CHAPTER 4 Implant Choices: The Biomechanics of Anchors and Sutures
HISTORY
Before the development of suture anchors, the attachment of ligament or tendon to bone was accomplished by first creating a bone tunnel and then passing sutures through the bone tunnel. Awls or drills were used to create the bone tunnels. Suture was passed through the tunnels and then tied over the bone bridge. This technique worked relatively well for open procedures, but could not be used for arthroscopic repairs.1 As surgeons attempted to do more through less invasive surgeries, the first-generation suture anchor was introduced by Mitek, called the G1 anchor.2 This anchor gave the surgeon the ability to attach a suture to bone without having to create a bone tunnel.
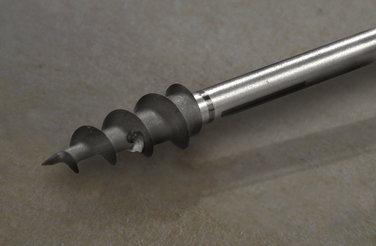
The first screw-in suture anchor was developed about the same time as the G1, called the Statak anchor. This anchor was designed by Marlowe Goble and had a suture secured in the center of a screw anchor.1 Since the introduction of these original suture anchor designs, dozens of different screw-in and non–screw-in anchors have been developed. All these anchors are designed to achieve the goal of attaching a suture to bone.
SUTURE ANCHORS
There are many suture anchors on the market today. In general, they can be classified as screw-in or and non–screw-in anchors. To assist with the selection of the proper anchor, it is important to understand the basic biology of tissue healing. The three main phases of tissue healing have been summarized by Barber and Boothby1 and progress from inflammation through repair and finally tissue remodeling. Initially, inflammatory cells fill the gaps between the tendon and the bone. The inflammatory cells gradually become organized and are then invaded by a vascular supply, which aids in the removal of debris and the formation of collagen-forming cells. These cells act to close the tissue gap. This entire process takes at least 12 weeks, but is likely to vary according to the specific tissue in question, as well as the patient’s preinjury metabolic status and inherent vascularity.3 A surgeon must select an anchor that will hold the tissue in close enough proximity to the bone so that gapping does not occur before the final phases of tissue healing can occur.
A good suture anchor has several characteristics, which have been outlined by Barber and colleagues.1,4,5 The suture anchor should do the following: (1) fix the suture to bone; (2) not pull out of the bone with stress; (3) be easy to place surgically; (4) allow for arthroscopic knot tying; (5) have the capacity to hold multiple sutures; and (6) not cause long-term morbidity. Some of the specific anchor qualities that should be considered include the size and shape of the anchors, type and location of the eyelet in the anchor, anchor material, method of insertion, and method of failure (Box 4-1).3 Barber and associates have carried out a number of studies on the fixation strength of various suture anchors and their modes of failure and have recently published updates with information on the latest designs.6,7
Anchor Size
Suture anchors come in many different sizes. Both the diameter of the outside of the anchor and the core of the anchor should be considered.1,5 Historically, larger screw-in anchors with deep threads were the anchor of choice in humeral heads that were osteoporotic. However, newer non–screw-in anchors with smaller diameters may show comparable strength,3 although anchor performance is affected by the quality of the bone, which can be a significant concern, especially in older patients. For rotator cuff repairs, the larger suture anchors are advantageous because they can hold more sutures than smaller anchors. Very large suture anchors (6.5 mm and larger) cause crowding and limit the placement of all the anchors in ideal locations. Therefore, with the improved strength of smaller diameter anchors, these extremely large anchors are often not practical.4
When placing sutures into the dense bone of the glenoid for labral repairs, smaller anchors may have an advantage because they are less likely to cause significant damage to the articular cartilage.1 The limitation is that they are often not able to accommodate as many sutures per anchor.
