9 Implementing an outcome-based approach in practice
The ostriches, the peacocks and the beavers
Outcome-based education, as discussed in Chapter 6, is about more than defining and publishing a set of learning outcomes that must be achieved before the end of the course. OBE is characterised by a curriculum with the learning strategies and learning opportunities designed to ensure that students achieve the learning outcomes specified and with an assessment process matched to the learning outcomes. Individual students are assessed to ensure that they achieve the outcomes. Remediation and enrichment for students is provided as appropriate.
Planning an OBE programme
An OBE curriculum starts with the question – what are the expected learning outcomes to be achieved by the end of the programme and what capabilities should the graduate have as a practising doctor? An outcome framework is used, as described in Chapter 8, to describe the broad performance capabilities. These in turn are specified in more detail. For example, in the broad domain of patient management a more detailed set of learning outcomes includes surgery, drugs, physiotherapy, social dimensions and alternative therapies.
Student progression in an OBE curriculum
Four dimensions can be considered with regard to students’ achievements of learning outcomes and their progression through the course and these are described in Chapter 12.
An OBE implementation inventory
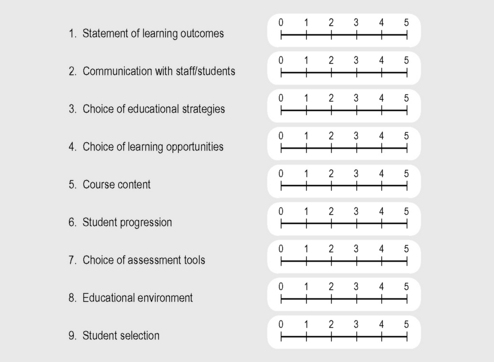
An OBE implementation inventory can be used to describe a school’s or postgraduate body’s level of adoption of an OBE approach in their education programme. This can be rated on a five-point scale in each of nine dimensions as shown in Figure 9.1:
1. The extent to which there is a clear and unambiguous statement of the learning outcomes expected.
2. Whether staff and students in an institution are made aware of and are familiar with the outcome statements.
3. The extent to which the educational strategies adopted, such as problem-based learning, community-based learning or inter-professional learning, reflect the learning outcomes. The ability to work as a member of a team alongside other healthcare professionals, for example, can be facilitated through inter-professional learning experiences.
4. The matching of the learning opportunities selected with the learning outcomes. Almost certainly this will require the use of a range of teaching and learning methods.
5. A significant problem facing medical education is the rapid expansion of knowledge with the associated danger of information overload and curriculum congestion. Consideration of the learning outcomes can help to determine what content should be covered in the curriculum.
6. The students’ achievements of the learning outcomes can be used to assess their progression through the curriculum and to determine whether they are able to proceed to the next stage.
7. The learning outcomes are important in relation to assessment. Serious problems arise when there is a mismatch between the learning outcomes, the learning experiences and the student assessment.
8. In planning an education programme, increased attention is being paid to the educational environment. This is described in Chapter 18. In OBE, the learning outcomes specified can indicate what should be a desirable learning environment. For example, a learning outcome addressing teamwork skills should suggest the need for an educational environment that supports collaborative working rather than the more typical environment where competition is rewarded.
9. The final dimension in the inventory relates to the selection of students. It can be argued that with an OBE approach, the exit learning outcomes should be reflected in the admission criteria for students. Students should be assessed on the entry-level requirements for each of the outcome domains such as communication skills, problem solving and attitudes.
Reflect and react
1. Where on the OBE inventory does your school or postgraduate body lie? Are you well on the way to an outcome-based approach or are you still at the early stages of implementation?
2. Have you clearly identified outcomes for your own areas of teaching responsibility and is it clear how these contribute to the overall outcomes for the training or education programme?
3. Consider how you use learning outcomes to monitor and guide students’ progression.
Harden R.M. Outcome-based education – the ostrich, the peacock and the beaver. Med. Teach.. 2007;29:666-671.
Harden R.M. Learning outcomes as a tool to assess progression. Med. Teach.. 2007;29:678-682.
A description of how students progress to the achievement of the learning outcomes.
Burke J., editor. Outcomes, Learning and the Curriculum. Implications for NVQs, GNVQs and other qualifications. London: The Falmer Press, 1995.
Holmboe E.S., Ward D.S., Reznick R.K., et al. Faculty development in assessment: the missing link in competency-based medical education. Acad. Med.. 2011;86:460-467.