CHAPTER 21 Imperforate Anus
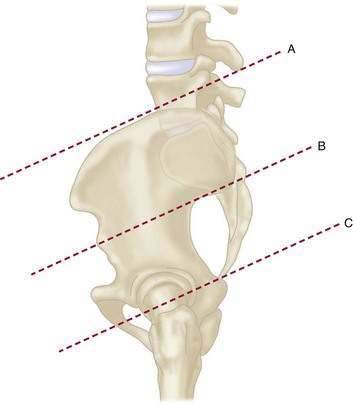
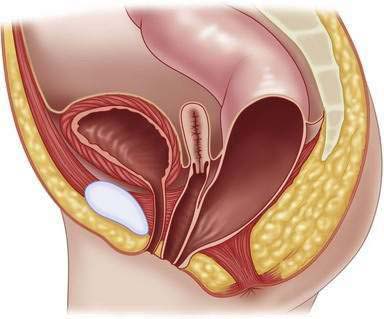
Step 1: Surgical Anatomy
Step 2: Preoperative Considerations
Associated Defects
Sacrum and Spine
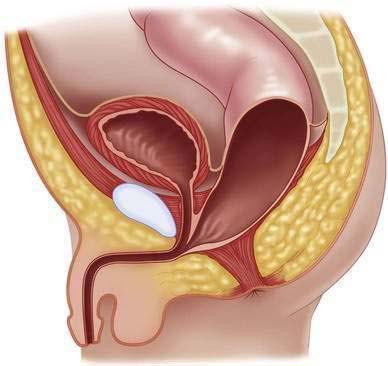
Urogenital Defects
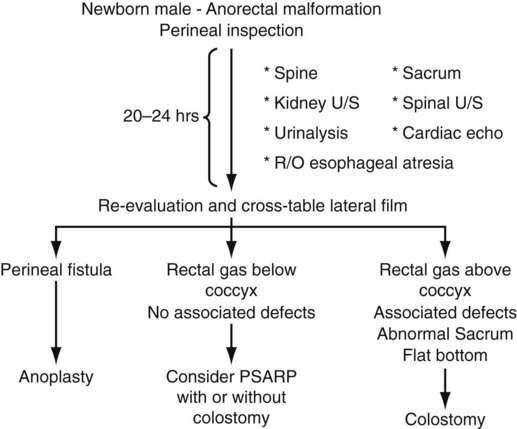
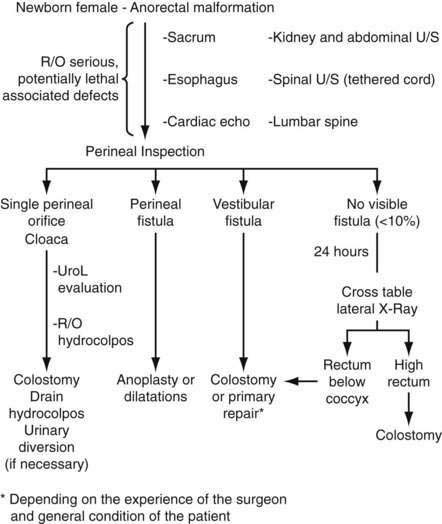
Management of Anorectal Malformations During the Neonatal Period
Males
Females
High-Pressure Distal Colostography
Step 3: Operative Steps
Males
Perineal (Cutaneous) Fistula
Rectourethral Fistula
Rectobladder Neck Fistula
Imperforate Anus Without Fistula
Rectal Atresia
Females
Vestibular Fistula
Colostomy
Definitive Repair
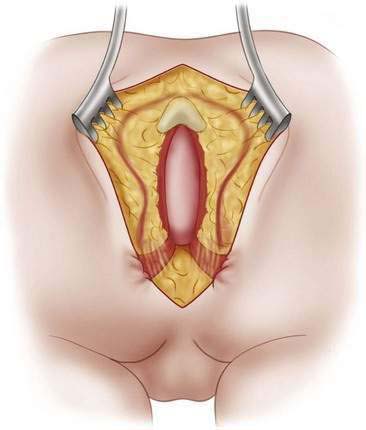
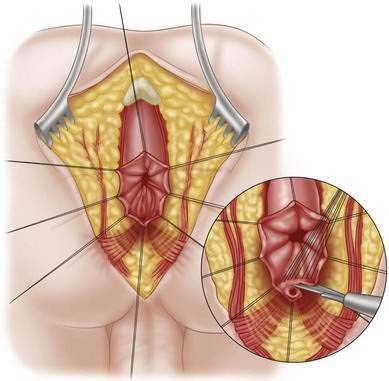
Incision
Perineal (Cutaneous) Fistulas
Rectourethral Fistula
Rectobladder Neck Fistula
Imperforate Anus Without Fistula
Rectal Atresia and Stenosis
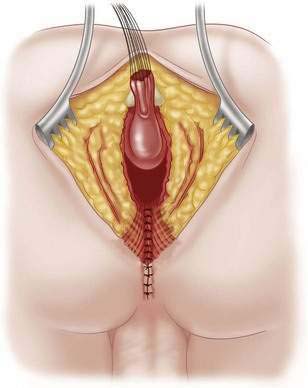
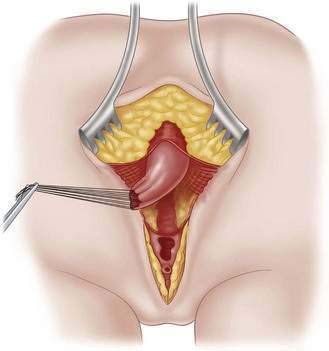
Repair in Girls
Vestibular Fistula
Rectovaginal Fistula
Step 4: Postoperative Care
Step 5: Pearls and Pitfalls
Belizon A, Levitt MA, Shoshany G, et al. Rectal prolapse following posterior sagittal anorectoplasty for anorectal malformations. J Pediatr Surg. 2005;40:192-196.