Anchor Type
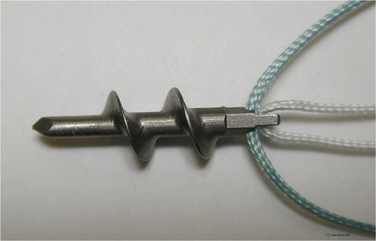
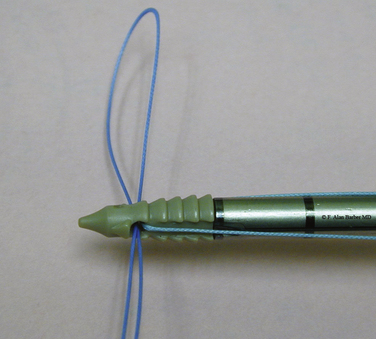
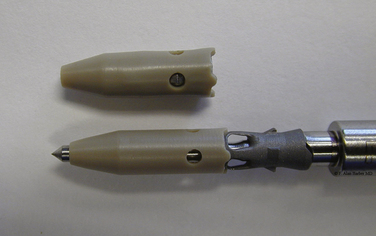
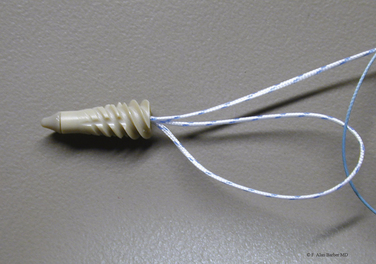
Anchors come in several different shapes. In general, they can be divided between screw-in and non–screw-in designs (Figs. 4-1 and 4-2). As described by Barber,4 non–screw-in anchors are those that toggle, push in, or change their morphology after being pushed into the bone (Fig. 4-3).
Another variation is an anchor that works more like a tack. These have a bar or disk attached, which holds the tendon on the bone. There are several disadvantages of these designs. They often create a larger hole in the tendon and are usually very difficult to remove once they are placed in the bone.1 They do, however, eliminate the need to pass sutures through the tissue or tie any knots.4
Screw anchors are a good anchor choice for the osteoporotic bone of the humeral head and tuberosity. The screw in anchors typically have high load to failure strength. However, Pedowitz18 has demonstrated that even screw-in anchors can have significant translation in the humeral head after cyclical loading, particularly when load is applied oblique to the angle of anchor insertion, which is the physiologic direction of loading with a rotator cuff repair. Many of the suture anchors, both screw-in and non–screw-in, now allow easy movement of the suture through the eyelet so that sliding knots can be used. Many anchors have eyelets large enough to allow multiple sutures to pass and some allow the surgeon to change out the suture if they desire.4
Anchor Eyelets
The shape of an anchor’s eyelet is another important consideration. The eyelet can be a potential site of anchor failure.4,9 The rotation of the eyelet in relationship to the line of force has been shown to affect suture fretting and load to failure force.10,11 This may be more pronounced with metal suture anchors because the eyelets might have sharp edges that can contribute to suture failure if the alignment of the suture and the eyelet is not correct.3
Many anchors now have two or more sutures loaded into them. To accommodate multiple sutures, different eyelet designs have been used. These designs include a long vertically oriented eyelet, a wide horizontally orientated eyelet, or a distal cross bar.4 The horizontal eyelets make it easier to tie sliding knots with both sutures. Some designs have been introduced that have eyelets made from a braided flexible suture. To avoid the problem of having multiple sutures binding up inside the eyelet, some anchors have two independent suture channels, which can be at different angles to each other or on different sides of the eyelet column.
Anchor Material
Metal and biodegradable anchors are used frequently. Recently, there has been a trend toward the development of more biodegradable anchors. The benefits of metal anchors have been summarized by Barber and Boothby.1 These anchors provide good strength and are relatively easy to insert, and can easily be evaluated with x-ray.
Modern biodegradable anchors have pull-out strengths similar to those of metal anchors and are just as easy to insert.12–14 As noted, the eyelets of biodegradable suture anchors may be associated with less damage to the suture, regardless of whether the suture is damaged.15 Barber and Boothby have noted other benefits associated with biodegradable anchors.1 They are easier to revise, can be used in pediatric patients, eventually resorb, and produce less artifact with magnetic resonance imaging (MRI). Overall, newer biodegradable anchors are becoming easier to use and provide excellent pull-out strength.16
Most of the bioabsorbable anchors are made out of polyglyconate (PGA) or poly-L-lactic acid (PLLA).1 Some are hybrid and are composed of PGA and PLLA. Each polymer behaves in a unique fashion. PGA has been linked to complications, including restricted shoulder motion and a hyperinflammatory response.1 PLLA can take up to 4 years to resorb completely and the problems reported with these implants have been primarily mechanical. A recent study of the use of PLLA anchors in labral repairs has demonstrated postoperative enlargement of drill holes that were filled with these anchors and a correlation with less favorable results in function and stability.17 However, another study, which followed patients for 7 to 8, has years noted that the drill holes used for the placement of PLLA anchors healed in most patients.18
Recently, nonbioabsorbable and nonmetallic materials have been introduced in suture anchors. Polyetheretherketone (PEEK) is a chemically resistant crystalline thermoplastic that maintains its integrity in a wide pH range. It withstands high temperatures and can be found in automotive, aerospace, and industrial applications. As a suture anchor, it creates a nonabsorbable, strong, radiolucent anchor that may be drilled out during revision surgery. However, radiolucent anchors (absorbable or nonabsorbable) may be difficult to localize if they become dislodged at some point after surgery; this is important, because these anchors can cause significant injury to articular cartilage and other periarticular tissues (Figs. 4-4 and 4-5).
