscesses in a population at risk for community-acquired methicillin-resistant Staphylococcus aureus infection. Antimicrob Agents Chemother. 2007;51(11):4044-4048.
3. Loeb M, Main C, Walker-Dilks C, et al. Antimicrobial drugs for treating methicillin-resistant Staphylococcus aureus colonization. Cochrane Database Syst Rev. 2003(4):CD00340.
4. Wendt C, Schinke S, Wurtemberger M, et al. Value of whole-body washing with chlorhexidine for the eradication of methicillin-resistant Staphylococcus aureus: a randomized, placebo-controlled, double-blind clinical trial. Infect Control Hosp Epidemiol. 2007;28(9):1036-1043.
5. Ho YH, Tan M, Chui CH, et al. Randomized controlled trial of primary fistulotomy with drainage alone for perianal abscesses. Dis Colon Rectum. 1997;40(12):1435-1438.
6. Puymirat E. A Lemierre syndrome variant caused by Staphylococcus aureus. Am J Emerg Med. 2008;26(3):380.e5-380.e7.
7. Korownyk C, Allan GM. Evidence-based approach to abscess management. Can Fam Physician. 2007;53(10):1680-1684.
8. Fitch MT, Manthey DE, McGinnis HD, et al. Videos in clinical medicine. Abscess incision and drainage. N Engl J Med. 2007;357(19):e20.
9. Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft-tissue infections. Clin Infect Dis. 2005;41(10):1373-1406.


 or
or  inch depending on lesion size
inch depending on lesion size