Belman BA, King LR. Urinary tract abnormalities associated with imperforate anus. J Urol. 1972;108:823-824.
Bianchi DW, Crombleholme TM, D’Alton ME. Cloacal exstrophy. In Fetology: Diagnosis and management of the fetal patient, 2nd ed. New York: McGraw-Hill, 2010; pp. 459-466
Boemers TM, de Jong TP, van Gool JD, Bax KM. Urologic problems in anorectal malformations. Part 2: Functional urologic sequelae. J Pediatr Surg. 1996;31(5):534-537.
deVries P, Peña A. Posterior sagittal anorectoplasty. J Pediatr Surg. 1982;17:638-643.
Drake JM. Occult tethered cord syndrome: not an indication for surgery. J Neurosurg. 2006;104(5):305-308.
Falcone RA, Levitt MA, Peña A, Bates MD. Increased heritability of certain phenotypes. J Pediatr Surg. 2007;42:124-128.
Georgeson K. Laparoscopic-assisted anorectal pull-through. Semin Pediatr Surg. 2007;16(4):266-269.
Georgeson KE, Inge TH, Albanese CT. Laparoscopically assisted anorectal pull-through for high imperforate anus: a new technique. J Pediatr Surg. 2000;35:927-931.
Goon HK. Repair of anorectal anomalies in the neonatal period. Pediatr Surg Int. 1990;5:246-249.
Gross GW, Wolfson PJ, Peña A. Augmented-pressure colostogram in imperforate anus with fistula. Pediatr Radiol. 1991;21:560-563.
Hong AR, Rosen N, Acuña MF, et al. Urological injuries associated with the repair of anorectal malformations in male patients. J Pediatr Surg. 2002;37:339-344.
Levitt M, Falcone R, Peña A. Pediatric fecal incontinence. In: Fecal incontinence: Diagnosis and treatment. New York: Springer; 2007:341-350.
Levitt M, Peña A. Surgery and constipation: when, how, yes, no? J Pediatr Gastroenterol Nutr. 2005;41:S58-S60.
Levitt MA, Stein DM, Peña A. Gynecological concerns in the treatment of teenagers with cloaca. J Pediatr Surg. 1998;33(2):188-193.
Livingston J, Elicevik M, Crombleholme T, et al. Prenatal diagnosis of persistent cloaca: a 10 year review. Am J Obstet Gynecol. 2006;195(6):S63.
Peña A, deVries P. Posterior sagittal anorectoplasty: important technical considerations and new applications. J Pediatr Surg. 1982;17:796-881.
Pena A, Grasshoff S, Levitt A. Reoperations for anorectal malformations. J Pediatr Surg. 2007;42:318-325.
Peña A, Guardino K, Tovilla JM, et al. Bowel management for fecal incontinence in patients with anorectal malformations. J Pediatr Surg. 1998;33(1):133-137.
Peña A, Levitt M. Colonic inertia disorders in pediatrics. Curr Prob Surg. 2002;39(7):661-730.
Peña A, Migotto-Krieger M, Levitt MA. Colostomy in anorectal malformations: a procedure with serious but preventable complications. J Pediatr Surg. 2006;41:748-756.
Seldon NR. Occult tethered cord syndrome: the case for surgery. J Neurosurg. 2006;104(5):302-304.
Shaul DB, Harrison EA. Classification of anorectal malformations—initial approach, diagnostic tests, and colostomy. Semin Pediatr Surg. 1997;6(4):187-195.
Stoll C, Alembik Y, Dott B. Associated malformations in patients with anorectal anomalies. Eur J Med Genet. 2007;50(4):281-290.
Vick LR, Gosche JR, Boulanger SC, Islam S. Primary laparoscopic repair of high imperforate anus in neonatal males. J Pediatr Surg. 2007;42:1877-1881.