It is important for the bioabsorbable implants to retain their strength during the critical phases of tissue healing. Clinically, they appear to do this.18 Once healing has occurred, other factors, including bone-implant reactions and the potential for loose body formation caused by implant breakage, become more important.8
Anchor Placement
In the past, surgeons were satisfied if they could get the tendon near the bone attachment site without a lot of tension. Recent appreciation and understanding of margin convergence and the interval slide technique have made it easier for surgeons to reattach the rotator cuff to the footprint on the greater tuberosity.4
Barber has outlined the different options for the placement of anchors to achieve attachment over the footprint.4 These include the following: (1) locating the anchors at the edge of the articular humeral cartilage to reduce tension on the tendon; (2) locating the anchors more laterally but on top of the tuberosity; (3) locating the anchors on the side of the humeral shaft (over the edge) in the cortical bone, and using a tension band suture to compress the tendon down to the prepared site on the greater tuberosity; and (4) using a double row of anchors, one that fixes the tendon near the articular cartilage and the second more laterally to fix the rest of the rotator cuff tendon across the full extent of the normal cuff footprint.”
Although double-row repairs help increase the bone-tendon contact area, hopefully to facilitate healing, the increased surgical costs, anchor crowding, and potential of complicating any revision surgery should be considered.4 A recent study in an animal model has shown no statistically significant difference in the strength of a rotator cuff repair when two or four anchors were used.19 Another study has shown no biomechanical advantage of single-row versus double-row repairs in a bovine model.20 However, other biomechanical studies have supported the use of double-row repairs, especially in large, unstable rotator cuff tears, because double-row repairs are significantly more resistant to cyclic displacement and exhibit decreased gap formation when compared with single-row repairs in tension-free and tension repairs.21–23 Double-row repairs have also been shown to cover over twice the amount of the footprint when compared with a single-row repair.24 A variety of double row techniques have been shown to work well for rotator cuff repairs.25 Meier and Meier23 have shown that double-row fixation could be even stronger than a traditional transosseous repair. Overall, the primary advantages of this technique are increased contact area and probably increased stability. The primary disadvantages of a double-row repair are increased cost, increased surgical time, and potential for stress overload of the repair because of excessive lateralization of the residual tendon.
There are three main techniques to pass the suture through the tissue. In the anchor-first method, the anchor is placed into the bone and then the suture is passed through the tissue. The In the suture-first technique, the suture is passed through the soft tissue and then loaded onto an anchor, which is subsequently placed into the bone. The final technique is a transtissue technique, in which a threaded anchor is passed through the soft tissue and directly into the bone. The most popular technique is the anchor-first technique, which can use screw and non–screw-in anchors.5
Another consideration regarding suture anchor placement is bone density. There are regional differences in bone density in the greater tuberosity. The anterior area of the greater tuberosity is denser than the posterior area and therefore load to failure has been shown to be different in these two areas.4 Tingart and colleagues 26 have concluded that suture anchors should be placed in the proximal-anterior and middle parts of the greater tuberosity because of concern about anchor failure in other areas that are associated with poor bone density. Bone mineral density is a predictor of initial strength, final gap opening, and pull-out strength for all types of suture anchors. Therefore, as predicted, studies have confirmed that gapping is more common over the posterior aspect of the tuberosity rather than the anterior aspect.13,14,27 Similarly, anchors fail earlier in older bone as compared with younger bone because of osteoporosis.28
The angle of anchor insertion should also be considered. Studies have provided evidence in support of and against the insertion at approximately 45 degrees off the vertical (dead man angle).8 This 45-degree angle should be considered the maximum acceptable angle for insertion. More acute angles of insertion often place the anchor into better bone, especially with rotator cuff repair. Chronic cuff tears are often associated with an osteoporotic (hollow) humeral head, and a more tangential (acute) insertion angle placing the anchor into the subchondral bone at the top of the humeral head will provide better fixation strength. The depth of anchor insertion is also important, because studies have shown that anchors inserted deeply fail by suture cutting through the bone, or they displace by rotating and translating toward the cortical surface, whereas those inserted proud were associated with failure at the eyelet.29,30 The ideal depth of insertion appears to be just below the cortical bone, so that the anchor is not prominent, while at the same time attempting to use the cortical bone for fixation when possible, as opposed to deliberate anchor insertion into weaker cancellous bone (Fig. 4-6).
