16 Implications of Pediatric Renal, Endocrine, and Oncologic Disease
Renal
Hypertension
Key Points
Chronic Renal Failure
The Echo Exam: Step-by-Step Approach
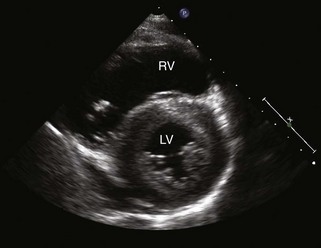
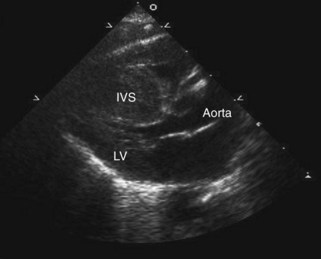
Step 1: Evaluate Cardiac Size
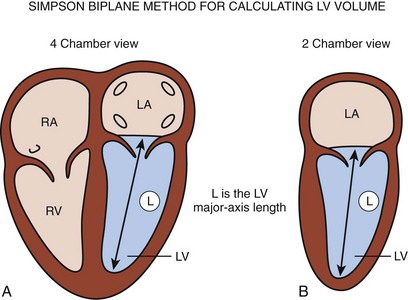
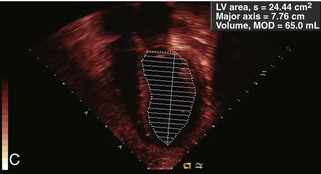
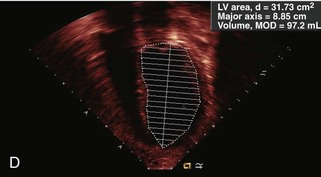
Step 2: Evaluate Systolic Cardiac Function
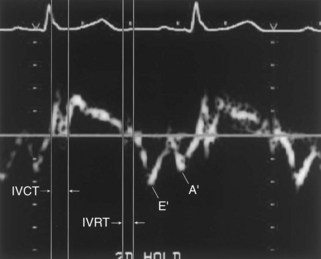
Step 3: Evaluate Diastolic Cardiac Function
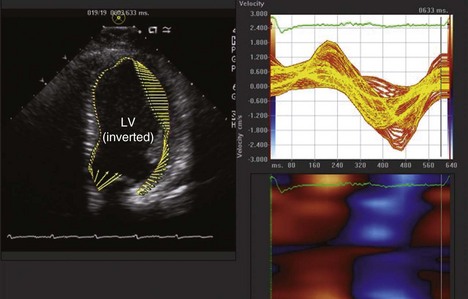
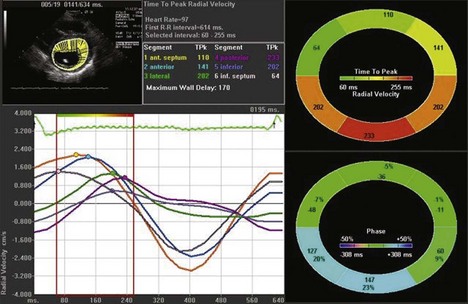
Step 4: Evaluate for Dyssynchrony
Endocrine
Hypothyroidism
Hyperthyroidism
Metabolic Syndrome
Maternal Diabetes
The Echo Exam: Step-by-Step Approach
Step 3: Evaluate Cardiac Structure
Oncologic Disease
Chemotherapeutic agents and radiation are associated with the development of CMs.
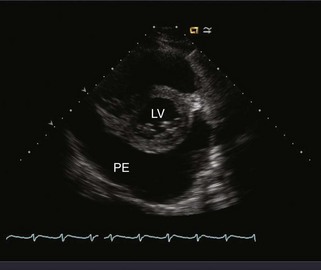
Dilated Cardiomyopathy
Restrictive Cardiomyopathy
1 Lopez L, Colan S, Frommelt P, et al. Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the Pediatric Measurements Writing Group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J Am Soc Echocardiogr. 2010;23:465-495.
2 Khoury PR, Mitsnefes M, Daniels SR, et al. Age-specific reference intervals for indexed left ventricular mass in children. J Am Soc Echocardiogr. 2009;22:709-714.
Description of a standard method for indexing LVM in the pediatric population using height and age.
3 Ucar T, Tutar E, Yalcinkaya F, et al. Global left ventricular function by tissue Doppler imaging in pediatric dialysis patients. Pediatr Nephrol. 2008:779-785.
4 Harkl AD, Cransberg K, Osch-Gevers MV, et al. Diastolic dysfunction in paediatric patients on peritoneal dialysis. Nephrol Dial Transplant. 2009;24:1987-1991.
5 Kupferman J, Paterno K, Mahgerefeh J, et al. Improvement of left ventricular mass with antihypertensive therapy in children with hypertension. Pediatr Nephrol. 2010;25:1513-1518.
6 Chavers BM, Shuling L, Collins AJ, et al. Cardiovascular disease in pediatric chronic dialysis patients. Kidney Int. 2002;62:648-653.
7 Greenbaum LA, Warady BA, Furth SL. Current advances in chronic kidney disease in children: growth, cardiovascular, and neurocognitive risk factors. Semin Nephrol. 2009;29:425-434.
8 Friedberg MK, Silverman NH, Dubin AM, et al. Mechanical dyssynchrony in children with systolic dysfunction secondary to cardiomyopathy: a Doppler tissue and vector velocity imaging study. J Am Soc Echocardiogr. 2007;20:756-763.
9 Lopez L. Advances in echocardiography. Curr Opin Pediatr. 2009;21:579-584.
10 DiBonito P, Moio N, Scilla C, et al. Preclinical manifestations of organ damage associated with the metabolic syndrome and its factors in outpatient children. Atherosclerosis. 2010;213:611-615.
A description of the cardiovascular findings associated with metabolic syndrome including LVH.
11 Abu-Sulaiman RM, Subaih B. Congenital heart disease in infants of diabetic mothers: echocardiographic study. Pediatr Cardiol. 2004;25:137-140.
Summary of findings in infants of diabetic mothers including HCM and conotruncal defects.
12 Van der Pal HJ, van Dalen EC, Hauptmann M, et al. Cardiac function in 5-year survivors of childhood cancer. Arch Inter Med. 2010;170:1247-1255.