Immunology of the skin
The immunological components of skin can be separated into structures, cells and immunogenetics.
Cells
Professional antigen presenting cells
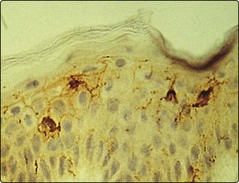
The Langerhans cells (epidermis) and dermal dendritic cells are the outermost sentinels of the cellular immune system (Fig. 1). They are dendritic, bone marrow-derived cells. Langerhans cells are characterized ultrastructurally by a unique cytoplasmic organelle known as the Birbeck granule. Recent work has shown the important role ultraviolet radiation plays in inducing photoimmunosuppression, which is mediated by effects on the skin dendritic cell population.
T lymphocytes
Different types of T cell with differing functions are recognized in the skin, for example:
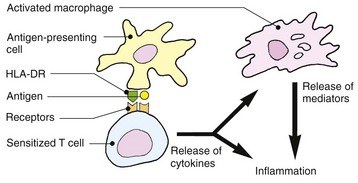
 CD4+ function is classified by cytokine production (Fig. 2), which also determines how they regulate class-switching of B cells to IgG (Th1) or IgE (Th2) production.
CD4+ function is classified by cytokine production (Fig. 2), which also determines how they regulate class-switching of B cells to IgG (Th1) or IgE (Th2) production.
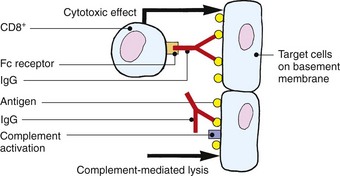
 CD8+ cells are capable of cytokine production (Tc1 and Tc2, etc.) and target cell killing mediated by granzyme B and perforin production.
CD8+ cells are capable of cytokine production (Tc1 and Tc2, etc.) and target cell killing mediated by granzyme B and perforin production.
 NKT (CD4+ or CD8+ or double or nil expressing) cells express a T cell receptor and NK cell surface markers. NKT cells are capable of high levels of cytokine production.
NKT (CD4+ or CD8+ or double or nil expressing) cells express a T cell receptor and NK cell surface markers. NKT cells are capable of high levels of cytokine production.
Immunogenetics
The tissue-type antigens of an individual are found in the MHC, located in humans on the human leucocyte antigen (HLA) gene cluster on chromosome 6. The classical HLA genes are HLA-A, B and C (MHC class I) and DP, DQ and DR (MHC class II). The MHC class I complexes (CD8+ restricted) are ubiquitously expressed but MHC class II (CD4+ restricted) is confined to professional antigen presenting cells (including B lymphocytes, Langerhans cells, dermal dendritic cells and macrophages). During inflammation, other cell types such as endothelial cells and keratinocytes can express MHC class II. There are specific HLA genes associated with an increased likelihood of certain diseases, some of which are ‘autoimmune’ in nature (Table 1).
| Disease | HLA antigen | Relative risk |
|---|---|---|
| Behçet’s disease | B5 | 10 |
| Dermatitis herpetiformis | B8DRw3 | 15>15 |
| Pemphigus | DRw4 | 10 |
| Psoriasis | B13Dw7Cw6 | 41012 |
| Psoriatic arthropathy | B27 | 10 |
| Bw38 | 9 | |
| Reiter’s disease | B27 | 35 |
Hypersensitivity reactions and the skin
Type IV (cell mediated or delayed)
Lymphocytes sensitized by cutaneous dendritic cells in the draining lymph node proliferate and undertake immunosurveillance of the tissues. On re-encounter with their cognate antigen–MHC complex, they become activated and induce inflammation and/or cell killing. From antigen exposure to sensitization takes 7–14 days. However, long-lived memory cells are able to undertake rapid expansion at a subsequent exposure and provide lasting immunity. Allergic contact dermatitis (see p. 34) and the tuberculin reaction to intradermally administered antigen are both forms of type IV reaction. The responses to skin infections such as leprosy or tuberculosis are granulomatous variants of the reaction.
Immunology
 Skin provides a physical barrier to infection and possesses antimicrobial peptides.
Skin provides a physical barrier to infection and possesses antimicrobial peptides.
 Dendritic cells in the skin, including epidermal Langerhans cells, form outposts of the cellular immune system and can present antigens to immunocompetent cells, e.g. T lymphocytes.
Dendritic cells in the skin, including epidermal Langerhans cells, form outposts of the cellular immune system and can present antigens to immunocompetent cells, e.g. T lymphocytes.
 T cells circulate through normal skin and form part of the skin-associated lymphoid tissue. They are localized by adhesion molecules.
T cells circulate through normal skin and form part of the skin-associated lymphoid tissue. They are localized by adhesion molecules.
 Keratinocytes can be immunologically active cells.
Keratinocytes can be immunologically active cells.
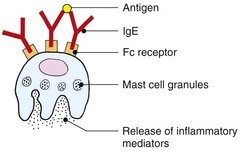
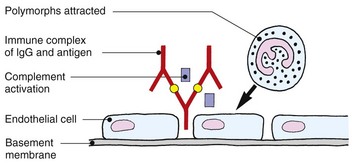
 All four types of hypersensitivity reaction occur in the skin.
All four types of hypersensitivity reaction occur in the skin.
 Genetic factors modulate immunological responses. Certain HLA antigens are associated with increased risk of skin disease, e.g. HLA-DRw4 with pemphigus.
Genetic factors modulate immunological responses. Certain HLA antigens are associated with increased risk of skin disease, e.g. HLA-DRw4 with pemphigus.