Anchor Failure
In the entire construct, there are many potential sources of failure. One form of failure is pull-out of the anchor from the bone. This type of failure is more common with push-in designs.1 Pull-out is more likely to occur in osteoporotic bone and is less likely in areas of good cortical bone. If the anchor toggles, the angle of insertion is too great (>45 degrees), or the sutures can create a trough in the bone; these can all increase the likelihood of suture pull-out.1 One study comparing standard and intracortical suture anchors found that after cyclic loading, anchor motion in the bone accounted for one third of the total displacement of the suture or anchor construct for both types of anchors. This led to increased construct displacement, which clinically might lead to failure of the repair.31 Although rarely needed, bone cement (or other substrate-strengthening strategies) can be used to augment suture anchor fixation; this reduces the risk of anchor pull-out, regardless of whether the suture anchor is stripped or not.32
The weakest link in the construct is probably the suture-tendon interface. The potential for sutures to cut through tendon fibers is a concern both during surgery, when a sliding knot pulls the suture through the tendon because of excessive force, and postoperatively, with cyclic loading.1 Several options to help decrease the chances of this type of failure include using knots that will grasp the tendon more effectively, using more sutures to distribute the force across a larger area,4 and using suture reinforcement adjacent to transtendon sutures (a so-called rip-stop suture).
Another form of anchor failure is seen with eyelet breakage. Strong sutures cycling through a biodegradable eyelet or a suture eyelet can lead to breakage of the eyelet itself. With multiple sutures passed through a single eyelet, there is increased stress on the eyelet and, if one suture cuts through the eyelet, all the sutures in that anchor then fail.1
Suture breakage is also a possible mode of failure. With the newer supersutures on the market, the risk of breaking an undamaged suture is relatively low. However, the risk goes up substantially if the suture becomes frayed or nicked—for example, by suture-passing instruments or sharp stabbing instruments. Sutures can be damaged on insertion and knot tying, with inadvertent clamping of the suture in the area where the knot will lie, using damaged arthroscopic instruments, or nicking the coating of the suture in any other way.1 If the anchor is placed too deeply, the suture could rub against the bone edge and potentially rupture.
SUTURES
Suture Size
The size of the suture is a major factor in the strength of the repair (Box 4-2). Therefore, this should influence the anchor that is chosen. If performing labral repair, a no. 2 suture should exceed the strength needed for the repair. The ability to pass the suture and tie it easily may be more of a concern in this application. The use of ultra–high-molecular-weight polyethylene (UHMWPE) in sutures makes the likelihood of suture breakage with cyclic loading after a cuff repair a lesser concern.1,5 However, the increased strength may put more stress on the eyelet or could increase the rate at which the suture cuts through the soft tissue. In addition, studies have shown that knots tied with UHMWPE can slip at lower levels when compared with comparably sized conventional braided polyester sutures.43 Pedowitz18 has demonstrated that intracortical anchors loaded with an UHMWPE were more likely to fail at the suture-anchor interface when compared with anchors loaded with the same size of braided polyester suture. These are concerns to be considered with the newer high-strength sutures.3
Suture Material
An ideal suture used for rotator cuff repair should be strong enough to withstand the forces that are applied to it, show little creep while the tissue is healing, be easy to use, allow knots to slide smoothly, and not cut through the tissue.3 The sutures used in rotator cuff repair can be divided into monofilament or braided sutures and absorbable or nonabsorbable sutures. An advantage of monofilament suture is the ease of passing it through tissue, especially in devices with hollow needles, because the suture’s stiffness facilitates pushing it within the tool. The disadvantage is that it is difficult to get knots to lie down and the knots have a tendency to slip.8 In contrast to monofilament sutures, braided sutures are typically stronger and more pliable. Conventional braided sutures have been replaced by stronger sutures that use UHMWPE. The first of these was FiberWire, introduced by Arthrex (Naples, Fla). Subsequently several companies introduced sutures based on a weave of UHMWPE. Despite the increased strength of these sutures, they can still slip.4 When compared with Ethibond (Ethicon, Somerville, NJ), a braided polyester nonabsorbable suture, a similarly sized FiberWire (no. 2) had a greater ultimate load to failure, greater stiffness, and greater stress relaxation.33 A recent study seems to indicate that FiberWire performs better when used with nonabsorbable anchors.15 However, as noted, studies have also shown that FiberWire can slip more often and be more likely to fail at the suture-anchor interface when compared with Ethibond.34,43 Orthocord (DePuy Orthopaedics, Warsaw, Ind) was more recently introduced; no. 2 Orthocord is made from a combination of UHMWPE (32%) and polydioxanone (PDS; Ethicon) (68%) and coated with polyglactin 910. It has a core of PDS and a UHMWPE sleeve. This is designed to have a low profile after the PDS has dissolved but yet retain it strength from the UHMWPE component. The load to failure for all these newer sutures, including FiberWire and Orthocord, typically exceeds that needed for secure bone to tendon fixation.1,35 Another advantage of sutures made out of UHMWPE is that they show a decreased resistance to fraying when compared with braided polyester sutures such as Ethibond or absorbable monofilament polydiaxonone suture such as PDS.34
As long as they maintain their strength until the healing process is complete, absorbable sutures are advantageous in the long run because they minimize residual knots that could cause mechanical impingement/subacromial space irritation. Monofilament PDS is an absorbable suture occasionally used with anchors in the shoulder; it has been shown to retain only 40% of its originally strength 6 weeks after surgery and dissolves 9 weeks after implantation.1 Despite their early degradation, successful rotator cuff repairs have been performed with these sutures.8 There may be no optimal suture for rotator cuff repair. The basic principle holds that the suture must be strong enough and last long enough to provide mechanical stability until solid tissue healing is achieved.
Knot Types
For knot comparison, the surgeon’s knot or square knot is the standard. The challenge in placing a surgeon’s knot arthroscopically is that it can slip before placement of the initial back-up hitch. Then, after being locked by that hitch, the knot is difficult to advance. Loop security is just as important as knot security for the repair construct because loose loops give up slack with every load and create a gap at the tendon-bone interface. Reversed posts and reversed hitches are more secure than stacked half-hitches on a single post. It is possible to reverse the post of an arthroscopic knot by changing the tension on the limbs when the hitch is brought into the cannula.8
Many arthroscopic knots have been described. Most work well as long as the surgeon maintains good loop and knot security. Some of the common knots are the Duncan loop, Revo knot, San Diego knot, SMC knot, Tennessee slider, and Weston knot (Figs. 4-7 to 4-12). An arthroscopic surgeon should be good at tying at least one sliding knot and one nonsliding knot. Arthroscopic knots can essentially be locked into place by the placement of at least three reversed throws on reversed posts to back up the initial knot.8 Different knots perform differently for different surgeons and with different sutures. Therefore, each surgeon should find a good suture material and knot combination that works well: this tends to be a personal choice. Recent evidence has suggested that because of the increased tendency of the newer high strength sutures to slip, the Duncan knot and Weston knot should be avoided if an UHMWPE-based suture is used.34

FIGURE 4-7 The Duncan loop.
(From Barber FA, Herbert MA, Beavis RC. Cyclic load of arthroscopic knots and high strength sutures. Arthroscopy. 2009; 25:192-199.)

FIGURE 4-8 The Revo knot.
(From Barber FA, Herbert MA, Beavis RC. Cyclic load of arthroscopic knots and high strength sutures. Arthroscopy. 2009; 25:192-199.)

FIGURE 4-9 The San Diego knot.
(From Barber FA, Herbert MA, Beavis RC. Cyclic load of arthroscopic knots and high strength sutures. Arthroscopy. 2009; 25:192-199.)

FIGURE 4-10 The SMC knot.
(From Barber FA, Herbert MA, Beavis RC. Cyclic load of arthroscopic knots and high strength sutures. Arthroscopy. 2009; 25:192-199.)

FIGURE 4-11 The Tennessee slider.
(From Barber FA, Herbert MA, Beavis RC. Cyclic load of arthroscopic knots and high strength sutures. Arthroscopy. 2009; 25:192-199.)

FIGURE 4-12 The Weston knot.
(From Barber FA, Herbert MA, Beavis RC. Cyclic load of arthroscopic knots and high strength sutures. Arthroscopy. 2009; 25:192-199.)
A welding technique for polypropylene suture has been described that eliminates the need for knot tying. In the laboratory, welded loops appear to have less elongation but also lower mean loads to failure. Their in vivo performance and clinical outcomes are yet to be determined.8 Knotless suture anchors are also becoming more prevalent. Laboratory studies have shown that they have strength to support soft tissue repairs, especially around the glenoid, but also when incorporated into rotator cuff repairs.25,27,36
Suture Configuration
A number of suture configurations can be used to stabilize tendons. Some are similar to those used in open repair and others are specifically designed for arthroscopic procedures. The holding power of a suture is often limited because the tendon is frequently degenerative and atrophic. Studies of the Mason-Allen stitch configuration have had mixed results. Some have demonstrated superior strength in load to failure testing when compared with a mattress suture or simple suture.3 Other studies of the arthroscopically placed Mason-Allen stitch did not show an increase the strength of a repair and, in some cases, even had increased early gap formation when compared with mattress suture configurations.8,37 The gap formation was attributed to the slack that was present in the complex loops of the suture in the tendon; this emphasizes the importance of taking the slack out of any grasping stitch prior to arthroscopic knot tying. In an animal model, Cummins and associates38 have concluded that suture configurations that pass more frequently through the tendon enhance initial repair strength.
In general, more sutures in a cuff repair should decrease the load per suture or knot and should improve holding power of the construct. Adding more points of fixation should also increase the surface contact area for tissue healing and has been shown to increase initial repair strength.38 The downside of having too many sutures and anchors include the potential for devascularization and interference with the healing response, bulkiness and subsequent mechanical irritation in the subacromial space, technical difficulty, and added expense.8
Suture Number
Most newly developed suture anchors allow multiple sutures to be used per device. For rotator cuff surgery, these anchors with two or more sutures have an advantage because of the tension of the repair and have been shown to improve initial repair strength.38 One study found rotator cuff repair in cadavers with two doubly loaded suture anchors to have better initial fixation than two singly loaded suture anchors, repair with rotator cuff tacks, and even open transosseous repair.39 It is not necessarily advantageous in labral repairs because multiple points of fixation are more important, which this is best accomplished with smaller anchors.5 Biodegradable anchors loaded with two sutures each do well when cyclically loaded, even in older bone.28 When comparing suture anchors with two or three sutures, three simple sutures hold better than two simple sutures alone and also held better than a single mattress and two simple sutures.40 In general, our objective is to balance the repair so that a similar magnitude of tension will be applied to all sutures postoperatively. Otherwise, the single suture with an unduly high amount of tension will tend to fail first, followed by the next suture to see high tension, and so on. If the repair is unbalanced, construct strength will be defined by that element of the repair that sees the highest initial loads (in other words, by the weakest link in the chain).
Modes of Suture Failure
Sutures can fail because of a variety of reasons. Suture failure can be related to surgical technique, quality of the soft tissue, and quality of the anchors and suture material used.41 Two common suture difficulties include knots not sliding and sutures breaking. With familiarity of the implant and practice, these complications can be minimized. If the knot will not slide or gets becomes in a cannula, options include attempts to remove the device or untie the knot, or placement of another device in or near the site of the original anchor. If a suture breaks, another type of anchor or suture may need to be used. If the suture pulls out of the tissue, the tissue quality in the location of the originally placed suture should be reassessed before another suture is placed in the same tissue. If the tissue is not healthy, a new location may need to be selected for placement of the suture. The surgeon should avoid macerating good tissue with too many suture passes. Chokshi and coworkers42 have demonstrated that suture-passing devices that create larger holes in the cuff can compromise the integrity of the repair. However, an increased number of sutures can provide better and more balanced fixation and prevent soft tissue disruption.41 A recent study has demonstrated that external rotation places increased tension on anterior sutures used for a supraspinatus tendon repair. Similarly, it was shown that internal rotation places increased tension on posterior sutures. This study suggests that internal rotation and external rotation stretching be avoided during the healing of supraspinatus repairs to prevent too much tension from being placed on the anterior or posterior sutures, which could lead to failure.44
SUMMARY
There are a number of biomechanical factors that should be considered when selecting sutures and suture anchors for arthroscopic shoulder surgery. Regardless whether a screw-in or non–screw-in anchor is selected, the anchor must be able to maintain the soft tissue in close enough proximity to the bone until natural biologic healing of the tissue to the bone has occurred. Although there is little practical use for very large anchors, larger anchors do tend to have a higher load to failure than smaller diameter anchors. Smaller diameter anchors are appropriate for the glenoid to minimize articular cartilage damage. Anchor eyelets can be a potential site of suture abrasion or suture anchor failure and should also be a consideration in the selection of an appropriate anchor. More biodegradable anchors are being developed. Both biodegradable and metal anchors have their own potential complications. Depth and bone density are important factors related to the placement of suture anchors. Anchors can fail because of pull-out of the anchor, suture breakage, sutures pulling through the tissue, or eyelet failure. Suture size has an impact on the strength of the repair. Newer sutures are being introduced that have very high failure strengths. Various arthroscopic knots have been described; each surgeon should find at least one that works well for him or her. It is important to get the tension out of any suture configuration that is chosen before the knots are tied to prevent gapping when the construct is cyclically loaded. For rotator cuff repairs, suture anchors with two or more sutures per anchor are preferred.
PEARLS&PITFALLS
PEARLS
PITFALLS
1. Barber FA, Boothby MH. Suture anchor options. In: Levine WN, Blaine TA, Ahmad CS, editors. Minimally Invasive Shoulder and Elbow Surgery. New York: Informa Healthcare; 2007:34-54.
2. Kaar TK, Schenck RCJr, Wirth MA, Rockwood CA. Complications of metallic suture anchors in shoulder surgery. Arthroscopy. 2001;17:31-37.
3. McFarland EG, Park HB, Keyurapan E, et al Suture anchors and tacks for shoulder surgery, part 1: biology and biomechanics. Am J Sports Med, 33; 2005:1918-1923.
4. Barber FA. Suture anchor options. In: Abrams JS, Bell RH, editors. Arthroscopic Rotator Cuff Surgery: A Practical Approach to Management. New York: Springer; 2008:34-54.
5. Barber FA, Boothby MH, Richards DP. New suture and suture anchors in sports medicine. Sports Med Arthrosc Rev. 2006:14177-14184.
6. Barber FA, Herbert MA, Beavis RC, et al Suture anchor materials, eyelets, and designs: update 2008. Arthroscopy, 24; 2008:859-867.
7. Barber FA, Herbert MA, Coons DA, et al. Sutures and suture anchors—update 2006. Arthroscopy. 2006;22:1063-1069.
8. Deakin M, Stubbs D, Bruce W, et al. Suture strength and angle of load application in a suture anchor eyelet. Arthroscopy. 2005;21:1447-1451.
9. Meyer DC, Nyffeler RW, Fucentese SF, Gerber C. Failure of suture material at suture anchor eyelets. Arthroscopy. 2002;18:1013-1019.
10. Bardana DD, Burks RT, West JR, Greis PE The effect of suture anchor design and orientation on suture abrasion: An in vitros study. Arthroscopy, 19; 2003:274-281.
11. Dejong ES, DeBerardino TM, Brooks DE, et al. In vivo comparison of a metal versus a biodegradable suture anchor. Arthroscopy. 2004;20:511-516.
12. Tashjian RZ, Levanthal E, Spenciner DB, et al Initial fixation strength of massive rotator cuff tears: in vitro comparisons of single-row suture anchor and transosseous tunnel constructs. Arthroscopy, 23; 2007:710-716.
13. Meyer DC, Mayer J, Wber U, et al Ultrasonically implanted PLA suture anchors are stable in osteopenic bone. Clin Orthop (442); 2006:143-148.
14. Wright RB, Budoff JE, Yeh ML The properties of damaged and undamaged suture used in metal and bioabsorbable anchors: an in vitro study. Arthroscopy, 23; 2007:655-661.
15. Ozbaydar M, Elhassan B, Warner JJP The use of anchors in shoulder surgery: a shift from metallic to bioabsorbable anchors. Arthroscopy, 23; 2007:1124-1126.
16. Take Y, Yoneda M, Hayashida K, et al Enlargement of drill holes after use of a biodegradable suture anchor: quantitative study on consecutive postoperative radiographs. Arthroscopy, 24; 2008:251-257.
17. Magnusson L, Ejerhed L, Rostgård L, et al. Absorbable implants for open shoulder stabilization. A 7-8-year clinical and radiographic follow-up. Knee Surg Sports Traumatol Arthrosc. 2006;14:182-188.
18. Pedowitz RA. Shoulder anatomy and biomechanics. In: Johnson DH, Pedowitz RA, editors. Practical Orthopaedic Sports Medicine and Arthroscopy. Philadelphia: Lippincott Williams & Wilkins; 2007:145-159.
19. Fealy S, Rodeo SA, MacGillivray JD, et al. Biomechanical evaluation of the relation between number of suture anchors and strength of the bone-tendon interface in a goat rotator cuff model. Arthroscopy. 2006;22:595-602.
20. Mahar A, Tamborlane J, Oka R, et al. Single-row suture anchor repair of the rotator cuff is biomechanically equivalent to double-row repair in a bovine model. Arthroscopy. 2007;23:1265-1270.
21. Milano G, Grasso A, Zarelli D, et al Comparison between single-row and double-row rotator cuff repair: a biomechanical study. Knee Surg Sports Traumatol Arthrosc, 16; 2008:75-80.
22. Cole BJ, El Attrache NS, Anbari A Arthroscopic rotator cuff repairs: an anatomic and biomechanical rationale for different suture anchor configurations. Arthrsocopy, 23; 2007:662-669.
23. Meier SW, Meier JD The effect of double-row fixation on initial repair strength in rotator cuff repair: a biomechanical study. Arthroscopy, 22; 2006:1168-1173.
24. Brady PC, Arrigoni P, Burkhart SS. Evaluation of residual rotator cuff defects after in vivo single- versus double-row rotator cuff repairs. Arthroscopy. 2006;22:1070-1075.
25. Zheng N, Harris HW, Andrews JR Failure analysis of rotator cuff repair: a comparison of three double-row techniques. J Bone Joint Surg Am, 90; 2008:1034-1042.
26. Tingart MJ, Apreleva M, Lehtinen J, et al Anchor design and bone mineral density affect the pull-out strength of suture anchors in rotator cuff repair: which anchors are best to use in patients with low bone quality. Am J Sports Med, 32; 2004:1466-1473.
27. Brown BS, Cooper AD, McIff TE, et al. Initial fixation and cyclic loading stability of knotless suture anchors for rotator cuff repair. J Shoulder Elbow Surg. 2008;17:313-318.
28. Barber FA, Coons DA, Ruiz-Suarez M. Cyclic load testing of biodegradable suture anchors containing 2 high-strength sutures. Arthroscopy. 2007;23:355-360.
29. Mahar AT, Tucker BS, Upasani VV, et al. Increasing the insertion depth of suture anchors for rotator cuff repair does not improve biomechanical stability. J Shoulder Elbow Surg. 2005;14:626-630.
30. Bynum CK, Lee S, Mahar A, et al. Failure mode of suture anchors as a function of insertion depth. Am J Sports Med. 2005;33:1030-1034.
31. Mahar A, Allred DW, Wedemeyer M, et al. A biomechanical and radiographic analysis of standard and intracortical suture anchors for arthroscopic rotator cuff repair. Arthroscopy. 2006;22:130-135.
32. Giori NJ, Sohn DH, Mirza FM, et al Bone cement improves suture anchor fixation. Clin Orthop (451); 2006:236-241.
33. Acton D, Perry A, Evans R, et al. The effect of two nonresorbable suture types on the mechanical performance over a metal suture eyelet. Knee Surg Sports Traumatol Arthrosc. 2004;12:165-168.
34. Bisson LJ, Manohar LM, Wilkins RD, et al Influence of suture material on the biomechanical behavior of suture-tendon specimens: a controlled study in bovine rotator cuff. Am J Sports Med, 36; 2008:907-912.
35. Wüst DM, Meyer DC, Favre P, Gerber C. Mechanical and handling properties of braided polyblend polyethylene sutures in comparison to braided polyester and monofilament polydioxanone sutures. Arthroscopy. 2006;22:1146-1153.
36. Leedle BP, Miller MD. Pullout strength of knotless suture anchors. Arthroscopy. 2005;21:81-85.
37. Klinger HM, Buchhorn GH, Heidrich G, et al Biomechanical evaluation of rotator cuff repairs in a sheep model: suture anchors using arthroscopic Mason-Allen stitiches. Clin Biomech, 23; 2008:291-298.
38. Cummins CA, Appleyard RC, Stickland S, et al Rotator cuff repair: an ex vivo analysis of suture anchor repair techniques on initial load to failure. Arthroscopy, 21; 2005:1236-1241.
39. Chhabra A, Goradia VK, Francke EI, et al In vitro analysis of rotator cuff repairs: a comparison of arthroscopically inserted tacks or anchors with open transosseous repairs. Arthroscopy, 21; 2005:323-327.
40. Coons DA, Barber FA, Herbert MA Triple-loaded single-anchor stitch configuration: an analysis of cyclically loaded suture-tendon interface security. Arthroscopy, 22; 2006:1154-1158.
41. Park HB, Keyurapan E, Gill HS, et al Suture anchors and tacks for shoulder surgery, part II: the prevention and treatment of complications. Am J Sports Med, 34; 2006:136-144.
42. Chokshi BV, Kubiak EN, Jazrawi LM, et al. The effect of arthroscopic suture-passing instruments on rotator cuff damage and repair strength. Bull Hosp Joint Dis. 2006;63:123-125.
43. Abbi G, Espinoza L, Odell T, et al Evaluation of 5 Knots and 2 Suture Materials for Arthroscopic Rotator Cuff Repair: Very Strong Sutures Can Still Slip. Arthroscopy: The Journal of Arthroscopic and Related Surgery, 22(1); 2006:38-43.
44. Ahmad CS, Kleweno C, Jacir AM, et al Biomechanical performance of rotator cuff repairs with humeral rotation: a new rotator cuff repair failure model. Am J Sports Med, 36(5); 2008:888-892.